
- •Contents
- •Preface
- •Contributors
- •1 Vessels
- •1.1 Aorta, Vena Cava, and Peripheral Vessels
- •Aorta, Arteries
- •Anomalies and Variant Positions
- •Dilatation
- •Stenosis
- •Wall Thickening
- •Intraluminal Mass
- •Perivascular Mass
- •Vena Cava, Veins
- •Anomalies
- •Dilatation
- •Intraluminal Mass
- •Compression, Infiltration
- •1.2 Portal Vein and Its Tributaries
- •Enlarged Lumen Diameter
- •Portal Hypertension
- •Intraluminal Mass
- •Thrombosis
- •Tumor
- •2 Liver
- •Enlarged Liver
- •Small Liver
- •Homogeneous Hypoechoic Texture
- •Homogeneous Hyperechoic Texture
- •Regionally Inhomogeneous Texture
- •Diffuse Inhomogeneous Texture
- •Anechoic Masses
- •Hypoechoic Masses
- •Isoechoic Masses
- •Hyperechoic Masses
- •Echogenic Masses
- •Irregular Masses
- •Differential Diagnosis of Focal Lesions
- •Diagnostic Methods
- •Suspected Diagnosis
- •3 Biliary Tree and Gallbladder
- •3.1 Biliary Tree
- •Thickening of the Bile Duct Wall
- •Localized and Diffuse
- •Bile Duct Rarefaction
- •Localized and Diffuse
- •Bile Duct Dilatation and Intraductal Pressure
- •Intrahepatic
- •Hilar and Prepancreatic
- •Intrapancreatic
- •Papillary
- •Abnormal Intraluminal Bile Duct Findings
- •Foreign Body
- •The Seven Most Important Questions
- •3.2 Gallbladder
- •Changes in Size
- •Large Gallbladder
- •Small/Missing Gallbladder
- •Wall Changes
- •General Hypoechogenicity
- •General Hyperechogenicity
- •General Tumor
- •Focal Tumor
- •Intraluminal Changes
- •Hyperechoic
- •Hypoechoic
- •Nonvisualized Gallbladder
- •Missing Gallbladder
- •Obscured Gallbladder
- •4 Pancreas
- •Diffuse Pancreatic Change
- •Large Pancreas
- •Small Pancreas
- •Hypoechoic Texture
- •Hyperechoic Texture
- •Focal Changes
- •Anechoic Lesion
- •Hypoechoic Lesion
- •Isoechoic Lesion
- •Hyperechoic Lesion
- •Irregular (Complex Structured) Lesion
- •Dilatation of the Pancreatic Duct
- •Marginal/Mild Dilatation
- •Marked Dilatation
- •5 Spleen
- •Nonfocal Changes of the Spleen
- •Diffuse Parenchymal Changes
- •Large Spleen
- •Small Spleen
- •Focal Changes of the Spleen
- •Anechoic Mass
- •Hypoechoic Mass
- •Hyperechoic Mass
- •Splenic Calcification
- •6 Lymph Nodes
- •Peripheral Lymph Nodes
- •Head/Neck
- •Extremities (Axilla, Groin)
- •Abdominal Lymph Nodes
- •Porta Hepatis
- •Splenic Hilum
- •Mesentery (Celiac, Upper and Lower Mesenteric Station)
- •Stomach
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •Small/Large Intestine
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •8 Peritoneal Cavity
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Wall Structures
- •Smooth Margin
- •Irregular Margin
- •Intragastric Processes
- •Intraintestinal Processes
- •9 Kidneys
- •Anomalies, Malformations
- •Aplasia, Hypoplasia
- •Cystic Malformation
- •Anomalies of Number, Position, or Rotation
- •Fusion Anomaly
- •Anomalies of the Renal Calices
- •Vascular Anomaly
- •Diffuse Changes
- •Large Kidneys
- •Small Kidneys
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Irregular Structure
- •Circumscribed Changes
- •Anechoic Structure
- •Hypoechoic or Isoechoic Structure
- •Complex Structure
- •Hyperechoic Structure
- •10 Adrenal Glands
- •Enlargement
- •Anechoic Structure
- •Hypoechoic Structure
- •Complex Echo Structure
- •Hyperechoic Structure
- •11 Urinary Tract
- •Malformations
- •Duplication Anomalies
- •Dilatations and Stenoses
- •Dilated Renal Pelvis and Ureter
- •Anechoic
- •Hypoechoic
- •Hypoechoic
- •Hyperechoic
- •Large Bladder
- •Small Bladder
- •Altered Bladder Shape
- •Intracavitary Mass
- •Hypoechoic
- •Hyperechoic
- •Echogenic
- •Wall Changes
- •Diffuse Wall Thickening
- •Circumscribed Wall Thickening
- •Concavities and Convexities
- •12.1 The Prostate
- •Enlarged Prostate
- •Regular
- •Irregular
- •Small Prostate
- •Regular
- •Echogenic
- •Circumscribed Lesion
- •Anechoic
- •Hypoechoic
- •Echogenic
- •12.2 Seminal Vesicles
- •Diffuse Change
- •Hypoechoic
- •Circumscribed Change
- •Anechoic
- •Echogenic
- •Irregular
- •12.3 Testis, Epididymis
- •Diffuse Change
- •Enlargement
- •Decreased Size
- •Circumscribed Lesion
- •Anechoic or Hypoechoic
- •Irregular/Echogenic
- •Epididymal Lesion
- •Anechoic
- •Hypoechoic
- •Intrascrotal Mass
- •Anechoic or Hypoechoic
- •Echogenic
- •13 Female Genital Tract
- •Masses
- •Abnormalities of Size or Shape
- •Uterus
- •Abnormalities of Size or Shape
- •Myometrial Changes
- •Intracavitary Changes
- •Endometrial Changes
- •Fallopian Tubes
- •Hypoechoic Mass
- •Anechoic Cystic Mass
- •Solid Echogenic or Nonhomogeneous Mass
- •14 Thyroid Gland
- •Diffuse Changes
- •Enlarged Thyroid Gland
- •Small Thyroid Gland
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Circumscribed Changes
- •Anechoic
- •Hypoechoic
- •Isoechoic
- •Hyperechoic
- •Irregular
- •Differential Diagnosis of Hyperthyroidism
- •Types of Autonomy
- •15 Pleura and Chest Wall
- •Chest Wall
- •Masses
- •Parietal Pleura
- •Nodular Masses
- •Diffuse Pleural Thickening
- •Pleural Effusion
- •Anechoic Effusion
- •Echogenic Effusion
- •Complex Effusion
- •16 Lung
- •Masses
- •Anechoic Masses
- •Hypoechoic Masses
- •Complex Masses
- •Index
12
Intrascrotal Mass
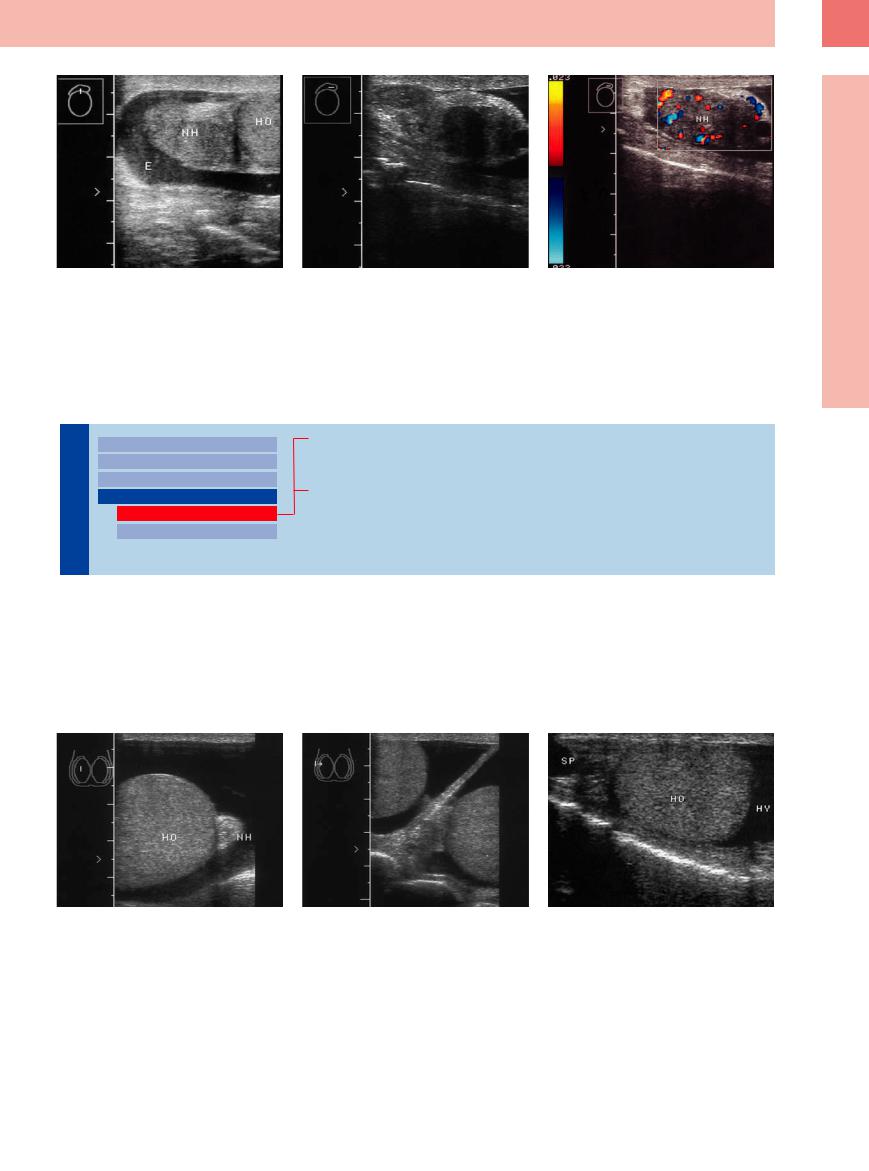
Fig. 12.34 Epididymitis. |
b Left epididymis: hypoechoic mass. |
c Color Doppler shows conspicuous vascularity. |
a Enlarged epididymis (NH) with accompanying inflam- |
|
|
matory fluid (hydrocele; E). HO = testis. |
|
|
■ Intrascrotal Mass
Anechoic or Hypoechoic
Epididymis |
|
|
Diffuse Change |
|
|
|
|
||
|
|
|
Circumscribed Lesion |
|
|
|
|||
|
|
|
Epididymal Lesion |
|
|
|
|
||
|
|
|
Intrascrotal Mass |
|
|
|
|||
Testis, |
|
|
|
Anechoic or Hypoechoic |
|
|
|
||
|
|
|
Echogenic |
|
|
|
|
|
|
Hydrocele
Varicocele
Hematocele
Hydrocele 






















































The normal scrotum contains a small amount of serous fluid between the two layers (visceral layer and parietal layer) of the tunica vaginalis of the testis. A hydrocele is a collection of watery fluid in the tunica vaginalis. It often communicates with ascitic fluid in the abdomi-
nal cavity, the pressure rise in the abdomen causing the previously closed vaginal process to become patent. Inflammatory hydroceles are also common, however (e. g., secondary to epididymitis), and cause a cyst-like expansion of the tunica vaginalis. Transient hydroceles are
also occasionally detected in small infants. Internal echoes suggest infected hydrocele. Hydrocele occurs also in testicular torsion, tumors, and trauma (Fig.12.35).
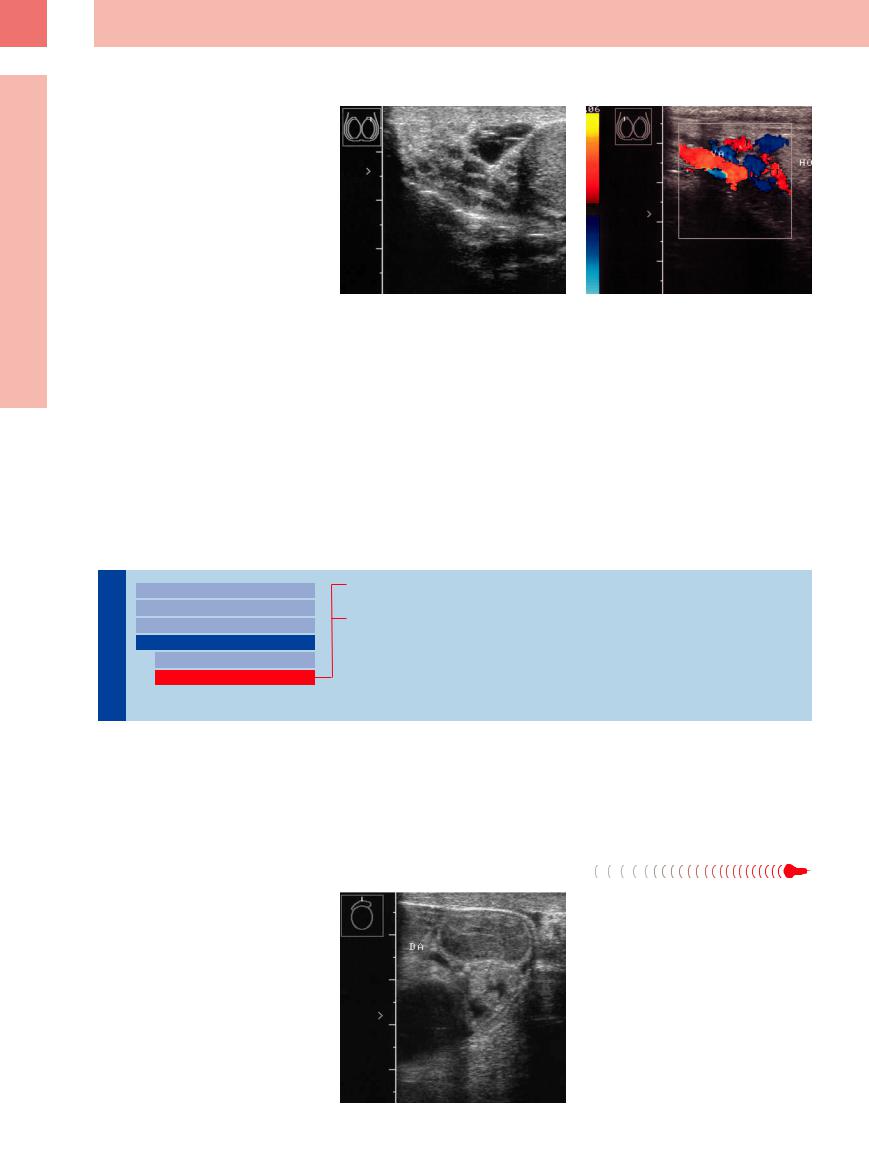
Fig. 12.35 a and b Bilateral hydroceles.
a Right side: testis (HO) and epididymis (NH) surrounded by fluid.
b Sections of both testes with scrotal septum.
c Hydrocele (HY) and spermatocele (SP): anechoic mass around the testis (HO). The spermatocele does not change its position, unlike the mobile fluid in the hydrocele.
435
12
Prostate, Seminal Vesicles, Testis, Epididymis
Varicocele 






















































A varicocele is defined as a palpable and visible dilatation of the veins of the pampiniform plexus. It is caused by retrograde flow in the testicular vein or by an absence of venous valves. It occurs predominantly on the left side and is occasionally bilateral. Treatment is unnecessary in patients who have no complaints and a normal semen analysis or azoospermia. Otherwise, surveillance should be maintained to assess the need for operative treatment.
Ultrasound demonstrates convoluted, anechoic venous structures arranged around the testis, with a luminal diameter greater than 2 mm. Color duplex examination reveals lowflow waveforms. If no flow is detected, the stasis may be caused by intra-abdominal or retroperitoneal tumor compression or tumor invasion of the testicular vein, which is occasionally definable with ultrasound in thin patients. Varicocele occurs more commonly on
Fig. 12.36 Varicocele.
a B-mode image of the right testis: multiple anechoic foci of vascular ectasia around the epididymis.
the left side. A rarer form is a hydrocele radiating into the testis of up to 2 cm in diameter (intratesticular hydrocele). They are to be con-
b Color Doppler during a Valsalva maneuver shows extensive vascularity. HO = testis; VA = varicocele.
sidered suspect until a tumor is disproved: a cystic appearance with Doppler signals in CDS is a neoplasia (Fig.12.36).
Hematocele 





















































A hematocele is a collection of free blood in the |
dominantly anechoic, hypoechoic, or even ir- |
scrotal cavity. It is generally preceded by sur- |
regular mass, depending on the age of the |
gical or other trauma. Ultrasound shows a pre- |
hematoma (Fig.12.29, Fig.12.30). |
Echogenic
Epididymis |
|
|
Diffuse Change |
|
|
|
|
||
|
|
|
Circumscribed Lesion |
|
|
|
|||
|
|
|
Epididymal Lesion |
|
|
|
|
||
|
|
|
Intrascrotal Mass |
|
|
|
|||
Testis, |
|
|
|
Anechoic or Hypoechoic |
|
|
|
Echogenic |
|
|
|
|
|
|
Fibroma of the Tunica/Corpus Librum
Scrotal Hernia
Fibroma of the Tunica/Corpus Librum
the Tunica/Corpus Librum 







































Benign intrascrotal fibrous proliferation, often |
the scrotum may represent a loose body (cor- |
affecting the tunica (fibrous pseudotumor), is |
pus librum) caused by torsion of the appendix |
difficult to distinguish from a malignant tumor. |
testis, residuals from the hydatid of Morgagni. |
It can be hyperechoic. Calcified bodies within |
|
Scrotal Hernia





























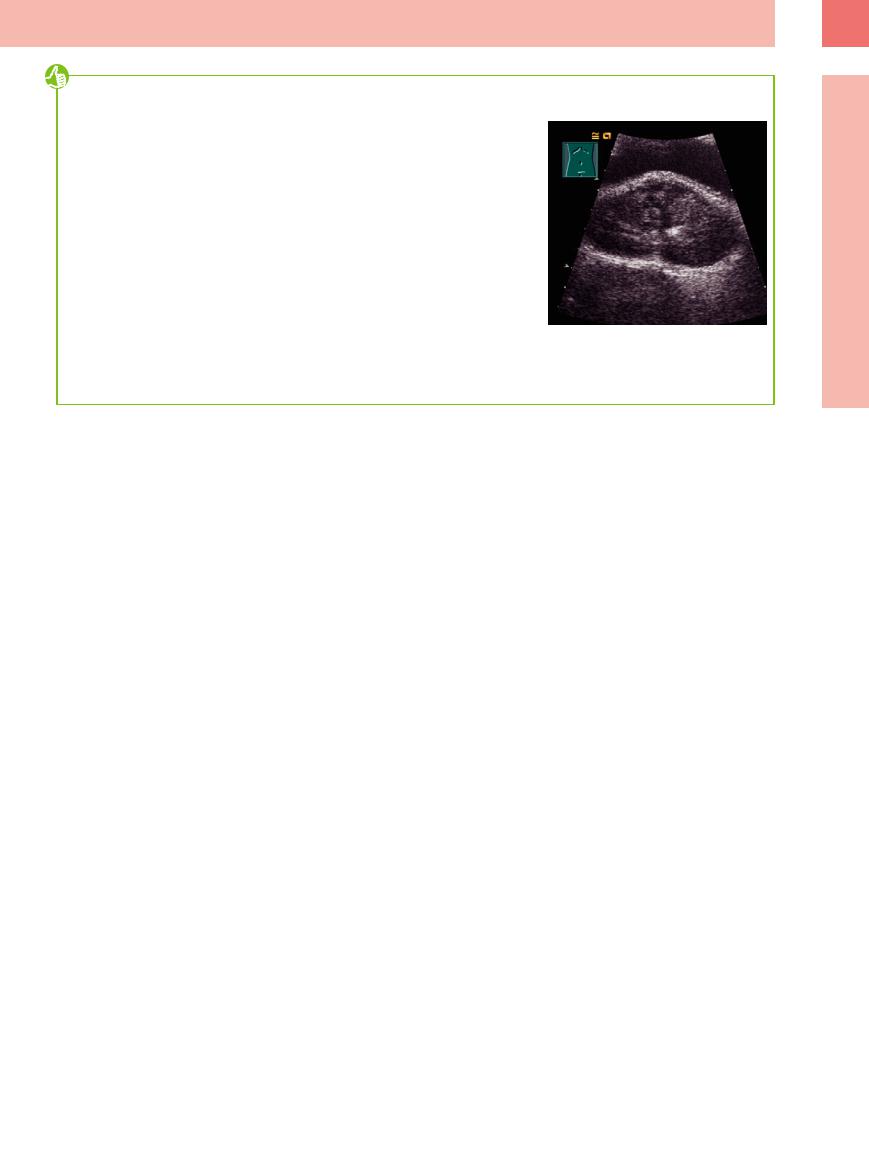
Sonography is an excellent modality for the investigation of intrascrotal swelling. One cause of such swelling is a scrotal hernia. The hernial sac is found to contain bowel structures, which are easily identified as such with ultrasound (Fig.12.37).
Fig. 12.37 Scrotal hernia: hyperechoic bowel structures within the scrotal cavity. DA = intestine.
436
Tips, tricks, and pitfalls
General
●When examining the pelvis systematically the bladder must be filled; with a voided bladder some abnormalities may not be noticed.
●Integrate the patient’s history and clinical examination.
●Pay attention to the complex anatomy: the prostate first comes into view only when the full bladder is followed and the scan direction is directed into the depths of the pelvis; the seminal vesicles are located cranially and dorsally to the prostate.
●Use of CDS and CEUS.
●Use of differentiated examination technique has great significance in diagnosing the pelvic organs: pelvic wall, rectum (wall thickness, carcinoma?), endosonography (TRUS of the prostate, staging; Fig. 12.10b).
References
[1]Böcking A, Riede UN. Vorsteherdrüse. In: Riede UN, Schaefer HE (eds.). Allgemeine und spezielle Pathologie. Stuttgart: Thieme, 1993
[2]Terris MK, Stamey TA. Determination of prostate volume by transrectal ultrasound. J Urol 1991;145(5):984–987
[3]Edge S, Byrd DR, Compton CC, et al. (eds.). AJCC Cancer Staging Manual. 7th ed. Berlin: Springer, 2010
Special
●Carry out forced diuresis for differentiating the wall layers of the bladder including the ureterovesical junction and the rectosigmoid.
●Examination and measurement of the prostate in older men: a large prostate protruding into the bladder floor is BPH and not a carcinoma (Fig. 12.38); the latter develop in the outer and dorsal zone. Abdominal ultrasound is not useful in the early detection of prostate cancer.
●Suppurative infection of the seminal vesicles may produce uncertain lower abdominal pain, therefore include them in the examination.
●Don’t forget: inguinal ring; iliac vessels.
[4]Cooner WH, Mosley BR, Rutherford CL Jr, et al. Prostate cancer detection in a clinical urological practice by ultrasonography, digital rectal examination and prostate specific antigen. J Urol 1990;143(6):1146–1152, discussion 1152–1154
[5]Schröder FH, Hugosson J, Roobol MJ, et al; ERSPC Investigators. Prostate-cancer mortality at 11 years of follow-up. N Engl J Med 2012;366(11):981–990
[6]Fabricus PG. Prostataund Samenblasentumoren. In: Jocham D, Miller K (eds.). Praxis der Urologie. Stuttgart: Thieme, 1994
Fig. 12.38 Enlarged irregular median lobe of the prostate. Indentation of the bladder floor and dorsal displacement of the remaining parts of the prostate; no cancer.
[7]Frentzel-Beyme B. Sonographie der Prostata. Radiologe 1994;34:109–115
[8]Waterhouse RL, Resnick MI. The use of transrectal prostatic ultrasonography in the evaluation of patients with prostatic carcinoma. J Urol 1989;141(2):233–239
[9]Middleton WD, Siegel BA, Melson GL, Yates CK, Andriole GL. Acute scrotal disorders: prospective comparison of color Doppler US and testicular scintigraphy. Radiology 1990; 177(1):177–181
[10]Schwerk WB, Schwerk WN. Sonographie des Skrotalinhaltes. In: Braun G, Schwerk WB (eds.). Ultraschalldiagnostik. Ecomed, 1994
12
Intrascrotal Mass
437

