
- •Contents
- •Preface
- •Contributors
- •1 Vessels
- •1.1 Aorta, Vena Cava, and Peripheral Vessels
- •Aorta, Arteries
- •Anomalies and Variant Positions
- •Dilatation
- •Stenosis
- •Wall Thickening
- •Intraluminal Mass
- •Perivascular Mass
- •Vena Cava, Veins
- •Anomalies
- •Dilatation
- •Intraluminal Mass
- •Compression, Infiltration
- •1.2 Portal Vein and Its Tributaries
- •Enlarged Lumen Diameter
- •Portal Hypertension
- •Intraluminal Mass
- •Thrombosis
- •Tumor
- •2 Liver
- •Enlarged Liver
- •Small Liver
- •Homogeneous Hypoechoic Texture
- •Homogeneous Hyperechoic Texture
- •Regionally Inhomogeneous Texture
- •Diffuse Inhomogeneous Texture
- •Anechoic Masses
- •Hypoechoic Masses
- •Isoechoic Masses
- •Hyperechoic Masses
- •Echogenic Masses
- •Irregular Masses
- •Differential Diagnosis of Focal Lesions
- •Diagnostic Methods
- •Suspected Diagnosis
- •3 Biliary Tree and Gallbladder
- •3.1 Biliary Tree
- •Thickening of the Bile Duct Wall
- •Localized and Diffuse
- •Bile Duct Rarefaction
- •Localized and Diffuse
- •Bile Duct Dilatation and Intraductal Pressure
- •Intrahepatic
- •Hilar and Prepancreatic
- •Intrapancreatic
- •Papillary
- •Abnormal Intraluminal Bile Duct Findings
- •Foreign Body
- •The Seven Most Important Questions
- •3.2 Gallbladder
- •Changes in Size
- •Large Gallbladder
- •Small/Missing Gallbladder
- •Wall Changes
- •General Hypoechogenicity
- •General Hyperechogenicity
- •General Tumor
- •Focal Tumor
- •Intraluminal Changes
- •Hyperechoic
- •Hypoechoic
- •Nonvisualized Gallbladder
- •Missing Gallbladder
- •Obscured Gallbladder
- •4 Pancreas
- •Diffuse Pancreatic Change
- •Large Pancreas
- •Small Pancreas
- •Hypoechoic Texture
- •Hyperechoic Texture
- •Focal Changes
- •Anechoic Lesion
- •Hypoechoic Lesion
- •Isoechoic Lesion
- •Hyperechoic Lesion
- •Irregular (Complex Structured) Lesion
- •Dilatation of the Pancreatic Duct
- •Marginal/Mild Dilatation
- •Marked Dilatation
- •5 Spleen
- •Nonfocal Changes of the Spleen
- •Diffuse Parenchymal Changes
- •Large Spleen
- •Small Spleen
- •Focal Changes of the Spleen
- •Anechoic Mass
- •Hypoechoic Mass
- •Hyperechoic Mass
- •Splenic Calcification
- •6 Lymph Nodes
- •Peripheral Lymph Nodes
- •Head/Neck
- •Extremities (Axilla, Groin)
- •Abdominal Lymph Nodes
- •Porta Hepatis
- •Splenic Hilum
- •Mesentery (Celiac, Upper and Lower Mesenteric Station)
- •Stomach
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •Small/Large Intestine
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •8 Peritoneal Cavity
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Wall Structures
- •Smooth Margin
- •Irregular Margin
- •Intragastric Processes
- •Intraintestinal Processes
- •9 Kidneys
- •Anomalies, Malformations
- •Aplasia, Hypoplasia
- •Cystic Malformation
- •Anomalies of Number, Position, or Rotation
- •Fusion Anomaly
- •Anomalies of the Renal Calices
- •Vascular Anomaly
- •Diffuse Changes
- •Large Kidneys
- •Small Kidneys
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Irregular Structure
- •Circumscribed Changes
- •Anechoic Structure
- •Hypoechoic or Isoechoic Structure
- •Complex Structure
- •Hyperechoic Structure
- •10 Adrenal Glands
- •Enlargement
- •Anechoic Structure
- •Hypoechoic Structure
- •Complex Echo Structure
- •Hyperechoic Structure
- •11 Urinary Tract
- •Malformations
- •Duplication Anomalies
- •Dilatations and Stenoses
- •Dilated Renal Pelvis and Ureter
- •Anechoic
- •Hypoechoic
- •Hypoechoic
- •Hyperechoic
- •Large Bladder
- •Small Bladder
- •Altered Bladder Shape
- •Intracavitary Mass
- •Hypoechoic
- •Hyperechoic
- •Echogenic
- •Wall Changes
- •Diffuse Wall Thickening
- •Circumscribed Wall Thickening
- •Concavities and Convexities
- •12.1 The Prostate
- •Enlarged Prostate
- •Regular
- •Irregular
- •Small Prostate
- •Regular
- •Echogenic
- •Circumscribed Lesion
- •Anechoic
- •Hypoechoic
- •Echogenic
- •12.2 Seminal Vesicles
- •Diffuse Change
- •Hypoechoic
- •Circumscribed Change
- •Anechoic
- •Echogenic
- •Irregular
- •12.3 Testis, Epididymis
- •Diffuse Change
- •Enlargement
- •Decreased Size
- •Circumscribed Lesion
- •Anechoic or Hypoechoic
- •Irregular/Echogenic
- •Epididymal Lesion
- •Anechoic
- •Hypoechoic
- •Intrascrotal Mass
- •Anechoic or Hypoechoic
- •Echogenic
- •13 Female Genital Tract
- •Masses
- •Abnormalities of Size or Shape
- •Uterus
- •Abnormalities of Size or Shape
- •Myometrial Changes
- •Intracavitary Changes
- •Endometrial Changes
- •Fallopian Tubes
- •Hypoechoic Mass
- •Anechoic Cystic Mass
- •Solid Echogenic or Nonhomogeneous Mass
- •14 Thyroid Gland
- •Diffuse Changes
- •Enlarged Thyroid Gland
- •Small Thyroid Gland
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Circumscribed Changes
- •Anechoic
- •Hypoechoic
- •Isoechoic
- •Hyperechoic
- •Irregular
- •Differential Diagnosis of Hyperthyroidism
- •Types of Autonomy
- •15 Pleura and Chest Wall
- •Chest Wall
- •Masses
- •Parietal Pleura
- •Nodular Masses
- •Diffuse Pleural Thickening
- •Pleural Effusion
- •Anechoic Effusion
- •Echogenic Effusion
- •Complex Effusion
- •16 Lung
- •Masses
- •Anechoic Masses
- •Hypoechoic Masses
- •Complex Masses
- •Index
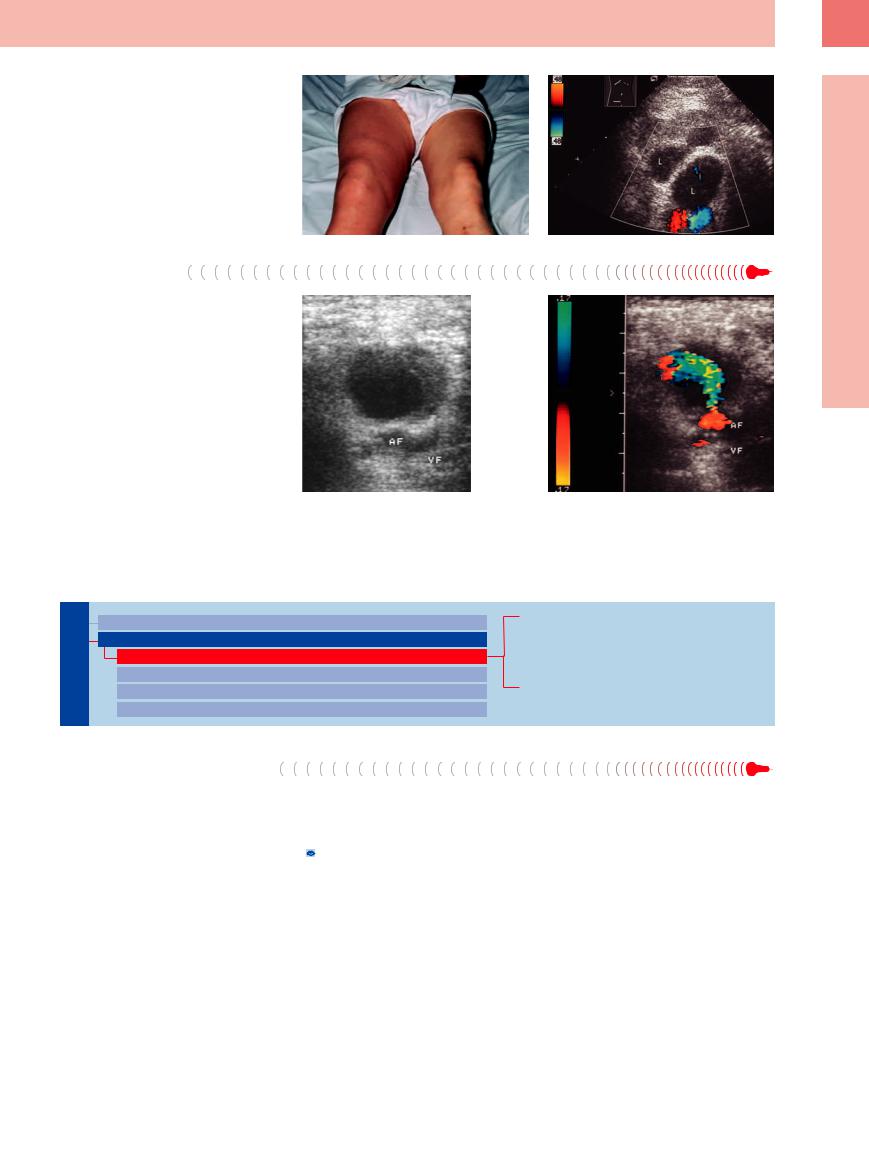
Fig. 6.24
a A 55-year-old patient with swollen right leg.
b Ultrasound showed multiple abnormally large lymph nodes (L) without any sign of deep venous thrombosis. Needle biopsy confirmed the diagnosis of Hodgkin disease. The swollen leg was explained by impaired lymphatic drainage.
Other Structures
●Axilla. Scar, postoperative fibrosis, seroma, thrombosis of the axillary vein, cellulitis, panniculitis, abscess, myositis.
●Groin. Undescended testis, inguinal hernia, varicosity, lymphocele, hematoma, abscess, false aneurysm (Fig. 6.25).
Fig. 6.25
a Mass with liquefied center in the right groin. AF = femoral artery; VF = femoral vein.
b Color-flow Doppler imaging confirmed the diagnosis of a false aneurysm.
■ Abdominal Lymph Nodes
Porta Hepatis
Nodes |
Peripheral Lymph Nodes |
Inflammatory Lymph Nodes |
|
Abdominal Lymph Nodes |
Metastases |
||
Porta Hepatis |
Malignant Lymphoma |
||
Lymph |
|||
Splenic Hilum |
Other Structures |
||
|
|||
Mesentery (Celiac, Upper and Lower Mesenteric Station) |
|||
Retroperitoneum (Para-Aortic, Paracaval, Aortointercaval, and Iliac Station) |
|||
|
|||
Inflammatory Lymph Nodes |
|
||
Enlarged inflammatory lymph nodes at the |
comitant hepatitis (Epstein–Barr virus infec- |
||
porta hepatis are quite common and can easily |
tion, chickenpox, HIV, etc.), autoimmune hep- |
||
be demonstrated on ultrasound. Most of these |
atitis, primary biliary cirrhosis, primary scle- |
||
lymph nodes are small (<2 cm), ovoid or elon- |
rosing cholangitis, and bacterial cholangitis |
||
gated, and likely echogenic. They are almost |
( 6.6). |
||
always found in acute hepatitis (A, B, C), con- |
|
||
6
Abdominal Lymph Nodes
247
6
Lymph Nodes
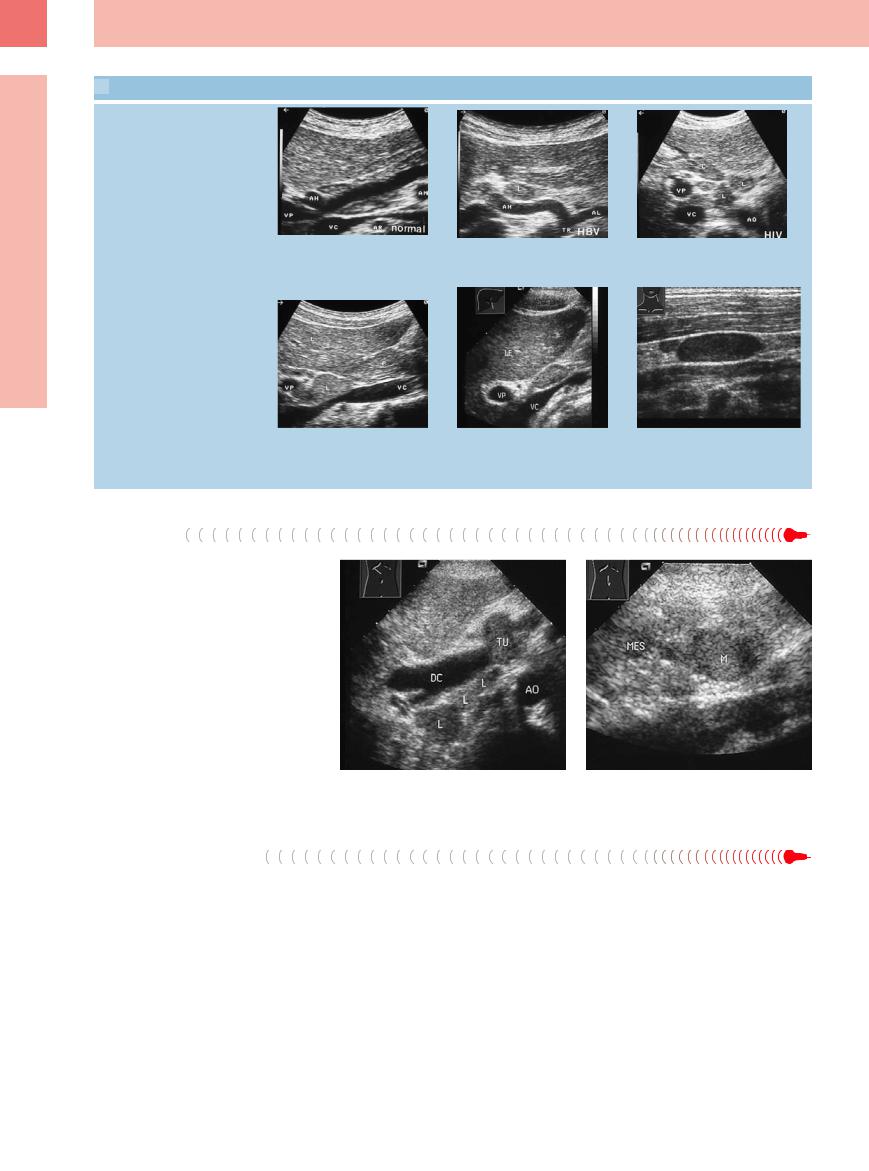
 6.6 Enlarged Reactive Lymph Nodes at the Porta Hepatis
6.6 Enlarged Reactive Lymph Nodes at the Porta Hepatis
Without clinical symptoms: hepatitis,
HIV
a Enlarged lymph node (cursors) with subtle hilar signs in an asymptomatic patient.
Cholangitis, mononucleosis
d Enlarged reactive lymph node (L) in primary sclerosing cholangitis. DC = common bile duct; P = pancreas; VC = vena cava; VP = portal vein.
b Enlarged echogenic lymph (L) node in hepatitis. AH = hepatic artery; AL = splenic artery; TR = celiac axis.
e and f Mononucleosis.
e Echogenic lymph node at the porta hepatis. LE = liver; VC = vena cava; VP = portal vein.
c Enlarged lymph node (L) in an HIV-pos- itive patient. AO = aorta; VC = vena cava; VP = portal vein.
f Hypoechoic cervical lymph node. The echogenicity depends on the localization.
Metastases
There are no definite ultrasound criteria for ruling out possible malignancy. Enlarged lymph nodes in primary tumors of the liver will be diagnosed as definite metastasis or reactive lymphadenitis only after surgery; however, it can be stated that the probability of malignant invasion will increase with increasing size of the lymph node (Fig. 6.26).
|
Fig. 6.26a and b Enlarged lymph node (L) in pancreatic cancer (TU). Only histology can confirm possible lymph node |
|
metastasis. AO = aorta; DC = common hepatic duct; M = mesenteric lymph node; MES = mesentery. |
Malignant Lymphoma |
|
Involvement of the porta hepatis is observed |
branches close to the hilum (so-called “peri- |
particularly in systemic low-grade lymphoma. |
portal cuffing”) has to be differentiated from |
Different patterns of invasion have been noted |
actual lymphoma involving the porta hepatis. |
(Fig. 6.7). Hypoechoic perivascular transforma- |
Periportal cuffing is more likely to be found in |
tion of the portal vein and its intrahepatic |
impaired lymphatic drainage (Fig. 6.27). |
248
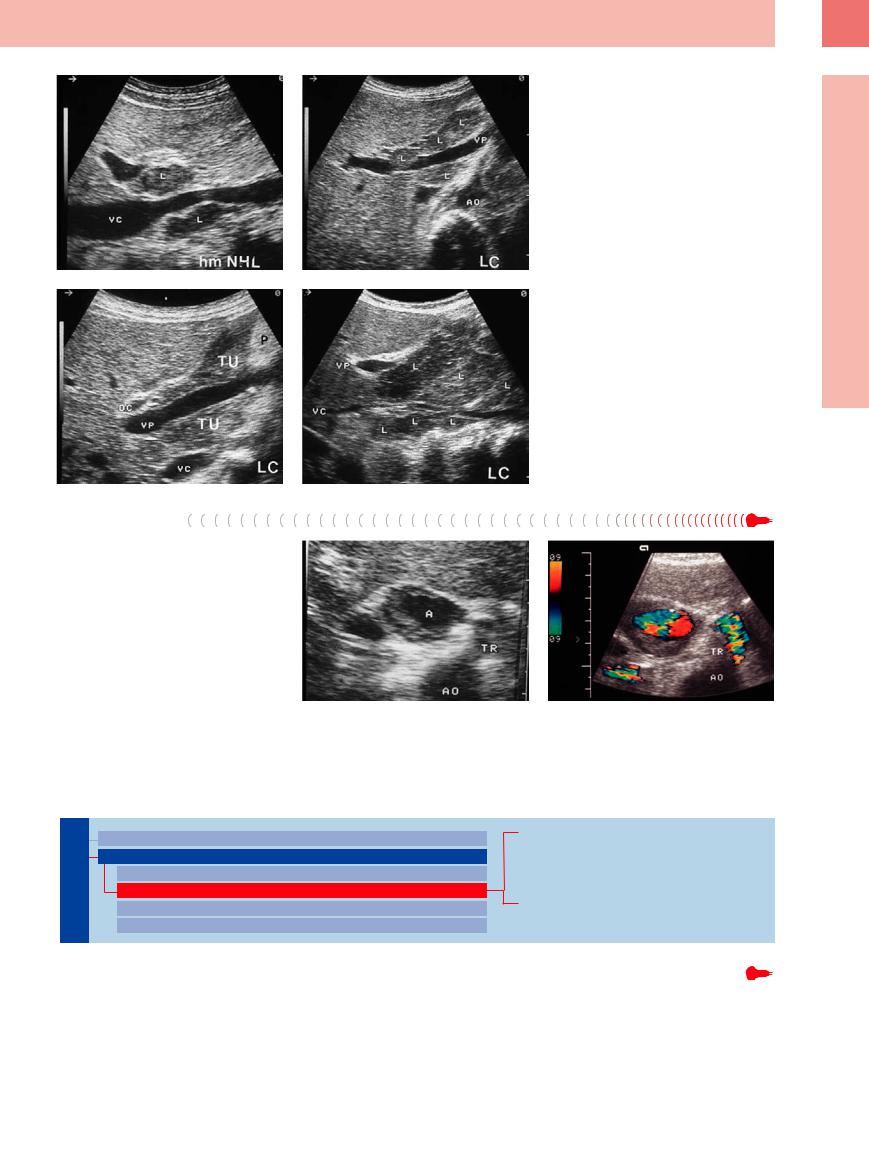
Fig. 6.27 Different invasion patterns in lymph nodes (L) of the porta hepatis in malignant melanoma. L = lymph node; VC = vena cava; VP = portal vein; AO = aorta.
a Individual lymph nodes in high-grade lymphoma.
b Multiple lymph nodes in lymphocytic lymphoma (LC).
c Extensive lymph nodes (TU) in lymphocytic lymphoma.
d Large “bulky” tumor transformation in lymphocytic lymphoma. DC = common bile duct; VP = portal vein; VC = vena cava; P = pancreas.
6
Abdominal Lymph Nodes
Other Structures
●Hematoma at the porta hepatis, abscess.
●Cavernous transformation of the portal vein, thrombosis of the portal vein, varicosities in portal hypertension, aneurysm of the hepatic artery (Fig. 6.28).
Fig. 6.28
a Hypoechoic mass with anechoic center (A). TR = celiac axis; AO = aorta.
b Color-flow Doppler scanning confirms the tentative diagnosis of hepatic artery aneurysm.
Splenic Hilum
Lymph Nodes
Peripheral Lymph Nodes
Abdominal Lymph Nodes
Porta Hepatis
Splenic Hilum
Mesentery (Celiac, Upper and Lower Mesenteric Station)
Retroperitoneum (Para-Aortic, Paracaval, Aortointercaval, and Iliac Station)
Inflammatory Lymph Nodes
Metastases
Malignant Lymphoma
Other Structures
Inflammatory Lymph Nodes 












































Enlargement of the lymph nodes of the splenic hilum is somewhat infrequent but is visualized quite well by insonation through the spleen. Reactive lymphadenitis of lymph nodes at the splenic hilum is almost never seen.
249
6
Lymph Nodes
Metastases
Metastases have been demonstrated in adenocarcinoma of the pancreatic tail, neuroendocrine tumors of the pancreas, gastric cancer, and less frequently in peritoneal metastasis. The principal misgivings about assessment of possible malignancy apply here as well. Possible invasion of the tumor into the spleen can be demonstrated on ultrasound (Fig. 6.29).
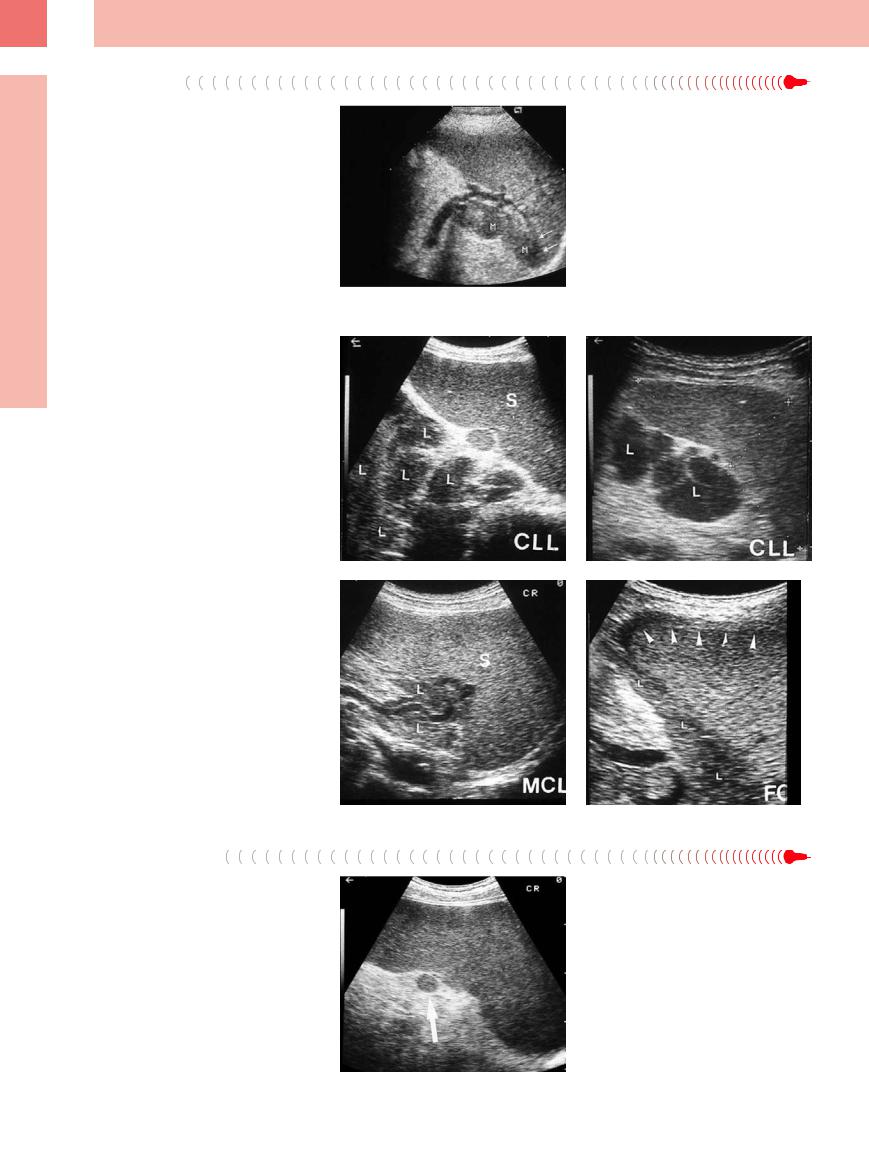
Fig. 6.29 Lymph node metastasis at the splenic hilum in ovarian cancer. M = stomach.
Malignant Lymphoma
















































It is particularly the low-grade lymphomas that display involvement of the splenic hilum as part of systemic disease (Fig. 6.30).
Fig. 6.30 Different invasion patterns visualized in lymph nodes (L) of the splenic hilum in malignant lymphoma. S = spleen.
a Individual lymph nodes in chronic lymphocytic leukemia (CLL).
b Numerous confluent lymph nodes in CLL.
c Diffuse lymph node infiltration of a mantle cell lymphoma (MCL).
d Perisplenic invasion by follicular center lymphoma.
Other Structures
●Accessory spleen (Fig. 6.31), abscess
●Pancreatic mass (tumor, cyst, necrosis) (Fig. 6.32)
●Adrenal mass (metastasis, pheochromocytoma, incidentaloma)
●Vascular process (splenic varicosity, thrombosis of the splenic vein, splenic artery aneurysm)
Fig. 6.31 Small accessory spleen (arrow) at the splenic hilum in CLL.
250
