
- •Contents
- •Preface
- •Contributors
- •1 Vessels
- •1.1 Aorta, Vena Cava, and Peripheral Vessels
- •Aorta, Arteries
- •Anomalies and Variant Positions
- •Dilatation
- •Stenosis
- •Wall Thickening
- •Intraluminal Mass
- •Perivascular Mass
- •Vena Cava, Veins
- •Anomalies
- •Dilatation
- •Intraluminal Mass
- •Compression, Infiltration
- •1.2 Portal Vein and Its Tributaries
- •Enlarged Lumen Diameter
- •Portal Hypertension
- •Intraluminal Mass
- •Thrombosis
- •Tumor
- •2 Liver
- •Enlarged Liver
- •Small Liver
- •Homogeneous Hypoechoic Texture
- •Homogeneous Hyperechoic Texture
- •Regionally Inhomogeneous Texture
- •Diffuse Inhomogeneous Texture
- •Anechoic Masses
- •Hypoechoic Masses
- •Isoechoic Masses
- •Hyperechoic Masses
- •Echogenic Masses
- •Irregular Masses
- •Differential Diagnosis of Focal Lesions
- •Diagnostic Methods
- •Suspected Diagnosis
- •3 Biliary Tree and Gallbladder
- •3.1 Biliary Tree
- •Thickening of the Bile Duct Wall
- •Localized and Diffuse
- •Bile Duct Rarefaction
- •Localized and Diffuse
- •Bile Duct Dilatation and Intraductal Pressure
- •Intrahepatic
- •Hilar and Prepancreatic
- •Intrapancreatic
- •Papillary
- •Abnormal Intraluminal Bile Duct Findings
- •Foreign Body
- •The Seven Most Important Questions
- •3.2 Gallbladder
- •Changes in Size
- •Large Gallbladder
- •Small/Missing Gallbladder
- •Wall Changes
- •General Hypoechogenicity
- •General Hyperechogenicity
- •General Tumor
- •Focal Tumor
- •Intraluminal Changes
- •Hyperechoic
- •Hypoechoic
- •Nonvisualized Gallbladder
- •Missing Gallbladder
- •Obscured Gallbladder
- •4 Pancreas
- •Diffuse Pancreatic Change
- •Large Pancreas
- •Small Pancreas
- •Hypoechoic Texture
- •Hyperechoic Texture
- •Focal Changes
- •Anechoic Lesion
- •Hypoechoic Lesion
- •Isoechoic Lesion
- •Hyperechoic Lesion
- •Irregular (Complex Structured) Lesion
- •Dilatation of the Pancreatic Duct
- •Marginal/Mild Dilatation
- •Marked Dilatation
- •5 Spleen
- •Nonfocal Changes of the Spleen
- •Diffuse Parenchymal Changes
- •Large Spleen
- •Small Spleen
- •Focal Changes of the Spleen
- •Anechoic Mass
- •Hypoechoic Mass
- •Hyperechoic Mass
- •Splenic Calcification
- •6 Lymph Nodes
- •Peripheral Lymph Nodes
- •Head/Neck
- •Extremities (Axilla, Groin)
- •Abdominal Lymph Nodes
- •Porta Hepatis
- •Splenic Hilum
- •Mesentery (Celiac, Upper and Lower Mesenteric Station)
- •Stomach
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •Small/Large Intestine
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •8 Peritoneal Cavity
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Wall Structures
- •Smooth Margin
- •Irregular Margin
- •Intragastric Processes
- •Intraintestinal Processes
- •9 Kidneys
- •Anomalies, Malformations
- •Aplasia, Hypoplasia
- •Cystic Malformation
- •Anomalies of Number, Position, or Rotation
- •Fusion Anomaly
- •Anomalies of the Renal Calices
- •Vascular Anomaly
- •Diffuse Changes
- •Large Kidneys
- •Small Kidneys
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Irregular Structure
- •Circumscribed Changes
- •Anechoic Structure
- •Hypoechoic or Isoechoic Structure
- •Complex Structure
- •Hyperechoic Structure
- •10 Adrenal Glands
- •Enlargement
- •Anechoic Structure
- •Hypoechoic Structure
- •Complex Echo Structure
- •Hyperechoic Structure
- •11 Urinary Tract
- •Malformations
- •Duplication Anomalies
- •Dilatations and Stenoses
- •Dilated Renal Pelvis and Ureter
- •Anechoic
- •Hypoechoic
- •Hypoechoic
- •Hyperechoic
- •Large Bladder
- •Small Bladder
- •Altered Bladder Shape
- •Intracavitary Mass
- •Hypoechoic
- •Hyperechoic
- •Echogenic
- •Wall Changes
- •Diffuse Wall Thickening
- •Circumscribed Wall Thickening
- •Concavities and Convexities
- •12.1 The Prostate
- •Enlarged Prostate
- •Regular
- •Irregular
- •Small Prostate
- •Regular
- •Echogenic
- •Circumscribed Lesion
- •Anechoic
- •Hypoechoic
- •Echogenic
- •12.2 Seminal Vesicles
- •Diffuse Change
- •Hypoechoic
- •Circumscribed Change
- •Anechoic
- •Echogenic
- •Irregular
- •12.3 Testis, Epididymis
- •Diffuse Change
- •Enlargement
- •Decreased Size
- •Circumscribed Lesion
- •Anechoic or Hypoechoic
- •Irregular/Echogenic
- •Epididymal Lesion
- •Anechoic
- •Hypoechoic
- •Intrascrotal Mass
- •Anechoic or Hypoechoic
- •Echogenic
- •13 Female Genital Tract
- •Masses
- •Abnormalities of Size or Shape
- •Uterus
- •Abnormalities of Size or Shape
- •Myometrial Changes
- •Intracavitary Changes
- •Endometrial Changes
- •Fallopian Tubes
- •Hypoechoic Mass
- •Anechoic Cystic Mass
- •Solid Echogenic or Nonhomogeneous Mass
- •14 Thyroid Gland
- •Diffuse Changes
- •Enlarged Thyroid Gland
- •Small Thyroid Gland
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Circumscribed Changes
- •Anechoic
- •Hypoechoic
- •Isoechoic
- •Hyperechoic
- •Irregular
- •Differential Diagnosis of Hyperthyroidism
- •Types of Autonomy
- •15 Pleura and Chest Wall
- •Chest Wall
- •Masses
- •Parietal Pleura
- •Nodular Masses
- •Diffuse Pleural Thickening
- •Pleural Effusion
- •Anechoic Effusion
- •Echogenic Effusion
- •Complex Effusion
- •16 Lung
- •Masses
- •Anechoic Masses
- •Hypoechoic Masses
- •Complex Masses
- •Index
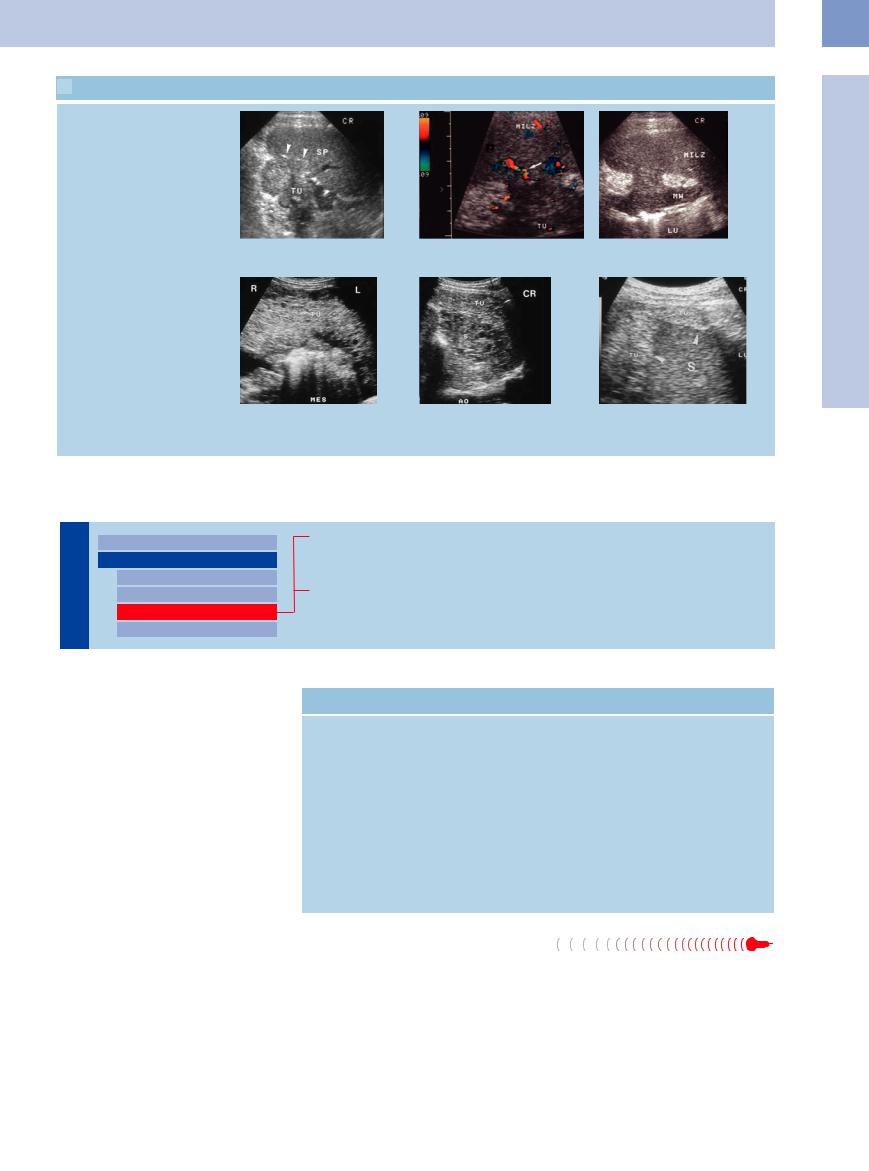
 5.11 Splenic Metastasis in Direct Extension
5.11 Splenic Metastasis in Direct Extension
Direct extension
a Cancer of the pancreatic tail (TU) in- b and c Gastric cancer (TU) invading the spleen (Milz). The blood supply of the tumor vading the spleen (SP) in direct extension. (arrow) can be demonstrated. LU = lumen; MW = stomach wall.
Encasement and infiltration
d–f Mucinous cancer of the colon. |
e Perisplenic and splenic invasion by the |
f Hyperechoic perisplenic invasion by the |
d Tumor (TU) invasion of the greater |
tumor (TU). S = spleen; AO = aorta. |
tumor (TU) in ovarian cancer with peri- |
|
toneal metastasis. S = spleen. |
|
omentum (MES). |
|
|
|
|
Hyperechoic Mass
Spleen |
|
Anechoic Mass |
||
|
|
|
Nonfocal Changes of the Spleen |
|
|
|
|
Focal Changes of the Spleen |
|
|
|
|
|
Hypoechoic Mass |
|
|
|
|
Hyperechoic Mass |
|
|
|
|
|
|
|
|
|
Splenic Calcification |
Hemangioma
Hamartoma
Lymphoma and Myeloproliferative Disorders
Table 5.5 lists the differential diagnosis of hyperechoic splenic masses and their incidence.
Benign solid hyperechoic splenic tumor is usually diagnosed as an incidental finding in abdominal ultrasound studies. It is extremely rare, the most common being hemangiomas and hamartomas.
The main advantage of using ultrasound with other tomographic imaging modalities is the ability to differentiate these entities from primarily malignant splenic tumors, splenic metastases, or infiltrates in malignant lymphoma, and from other hyperechoic intrasplenic masses. Only rarely is ultrasound alone able to do that.
Table 5.5 Differential diagnosis of hyperechoic splenic mass
Frequent |
Rare |
● Hemangioma |
● Lymphoma infiltrate |
● Hamartoma |
● Hemorrhage |
|
● Abscess |
|
● Metastasis |
|
● Hemangiosarcoma |
|
● Extramedullary hematopoiesis |
|
● Gaucher disease |
|
● Niemann–Pick disease |
|
● Peliosis |
|
● Spherocytosis |
|
● Schistosomiasis |
|
● Littoral cell angioma |
Hemangioma 





























Hemangiomas are the most common benign |
mor arises from the sinus epithelium. Heman- |
tumors of the spleen. Their incidence in |
giomas may be solitary or come in multiples |
autopsy studies ranges from 0.03% to 14%. |
and are seen as part of a generalized angioma- |
They are mostly asymptomatic and are diag- |
tosis. Isolated splenic hemangiomatosis is a |
nosed as incidental findings. Their size varies |
rare entity and is usually detected as incidental |
from just a few millimeters to 15 cm. This pre- |
finding after splenectomy. Splenic hemangio- |
dominantly cavernous and rarely capillary tu- |
mas will grow slowly; rupture is the most com- |
mon complication, with an incidence of up to 25%.
Ultrasound appearance. Ultrasound can differentiate between two separate types:
●A primarily smooth, homogeneous, hyperechoic and mostly round lesion ( 5.12a–c)
5.12a–c)
5
Focal Changes of the Spleen
225
5
Spleen
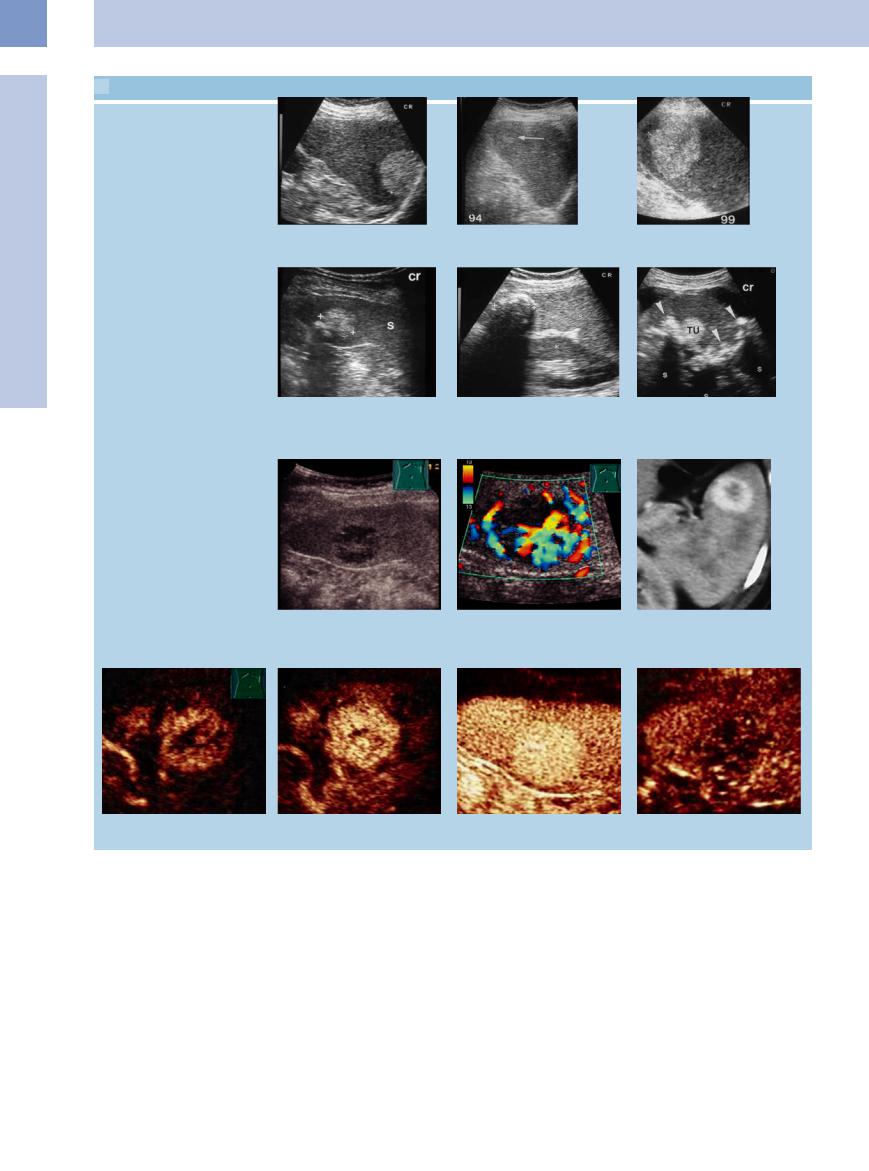
 5.12 Splenic Hemangioma
5.12 Splenic Hemangioma
Typical (hyperechoic) hemangiomas
a Hyperechoic splenic mass compatible |
b and c Growing hyperechoic splenic mass; splenectomy confirmed the diagnosis of a |
with hemangioma. |
cavernous hemangioma. |
Calcified hemangiomas
d Hyperechoic calcified splenic mass corresponding to hemangioma. S = spleen.
e Calcified splenic mass; these phenomena are more frequent in hemangiomas.
f Multiple hyperechoic splenic masses, compatible with hemangioma; in addition, marked intrasplenic calcification. TU = tumor; S = spleen.
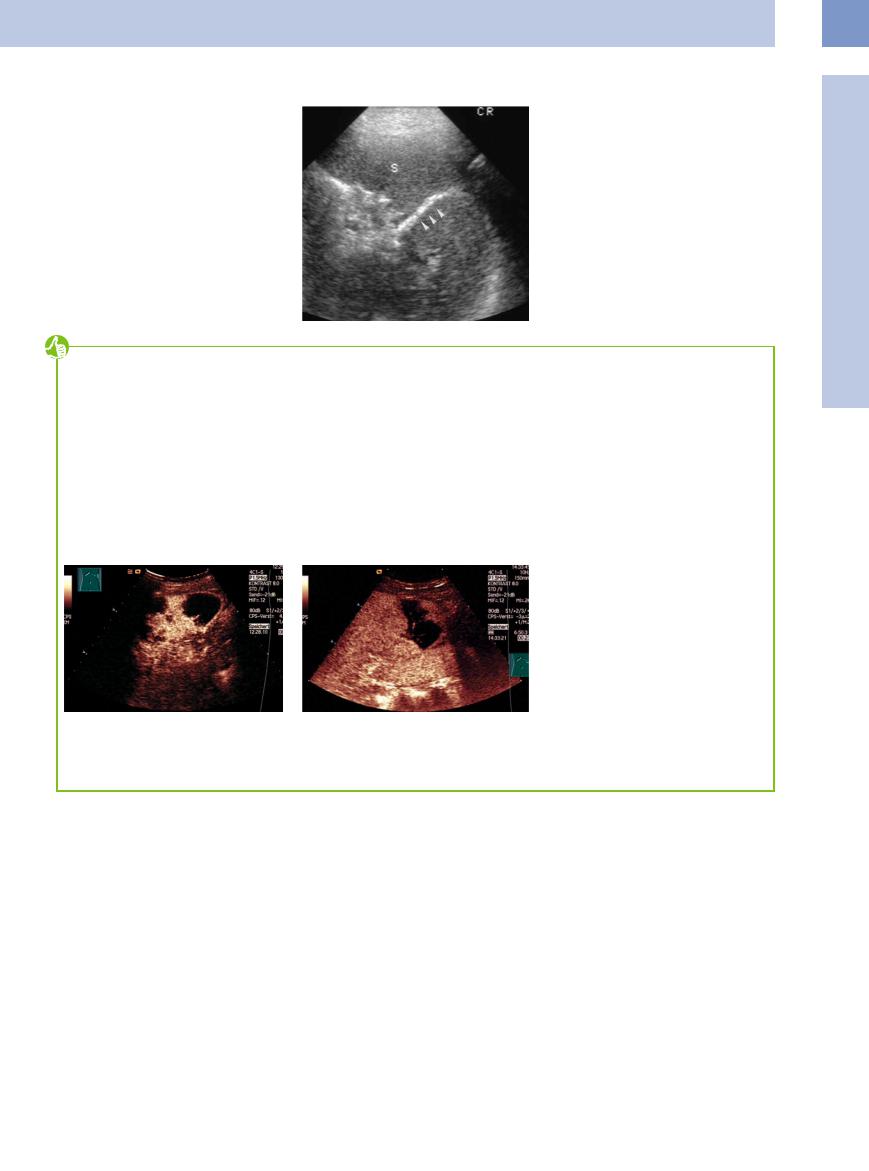
Atypical (hypervascularized) hemangioma
g–i Hypoechoic hypervascularized splenic tumor. |
i A highly vascularized tumor is visible on |
g and h Hypoechoic hypervascularized splenic tumor with enhanced vascularization in |
CT. |
|
|
CDS. |
|
j–m In CEUS the tumor shows a fast and enhanced contrast agent absorption. During the course of the examination the enhancement with contrast agent is slightly reduced in comparison to the surrounding splenic tissue.
●A complex lesion with hypoechoic, partly anechoic, areas and sometimes also calcifi-
cation with posterior shadowing (
5.12 d–f).
In terms of anatomic pathology, this corresponds to a homogeneous vascular pattern or liquid areas (partly hemorrhagic, partly filled with serous fluid).
Cystic hemangioma is a rare variant.
226
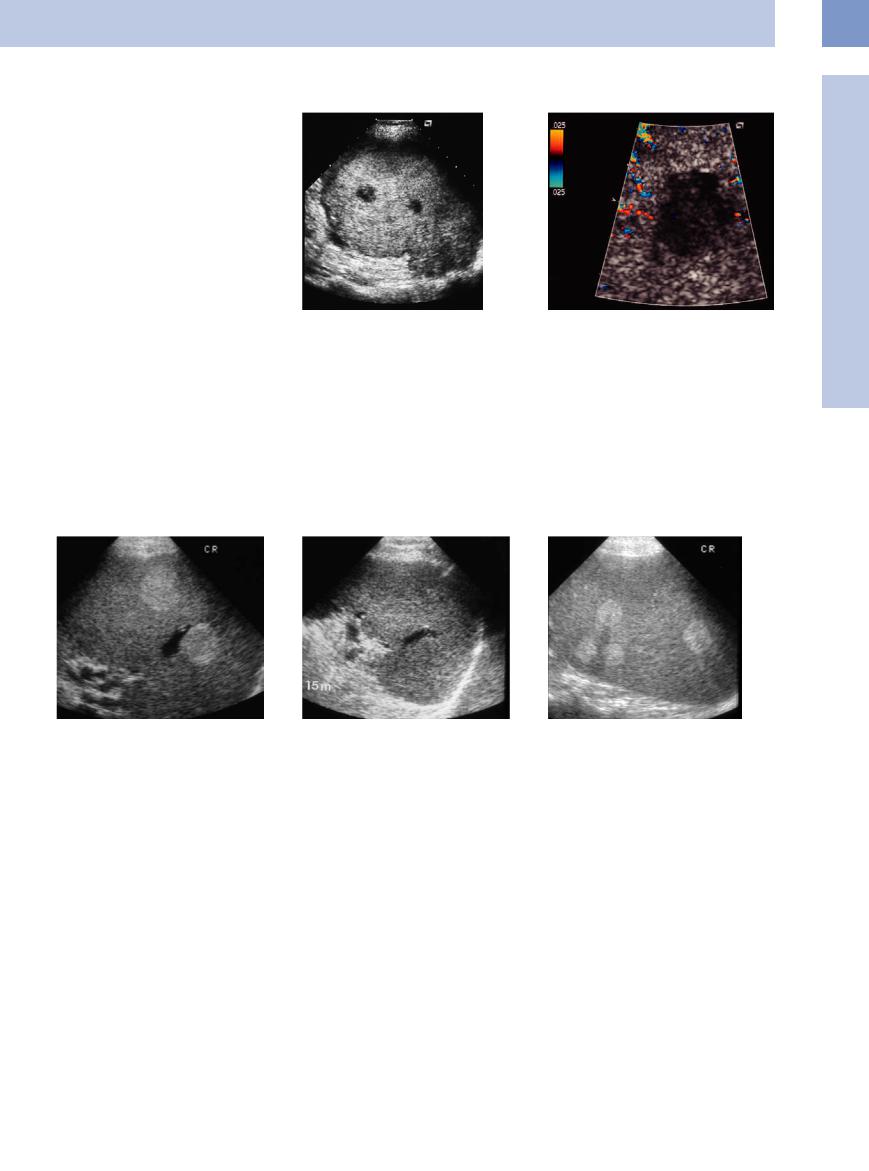
Hamartoma 





















































Hamartomas (splenomas or nodular hypersplenism) are regarded as infrequent congenital neoplasias of the spleen. Most often they will be solitary and are diagnosed as an incidental finding. Anatomic pathology shows them to be made up of normal splenic parenchyma. Their size ranges from several centimeters to more than fist-sized masses, but they rarely cause any symptoms (Fig. 5.31).
Ultrasound appearance. Ultrasound visualizes hamartomas as smoothly delineated tumors weakly contrasted against the splenic parenchyma, with a primarily homogeneous textural echo pattern, good through-transmission of
the ultrasound waves, and mild posterior en- |
Fig. 5.31a and b Large hyperechoic splenic mass with hypoechoic central areas. Splenectomy confirmed a splenoma. |
hancement. Their echogenicity is probably due |
|
to the density of breaks in acoustic impedance |
|
at the walls of their numerous microscopic |
|
fissured cavities. On color-flow Doppler scan- |
|
ning this mass will present as “silent tumor.” |
|
Lymphoma and Myeloproliferative
and Myeloproliferative Disorders
Disorders 



































Hyperechoic lesions may be identified as lym- |
also found in some patients with extramedul- |
phoma infiltrates in just a few cases (<10%) |
lary splenic hematopoiesis in myeloprolifera- |
(Fig. 5.32). They are primarily seen in CLL and |
tive disorders (Fig. 5.33). |
marked splenomegaly. Hyperechoic masses are |
|
5
Focal Changes of the Spleen
Fig. 5.32 Malignant lymphoma.
a Multiple hyperechoic masses. The pathological morphology of this finding remains unclear.
b These masses resolved under chemotherapy, indicating that they might have been lymphoma infiltrates.
Fig. 5.33 Multiple hyperechoic masses in a patient with myeloproliferative disorder. The pathological morphology of this finding remains unclear, possibly corresponding to extramedullary hematopoiesis.
227
5
Spleen
Splenic Calcification
Spleen |
|
Anechoic Mass |
||
|
|
|
Nonfocal Changes of the Spleen |
|
|
|
|
Focal Changes of the Spleen |
|
|
|
|
|
Hypoechoic Mass |
|
|
|
|
Hyperechoic Mass |
|
|
|
|
Splenic Calcification |
|
|
|
|
|
Focal Calcification
Diffuse Calcification
Vascular Calcification
Table 5.6 summarizes the differential diagnosis of splenic calcification.
On ultrasound calcification of the splenic parenchyma presents as solitary or multiple hyperechoic structures, characterized by total or partial posterior shadowing.
Definitive correlation with certain diseases based on the ultrasound findings alone is impossible in most cases. Since they do not require any treatment, the etiology of these mostly incidental findings remains unclear.
Table 5.6 Differential diagnosis of splenic calcification |
|
|
Frequent |
Rare |
|
● Metainfective “starry sky” |
● Splenic calcification |
|
● Calcified cyst |
● Calcified metastasis |
|
● Vascular calcification |
● Calcified hemangioma |
|
|
● Scarring after: |
|
|
– |
abscess |
|
– |
lymphoma |
|
– |
trauma |
|
– |
infarction |
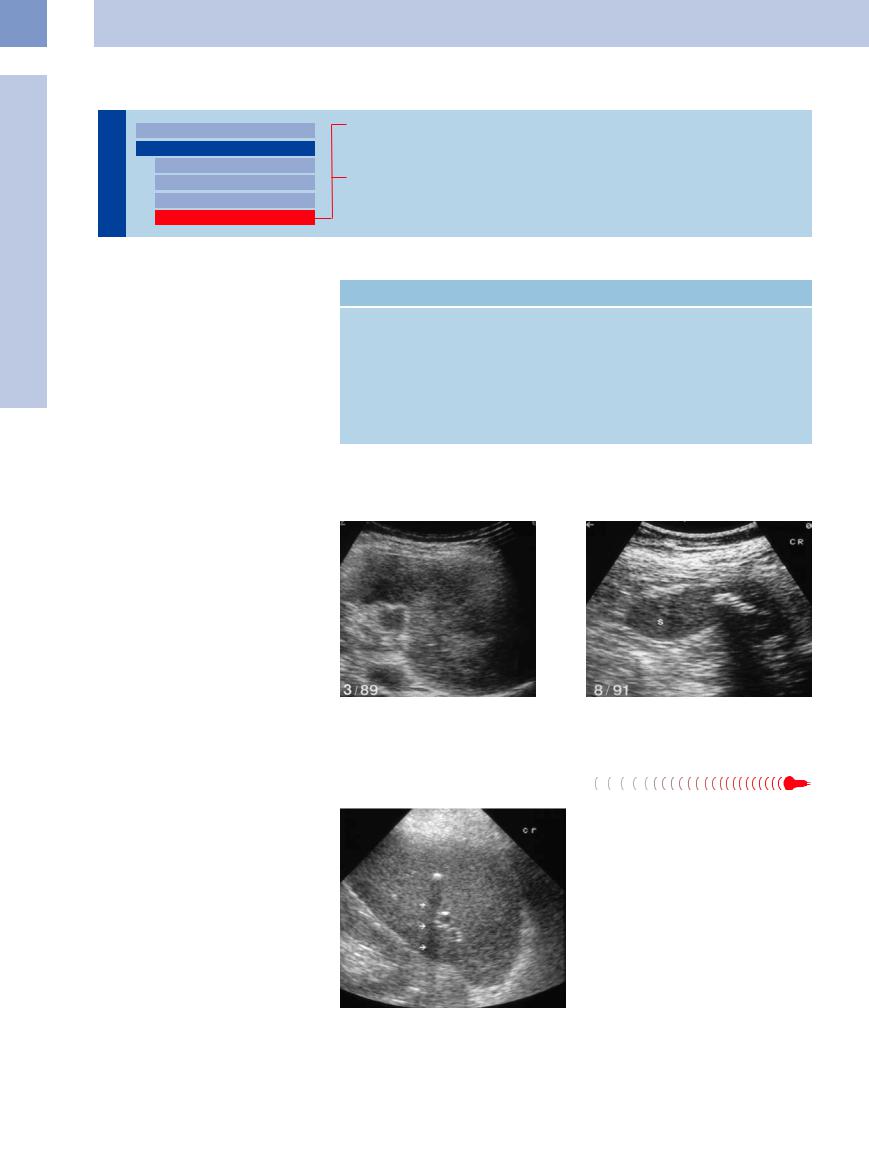
Focal Calcification


















































Focal calcification will be seen as residual scarring after infarction, hematoma, abscess, or invasive lymphoma, or as part of a metabolic disorder (e. g., chronic renal insufficiency) (Fig. 5.34). Calcification of metastases (e. g., medullary thyroid carcinoma) is rare. Splenic cysts may exhibit intramural calcification. In larger hemangiomas, hemorrhage may lead to calcification as well. Sometimes recurrent splenic infarction will leave substantial splenic scarring. Such a spleen will rarely be visualized as just a calcareous crescent, but this would be characteristic in homozygous sickle-cell anemia. Calcified lymph nodes at the splenic hilum will sometimes be seen as sequelae of tuberculosis.
Fig. 5.34 Malignant lymphoma. |
b Focal calcification of the spleen (S) after treatment as |
a Splenic involvement. |
residual scarring. |
Diffuse Calcification


























Diffusely distributed fine reflectors in the spleen will produce a pattern resembling a “starry sky” (Fig. 5.35). Quite often it is visualized as metainfective scarring and may be associated with calcification of other abdominal organs (e. g., in tuberculosis, systemic histoplasmosis, brucellosis, sarcoidosis, aspergillosis, candidiasis, lupus erythematosus, pneumocystis infection, and also amyloidosis).
Fig. 5.35 Multiple small calcifications in an elderly patient with miliary tuberculosis in her youth.
228
Vascular Calcification 
















































This should be differentiated from the vascular calcification of the arteries and veins (phleboliths), which is primarily seen at the splenic hilum but also as diffuse calcification within the parenchyma. The etiology remains unclear. It has been reported in a few patients with general vascular sclerosis, renal insufficiency, and long-standing portal hypertension (Fig. 5.36).
Tips, tricks, and pitfalls
In contrast to other organs the size of the spleen can be well estimated and measured. The longitudinal diameter may be sufficient in most cases; the thickness may be added in special cases. Corresponding to the conventional handling, the spleen should be depicted in a scan direction that shows the lower pole on the right image side.
The examination of the spleen is carried out in a supine position, also in a right decubitus position. A deep inspiration is not very helpful because of
Fig. 5.37 CEUS in a patient after blunt abdominal trauma depicts nonenhancing regions corresponding to hematomas or lesions within the spleen.
References
[1]Görg C. Milzdiagnostik mit Ultraschallkontrastmitteln. Konstanz: Schnetztor-Verlag GmbH, 2006
[2]Görg C, Bert T. Contrast enhanced sonography of focal splenic lesions with a second-gener- ation contrast agent. Ultraschall Med 2005;26(6):470–477
the overlapping of the phrenicocostal sinus blocking the sight of the spleen. A high intercostal scan direction is the best access. To inspect the convexity near the thoracic wall it is recommendable to use a 5 MHz transducer.
Cysts in the splenic–renal angle may derive from the spleen, the kidney or as pseudocysts from the pancreatic tail (additional scan from a transverse upper abdominal direction).
Solid masses within the spleen may predominantly signify an organ manifestation of a malig-
Fig. 5.38 In a patient with CLL and left flank pain, CEUS demonstrates a nonenhancing area at the lower pole as a sure sign of a splenic infarction. Some of these infarctions are nonapparent.
[3]Görg C, Schwerk WB. Milzsonographie. In: Braun B, Günther R, Schwerk WB (eds.). Ul- traschalldiagnostik—Lehrbuch und Atlas. Landsberg: ECO med, 2000
[4]Görg C. The forgotten organ: contrast enhanced sonography of the spleen. Eur J Radiol 2007;64(2):189–201
[5]Falk P. Maligne Lymphome in der Milz. Stuttgart: Fischer, 1991
Fig. 5.36 Vascular calcification in chronic renal insufficiency. S = spleen.
nant lymphoma, and require a complete investigation of all abdominal lymph node stations; splenic metastases are rare.
The spleen is involved in the portal circulation; therefore the investigation of the spleen should also include the hepatobiliary system especially in case of an enlarged spleen:
●searching for lymph nodes
●inspection of the portal system and the liver
Special consideration of the spleen is demanded in the early diagnosis of abdominal trauma (Fig. 5.37). An enlarged organ should be followed up by monitoring after 6, 12 and 18 h; so should free fluid detected within the abdomen.
Current studies show that liquid hematomas and small intraparenchymal hemorrhages, not detectable in other imaging procedures, are very well seen when contrast agents (CEUS) are used. CEUS may become the most sensitive procedure especially in trauma-related emergency admissions.
In the detection of disturbed circulation of the spleen CEUS is also a most sensitive procedure (Fig. 5.38). Very small infarctions are detectable, which is significant for prognosis and prevention.
[6]Neiman RS, Orazi A. Disorders of the spleen. 2nd ed. Philadelphia: W.B. Saunders, 1999
[7]Görg C, Görg K, Bert T, Barth P. Colour Doppler ultrasound patterns and clinical follow-up of incidentally found hypoechoic, vascular tumours of the spleen: evidence for a benign tumour. Br J Radiol 2006;79:319–325
5
Focal Changes of the Spleen
229

