
- •Contents
- •Preface
- •Contributors
- •1 Vessels
- •1.1 Aorta, Vena Cava, and Peripheral Vessels
- •Aorta, Arteries
- •Anomalies and Variant Positions
- •Dilatation
- •Stenosis
- •Wall Thickening
- •Intraluminal Mass
- •Perivascular Mass
- •Vena Cava, Veins
- •Anomalies
- •Dilatation
- •Intraluminal Mass
- •Compression, Infiltration
- •1.2 Portal Vein and Its Tributaries
- •Enlarged Lumen Diameter
- •Portal Hypertension
- •Intraluminal Mass
- •Thrombosis
- •Tumor
- •2 Liver
- •Enlarged Liver
- •Small Liver
- •Homogeneous Hypoechoic Texture
- •Homogeneous Hyperechoic Texture
- •Regionally Inhomogeneous Texture
- •Diffuse Inhomogeneous Texture
- •Anechoic Masses
- •Hypoechoic Masses
- •Isoechoic Masses
- •Hyperechoic Masses
- •Echogenic Masses
- •Irregular Masses
- •Differential Diagnosis of Focal Lesions
- •Diagnostic Methods
- •Suspected Diagnosis
- •3 Biliary Tree and Gallbladder
- •3.1 Biliary Tree
- •Thickening of the Bile Duct Wall
- •Localized and Diffuse
- •Bile Duct Rarefaction
- •Localized and Diffuse
- •Bile Duct Dilatation and Intraductal Pressure
- •Intrahepatic
- •Hilar and Prepancreatic
- •Intrapancreatic
- •Papillary
- •Abnormal Intraluminal Bile Duct Findings
- •Foreign Body
- •The Seven Most Important Questions
- •3.2 Gallbladder
- •Changes in Size
- •Large Gallbladder
- •Small/Missing Gallbladder
- •Wall Changes
- •General Hypoechogenicity
- •General Hyperechogenicity
- •General Tumor
- •Focal Tumor
- •Intraluminal Changes
- •Hyperechoic
- •Hypoechoic
- •Nonvisualized Gallbladder
- •Missing Gallbladder
- •Obscured Gallbladder
- •4 Pancreas
- •Diffuse Pancreatic Change
- •Large Pancreas
- •Small Pancreas
- •Hypoechoic Texture
- •Hyperechoic Texture
- •Focal Changes
- •Anechoic Lesion
- •Hypoechoic Lesion
- •Isoechoic Lesion
- •Hyperechoic Lesion
- •Irregular (Complex Structured) Lesion
- •Dilatation of the Pancreatic Duct
- •Marginal/Mild Dilatation
- •Marked Dilatation
- •5 Spleen
- •Nonfocal Changes of the Spleen
- •Diffuse Parenchymal Changes
- •Large Spleen
- •Small Spleen
- •Focal Changes of the Spleen
- •Anechoic Mass
- •Hypoechoic Mass
- •Hyperechoic Mass
- •Splenic Calcification
- •6 Lymph Nodes
- •Peripheral Lymph Nodes
- •Head/Neck
- •Extremities (Axilla, Groin)
- •Abdominal Lymph Nodes
- •Porta Hepatis
- •Splenic Hilum
- •Mesentery (Celiac, Upper and Lower Mesenteric Station)
- •Stomach
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •Small/Large Intestine
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •8 Peritoneal Cavity
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Wall Structures
- •Smooth Margin
- •Irregular Margin
- •Intragastric Processes
- •Intraintestinal Processes
- •9 Kidneys
- •Anomalies, Malformations
- •Aplasia, Hypoplasia
- •Cystic Malformation
- •Anomalies of Number, Position, or Rotation
- •Fusion Anomaly
- •Anomalies of the Renal Calices
- •Vascular Anomaly
- •Diffuse Changes
- •Large Kidneys
- •Small Kidneys
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Irregular Structure
- •Circumscribed Changes
- •Anechoic Structure
- •Hypoechoic or Isoechoic Structure
- •Complex Structure
- •Hyperechoic Structure
- •10 Adrenal Glands
- •Enlargement
- •Anechoic Structure
- •Hypoechoic Structure
- •Complex Echo Structure
- •Hyperechoic Structure
- •11 Urinary Tract
- •Malformations
- •Duplication Anomalies
- •Dilatations and Stenoses
- •Dilated Renal Pelvis and Ureter
- •Anechoic
- •Hypoechoic
- •Hypoechoic
- •Hyperechoic
- •Large Bladder
- •Small Bladder
- •Altered Bladder Shape
- •Intracavitary Mass
- •Hypoechoic
- •Hyperechoic
- •Echogenic
- •Wall Changes
- •Diffuse Wall Thickening
- •Circumscribed Wall Thickening
- •Concavities and Convexities
- •12.1 The Prostate
- •Enlarged Prostate
- •Regular
- •Irregular
- •Small Prostate
- •Regular
- •Echogenic
- •Circumscribed Lesion
- •Anechoic
- •Hypoechoic
- •Echogenic
- •12.2 Seminal Vesicles
- •Diffuse Change
- •Hypoechoic
- •Circumscribed Change
- •Anechoic
- •Echogenic
- •Irregular
- •12.3 Testis, Epididymis
- •Diffuse Change
- •Enlargement
- •Decreased Size
- •Circumscribed Lesion
- •Anechoic or Hypoechoic
- •Irregular/Echogenic
- •Epididymal Lesion
- •Anechoic
- •Hypoechoic
- •Intrascrotal Mass
- •Anechoic or Hypoechoic
- •Echogenic
- •13 Female Genital Tract
- •Masses
- •Abnormalities of Size or Shape
- •Uterus
- •Abnormalities of Size or Shape
- •Myometrial Changes
- •Intracavitary Changes
- •Endometrial Changes
- •Fallopian Tubes
- •Hypoechoic Mass
- •Anechoic Cystic Mass
- •Solid Echogenic or Nonhomogeneous Mass
- •14 Thyroid Gland
- •Diffuse Changes
- •Enlarged Thyroid Gland
- •Small Thyroid Gland
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Circumscribed Changes
- •Anechoic
- •Hypoechoic
- •Isoechoic
- •Hyperechoic
- •Irregular
- •Differential Diagnosis of Hyperthyroidism
- •Types of Autonomy
- •15 Pleura and Chest Wall
- •Chest Wall
- •Masses
- •Parietal Pleura
- •Nodular Masses
- •Diffuse Pleural Thickening
- •Pleural Effusion
- •Anechoic Effusion
- •Echogenic Effusion
- •Complex Effusion
- •16 Lung
- •Masses
- •Anechoic Masses
- •Hypoechoic Masses
- •Complex Masses
- •Index
7
Gastrointestinal Tract
Extended Wall Changes
Tract |
|
|
|
|
|
Stomach |
|
Enteritis |
|
|
|
|
|
|
|||||
|
|
|
|
|
Small/Large Intestine |
|
Celiac Disease (Sprue) |
||
|
|
|
|||||||
|
|||||||||
Gastrointestinal |
|
|
Focal Wall Changes |
|
Crohn Disease |
||||
|
|
Extended Wall Changes |
|
||||||
|
|
|
Ulcerative Colitis |
||||||
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
Dilated Lumen |
|
|
|
|
|
|
|
|
|
|
Amyloidosis |
|
|
|
|
|
|
|
|
Narrowed Lumen |
|
|
|
|
|
|
|
|
|
|
Pseudomembranous Enterocolitis |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Ischemia |
|
|
|
|
|
|
|
|
|
Hypertrophy |
|
|
|
|
|
|
|
|
|
Tumor |
|
|
|
|
|
|
|
|
|
Lymphoma |
Extended changes in the jejunal, ileal, and co- |
ischemic, invasive, and functional causes are |
||||||||
lonic wall are primarily due to acute infection |
much less common. Differential diagnosis has |
||||||||
or chronic inflammation, while toxic, allergic, |
to rule out extended malignant wall changes. |
||||||||
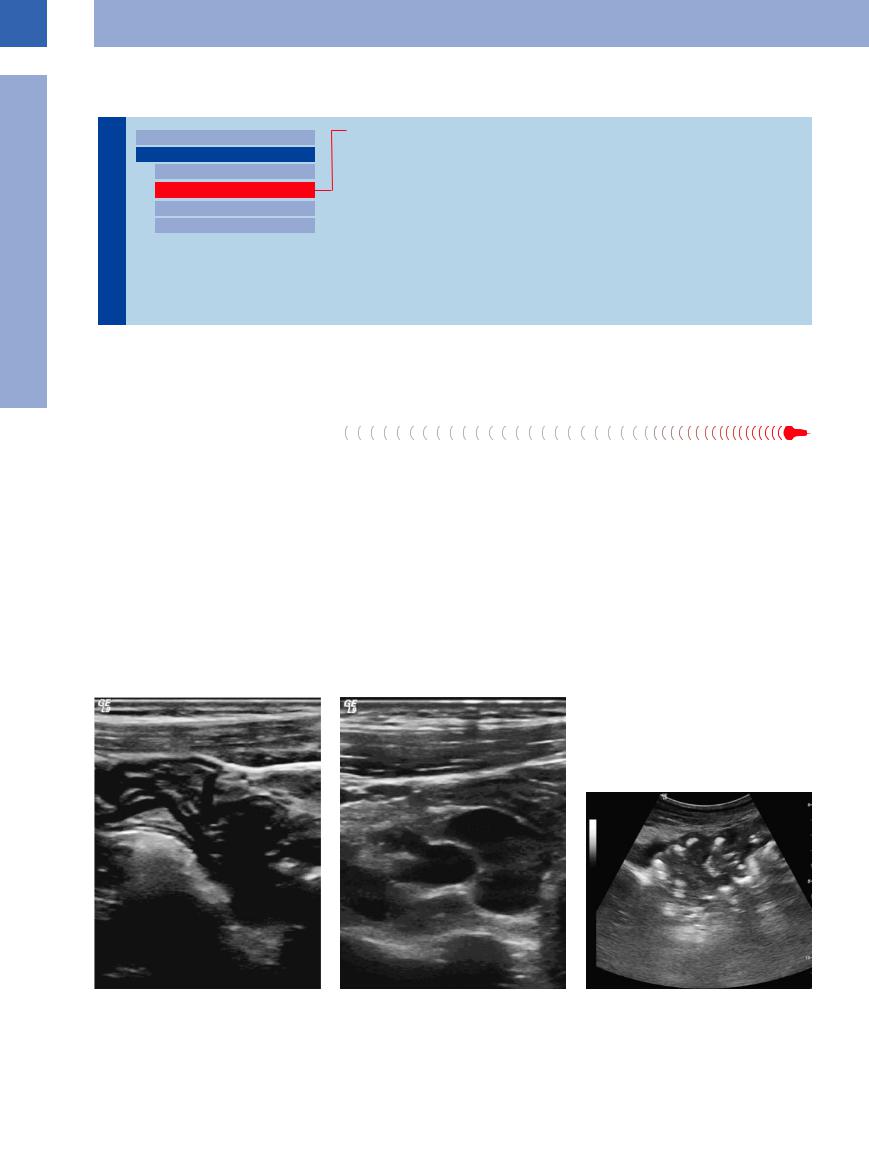
Enteritis 













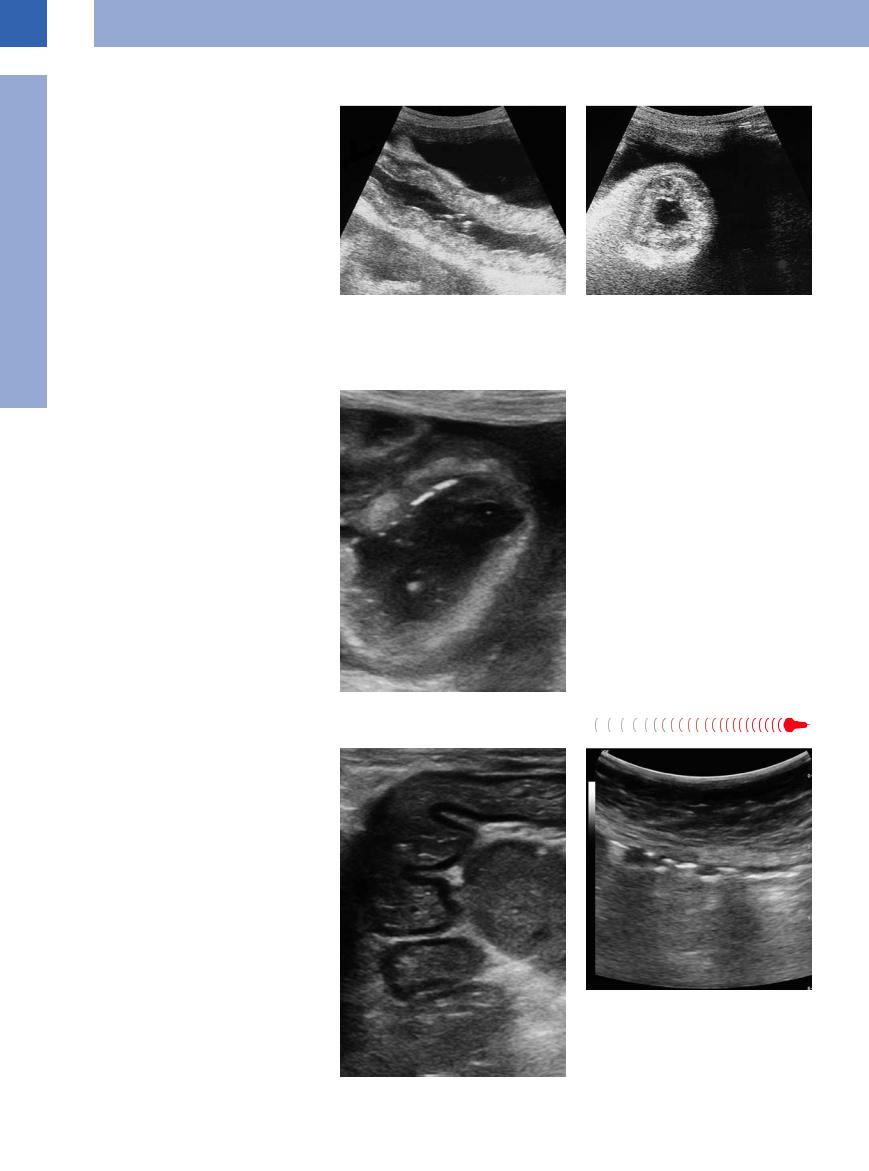
The continuous, extended edematous thickening of the mucosa in enteritis is seen primarily in the ileum but also in the jejunum and colon. There is markedly accentuated wall layering, with the mucosa and/or submucosa being particularly thick, resulting in a narrowed lumen of the bowel. In acute enteritis the intestinal lumen always contains some fluid, even in the fasting state, and this finding is present even before the clinical symptom of diarrhea (Figs. 7.55, 7.56, 7.57, 7.58).
In the small intestine the circular folds may be pronounced, while in the colon the haustra and folds may intertwine in gyrose fashion. One characteristic sign in the small bowel is
vigorous peristalsis that propagates in an orderly antegrade way and does not exhibit any tendency to pendulate. In acute enteritis the colon, too, will demonstrate peristaltic activity. Color flow Doppler scanning may visualize inflammatory hypervascularity in the intestinal wall that, at least in its initial stages, seems to correlate with the severity of the inflammation. Outside the bowel, ascites may be present, signifying the inflammatory peritoneal reaction, as well as enlarged mesenteric lymphadenopathy.
In severe necrotizing inflammation the peristaltic activity and the inflammatory hypervascularity will subside again. There will be diffuse
tenderness along the diseased bowel segment, and the intestinal wall will be characterized by indistinct wall layering; the appearance of gas bubbles has to be regarded as a particularly ominous sign. These gas bubbles will be carried along the venous system of the mesentery and are the cause of portovenous gas embolism in the liver.
Fig. 7.55 Enteritis. |
b Mesenteric lymph node enlargement. |
Fig. 7.56 Non-specific enteritis. |
a Enteritic small bowel. |
|
|
282
7
Small/Large Intestine
Fig. 7.57 Enteritis with demonstration of thickened wall, small amount of free peritoneal fluid collection (sympathic peritoneal irritation), inflammatory thickening of the lateral peritoneum.
Fig. 7.58 Enteritis in the case of a collagenosis/vasculitis. |
b Severe hypervascularization. |
a Edematous rigid lumen, accentuated wall layering. |
|
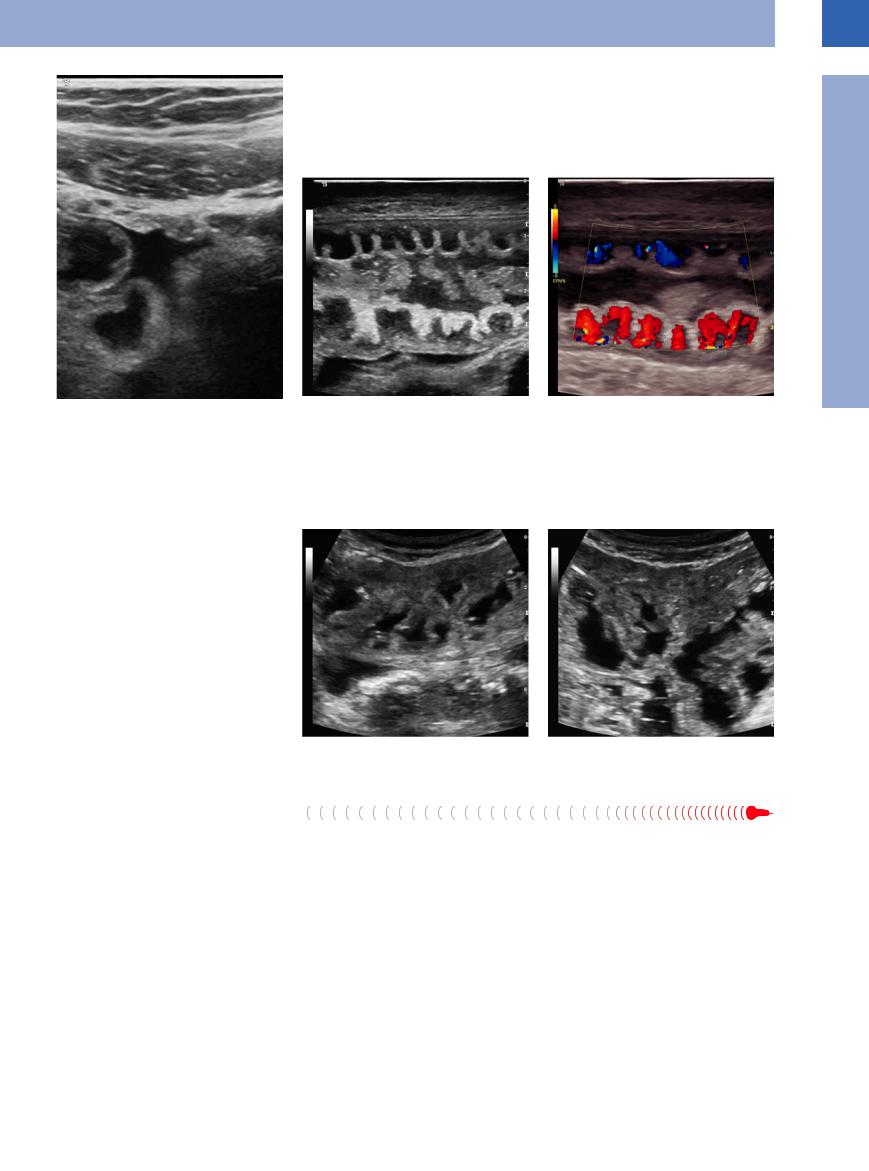
Celiac Disease  (Sprue)
(Sprue)
















































Being a special case of enteric reaction, celiac disease is characterized by edema with hypoechoic thickening of the intestinal wall and marked distension of the fluid-filled lumen. The hyperperistaltic loops of the small bowel twine around each other, giving rise to the term “tumbler phenomenon” (Fig. 7.59).
Fig. 7.59 Celiac disease (sprue).
a Longitudinal scan in the midabdomen.
Crohn Disease










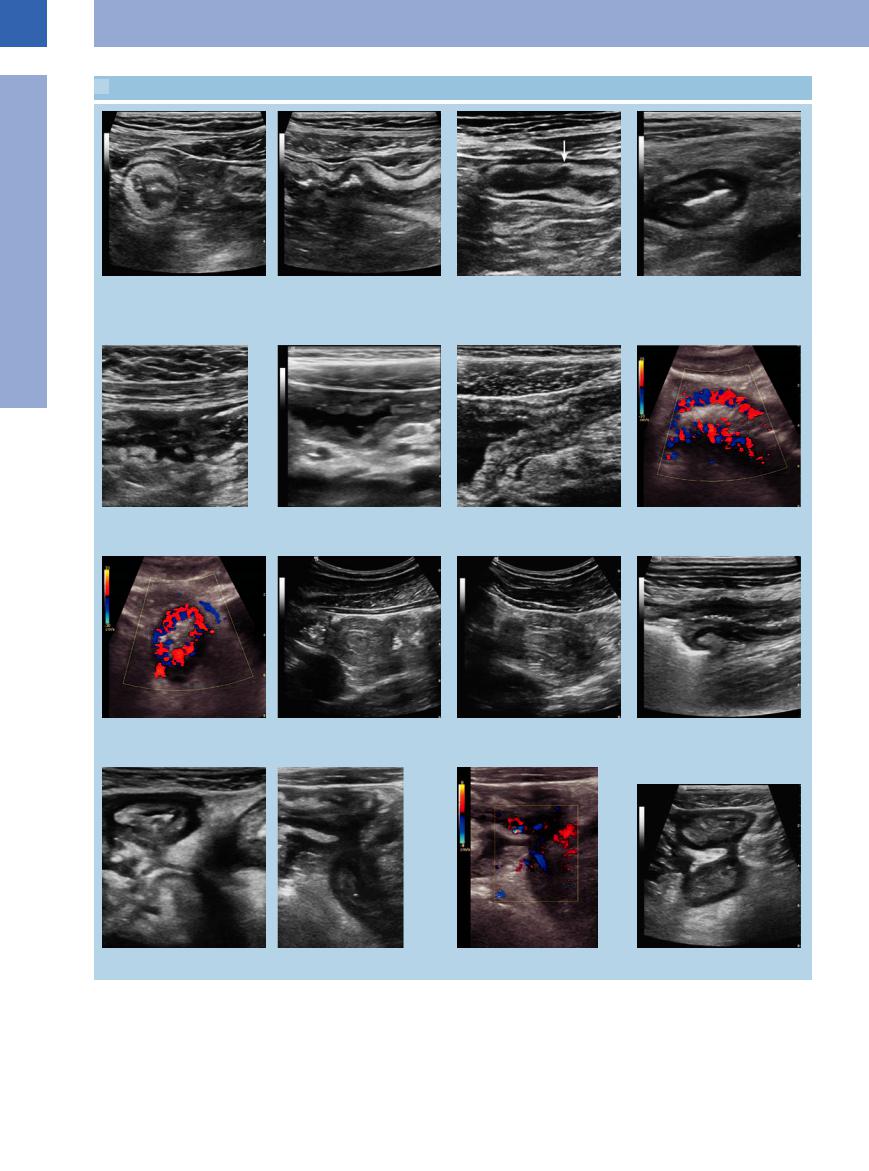
Crohn disease is a chronic inflammatory bowel disease occurring anywhere in the GI tract, with discontinuous extended involvement of individual bowel segments, the primary location being the terminal ileum and colon. In addition to the segmental pattern of the typical pathological changes demonstrated by ultrasound, the type and severity of the most frequent transmural inflammation and its complications, with their wildly mixed and constantly alternating pattern, are characteristic of Crohn disease (Fig. 7.60,  7.3).
7.3).
Types of wall change. In Crohn disease various types of change in the intestinal wall can be seen, depending on the transmural severity of the inflammation.
●On one hand, the layering of the wall becomes more pronounced and thickened, the intestinal lumen is narrowed, and, because of the impaired peristalsis (inflammatory rigidity), the segment involved may act as functional stenosis.
●On the other hand, the intestinal wall may display a complete loss of normal layering, and diffuse and irregular hypoechoic thick-
b Transverse scan in the midabdomen.
ening or hyperechoic widening, which may also result in aperistaltic narrowing of the lumen.
There is a gradual transition from one type of wall change to the other.
Complications. Complications of Crohn disease can be expected to arise from the functional and/or organic stenosis (colicky pain upstream of the stenotic segment, signs of mechanical ileus in the proximal bowel loops) as well as the local inflammation. Apart from local
283
7
Gastrointestinal Tract
 7.3 Crohn Disease
7.3 Crohn Disease
a and b Crohn disease, accentuated wall of the terminal ileum. |
c Accentuated layering of the intestinal |
d Terminal ileitis (Crohn disease) with a |
|
wall in the terminal ileum in Crohn disease |
hazy, thickened wall (pathologic gut |
|
and prevailing thickening of the submu- |
sign), starting loss of layering and marked |
|
cous membrane; demonstration of an ul- |
panniculitis. Lymph node enlargement. |
|
cer (arrow). |
|
e Crohn disease; distinct destruction of the wall layering of the terminal ileum.
f Cobblestone relief of the terminal ileum in Crohn disease; posterior hyperechoic mesenteritis and enlarged lymph nodes.
g Crohn disease with inflammatory stenosis (cobblestone relief) of the lumen and dilatation of the preceding bowel loop.
h and i Terminal ileitis with inflammatory hypervascularity.
h Longitudinal scan.
i Transverse scan. |
j and k Intussusception, short segment in Crohn disease. |
m Crohn disease with interenteric fistula. n and o Conglomerate in Crohn disease.
l Ileocolic junction in advanced Crohn disease: stenosis in the region of the terminal ileum.
p Crohn disease with interenteric fistula.
284
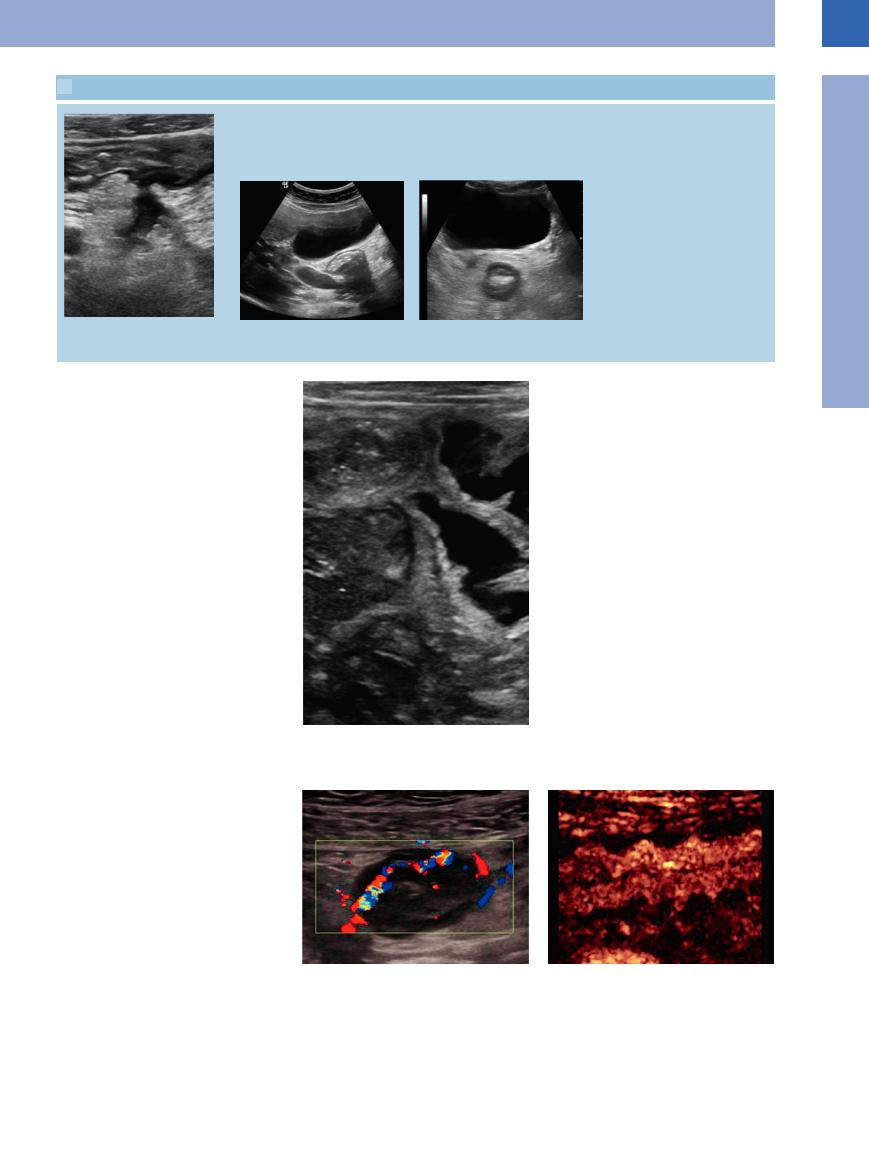
 7.3 Crohn Disease (Continued)
7.3 Crohn Disease (Continued)
q Fistula in Crohn disease. |
r Duodenal Crohn disease: pathologic ac- |
s Crohn colitis: pathological target sign of |
|
centuated target sign and distinct panni- |
the rectum posterior to the bladder with |
|
culitis. |
distinct panniculitis. |
tenderness, color flow Doppler scanning will |
Fig. 7.60 Enteritis in Crohn disease. |
|
|
reveal inflammatory hypervascularity in the |
|
intestinal wall and its vicinity. There will be |
|
hyperechoic panniculitis and inflammatory re- |
|
action of the greater omentum (hyperechoic |
|
halo) as well as complications such as forma- |
|
tion of abscesses, fistulas, and conglomerates |
|
containing several loops of bowel. |
|
Sensitivity and specificity are reported to be |
|
90.3% and 95% respectively in the diagnosis of |
|
inflammatory bowel disease,1,2 100% and 91% |
|
in detecting strictures, and 87% and 90% in the |
|
diagnosis of fistulas, with a bowel wall thicken- |
|
ing of at least 3 mm.3 Power Doppler has a high |
|
accuracy in the detection of disease acitivity.4 |
|
7
Small/Large Intestine
Ulcerative Colitis 


















































Ulcerative colitis is a continuous chronic inflammation of the distal left or even the entire colon. It manifests as an extended homogeneous slight thickening of the colonic wall with clearly identifiable wall layers and a tight lumen. There is no peristaltic activity or clear-cut hypervascularity or concurrent reaction of the adjacent tissue. On physical examination, extended diffuse tenderness may be triggered along the pathological gut signature (Fig. 7.61).
It seems possible to discriminate severe and moderate extent and activity with a specificity, sensitivity, and diagnostic accuracy of 96%, 90.3%, and 92.9% respectively.5
Fig. 7.61 Ulcerative colitis. |
b Florid ulcerative colitis of the descending colon (CEUS). |
a Florid ulcerative colitis of the descending colon (CDS). |
|
285
7
Gastrointestinal Tract
Amyloidosis 





















































Amyloid deposits in the wall of the bowel are a rare finding: they are seen as hyperechoic, homogeneous thickening of the entire intestinal wall with filiform stenosis of the lumen (Fig. 7.62), and there is no peristalsis.
Fig. 7.62 Amyloidosis. |
b Amyloidosis. Filiform narrowing of the lumen. |
a Hyperechoic homogeneous thickening of the entire |
|
intestinal wall. |
|
Pseudomembranous Enterocolitis 









































Antibiotic-associated colitis/pseudomembra- |
Fig. 7.63 Pseudomembranous colitis. |
|
|
nous colitis often affects the entire colon with |
|
emphasis on the distal part. This diagnosis can |
|
be suspected without the proof of clostridium |
|
toxin if the history allows it and if there is a |
|
marked hypoechoic hypervascular swelling of |
|
the intestinal wall, which can often be found in |
|
this type of colitis (Fig. 7.63). |
|
Ischemia
































In acute ischemia there will be edematous swelling of the bowel wall and, while the layering of the wall initially persists, eventually it will end in hypoechoic thickening and narrowing of the lumen. The lack of vascularization in color Doppler ultrasound (especially since the diseases to be considered in the differential diagnosis tend to be hypervascular) raises the suspicion of a circulation disorder. Color Doppler ultrasound is not sensitive enough to detect ischemia directly. With CEUS the lack of vascularization can be seen reliably (despite earlier findings) and the extent of the ischemia may even be delineated. Further studies with CEUS in ischemia are needed (Fig. 7.64, Fig. 7.65).
Fig. 7.65 Scan shows gas in the bowel loop wall in severe enterocolitis.
Fig. 7.64 Superinfected ischemic colitis: hypoechoic swelling; almost no evidence of vascularity.
286
