
- •Contents
- •Preface
- •Contributors
- •1 Vessels
- •1.1 Aorta, Vena Cava, and Peripheral Vessels
- •Aorta, Arteries
- •Anomalies and Variant Positions
- •Dilatation
- •Stenosis
- •Wall Thickening
- •Intraluminal Mass
- •Perivascular Mass
- •Vena Cava, Veins
- •Anomalies
- •Dilatation
- •Intraluminal Mass
- •Compression, Infiltration
- •1.2 Portal Vein and Its Tributaries
- •Enlarged Lumen Diameter
- •Portal Hypertension
- •Intraluminal Mass
- •Thrombosis
- •Tumor
- •2 Liver
- •Enlarged Liver
- •Small Liver
- •Homogeneous Hypoechoic Texture
- •Homogeneous Hyperechoic Texture
- •Regionally Inhomogeneous Texture
- •Diffuse Inhomogeneous Texture
- •Anechoic Masses
- •Hypoechoic Masses
- •Isoechoic Masses
- •Hyperechoic Masses
- •Echogenic Masses
- •Irregular Masses
- •Differential Diagnosis of Focal Lesions
- •Diagnostic Methods
- •Suspected Diagnosis
- •3 Biliary Tree and Gallbladder
- •3.1 Biliary Tree
- •Thickening of the Bile Duct Wall
- •Localized and Diffuse
- •Bile Duct Rarefaction
- •Localized and Diffuse
- •Bile Duct Dilatation and Intraductal Pressure
- •Intrahepatic
- •Hilar and Prepancreatic
- •Intrapancreatic
- •Papillary
- •Abnormal Intraluminal Bile Duct Findings
- •Foreign Body
- •The Seven Most Important Questions
- •3.2 Gallbladder
- •Changes in Size
- •Large Gallbladder
- •Small/Missing Gallbladder
- •Wall Changes
- •General Hypoechogenicity
- •General Hyperechogenicity
- •General Tumor
- •Focal Tumor
- •Intraluminal Changes
- •Hyperechoic
- •Hypoechoic
- •Nonvisualized Gallbladder
- •Missing Gallbladder
- •Obscured Gallbladder
- •4 Pancreas
- •Diffuse Pancreatic Change
- •Large Pancreas
- •Small Pancreas
- •Hypoechoic Texture
- •Hyperechoic Texture
- •Focal Changes
- •Anechoic Lesion
- •Hypoechoic Lesion
- •Isoechoic Lesion
- •Hyperechoic Lesion
- •Irregular (Complex Structured) Lesion
- •Dilatation of the Pancreatic Duct
- •Marginal/Mild Dilatation
- •Marked Dilatation
- •5 Spleen
- •Nonfocal Changes of the Spleen
- •Diffuse Parenchymal Changes
- •Large Spleen
- •Small Spleen
- •Focal Changes of the Spleen
- •Anechoic Mass
- •Hypoechoic Mass
- •Hyperechoic Mass
- •Splenic Calcification
- •6 Lymph Nodes
- •Peripheral Lymph Nodes
- •Head/Neck
- •Extremities (Axilla, Groin)
- •Abdominal Lymph Nodes
- •Porta Hepatis
- •Splenic Hilum
- •Mesentery (Celiac, Upper and Lower Mesenteric Station)
- •Stomach
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •Small/Large Intestine
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •8 Peritoneal Cavity
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Wall Structures
- •Smooth Margin
- •Irregular Margin
- •Intragastric Processes
- •Intraintestinal Processes
- •9 Kidneys
- •Anomalies, Malformations
- •Aplasia, Hypoplasia
- •Cystic Malformation
- •Anomalies of Number, Position, or Rotation
- •Fusion Anomaly
- •Anomalies of the Renal Calices
- •Vascular Anomaly
- •Diffuse Changes
- •Large Kidneys
- •Small Kidneys
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Irregular Structure
- •Circumscribed Changes
- •Anechoic Structure
- •Hypoechoic or Isoechoic Structure
- •Complex Structure
- •Hyperechoic Structure
- •10 Adrenal Glands
- •Enlargement
- •Anechoic Structure
- •Hypoechoic Structure
- •Complex Echo Structure
- •Hyperechoic Structure
- •11 Urinary Tract
- •Malformations
- •Duplication Anomalies
- •Dilatations and Stenoses
- •Dilated Renal Pelvis and Ureter
- •Anechoic
- •Hypoechoic
- •Hypoechoic
- •Hyperechoic
- •Large Bladder
- •Small Bladder
- •Altered Bladder Shape
- •Intracavitary Mass
- •Hypoechoic
- •Hyperechoic
- •Echogenic
- •Wall Changes
- •Diffuse Wall Thickening
- •Circumscribed Wall Thickening
- •Concavities and Convexities
- •12.1 The Prostate
- •Enlarged Prostate
- •Regular
- •Irregular
- •Small Prostate
- •Regular
- •Echogenic
- •Circumscribed Lesion
- •Anechoic
- •Hypoechoic
- •Echogenic
- •12.2 Seminal Vesicles
- •Diffuse Change
- •Hypoechoic
- •Circumscribed Change
- •Anechoic
- •Echogenic
- •Irregular
- •12.3 Testis, Epididymis
- •Diffuse Change
- •Enlargement
- •Decreased Size
- •Circumscribed Lesion
- •Anechoic or Hypoechoic
- •Irregular/Echogenic
- •Epididymal Lesion
- •Anechoic
- •Hypoechoic
- •Intrascrotal Mass
- •Anechoic or Hypoechoic
- •Echogenic
- •13 Female Genital Tract
- •Masses
- •Abnormalities of Size or Shape
- •Uterus
- •Abnormalities of Size or Shape
- •Myometrial Changes
- •Intracavitary Changes
- •Endometrial Changes
- •Fallopian Tubes
- •Hypoechoic Mass
- •Anechoic Cystic Mass
- •Solid Echogenic or Nonhomogeneous Mass
- •14 Thyroid Gland
- •Diffuse Changes
- •Enlarged Thyroid Gland
- •Small Thyroid Gland
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Circumscribed Changes
- •Anechoic
- •Hypoechoic
- •Isoechoic
- •Hyperechoic
- •Irregular
- •Differential Diagnosis of Hyperthyroidism
- •Types of Autonomy
- •15 Pleura and Chest Wall
- •Chest Wall
- •Masses
- •Parietal Pleura
- •Nodular Masses
- •Diffuse Pleural Thickening
- •Pleural Effusion
- •Anechoic Effusion
- •Echogenic Effusion
- •Complex Effusion
- •16 Lung
- •Masses
- •Anechoic Masses
- •Hypoechoic Masses
- •Complex Masses
- •Index
15
Pleural Effusion
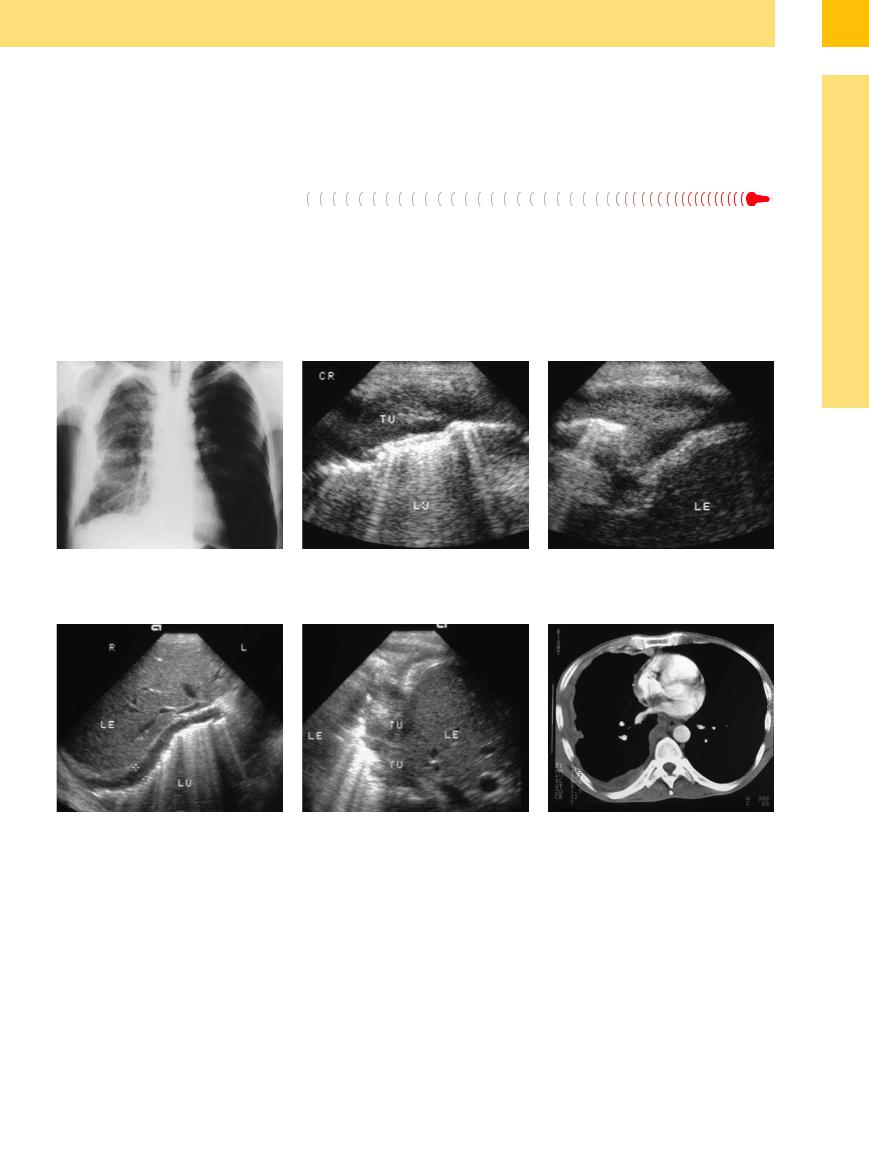
Fig. 15.14 A 40-year-old man with malignant mesothelioma.
a Chest radiograph shows encasement of the right lung.
b and c Right lateral intercostal scan shows extensive hypoechoic tumor encasement (TU) of the lung (LU). L = liver.
d and e Subcostal transhepatic scan shows diffuse tumor spread. Scattered nodular lesions (TU) are also demonstrated |
f CT: pleural tumor. |
in the lateral scan (e). |
|
■ Pleural Effusion
Pleural effusion is by far the most common space-occupying process occurring in the pleural cavity ( 15.7). The value of ultrasound lies in its ability to distinguish an effusion from other diffuse lung opacities that are seen on radiographs. Ultrasound is superior to conventional chest radiographs in both sensitivity and specificity. Free effusion volumes as small as 5 mL can be identified. Sonography cannot de-
15.7). The value of ultrasound lies in its ability to distinguish an effusion from other diffuse lung opacities that are seen on radiographs. Ultrasound is superior to conventional chest radiographs in both sensitivity and specificity. Free effusion volumes as small as 5 mL can be identified. Sonography cannot de-
tect a loculated interlobar effusion or localized mediastinal fluid.
A pleural effusion displays characteristic sonographic features with regard to its location ( 15.7a,b,d–f) (unilateral/bilateral), extent (
15.7a,b,d–f) (unilateral/bilateral), extent ( 15.7c,g–i), echogenicity (
15.7c,g–i), echogenicity ( 15.7j), and the presence of septations (
15.7j), and the presence of septations ( 15.7i,k,l), depending on the cause of the effusion (Table 15.5). Goecke et al.9 described a volumetry technique
15.7i,k,l), depending on the cause of the effusion (Table 15.5). Goecke et al.9 described a volumetry technique
that has proved useful for the sonographic assessment of effusion volume (Fig.15.15).
The etiological classification of a pleural effusion is based on clinical presentation, sonographic findings, and the result of percutaneous aspiration. Table 15.6 summarizes the differential diagnosis of pleural effusion and the characteristic ultrasound findings.
523
15
Pleura and Chest Wall
Table 15.5 Possible causes of pleural effusion |
|
|
Metastatic/hemodynamic |
Inflammatory |
Neoplastic |
(usually transudate) |
(usually exudate) |
(usually exudate) |
● Heart failure |
● Pleurisy |
● Pleural carcinomatosis |
● Hepatic cirrhosis |
● Pneumonia |
● Malignant mesothelioma |
● Uremia |
● Pulmonary infarction |
● Malignant lymphoma |
● Hypercalcemia |
● Connective tissue disease |
● Sarcoma |
|
● Pancreatitis |
|
Fig. 15.15 Diagram showing the technique of pleural effusion volumetry.9
Table 15.6 Differential diagnosis of pleural effusion
|
Transudate |
Exudate |
|
|
|
|
|
|
Inflammatory |
Hemorrhagic |
Chylous |
Purulent |
Malignant |
Analysis of |
Protein < 3 g% |
Protein > 3 g% |
Protein > 3 g% |
Protein > 3 g% |
Protein > 3 g% |
Protein > 3 g% |
aspirate |
Hypocellular |
Very cellular |
Bloody |
Milky, turbid |
Debris |
Possible tumor cells |
|
LDH < 200 U/l |
Cholesterol > 60 mg% |
|
Triglycerides |
|
|
|
|
|
|
> 100 mg% |
|
|
Sonographic |
Anechoic |
Anechoic to |
Anechoic to |
Hyperechoic |
Variable sedimenta- |
Variable septa, |
characteristics |
Fine pleural line |
hyperechoic |
hyperechoic |
“Snowstorm” |
tion |
fibrin strands |
|
Frequently |
Septa, fibrin strands |
Sedimentation |
|
Air echoes |
Pleural tumors |
|
bilateral |
Accentuated pleural line |
“Snowstorm” |
|
Pleural thickening |
Parenchymal lesion |
|
|
Parenchymal lesion |
|
|
|
|
Examples |
Heart failure |
Pneumonia |
Hematothorax |
Chest trauma |
Pleural empyema |
Pleural carcinoma- |
|
Hepatic cirrhosis |
Infarction |
Tumor hemor- |
|
Pulmonary abscess |
tosis |
|
Protein deficiency |
Connective tissue |
rhage |
|
Pyothorax |
NHL |
|
|
disease |
|
|
|
Mesothelioma |
NHL = Non-Hodgkin lymphoma.
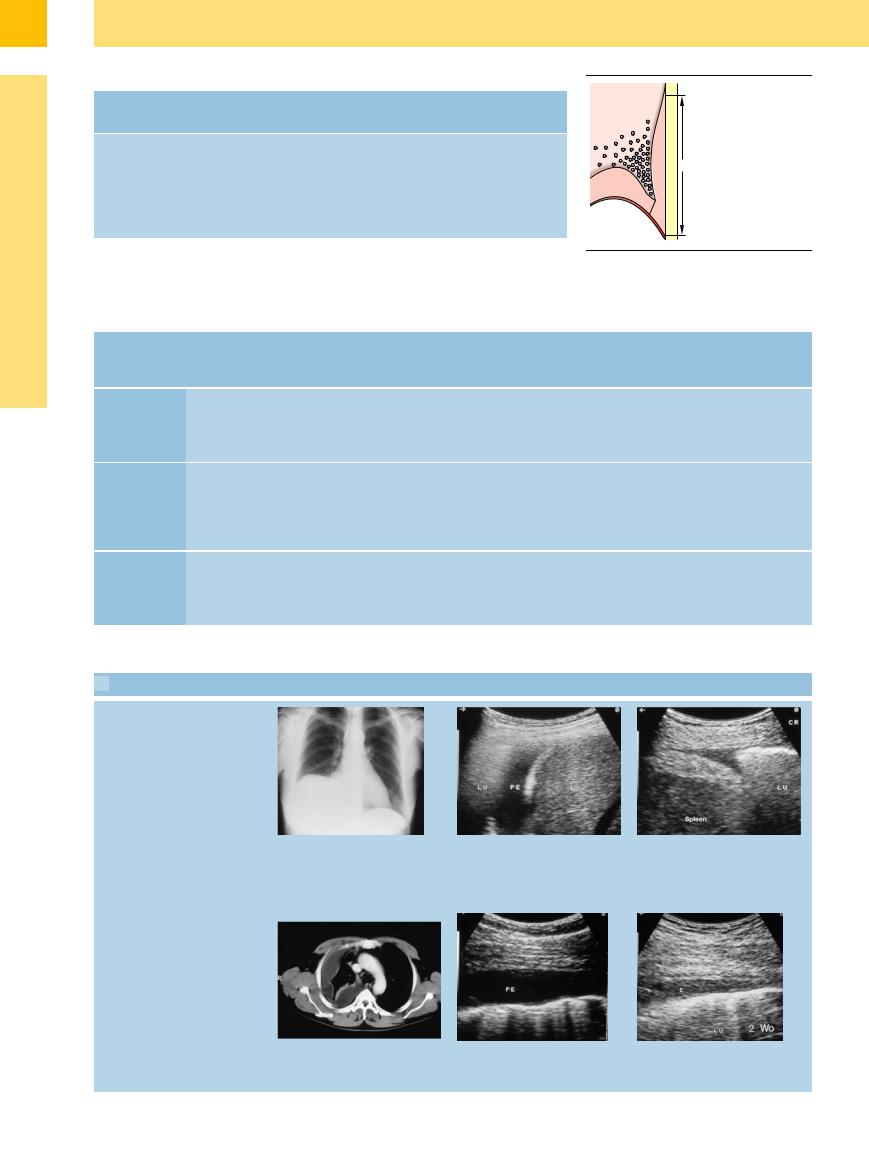
 15.7 Imaging Appearances of Pleural Effusion
15.7 Imaging Appearances of Pleural Effusion
Basal e usion, inflammatory
a–c Radiographic and sonographic appearances of pleural e usion.
a Chest radiograph shows elevation of the diaphragm in a 47-year-old woman.
b Right lateral intercostal scan demonstrates a subpulmonic e usion as the cause of the radiographic sign. PE = pleural e usion; L = liver; LU = lung.
c No e usion is visible in the conventional radiograph. Ultrasound reveals a small e usion on the left side. D = diaphragm; LU = lung.
Pleuritis with e usion
d–f A 48-year-old man with pleurisy.
d CT shows a localized fluid collection along the pleural wall.
e and f Ultrasound scans over a 6-month period document resolution of the pleural e usion (PE; E) in response to antibiotic therapy. LU = lung.
524
 15.7 Imaging Appearances of Pleural Effusion (Continued)
15.7 Imaging Appearances of Pleural Effusion (Continued)
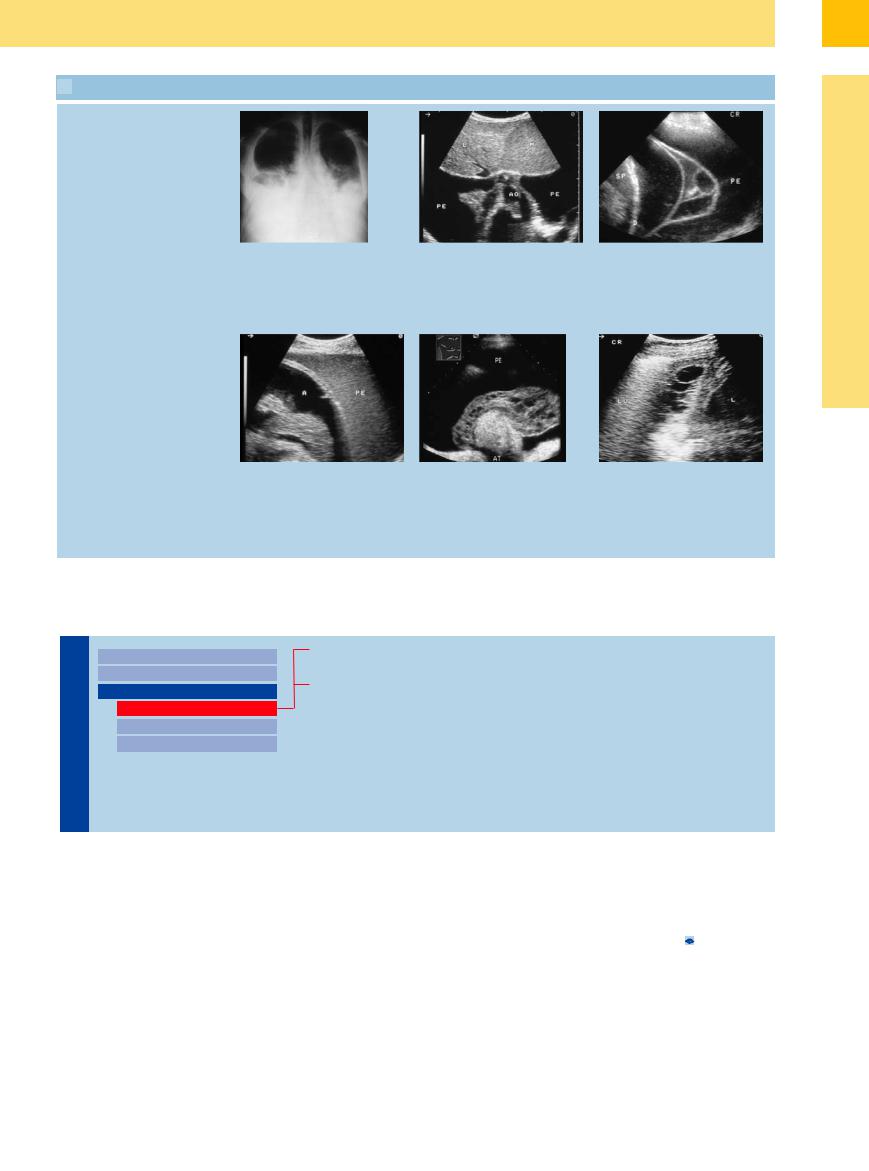
Malignant e usion: lymphoma
g and h A 39-year-old man with low-grade |
h Subcostal scan angled toward the head |
lymphoma. |
demonstrates the bilateral e usion. PE = |
g Chest radiograph shows conspicuous |
pleural e usion; L = liver. |
bilateral e usion. |
|
Malignant e usion: bronchial carcinoma
j–l E usion in patients with bronchial |
k A 74-year-old man with bronchial |
carcinoma. |
carcinoma and complete opacification of |
j Left lateral intercostal scan in a 53-year- |
the hemithorax on chest radiograph. |
old man. Ascites (A) appears as an echo- |
Ultrasound shows a conspicuous pleural |
free area, contrasting with the more |
e usion (PE) with upper lobar atelectasis |
echogenic pleural e usion (PE) on the left |
(AT). The atelectasis is surrounded by a |
side. |
honeycomb-like fibrin mass due to exu- |
|
dative e usion. |
i A 24-year-old man with Hodgkin disease. Left side cloudiness visible on chest radiograph and widening of the mediastinum. Ultrasound shows individual septa in an exudative pleural e usion. SP = spleen; D = diaphragm; PE = pleural e usion.
l Bronchial carcinoma in a 57-year-old man. Pleural e usion on the right side on chest radiograph. Right lateral intercostal scan shows septa in the pleural e usion with thickening of the pleura due to exudative e usion. L = liver; LU = lung.
Anechoic Effusion
Wall |
|
|
|
Chest Wall |
|
|
|
|
|
||
|
|
|
|
Parietal Pleura |
|
|
|
|
|||
|
|
|
|
Pleural Effusion |
|
Chest |
|
|
|
||
|
|
|
|
Anechoic Effusion |
|
|
|
|
|
|
|
andPleura |
|
|
|
|
Echogenic Effusion |
|
|
|
|
Complex Effusion |
|
|
|
|
|
|
|
Transudative Effusion
Exudative Effusion
Transudative Effusion
Effusion
















































An exudative type of pleural effusion (>2.5 g%) |
The effusion is usually benign by aspiration |
lateral chest wall that mimics a pleural effusion |
is distinguished from a transudative effusion |
cytology and occurs, for example, in heart fail- |
(Fig.15.16). An aortic aneurysm on the poste- |
(<2.5 g%) based on the protein content of the |
ure due to various causes. |
rior chest wall can also appear sonographically |
aspirate. A transudative effusion is anechoic |
With extreme cardiomegaly, the heart may |
as an anechoic liquid mass ( 15.5j–l). |
and is more often bilateral in varying degrees. |
occasionally appear as an anechoic area on the |
|
15
Pleural Effusion
525
15
Pleura and Chest Wall
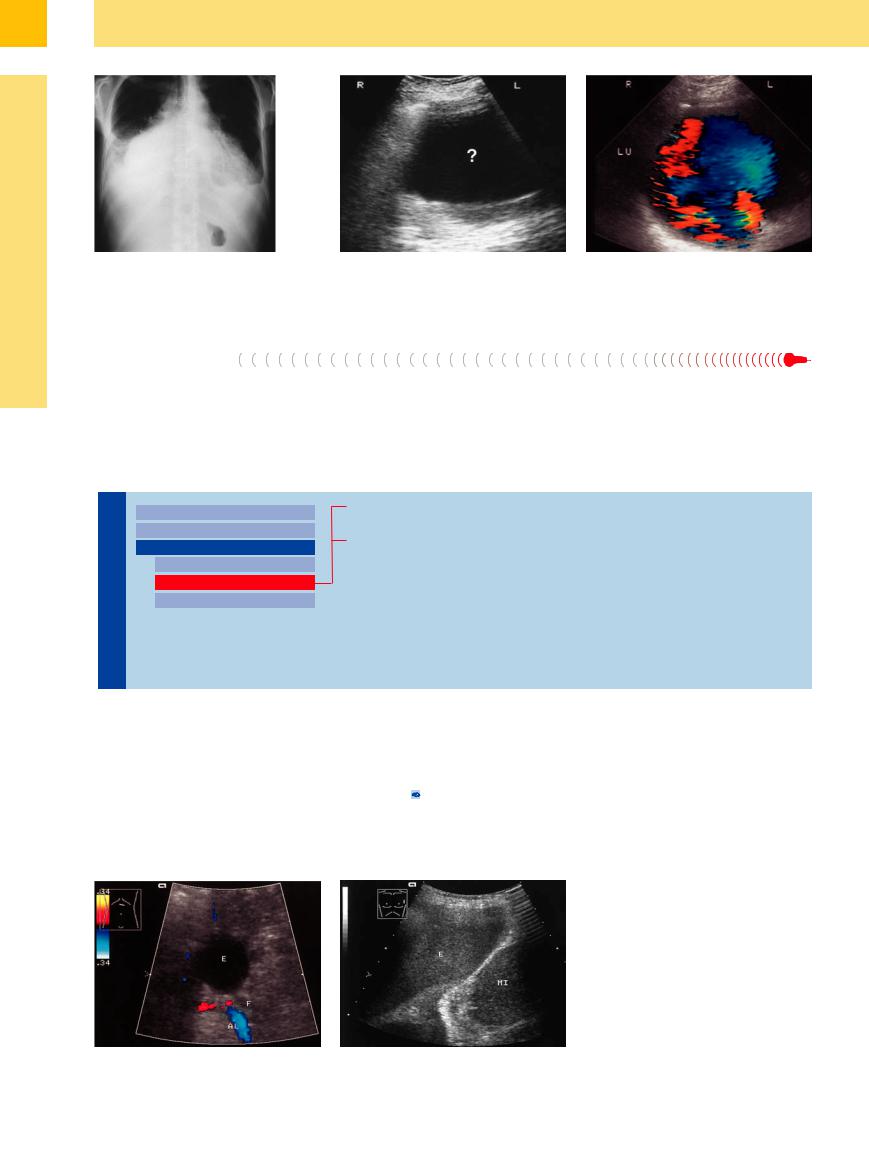
Fig. 15.16 A 54-year-old man with congestive heart failure.
a Chest radiograph shows pronounced cardiomegaly and possible pleural effusion.
Exudative Effusion
In principle, even protein-rich pleural effusions may appear anechoic. They consist mainly of parainfectious effusions (e. g., due to pleurisy,
b Right lateral intercostal scan shows an indeterminate hypoechoic mass (?).
pneumonia, polyserositis, or tuberculosis) and malignant effusions (e. g., due to bronchial or mammary carcinoma).
c Conspicuous flow patterns at color Doppler confirm that the mass is an enlarged right heart. LU = lung.
Echogenic Effusion
Wall |
|
|
|
Chest Wall |
|
|
|
|
|
||
|
|
|
|
Parietal Pleura |
|
|
|
|
|||
|
|
|
|
Pleural Effusion |
|
Chest |
|
|
|
||
|
|
|
|
Anechoic Effusion |
|
|
|
|
|
|
|
andPleura |
|
|
|
|
Echogenic Effusion |
|
|
|
|
||
|
|
|
|
Complex Effusion |
|
|
|
|
|
|
|
Benign Effusion
Malignant Effusion
Benign Effusion 



















































An echogenic pleural effusion is caused by |
The differential diagnosis of an echogenic |
Benign effusion also manifests itself as echo- |
small corpuscular reflectors suspended in the |
pleural effusion includes the following: |
genic. Fibrin strands and septa are commonly |
fluid. These may consist of fibrin components, |
● Inflammatory effusion (Fig.15.17a,b) |
observed in varying degrees. A benign effusion |
fat particles, corpuscular blood elements, air, or |
● Pyothorax ( 15.6 d–f) |
cannot be positively distinguished from a ma- |
cellular debris. Real-time ultrasound demon- |
● Hematothorax (Fig.15.17c,d) |
lignant effusion on the basis of sonographic |
strates moving echoes within the exudative |
● Chylothorax |
criteria alone. |
fluid. |
|
|
|
|
Fig. 15.17 Effusion caused by chronic recurrent pancrea- |
|
|
titis and pancreo-pleural fistula. |
|
|
a Demonstration of the fistula (F) to the pleura with |
|
|
effusion (E). AL= splenic artery. |
|
|
b Echogenic (in the drainage purulent) pleural effusion |
|
|
(E). MI = spleen. |
526
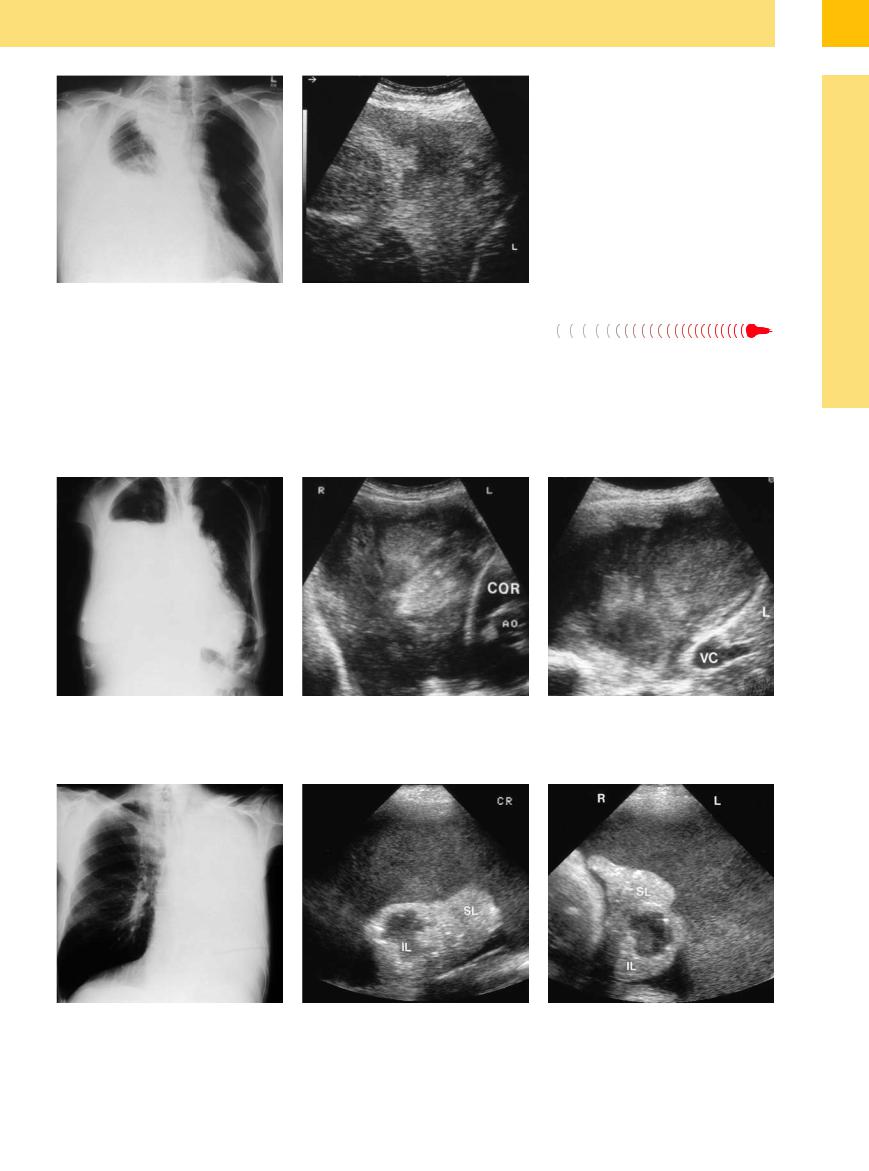
Fig. 15.17
c and d Bronchial carcinoma in a 60-year-old man.
c Chest radiograph shows almost complete opacification of the right lung.
d Right lateral intercostal scan shows a nonhomogeneous hyperechoic structure formed by echoes that move with respiration. Pleural fluid aspiration confirmed a hematothorax. L = liver.
Malignant Effusion 


























A malignant echogenic effusion is diagnosed |
pleural thickening that exceeds 1 cm or the |
the hemithorax. A larger pleural effusion leads |
when tumor cells are detected by aspiration |
detection of nodular foci of pleural thickening |
to partial atelectasis of the lung; this makes it |
cytology. The echogenicity of the effusion |
also suggests a malignant etiology. The diagno- |
possible to evaluate the lung parenchyma with |
(Fig.15.18) and the presence of fibrin strands |
sis should be confirmed by cytological analysis. |
ultrasound and detect any pulmonary nodules |
or septa are considered indirect but nonspecific |
Frequently the effusion is unilateral, and it is |
or a central tumor (Fig.15.19). |
signs. The sonographic detection of diffuse |
not uncommon to find diffuse opacification of |
|
15
Pleural Effusion
Fig. 15.18 Metastatic mucus-forming ovarian carcinoma in a 74-year-old woman.
a Chest radiograph shows almost complete opacification of the right lung.
Fig. 15.19 Bronchial carcinoma in a 63-year-old man. SL = superior lobe; IL = inferior lobe.
a Chest radiograph shows complete opacification of the left lung.
b and c Right anterior intercostal scan shows a nonhomogeneous echogenic mass containing faint echoes that move with respiration. Aspiration yielded mucoid material from an expansile tumor metastatic to ovarian carcinoma. COR = heart; VC = vena cava; L = liver; AO = aorta.
b and c Left lateral intercostal scan (b) and a second scan perpendicular to the first (c) demonstrate a hyperechoic effusion with complete atelectasis of the superior lobe (SL) and inferior lobe (IL). The inferior lobe contains a liquid mass consistent with necrotic liquefaction.
527
