
- •Contents
- •Preface
- •Contributors
- •1 Vessels
- •1.1 Aorta, Vena Cava, and Peripheral Vessels
- •Aorta, Arteries
- •Anomalies and Variant Positions
- •Dilatation
- •Stenosis
- •Wall Thickening
- •Intraluminal Mass
- •Perivascular Mass
- •Vena Cava, Veins
- •Anomalies
- •Dilatation
- •Intraluminal Mass
- •Compression, Infiltration
- •1.2 Portal Vein and Its Tributaries
- •Enlarged Lumen Diameter
- •Portal Hypertension
- •Intraluminal Mass
- •Thrombosis
- •Tumor
- •2 Liver
- •Enlarged Liver
- •Small Liver
- •Homogeneous Hypoechoic Texture
- •Homogeneous Hyperechoic Texture
- •Regionally Inhomogeneous Texture
- •Diffuse Inhomogeneous Texture
- •Anechoic Masses
- •Hypoechoic Masses
- •Isoechoic Masses
- •Hyperechoic Masses
- •Echogenic Masses
- •Irregular Masses
- •Differential Diagnosis of Focal Lesions
- •Diagnostic Methods
- •Suspected Diagnosis
- •3 Biliary Tree and Gallbladder
- •3.1 Biliary Tree
- •Thickening of the Bile Duct Wall
- •Localized and Diffuse
- •Bile Duct Rarefaction
- •Localized and Diffuse
- •Bile Duct Dilatation and Intraductal Pressure
- •Intrahepatic
- •Hilar and Prepancreatic
- •Intrapancreatic
- •Papillary
- •Abnormal Intraluminal Bile Duct Findings
- •Foreign Body
- •The Seven Most Important Questions
- •3.2 Gallbladder
- •Changes in Size
- •Large Gallbladder
- •Small/Missing Gallbladder
- •Wall Changes
- •General Hypoechogenicity
- •General Hyperechogenicity
- •General Tumor
- •Focal Tumor
- •Intraluminal Changes
- •Hyperechoic
- •Hypoechoic
- •Nonvisualized Gallbladder
- •Missing Gallbladder
- •Obscured Gallbladder
- •4 Pancreas
- •Diffuse Pancreatic Change
- •Large Pancreas
- •Small Pancreas
- •Hypoechoic Texture
- •Hyperechoic Texture
- •Focal Changes
- •Anechoic Lesion
- •Hypoechoic Lesion
- •Isoechoic Lesion
- •Hyperechoic Lesion
- •Irregular (Complex Structured) Lesion
- •Dilatation of the Pancreatic Duct
- •Marginal/Mild Dilatation
- •Marked Dilatation
- •5 Spleen
- •Nonfocal Changes of the Spleen
- •Diffuse Parenchymal Changes
- •Large Spleen
- •Small Spleen
- •Focal Changes of the Spleen
- •Anechoic Mass
- •Hypoechoic Mass
- •Hyperechoic Mass
- •Splenic Calcification
- •6 Lymph Nodes
- •Peripheral Lymph Nodes
- •Head/Neck
- •Extremities (Axilla, Groin)
- •Abdominal Lymph Nodes
- •Porta Hepatis
- •Splenic Hilum
- •Mesentery (Celiac, Upper and Lower Mesenteric Station)
- •Stomach
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •Small/Large Intestine
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •8 Peritoneal Cavity
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Wall Structures
- •Smooth Margin
- •Irregular Margin
- •Intragastric Processes
- •Intraintestinal Processes
- •9 Kidneys
- •Anomalies, Malformations
- •Aplasia, Hypoplasia
- •Cystic Malformation
- •Anomalies of Number, Position, or Rotation
- •Fusion Anomaly
- •Anomalies of the Renal Calices
- •Vascular Anomaly
- •Diffuse Changes
- •Large Kidneys
- •Small Kidneys
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Irregular Structure
- •Circumscribed Changes
- •Anechoic Structure
- •Hypoechoic or Isoechoic Structure
- •Complex Structure
- •Hyperechoic Structure
- •10 Adrenal Glands
- •Enlargement
- •Anechoic Structure
- •Hypoechoic Structure
- •Complex Echo Structure
- •Hyperechoic Structure
- •11 Urinary Tract
- •Malformations
- •Duplication Anomalies
- •Dilatations and Stenoses
- •Dilated Renal Pelvis and Ureter
- •Anechoic
- •Hypoechoic
- •Hypoechoic
- •Hyperechoic
- •Large Bladder
- •Small Bladder
- •Altered Bladder Shape
- •Intracavitary Mass
- •Hypoechoic
- •Hyperechoic
- •Echogenic
- •Wall Changes
- •Diffuse Wall Thickening
- •Circumscribed Wall Thickening
- •Concavities and Convexities
- •12.1 The Prostate
- •Enlarged Prostate
- •Regular
- •Irregular
- •Small Prostate
- •Regular
- •Echogenic
- •Circumscribed Lesion
- •Anechoic
- •Hypoechoic
- •Echogenic
- •12.2 Seminal Vesicles
- •Diffuse Change
- •Hypoechoic
- •Circumscribed Change
- •Anechoic
- •Echogenic
- •Irregular
- •12.3 Testis, Epididymis
- •Diffuse Change
- •Enlargement
- •Decreased Size
- •Circumscribed Lesion
- •Anechoic or Hypoechoic
- •Irregular/Echogenic
- •Epididymal Lesion
- •Anechoic
- •Hypoechoic
- •Intrascrotal Mass
- •Anechoic or Hypoechoic
- •Echogenic
- •13 Female Genital Tract
- •Masses
- •Abnormalities of Size or Shape
- •Uterus
- •Abnormalities of Size or Shape
- •Myometrial Changes
- •Intracavitary Changes
- •Endometrial Changes
- •Fallopian Tubes
- •Hypoechoic Mass
- •Anechoic Cystic Mass
- •Solid Echogenic or Nonhomogeneous Mass
- •14 Thyroid Gland
- •Diffuse Changes
- •Enlarged Thyroid Gland
- •Small Thyroid Gland
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Circumscribed Changes
- •Anechoic
- •Hypoechoic
- •Isoechoic
- •Hyperechoic
- •Irregular
- •Differential Diagnosis of Hyperthyroidism
- •Types of Autonomy
- •15 Pleura and Chest Wall
- •Chest Wall
- •Masses
- •Parietal Pleura
- •Nodular Masses
- •Diffuse Pleural Thickening
- •Pleural Effusion
- •Anechoic Effusion
- •Echogenic Effusion
- •Complex Effusion
- •16 Lung
- •Masses
- •Anechoic Masses
- •Hypoechoic Masses
- •Complex Masses
- •Index
Invasive Sclerosing Thyroiditis (Riedel Goiter)
Goiter)



































The cause of this “stony hard” thyroid enlargement is poorly understood, but it shows similarities to other fibrosclerosis such as the retroperitoneal fibrosis in Ormond disease. In this type of goiter, inflammation spreads from an extrathyroid source to involve the thyroid gland and other tissues in the neck. It belongs in the broader category of immune thyroiditis because it is associated with lymphocytic infil-
trates and leads to scarring and the formation of hyaline connective tissue.
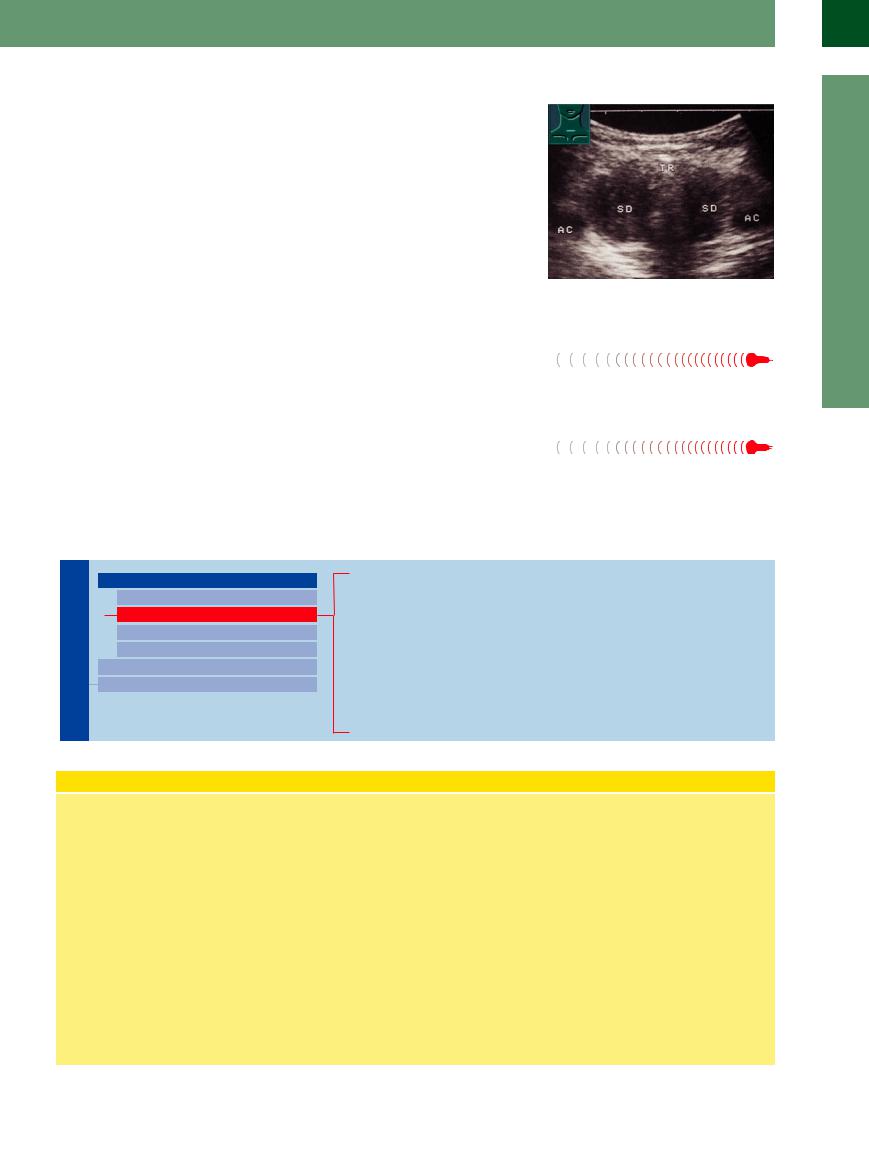
Sonographic features. The diffuse, intense hypoechoicity reflects both the presence of hypoechoic connective tissue and the inflamed condition of the thyroid, which shows a balloonlike enlargement similar to that in Graves disease (Fig.14.18).
Fig. 14.18 Riedel goiter. The thyroid exhibits balloon-like swelling with an intensely hypoechoic structure. Hypothyroidism in chronic fibrous thyroiditis.
Goiter in Acromegaly
Acromegaly 

























A goiter is almost always present in acromeg- |
goiter (73%), depending on the duration of the |
aly. It may be a diffuse goiter (93%) or a nodular |
acromegaly.8 |
Amyloidosis 






























Amyloid deposition in the thyroid, whether |
dosis, is extremely rare and leads to a relatively |
isolated or in a setting of generalized amyloi- |
coarse, diffuse increase in echogenicity. |
Small Thyroid Gland
Thyroid Gland

Diffuse Changes
Enlarged Thyroid Gland
Small Thyroid Gland
Hypoechoic Structure
Hyperechoic Structure
Circumscribed Changes
Differential Diagnosis of Hyperthyroidism
Acquired Autoimmune Thyroiditis (AIT): Atrophic Lymphocytic Thyroiditis (Juvenile)
Acquired Autoimmune Thyroiditis (AIT)
in Polyglandular Autoimmune Syndrome (PAS) Lithiumor Amiodarone-Induced Thyroiditis Neonatal Hypothyroidism
Postoperative Thyroid/Unilateral Aplasia Radioiodine-Treated Thyroid Radiation-Induced Hypothyroidism
Concept of Acquired Autoimmune Thyroiditis
Acquired autoimmune thyroiditis (AIT) is a |
dren and adolescents but is also seen in |
||
collective term for various conditions that |
older patients with latent autoimmune |
||
are probably synonymous with chronic lym- |
diabetes of adults (type II and III PAS or |
||
phocytic Hashimoto thyroiditis: |
|
PGA). Other, coexisting hormonal defi- |
|
● Chronic |
Hashimoto-type |
AIT (see |
ciencies occur in the following percen- |
above). This presents as a hypothyroid- |
tages of cases:4 |
||
ism with no other associated diseases |
– Hypoparathyroidism 80–90% |
||
and is characterized by the detection of |
– Adrenal insufficiency (Addison dis- |
||
anti-TPO and antithyroglobulin antibod- |
ease) 60–70% |
||
ies and a typical diffusely hypoechoic so- |
– Hypogonadism 40–50% |
||
nographic |
pattern. Small, |
hyperechoic |
– Type 1 diabetes 10–20% |
foci of scarring appear in the late stage. |
– Autoimmune gastritis |
||
The peak frequency of atrophic thyroidi- |
Conversely, 70–80% of patients who have |
||
tis lies between 50 and 60 years of age. |
|||
● Polyglandular autoimmune syndrome |
had type 1 diabetes for an average of |
||
(PAS). This is an autoimmune hypothyr- |
18 years also have hypothyroidism. |
||
oidism that is associated with type 1 diabetes and most commonly occurs in chil-
In the type II form of PGA, AIT and type 1 diabetes are accompanied by hypogonadism, myasthenia, vitiligo, and alopecia.
In type III PGA, type 1 diabetes is accompanied by an AIT or by adrenal insufficiency with Hashimoto AIT.
●Chronic thyroiditis (juvenile) with transient hyperthyroidism.
●Postpartum thyroiditis (see below).
●Other forms of AIT such as lithium-, amiodaroneor interferon-induced thyroiditis are probably separate entities that do not fall under the heading of Hashimoto thyroiditis.
14
Diffuse Changes
483
14
Thyroid Gland
Acquired Autoimmune Thyroiditis
Autoimmune Thyroiditis  (AIT):
(AIT):






































Atrophic Lymphocytic Thyroiditis (Juvenile)
Atrophic thyroiditis is responsible for most cases of silent hypothyroidism in adults, followed by hypothyroidism after a thyroid resection. The atrophic form is far more common than the classic Hashimoto thyroiditis associated with a goiter (see above).
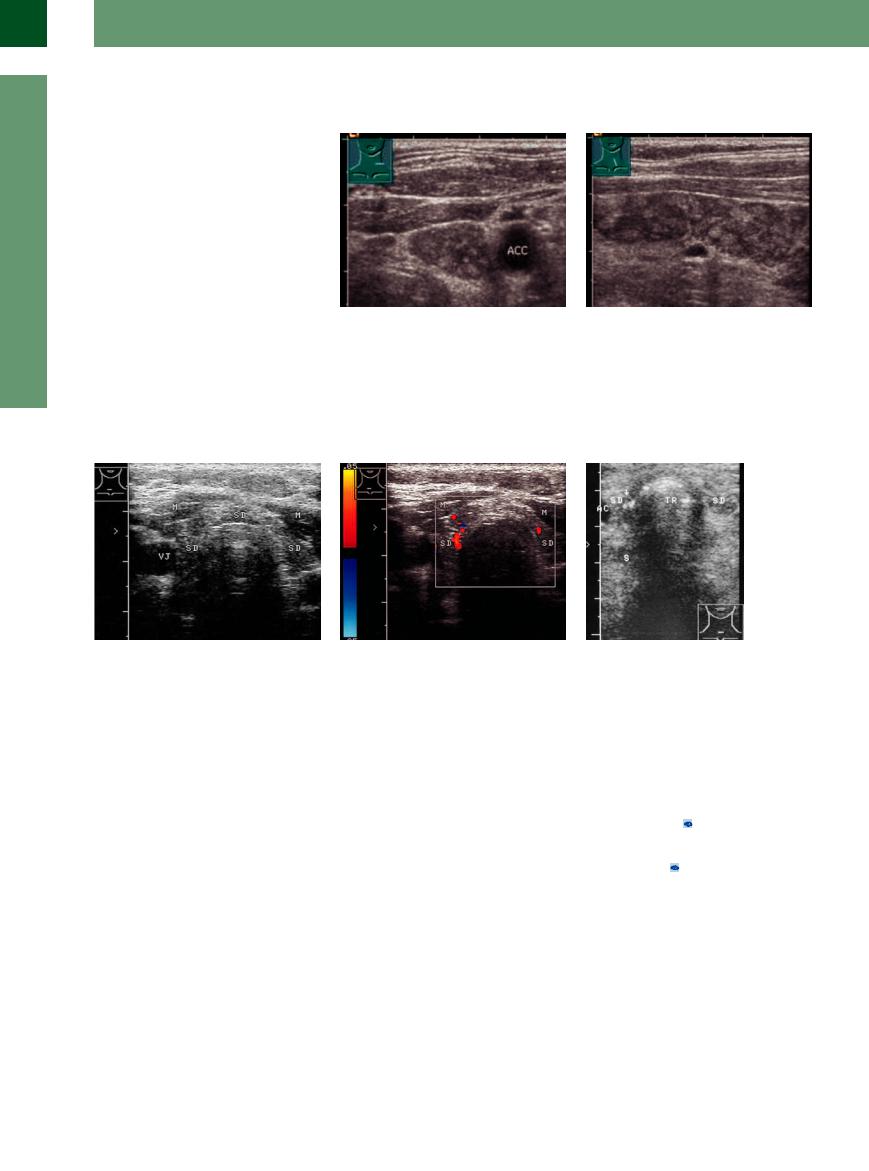
Sonographic features. Ultrasound shows a markedly small thyroid, often asymmetrical, with a homogeneous grainy or patchy hypoechoic texture containing fine, hyperechoic areas of scarring. The scars may produce contour irregularities (Fig.14.19a, Fig.14.20a).
Color duplex examination shows a fine or coarse pattern of vascular signals that may still be very pronounced or already diminished owing to scarring (Fig. 14.19b, Fig.14.20b).
Scans at the end stage of myxedema may still show residual areas of thyroid tissue, whose volume is less than that of a normal thyroid lobe (Fig.14.21).
Fig. 14.19 Chronic atrophic initial stage-autoimmune Hashimoto thyroiditis. M = sternocleidomastoid muscle; I = isthmus with a section of muscle; TR = trachea.
a Transverse scan shows a hypoechoic background texture with small, hyperechoic inclusions, probably due to focal scarring.
b Longitudinal scan on the left side.
Fig. 14.20 Atrophy in autoimmune Hashimoto thyroiditis |
b Color duplex. The initial hypervascularity is still appre- |
Fig. 14.21 Myxedema due to complete thyroid atrophy |
with severe hypothyroidism. M = muscle; VJ = jugular |
ciated in the thyroid remnants. |
(TH) with microcalcifications and acoustic shadowing (S). |
vein. |
|
TR = trachea. |
a Atrophic thyroid gland (TH) with a patchy hypoechoic |
|
|
texture. |
|
|
Acquired Autoimmune Thyroiditis
Autoimmune Thyroiditis  (AIT)
(AIT)  in
in





































Polyglandular Autoimmune Syndrome (PAS)
Diabetes-associated AIT is common in long- |
The echo texture and vascularity are like |
moto thyroiditis. The thyroid gland becomes |
standing cases of diabetes. For this reason, a |
those seen in other types of AIT, as are the |
small in the advanced stage, presenting a hy- |
TSH test and/or thyroid ultrasound scan should |
clinical manifestations and patterns of elevated |
poechoic structure ( 14.1a–c). |
be performed in any patient who has more |
anti-TPO antibodies and borderline anti-TSH |
Largely identical patterns are also seen in |
than a 10-year history of type 1 diabetes. |
receptor antibodies, although the TPO titers |
non-diabetes-associated forms of autoimmune |
|
often do not reach the same level as in Hashi- |
hypothyroidism ( 14.1 d–f). |
484
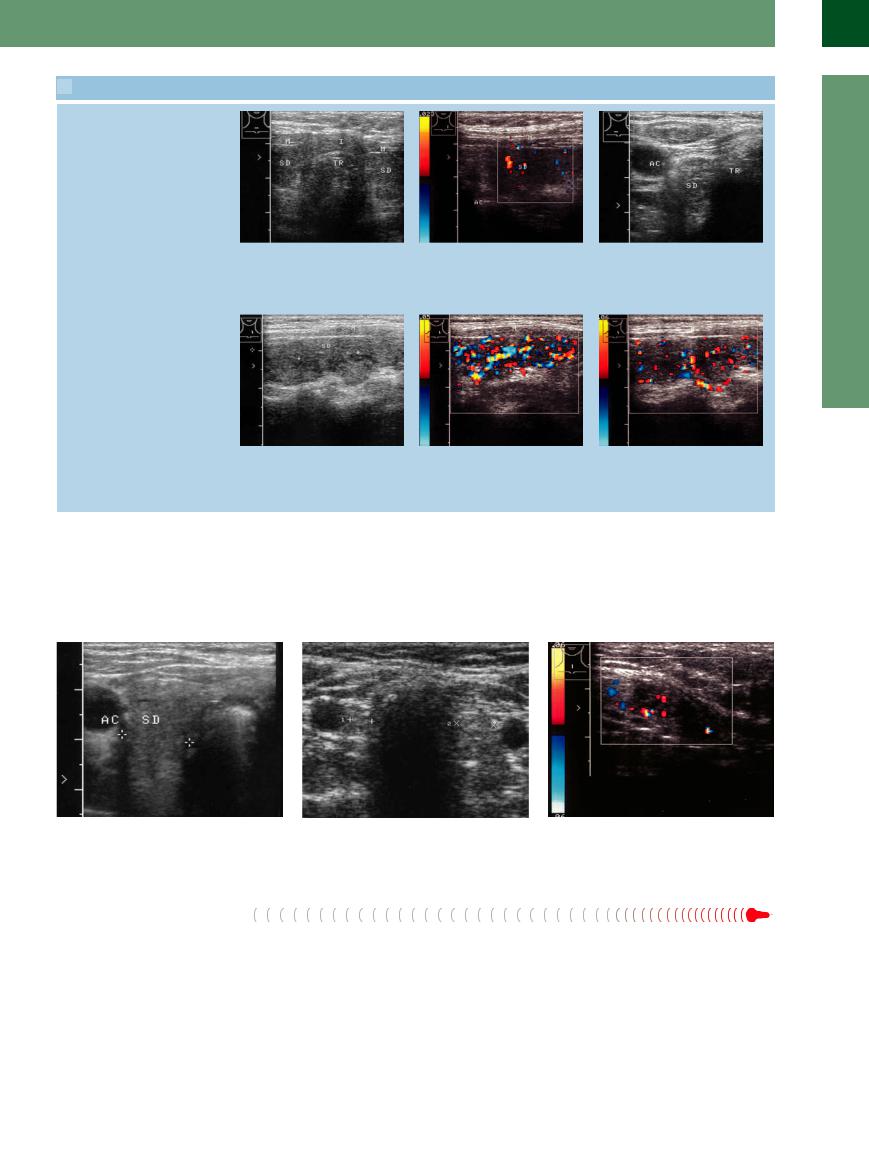
 14.1 Acquired Autoimmune Thyroiditis in Polyglandular Autoimmune Syndrome
14.1 Acquired Autoimmune Thyroiditis in Polyglandular Autoimmune Syndrome
AIT in type 1 diabetes mellitus
a Small thyroid lobes (TH), uniformly |
b Color Doppler view of the left lobe in a |
c Severely atrophic thyroid gland (TH) in |
hypoechoic to the muscle (M). I = |
(TH) with a very low PRF (corresponding |
long-standing diabetes mellitus. Only a |
isthmus, TR = trachea. |
to a Vmax of 0.023 m/s) shows scant |
greatly enlarged view can identify rem- |
|
vascularity. |
nants between the common carotid |
|
|
artery (AC) and trachea (TR). |
AIT, autoimmune gastritis, operated renal cell carcinoma
14
Diffuse Changes
d Very high anti-TPO titers and low titers of anti-TSH receptor antibodies in a 50- year-old woman with hypothyroidism. Longitudinal scan on the left side. TH = thyroid gland; M = muscle.
e and f Color Doppler scans of the left thyroid lobe. Longitudinal scan shows intense, irregular color-flow signals with spared areas, which are also spared from hypoechoicity in the B-mode image (d) (may be autonomous adenomas not involved by the AIT).
Lithiumor Amiodarone-Induced
Amiodarone-Induced Thyroiditis
Thyroiditis




































Both lithium and amiodarone can cause or ignite a chronic thyroiditis. Hyperthyroidism develops, and a hypothyroid atrophy of the
thyroid gland can develop with long-term use (Fig.14.22).
Fig. 14.22
a Hypothyroidism under amiodarone. Small hypoechoic thyroid (SD); TR= trachea, AC= common carotid artery.
b Thyroid atrophy following 10 years of lithium therapy. |
c Lithium-induced hyperthyroidism: small left thyroid |
Small, hypoechoic thyroid remnants. |
gland with intensively hypoechoic echo texture and mod- |
|
erate vascularity by color duplex. |
Neonatal Hypothyroidism
Hypothyroidism
This condition is often based on ectopic thyroid tissue (lingual thyroid, aplasia), as indicated by the absence of detectable thyroglobulin.
In a study of 38 newborns with congenital primary hypothyroidism, Meller et al.9 found 7 cases of athyrosis, 9 lingual goiters, and 15 infants with an iodine organification defect (4 with Pendred syndrome). Ectopic thyroid tis-
sue could be detected only by radionuclide scanning. In four of the patients, the correct diagnosis could be made only by scintigraphy using the perchlorate depletion test.
Ultrasound yielded a false-negative diagnosis in two patients with hypoplasia and a falsepositive diagnosis in two other patients with athyrosis. Thus, while ultrasound has limited
value in terms of diagnostic accuracy, thyroid sonography is still an essential routine study for detecting an orthotopic or ectopic thyroid gland. Radionuclide scanning is still superior for locating an ectopic thyroid, however.
Immunogenic neonatal hypothyroidism often results from the transmission of maternal blocking antibodies to the fetus.
485
14
Thyroid Gland
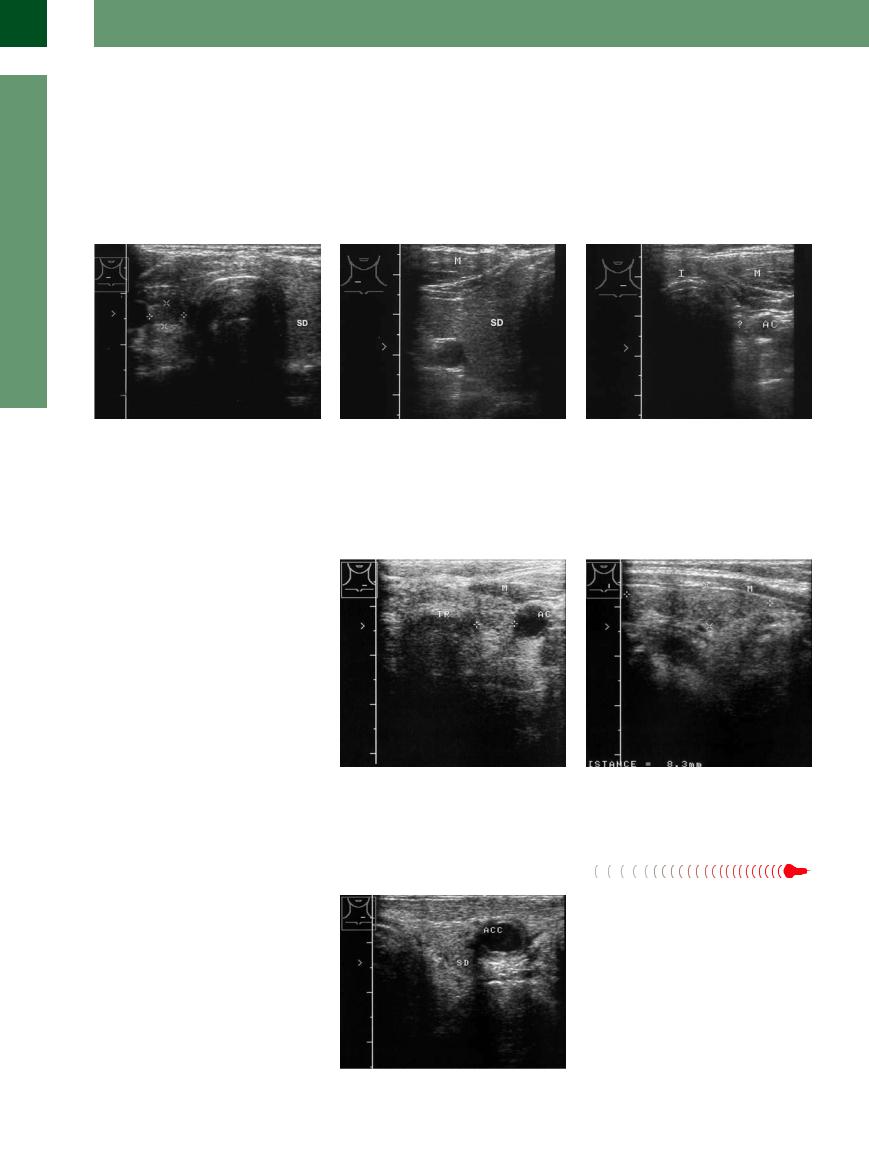
Postoperative Thyroid/Unilateral Aplasia
Aplasia 





































During surgical resection of the thyroid gland (strumectomy), the poles are exposed and the posterior portions of the gland are dissected free in the area of the recurrent nerve. The isthmus is resected first, followed by the other parts of the gland, leaving a remnant of thyroid tissue measuring approximately 2–4 cm × 2 cm × 2 cm. Nodular areas are resected completely.
Thus, a subtotal strumectomy leaves behind a greatly diminished residual gland that can be identified and measured sonographically (Fig.14.23).
When a total strumectomy is performed for thyroid carcinoma, all portions of the gland are resected after the recurrent nerve has been
dissected free. Ultrasound does not demonstrate a thyroid remnant in these cases.
In both operations, the parathyroid glands posterior to the upper and lower poles of the thyroid are left intact.
Unilateral aplasia is occasionally detected incidentally in adults (previous surgery should be excluded).
Fig. 14.23 Small residual thyroid (TH, cursors) following a subtotal strumectomy. The remnant displays a normal echo structure.
a Postoperative thyroid gland: small amount of residual thyroid tissue on the right side (cursors).
band c Unilateral aplasia of the thyroid gland.
bStrong right lobe (SD).
c On the left side no detectable lobe. Normal thyroid function, no history of surgery. AC = common carotid artery; I = isthmus; M = muscle.
Radioiodine-Treated Thyroid
Thyroid 












































Following radioiodine treatment with iodine127, the thyroid volume may continued to decrease even 1–2 years after the therapy. Volume reductions of 20–40% are typically achieved, with some cases showing up to a 70% reduction. Hypothyroidism can develop in 15% of cases (Fig.14.24).2
Fig. 14.24 Left thyroid lobe (cursors) following radioiodine |
b Longitudinal scan. |
therapy. The organ is markedly reduced in size and shows |
|
slightly irregular contours. AC = common carotid artery; |
|
M = muscle; TR = trachea. |
|
a Transverse scan. |
|
Radiation-Induced Hypothyroidism
Hypothyroidism


















In these cases the cause of the hypothyroidism is determined from the history. Ultrasound generally shows a small thyroid gland with normal or slightly increased echogenicity. The contours may be irregular owing to scarring (Fig.14.25).
Fig. 14.25 Radiation-induced hypothyroidism. The patient underwent surgery for palatal carcinoma with radiation to the neck nodes. Hypothyroidism developed years later. a Transverse scan on the left side shows a small thyroid lobe (TH) and irregular, indistinct vessels that are distorted due to scarring. ACC = common carotid artery.
486
