
- •Contents
- •Preface
- •Contributors
- •1 Vessels
- •1.1 Aorta, Vena Cava, and Peripheral Vessels
- •Aorta, Arteries
- •Anomalies and Variant Positions
- •Dilatation
- •Stenosis
- •Wall Thickening
- •Intraluminal Mass
- •Perivascular Mass
- •Vena Cava, Veins
- •Anomalies
- •Dilatation
- •Intraluminal Mass
- •Compression, Infiltration
- •1.2 Portal Vein and Its Tributaries
- •Enlarged Lumen Diameter
- •Portal Hypertension
- •Intraluminal Mass
- •Thrombosis
- •Tumor
- •2 Liver
- •Enlarged Liver
- •Small Liver
- •Homogeneous Hypoechoic Texture
- •Homogeneous Hyperechoic Texture
- •Regionally Inhomogeneous Texture
- •Diffuse Inhomogeneous Texture
- •Anechoic Masses
- •Hypoechoic Masses
- •Isoechoic Masses
- •Hyperechoic Masses
- •Echogenic Masses
- •Irregular Masses
- •Differential Diagnosis of Focal Lesions
- •Diagnostic Methods
- •Suspected Diagnosis
- •3 Biliary Tree and Gallbladder
- •3.1 Biliary Tree
- •Thickening of the Bile Duct Wall
- •Localized and Diffuse
- •Bile Duct Rarefaction
- •Localized and Diffuse
- •Bile Duct Dilatation and Intraductal Pressure
- •Intrahepatic
- •Hilar and Prepancreatic
- •Intrapancreatic
- •Papillary
- •Abnormal Intraluminal Bile Duct Findings
- •Foreign Body
- •The Seven Most Important Questions
- •3.2 Gallbladder
- •Changes in Size
- •Large Gallbladder
- •Small/Missing Gallbladder
- •Wall Changes
- •General Hypoechogenicity
- •General Hyperechogenicity
- •General Tumor
- •Focal Tumor
- •Intraluminal Changes
- •Hyperechoic
- •Hypoechoic
- •Nonvisualized Gallbladder
- •Missing Gallbladder
- •Obscured Gallbladder
- •4 Pancreas
- •Diffuse Pancreatic Change
- •Large Pancreas
- •Small Pancreas
- •Hypoechoic Texture
- •Hyperechoic Texture
- •Focal Changes
- •Anechoic Lesion
- •Hypoechoic Lesion
- •Isoechoic Lesion
- •Hyperechoic Lesion
- •Irregular (Complex Structured) Lesion
- •Dilatation of the Pancreatic Duct
- •Marginal/Mild Dilatation
- •Marked Dilatation
- •5 Spleen
- •Nonfocal Changes of the Spleen
- •Diffuse Parenchymal Changes
- •Large Spleen
- •Small Spleen
- •Focal Changes of the Spleen
- •Anechoic Mass
- •Hypoechoic Mass
- •Hyperechoic Mass
- •Splenic Calcification
- •6 Lymph Nodes
- •Peripheral Lymph Nodes
- •Head/Neck
- •Extremities (Axilla, Groin)
- •Abdominal Lymph Nodes
- •Porta Hepatis
- •Splenic Hilum
- •Mesentery (Celiac, Upper and Lower Mesenteric Station)
- •Stomach
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •Small/Large Intestine
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •8 Peritoneal Cavity
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Wall Structures
- •Smooth Margin
- •Irregular Margin
- •Intragastric Processes
- •Intraintestinal Processes
- •9 Kidneys
- •Anomalies, Malformations
- •Aplasia, Hypoplasia
- •Cystic Malformation
- •Anomalies of Number, Position, or Rotation
- •Fusion Anomaly
- •Anomalies of the Renal Calices
- •Vascular Anomaly
- •Diffuse Changes
- •Large Kidneys
- •Small Kidneys
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Irregular Structure
- •Circumscribed Changes
- •Anechoic Structure
- •Hypoechoic or Isoechoic Structure
- •Complex Structure
- •Hyperechoic Structure
- •10 Adrenal Glands
- •Enlargement
- •Anechoic Structure
- •Hypoechoic Structure
- •Complex Echo Structure
- •Hyperechoic Structure
- •11 Urinary Tract
- •Malformations
- •Duplication Anomalies
- •Dilatations and Stenoses
- •Dilated Renal Pelvis and Ureter
- •Anechoic
- •Hypoechoic
- •Hypoechoic
- •Hyperechoic
- •Large Bladder
- •Small Bladder
- •Altered Bladder Shape
- •Intracavitary Mass
- •Hypoechoic
- •Hyperechoic
- •Echogenic
- •Wall Changes
- •Diffuse Wall Thickening
- •Circumscribed Wall Thickening
- •Concavities and Convexities
- •12.1 The Prostate
- •Enlarged Prostate
- •Regular
- •Irregular
- •Small Prostate
- •Regular
- •Echogenic
- •Circumscribed Lesion
- •Anechoic
- •Hypoechoic
- •Echogenic
- •12.2 Seminal Vesicles
- •Diffuse Change
- •Hypoechoic
- •Circumscribed Change
- •Anechoic
- •Echogenic
- •Irregular
- •12.3 Testis, Epididymis
- •Diffuse Change
- •Enlargement
- •Decreased Size
- •Circumscribed Lesion
- •Anechoic or Hypoechoic
- •Irregular/Echogenic
- •Epididymal Lesion
- •Anechoic
- •Hypoechoic
- •Intrascrotal Mass
- •Anechoic or Hypoechoic
- •Echogenic
- •13 Female Genital Tract
- •Masses
- •Abnormalities of Size or Shape
- •Uterus
- •Abnormalities of Size or Shape
- •Myometrial Changes
- •Intracavitary Changes
- •Endometrial Changes
- •Fallopian Tubes
- •Hypoechoic Mass
- •Anechoic Cystic Mass
- •Solid Echogenic or Nonhomogeneous Mass
- •14 Thyroid Gland
- •Diffuse Changes
- •Enlarged Thyroid Gland
- •Small Thyroid Gland
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Circumscribed Changes
- •Anechoic
- •Hypoechoic
- •Isoechoic
- •Hyperechoic
- •Irregular
- •Differential Diagnosis of Hyperthyroidism
- •Types of Autonomy
- •15 Pleura and Chest Wall
- •Chest Wall
- •Masses
- •Parietal Pleura
- •Nodular Masses
- •Diffuse Pleural Thickening
- •Pleural Effusion
- •Anechoic Effusion
- •Echogenic Effusion
- •Complex Effusion
- •16 Lung
- •Masses
- •Anechoic Masses
- •Hypoechoic Masses
- •Complex Masses
- •Index
■ Vena Cava, Veins
Anomalies
Vessels |
|
|
Aorta, Arteries |
|
|
|
|
||
|
|
|
Vena Cava, Veins |
|
|
|
|||
|
|
|
|
Anomalies |
|
|
|
|
|
|
|
|
|
Dilatation |
|
|
|
|
Intraluminal Mass |
|
|
|
|
Compression, Infiltration |
Anomalies/Duplication of the Inferior Vena Cava Anomalies of the Iliac Veins
Duplication of Renal and Peripheral Veins
Anomalies/Duplication of the Inferior Vena
the Inferior Vena  Cava
Cava 

































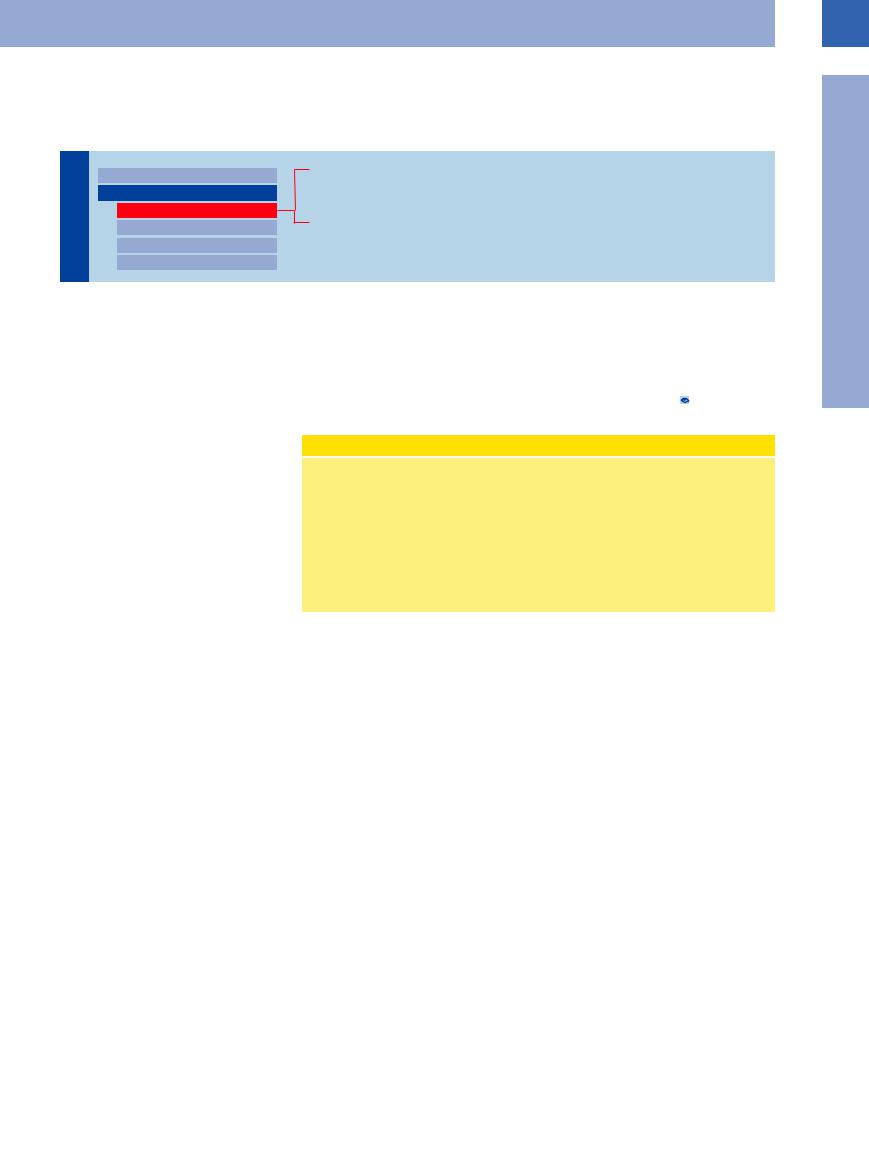
Anomalies. Anomalies of the vena cava are infrequent and most are incidental findings during ultrasonography, in which case they present problems regarding the differential diagnosis. Precise knowledge of the anatomy is invaluable in these instances. Agenesis is extremely rare and is usually associated with other clinically significant cardiovascular malformations during the prenatal and postnatal period. Situs inversus is discussed in the section on anomalies of the aorta (see Fig.1.6).
Duplication. Quite often duplication of the vena cava is overlooked because it does not result in any symptoms—except for thrombosis.
Duplication of the inferior vena cava is not especially rare. As part of complex embryonic
disorders, such duplication develops from the |
the inferior vena cava. The classification is |
embryonic post-, suband supracardinal veins, |
based on the three possible segments involved, |
which make up a primarily bilateral, symmet- |
and for the postrenal segment is subdivided |
ric, abdominal venous system fusing to the |
into the four types A to BC. 1.4 shows exam- |
secondary dextroverted asymmetric system of |
ples of vena cava duplication. |
Congenital Anomalies of the Inferior Vena Cava
●I Postrenal segment
–Type A: persistent right postcardinal vein (“retroor periaortic ureter”)
–Type B: persistent right supracardinal vein (“normal inferior vena cava”)
–Type C: persistent left supracardinal vein (“left inferior vena cava”)
–Type BC: persistent left and right supracardinal veins (“duplicated inferior vena cava”)
●II Renal segment
–Persistent ring of renal veins (“periaortic ureter”)
●III Prerenal or hepatic segment
–Missing hepatic segment (“azygos or hemiazygos vein continuation”)
1
Vena Cava, Veins
29
1
Vessels
 1.4 Duplicated Inferior Vena Cava
1.4 Duplicated Inferior Vena Cava
a Longitudinal right paramedian view of the abdomen: right iliac vein (VI) and inferior vena cava (VC).
c and d Transverse view at the umbilicus, B-mode image (c) and color-flow Doppler scan (d): there are two inferior venae cava (VC) with respective color signals. The left renal vein (VR) joins the left inferior vena cava and does not cross the aorta anteriorly in order to join the right vena cava as would be the case in normal anatomy. AO = aorta.
b Longitudinal left paramedian view of the abdomen: left iliac vein (VI) and inferior vena cava (VC); partial view of the iliac artery (AI).
e Oblique subxiphoidal median view: the left inferior vena cava (VC) crosses the aorta (AO) anteriorly and runs obliquely in a cephalad direction joining the right vena cava (VC) (other courses are possible) before entering the right atrium (RA).
f Retroaortal left renal vein: sonographic image and schematic presentation.
g Circumaortal left renal vein: sonographic image and schematic presentation.
h Transposition of the inferior vena cava: sonographic image and schematic presentation.
i Duplication of the inferior vena cava: sonographic image and schematic presentation.
Anomalies of the Iliac
of the Iliac Veins
Veins 












































Anomalies of the iliac veins are also known and may become a problem in surgery or thrombosis. In most cases it is an abnormal junction of
the left iliac vein with the right common iliac vein or a true duplication.
30
Duplication of Renal and Peripheral Veins
Renal and Peripheral Veins





































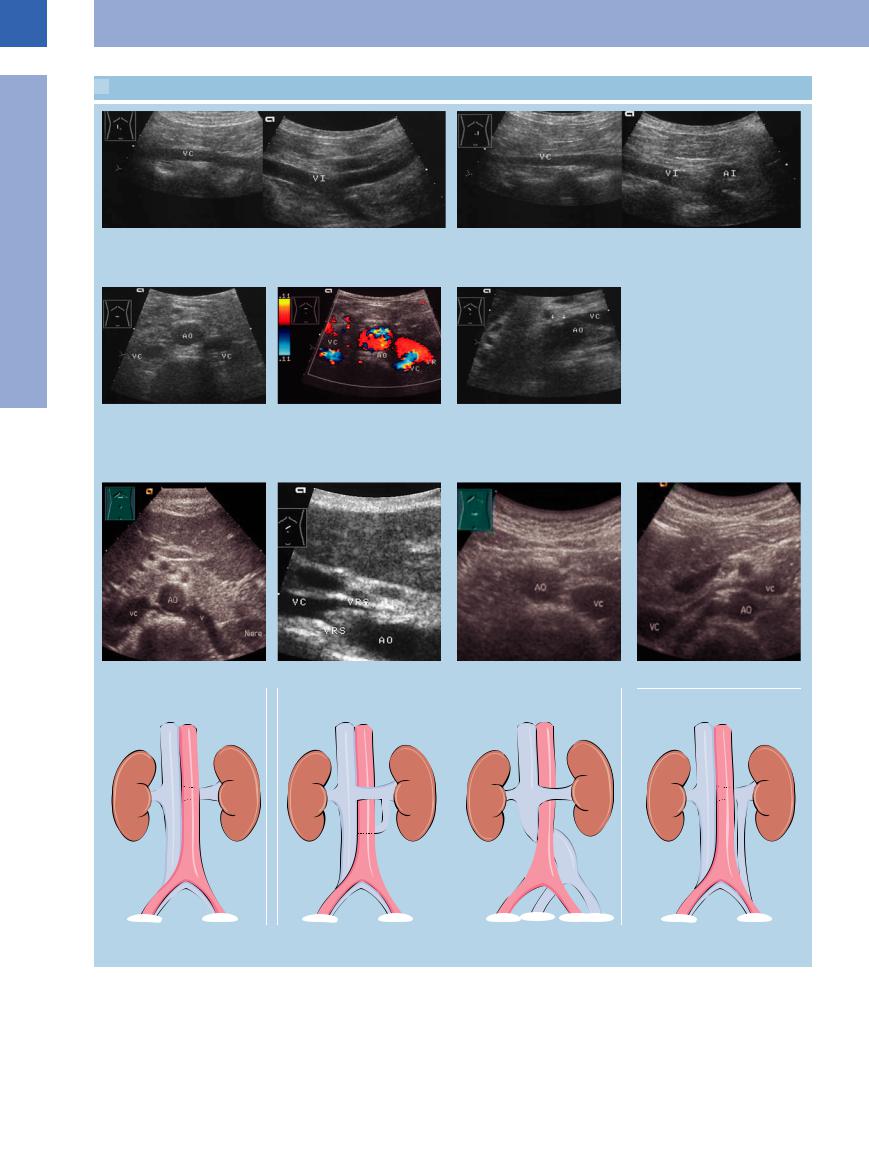
Fig. 1.61 Left renal vein divided into two branches (1, 2); branch 1 corresponds to the regular course crossing over the aorta (AO). VL = splenic vein, PS = pancreatic tail.
A retroaortic left renal vein, or duplicated renal veins, may become significant if there is thrombosis or the suspicion of tumor infiltration (Fig.1.61). Duplication of the popliteal vein is a frequent variant of normal anatomy, but duplicated femoral veins are rare. Most of these cases are incidental findings in the work-up of deep venous thrombosis (see below).
Dilatation
Vessels |
|
Aorta, Arteries |
|
|
|
|
|
Vena Cava, Veins |
|
|
|
|
|
Anomalies |
|
|
Dilatation |
|
|
Intraluminal Mass |
|
|
Compression, Infiltration |
Inferior Vena Cava Engorgement
Prestenotic and Poststenotic Dilatation
Thrombosis
Venectasia
Venous Insufficiency
Inferior Vena Cava Engorgement
Engorgement










































1
Vena Cava, Veins
Fig. 1.62 Inferior vena cava and hepatic vein engorgement.
a Marked expansion of the vena cava to 28.7 mm at end expiration (cursors).
The most common cause of an engorged inferior vena cava is cardiac congestion, which in turn may be due to right ventricular failure, pulmonary embolism, pericardial fibrosis (armored heart), or mitral valve disorders.
In ultrasonography, cardiac congestion is seen as engorgement of the right atrium and ventricle, inferior vena cava (beyond 20 mm),
b In inspiration, marked physiologic decrease of the diameter to 5.2 mm; engorgement of the vena cava must therefore be ruled out.
and hepatic veins (beyond 10 mm). The lack of physiological and respiration-induced variation in the caliber of the inferior vena cava and its incompressibility are vital diagnostic criteria and simply mirror the congestion of the vein. Engorgement of the inferior vena cava also implies enlarged venous tributaries (Fig.1.62).
c Severe cardiac-related engorgement of the vena cava (cursors); diameter 47.5 mm with dilated right atrium.
d Systolic increased hepatopetal flow (red) of the liver veins in tricuspid insufficiency and aortic–mitral valve defect. Retrograde conversion of the systolic wave (above the baseline in the spectral analysis; normally inferior to it). End-systolic expanded and end-diastolic increased flow.
31
1
Vessels
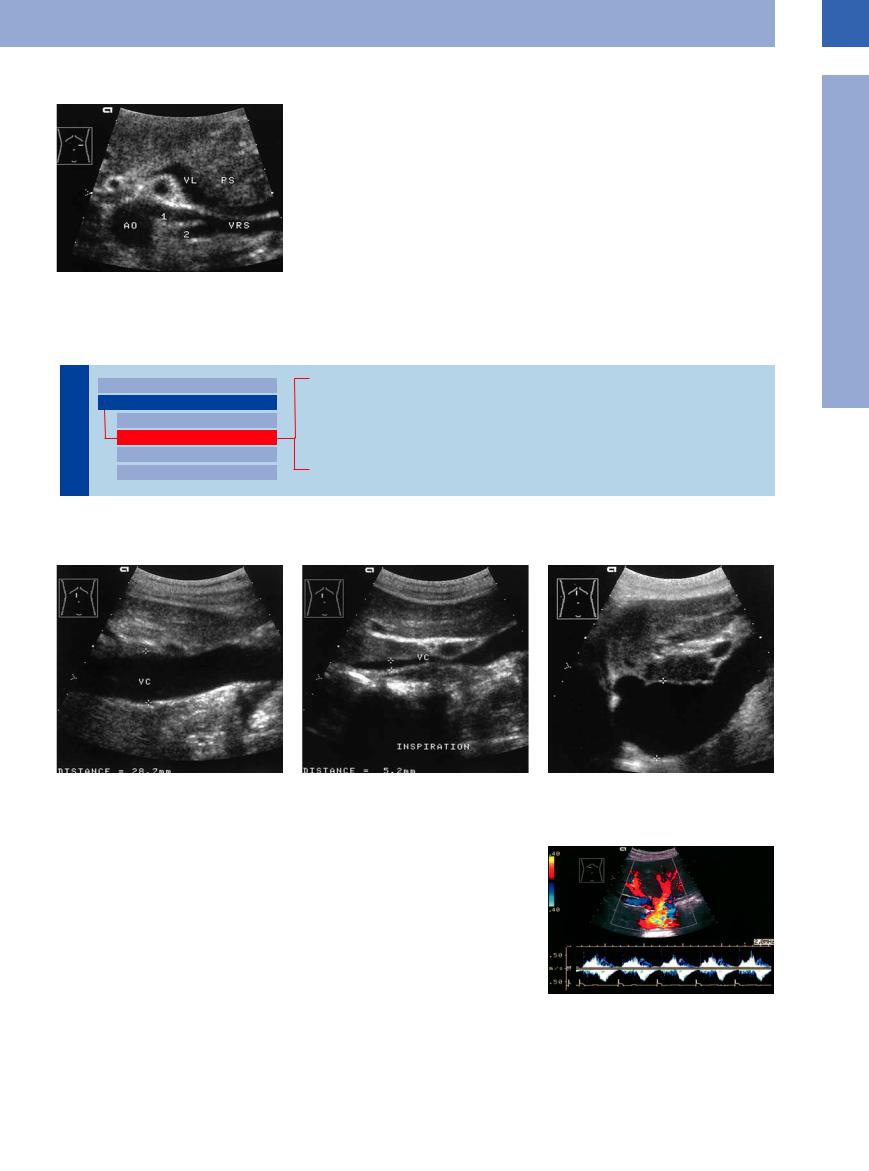
Prestenotic and Poststenotic Dilatation
Dilatation 






































Stenosis of the inferior vena cava will result in prestenotic and poststenotic enlargement of the vein, this sometimes being the only sign of any obstruction (Fig.1.63, Fig.1.64).
Fig. 1.63 Prestenotic enlargement of the inferior vena |
Fig. 1.64 Poststenotic enlargement of the inferior vena |
cava due to two renal arteries (arrows) crossing posteri- |
cava. |
orly. Color-flow Doppler scanning with fixed Doppler ve- |
a Decreased flow velocity with turbulence (“RBC noise,” |
locity of 23 cm/s. Because of decreased flow velocity |
arrows). |
there is no color signal in the vena cava segment (VC) |
|
proximal to the stenosis. |
|
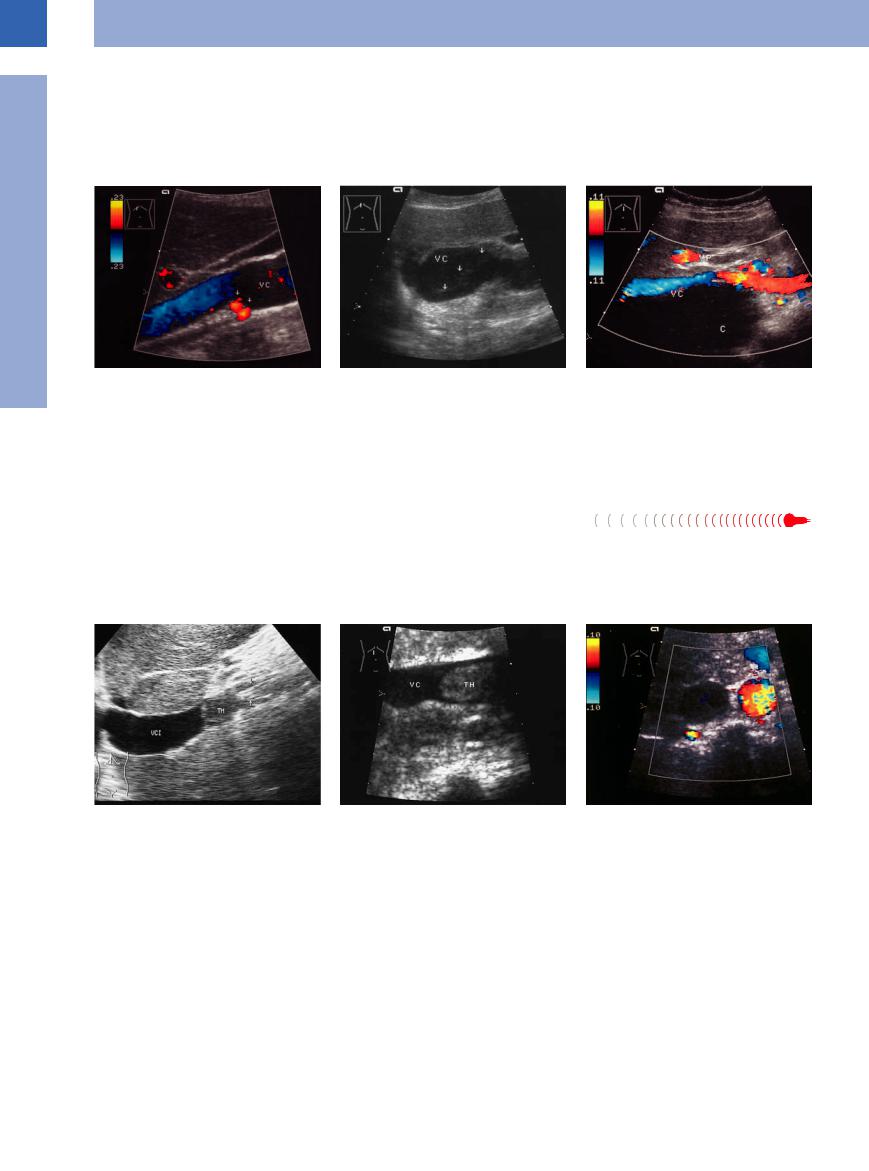
Thrombosis 






























Lesions in the vessel wall, venostasis, and hy- |
which should always be included in the differ- |
percoagulability (Virchow’s triad) will trigger |
ential diagnosis. |
venous thrombosis. The latter two also are |
In ultrasound imaging, the essential charac- |
causative factors in paraneoplastic thrombosis, |
teristics of venous thrombosis are a vein en- |
Fig. 1.65 |
b Vena cava thrombosis (VC, TH) in a patient with para- |
a Vena cava thrombosis (TH) in a patient with protein S |
neoplastic syndrome, 32-year-old man, metastatic germ |
and C deficiency, vena cava filter (arrows): thrombotic |
cell tumor. |
(TH) and poststenotic enlargement of the vena cava |
|
(VCI). |
|
b Slight prestenotic and poststenotic dilatation; colorflow Doppler scan: a 4 liter (!) liver cyst with hematoma, extending behind the vena cava (VC) with extended indentation of the posterior wall of the vein. VP = portal vein. C = cyst.
larged to more than 1.5 times the diameter of the respective artery15 and the lack of compressibility (Fig.1.65; see also Fig.1.13) (also see “Intraluminal Mass,” p. 34).
c Absence of flow signals (CDS) in the dilated vena cava (transverse upper abdomen section) due to a high-grade metastatic stenosis above; no thrombosis.
32
Venectasia






















































Segmental dilatation of a vein may be physio- |
physiological engorgement of the left renal |
ated from Baker cyst, since in the latter case |
logical in nature or due to impaired outflow or |
vein when crossing the aorta. Venous aneur- |
there will be no color signal in color-flow Dop- |
anatomy: for example, a large vena cava lumen |
ysms, e. g., in the popliteal vein, presenting |
pler scanning (Fig.1.66, Fig.1.67). |
in adolescents, distended jugular veins, or |
with painful swelling may easily be differenti- |
|
1
Vena Cava, Veins
Fig. 1.66 Ectatic internal jugular vein: marked enlarge- |
Fig. 1.67 Presumed Baker cyst. VS = lesser saphenous |
ment, slow turbulent flow demonstrated by the blue- |
vein. |
red color signal; very low flow velocity (fixed low pulse |
a Presumed cyst (Z) in the popliteal fossa. |
repetition frequency, PRF, with corresponding maximum |
|
velocity of 6 cm/s). |
|
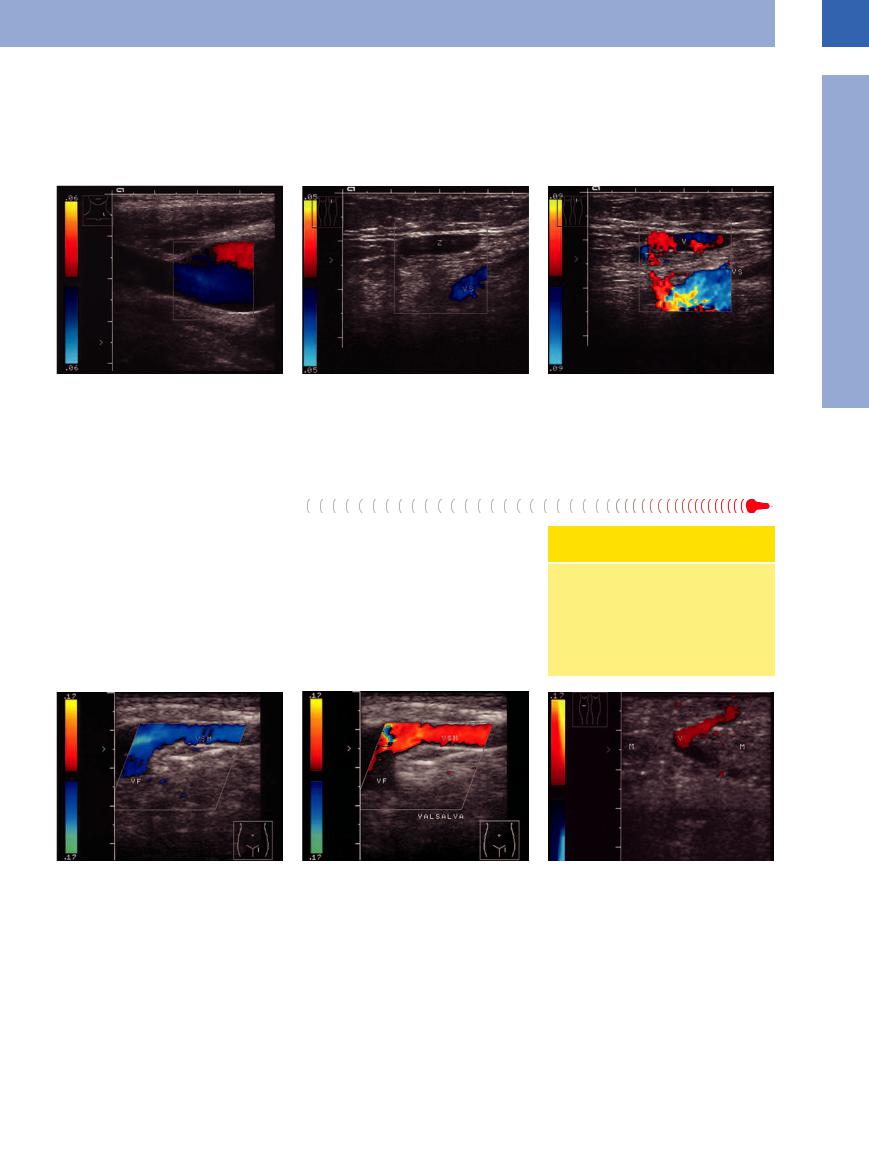
Venous Insufficiency 






Refluxing blood in a vein will lead to segmental dilatation, which in turn results in venous incompetence. Predisposed locations are:
●Saphenofemoral junction (“insufficient saphenous junction”)
●Saphenopopliteal junction (“insufficient parva junction”)
●Proximal femoral and popliteal vein
●Lower leg (varicosities, incompetent perforators)
The diagnosis is to be confirmed by color-flow Doppler scanning, and the severity can easily be graded according to the Hach classification16 (Fig.1.68, Fig.1.69).
b After extrinsic compression of the lower leg, color-flow Doppler evaluation detects venectasia (V) with proven incompetence of the saphenopopliteal junction.
Hach Classification of Greater Saphenous Insufficiency
●Stage I: Insufficient saphenous junction
●Stage II: Insufficient saphenous junction plus reflux to the distal thigh
●Stage III: Insufficient saphenous junction plus reflux to the proximal lower leg
Fig. 1.68 Incompetence of the saphenofemoral junction. a Junction of the enlarged greater saphenous vein (VSM) and the femoral vein (VF).
b Valsalva maneuver: color change from blue to red, confirming venous reflux.
Fig. 1.69 Incompetent Cockett perforators: venous runoff from the posterior tibial veins through the gastrocnemius muscle (M) to the superficial venous system.
33
