
- •Contents
- •Preface
- •Contributors
- •1 Vessels
- •1.1 Aorta, Vena Cava, and Peripheral Vessels
- •Aorta, Arteries
- •Anomalies and Variant Positions
- •Dilatation
- •Stenosis
- •Wall Thickening
- •Intraluminal Mass
- •Perivascular Mass
- •Vena Cava, Veins
- •Anomalies
- •Dilatation
- •Intraluminal Mass
- •Compression, Infiltration
- •1.2 Portal Vein and Its Tributaries
- •Enlarged Lumen Diameter
- •Portal Hypertension
- •Intraluminal Mass
- •Thrombosis
- •Tumor
- •2 Liver
- •Enlarged Liver
- •Small Liver
- •Homogeneous Hypoechoic Texture
- •Homogeneous Hyperechoic Texture
- •Regionally Inhomogeneous Texture
- •Diffuse Inhomogeneous Texture
- •Anechoic Masses
- •Hypoechoic Masses
- •Isoechoic Masses
- •Hyperechoic Masses
- •Echogenic Masses
- •Irregular Masses
- •Differential Diagnosis of Focal Lesions
- •Diagnostic Methods
- •Suspected Diagnosis
- •3 Biliary Tree and Gallbladder
- •3.1 Biliary Tree
- •Thickening of the Bile Duct Wall
- •Localized and Diffuse
- •Bile Duct Rarefaction
- •Localized and Diffuse
- •Bile Duct Dilatation and Intraductal Pressure
- •Intrahepatic
- •Hilar and Prepancreatic
- •Intrapancreatic
- •Papillary
- •Abnormal Intraluminal Bile Duct Findings
- •Foreign Body
- •The Seven Most Important Questions
- •3.2 Gallbladder
- •Changes in Size
- •Large Gallbladder
- •Small/Missing Gallbladder
- •Wall Changes
- •General Hypoechogenicity
- •General Hyperechogenicity
- •General Tumor
- •Focal Tumor
- •Intraluminal Changes
- •Hyperechoic
- •Hypoechoic
- •Nonvisualized Gallbladder
- •Missing Gallbladder
- •Obscured Gallbladder
- •4 Pancreas
- •Diffuse Pancreatic Change
- •Large Pancreas
- •Small Pancreas
- •Hypoechoic Texture
- •Hyperechoic Texture
- •Focal Changes
- •Anechoic Lesion
- •Hypoechoic Lesion
- •Isoechoic Lesion
- •Hyperechoic Lesion
- •Irregular (Complex Structured) Lesion
- •Dilatation of the Pancreatic Duct
- •Marginal/Mild Dilatation
- •Marked Dilatation
- •5 Spleen
- •Nonfocal Changes of the Spleen
- •Diffuse Parenchymal Changes
- •Large Spleen
- •Small Spleen
- •Focal Changes of the Spleen
- •Anechoic Mass
- •Hypoechoic Mass
- •Hyperechoic Mass
- •Splenic Calcification
- •6 Lymph Nodes
- •Peripheral Lymph Nodes
- •Head/Neck
- •Extremities (Axilla, Groin)
- •Abdominal Lymph Nodes
- •Porta Hepatis
- •Splenic Hilum
- •Mesentery (Celiac, Upper and Lower Mesenteric Station)
- •Stomach
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •Small/Large Intestine
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •8 Peritoneal Cavity
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Wall Structures
- •Smooth Margin
- •Irregular Margin
- •Intragastric Processes
- •Intraintestinal Processes
- •9 Kidneys
- •Anomalies, Malformations
- •Aplasia, Hypoplasia
- •Cystic Malformation
- •Anomalies of Number, Position, or Rotation
- •Fusion Anomaly
- •Anomalies of the Renal Calices
- •Vascular Anomaly
- •Diffuse Changes
- •Large Kidneys
- •Small Kidneys
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Irregular Structure
- •Circumscribed Changes
- •Anechoic Structure
- •Hypoechoic or Isoechoic Structure
- •Complex Structure
- •Hyperechoic Structure
- •10 Adrenal Glands
- •Enlargement
- •Anechoic Structure
- •Hypoechoic Structure
- •Complex Echo Structure
- •Hyperechoic Structure
- •11 Urinary Tract
- •Malformations
- •Duplication Anomalies
- •Dilatations and Stenoses
- •Dilated Renal Pelvis and Ureter
- •Anechoic
- •Hypoechoic
- •Hypoechoic
- •Hyperechoic
- •Large Bladder
- •Small Bladder
- •Altered Bladder Shape
- •Intracavitary Mass
- •Hypoechoic
- •Hyperechoic
- •Echogenic
- •Wall Changes
- •Diffuse Wall Thickening
- •Circumscribed Wall Thickening
- •Concavities and Convexities
- •12.1 The Prostate
- •Enlarged Prostate
- •Regular
- •Irregular
- •Small Prostate
- •Regular
- •Echogenic
- •Circumscribed Lesion
- •Anechoic
- •Hypoechoic
- •Echogenic
- •12.2 Seminal Vesicles
- •Diffuse Change
- •Hypoechoic
- •Circumscribed Change
- •Anechoic
- •Echogenic
- •Irregular
- •12.3 Testis, Epididymis
- •Diffuse Change
- •Enlargement
- •Decreased Size
- •Circumscribed Lesion
- •Anechoic or Hypoechoic
- •Irregular/Echogenic
- •Epididymal Lesion
- •Anechoic
- •Hypoechoic
- •Intrascrotal Mass
- •Anechoic or Hypoechoic
- •Echogenic
- •13 Female Genital Tract
- •Masses
- •Abnormalities of Size or Shape
- •Uterus
- •Abnormalities of Size or Shape
- •Myometrial Changes
- •Intracavitary Changes
- •Endometrial Changes
- •Fallopian Tubes
- •Hypoechoic Mass
- •Anechoic Cystic Mass
- •Solid Echogenic or Nonhomogeneous Mass
- •14 Thyroid Gland
- •Diffuse Changes
- •Enlarged Thyroid Gland
- •Small Thyroid Gland
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Circumscribed Changes
- •Anechoic
- •Hypoechoic
- •Isoechoic
- •Hyperechoic
- •Irregular
- •Differential Diagnosis of Hyperthyroidism
- •Types of Autonomy
- •15 Pleura and Chest Wall
- •Chest Wall
- •Masses
- •Parietal Pleura
- •Nodular Masses
- •Diffuse Pleural Thickening
- •Pleural Effusion
- •Anechoic Effusion
- •Echogenic Effusion
- •Complex Effusion
- •16 Lung
- •Masses
- •Anechoic Masses
- •Hypoechoic Masses
- •Complex Masses
- •Index
3
Biliary Tree and Gallbladder
3.2Gallbladder
C. Jakobeit
Anatomy























































Size
●Length 10 cm and diameter 4 cm (max.), when fasting
Shape
●Quite variable (depends on the constitution of the patient; also numerous variants)
●Fasting: ovoid, pear-shaped
●Visualization of fundus, body, and neck
Wall thickness
●Fasting 2–4 mm
●Postprandial 4–8 mm
●Wall single-layered when fasting, tri- ple-layered postprandially
The gallbladder is assessed according to criteria of location, size, shape, echogenicity, and intraluminal material.
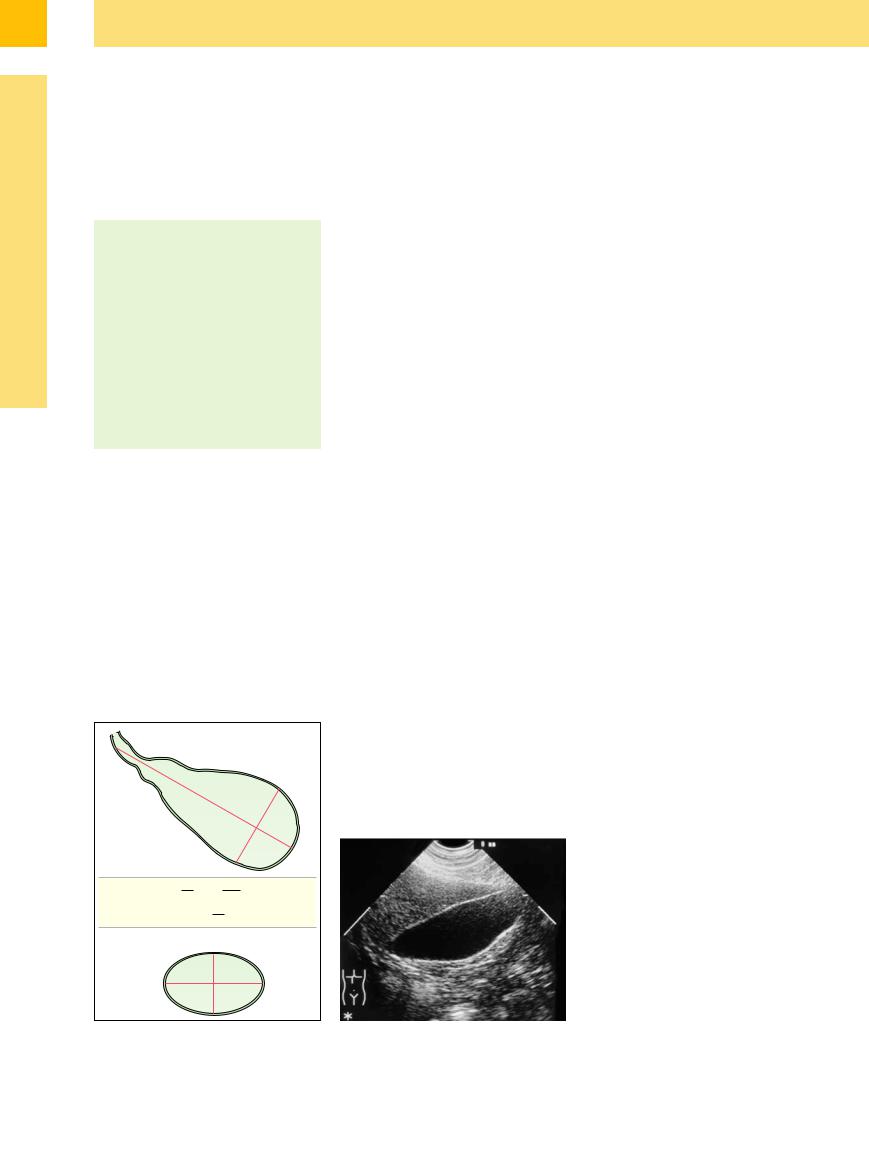
Size. Since the size of the gallbladder depends on its filling volume and on stimulation by the possible presence of food, it should be measured in the fasting state. The most reliable measurement of the length is obtained in the longitudinal view at the edge of the liver (in inspiration), while the subcostal oblique view (also in inspiration) yields the best measurement for the diameter. In healthy adults, the normal size of the gallbladder is up to 10 cm in
length and up to 4 cm in diameter. A postprandial study yields excellent results for gallbladder function: after stimulation the volume may be calculated as an ellipsoid of rotation: 0.5 × (length × width × height). The data for the volume measurements should be obtained 20, 40, and 60 minutes after stimulation by oral intake (Fig. 3.30). A healthy gallbladder empties at least 50% of its content after stimulation (study of healthy participants). If less than 30% of the filling volume is ejected the gallbladder is considered dysfunctional.
Shape. The shape of the gallbladder depends on the filling volume and thus varies widely. The shape and contour of the gallbladder are closely tied to the constitution of the patient and the state of filling of the adjacent organs (e. g., the intestines). With the patient fasting, the gallbladder is most often visualized as an ovoid or pear-shaped organ. Ultrasound can reasonably well delineate the anatomical divisions into fundus, body, and infundibulum. The wall of the gallbladder can easily be demonstrated as a single-layered lamina approximately 2–4 mm thick (Fig. 3.31). The wall in the fasting gallbladder will appear as a single layer because the gallbladder does not possess any true histological tunica submucosa and tunica muscularis. Postprandial contraction alters the appearance of the gallbladder wall to a triple layer (hyperechoic inner, hypoechoic
center, and hyperechoic outer layer), with a thickness that may be up to 4–8 mm (Fig. 3.32).
Variant shapes ( 3.5). The shape of the gallbladder is intimately tied to its degree of filling. The most important criterion denoting a healthy gallbladder is a wall smoothly and clearly demarcated from the hepatic fossa as well as the lumen. In many instances, precise measurements of the wall can only be taken on the hepatic side. Changes in shape and contour may be focal (more frequent) or diffuse. Posi- tion-induced foldover (
3.5). The shape of the gallbladder is intimately tied to its degree of filling. The most important criterion denoting a healthy gallbladder is a wall smoothly and clearly demarcated from the hepatic fossa as well as the lumen. In many instances, precise measurements of the wall can only be taken on the hepatic side. Changes in shape and contour may be focal (more frequent) or diffuse. Posi- tion-induced foldover ( 3.5a,b) will recede when being checked with the patient in a different position or while standing and can therefore be separated from true septation (
3.5a,b) will recede when being checked with the patient in a different position or while standing and can therefore be separated from true septation ( 3.5c–e).7 Most true septa are found in the neck and fundus, and the caplike septation in the latter is called a “Phrygian cap” (
3.5c–e).7 Most true septa are found in the neck and fundus, and the caplike septation in the latter is called a “Phrygian cap” ( 3.5f).
3.5f).
This region may be difficult to assess because of the proximity of the intestines. A subtle ultrasound study employing views of different orientation (during inspiration and after patient repositioning) is vital if any calculi hidden here are to be demonstrated. Tortuous or corkscrew-like gallbladders are known congenital variants ( 3.5 g). Multiple septa of the gallbladder are infrequent findings, and so are diverticula and doubling (
3.5 g). Multiple septa of the gallbladder are infrequent findings, and so are diverticula and doubling ( 3.5h). The congenital presence of two or more gallbladders is a rarity.
3.5h). The congenital presence of two or more gallbladders is a rarity.
Cystic duct. Demonstration of the cystic duct is easiest during deep inspiration (supine or left lateral decubitus). With subtle shifts of the probe, the cystic duct is visualized beginning from the infundibulum of the gallbladder. The distal segment of the cystic duct, most often joining the hepatic duct at the posterior aspect, is best demonstrated (by compression technique) with the patient supine in the plane through the porta hepatis, where it is anterior to the portal vein. The cuspidal junctional folds primarily found at the infundibulum are without pathology and are known as the spiral valve of Heister (Fig. 3.33). One frequently seen anatomical variant, the retroduodenal or intrapancreatic confluence into the CBD, is easily visible. Small hidden stones can be detected by good technique.8
Fig. 3.30 Calculation of the volume of the gallbladder. |
Fig. 3.31 Longitudinal section through a typical gallblad- |
|
der in the fasting state. The wall is well demarcated from |
|
the liver as a 2 mm single-layered lamina. |
146
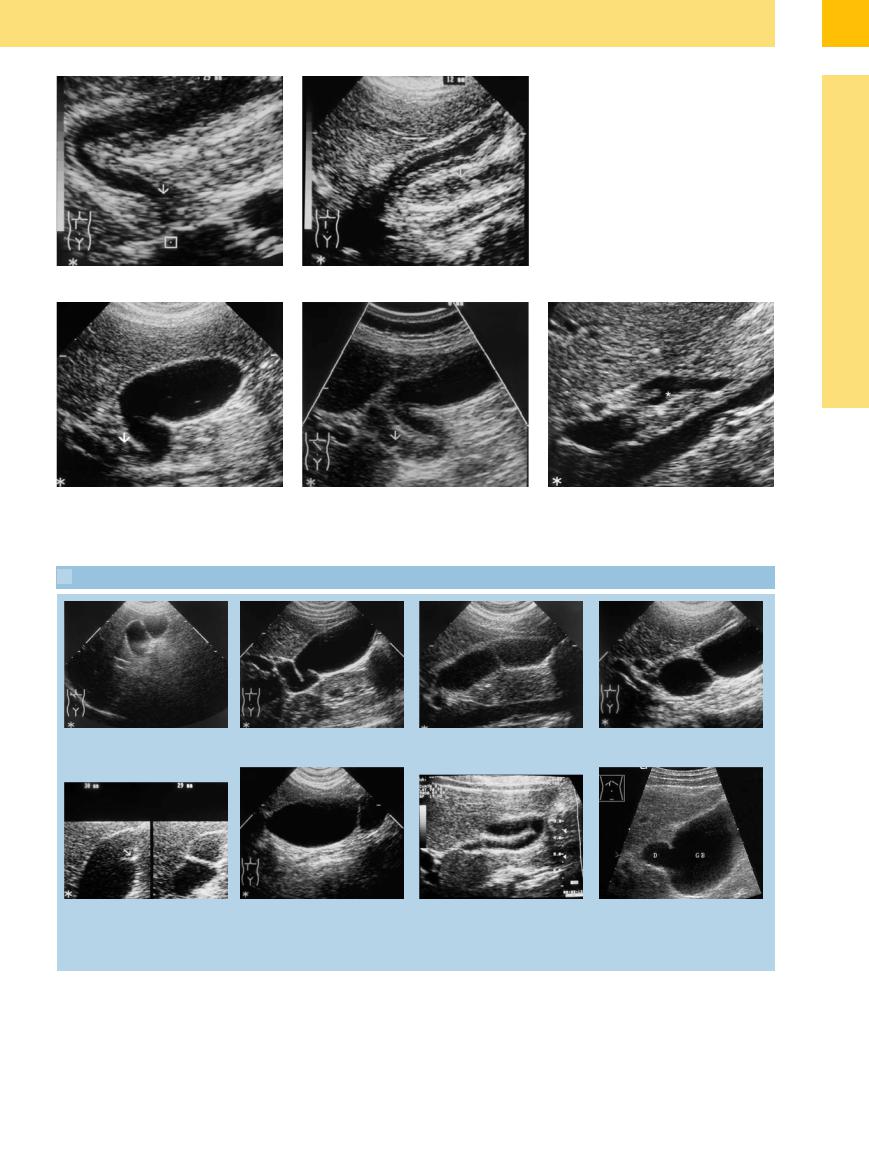
Fig. 3.32 Contracted gallbladder.
a Characteristic postprandial visualization.
b Checking the gallbladder function (after oral intake). Very well contracted, triple-layered postprandial wall, clearly demarcated from the liver and the lumen.
Fig. 3.33 Cystic duct. |
b Optimized visualization of the cystic duct with the |
c Junction of the cystic duct (*) at the posterior aspect of |
a Spiral valve of Heister at the junctional segment of the |
spiral valve of Heister. |
the common hepatic duct. |
cystic duct origin. |
|
|
 3.5 Variant Shapes of the Gallbladder
3.5 Variant Shapes of the Gallbladder
3
Gallbladder
a and b Foldover (pseudo-septation): an apparent septation in the body in the supine position is seen to be a normal demonstration in the left lateral decubitus position.
c and d True septation: even after repositioning the patient into the left lateral decubitus position, the septum in the neck of the gallbladder persists.
e Furrow: when supine (right), an appa- |
f Phrygian cap. |
rent septum in the body, which recedes |
|
almost completely in the left lateral de- |
|
cubitus position (left); now, only a slight |
|
furrow (arrow) with pseudoseptum re- |
|
mains. |
|
g Torsion and lateral displacement of the h Diverticula (D). GB = gallbladder. gallbladder
147
