
- •Contents
- •Preface
- •Contributors
- •1 Vessels
- •1.1 Aorta, Vena Cava, and Peripheral Vessels
- •Aorta, Arteries
- •Anomalies and Variant Positions
- •Dilatation
- •Stenosis
- •Wall Thickening
- •Intraluminal Mass
- •Perivascular Mass
- •Vena Cava, Veins
- •Anomalies
- •Dilatation
- •Intraluminal Mass
- •Compression, Infiltration
- •1.2 Portal Vein and Its Tributaries
- •Enlarged Lumen Diameter
- •Portal Hypertension
- •Intraluminal Mass
- •Thrombosis
- •Tumor
- •2 Liver
- •Enlarged Liver
- •Small Liver
- •Homogeneous Hypoechoic Texture
- •Homogeneous Hyperechoic Texture
- •Regionally Inhomogeneous Texture
- •Diffuse Inhomogeneous Texture
- •Anechoic Masses
- •Hypoechoic Masses
- •Isoechoic Masses
- •Hyperechoic Masses
- •Echogenic Masses
- •Irregular Masses
- •Differential Diagnosis of Focal Lesions
- •Diagnostic Methods
- •Suspected Diagnosis
- •3 Biliary Tree and Gallbladder
- •3.1 Biliary Tree
- •Thickening of the Bile Duct Wall
- •Localized and Diffuse
- •Bile Duct Rarefaction
- •Localized and Diffuse
- •Bile Duct Dilatation and Intraductal Pressure
- •Intrahepatic
- •Hilar and Prepancreatic
- •Intrapancreatic
- •Papillary
- •Abnormal Intraluminal Bile Duct Findings
- •Foreign Body
- •The Seven Most Important Questions
- •3.2 Gallbladder
- •Changes in Size
- •Large Gallbladder
- •Small/Missing Gallbladder
- •Wall Changes
- •General Hypoechogenicity
- •General Hyperechogenicity
- •General Tumor
- •Focal Tumor
- •Intraluminal Changes
- •Hyperechoic
- •Hypoechoic
- •Nonvisualized Gallbladder
- •Missing Gallbladder
- •Obscured Gallbladder
- •4 Pancreas
- •Diffuse Pancreatic Change
- •Large Pancreas
- •Small Pancreas
- •Hypoechoic Texture
- •Hyperechoic Texture
- •Focal Changes
- •Anechoic Lesion
- •Hypoechoic Lesion
- •Isoechoic Lesion
- •Hyperechoic Lesion
- •Irregular (Complex Structured) Lesion
- •Dilatation of the Pancreatic Duct
- •Marginal/Mild Dilatation
- •Marked Dilatation
- •5 Spleen
- •Nonfocal Changes of the Spleen
- •Diffuse Parenchymal Changes
- •Large Spleen
- •Small Spleen
- •Focal Changes of the Spleen
- •Anechoic Mass
- •Hypoechoic Mass
- •Hyperechoic Mass
- •Splenic Calcification
- •6 Lymph Nodes
- •Peripheral Lymph Nodes
- •Head/Neck
- •Extremities (Axilla, Groin)
- •Abdominal Lymph Nodes
- •Porta Hepatis
- •Splenic Hilum
- •Mesentery (Celiac, Upper and Lower Mesenteric Station)
- •Stomach
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •Small/Large Intestine
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •8 Peritoneal Cavity
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Wall Structures
- •Smooth Margin
- •Irregular Margin
- •Intragastric Processes
- •Intraintestinal Processes
- •9 Kidneys
- •Anomalies, Malformations
- •Aplasia, Hypoplasia
- •Cystic Malformation
- •Anomalies of Number, Position, or Rotation
- •Fusion Anomaly
- •Anomalies of the Renal Calices
- •Vascular Anomaly
- •Diffuse Changes
- •Large Kidneys
- •Small Kidneys
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Irregular Structure
- •Circumscribed Changes
- •Anechoic Structure
- •Hypoechoic or Isoechoic Structure
- •Complex Structure
- •Hyperechoic Structure
- •10 Adrenal Glands
- •Enlargement
- •Anechoic Structure
- •Hypoechoic Structure
- •Complex Echo Structure
- •Hyperechoic Structure
- •11 Urinary Tract
- •Malformations
- •Duplication Anomalies
- •Dilatations and Stenoses
- •Dilated Renal Pelvis and Ureter
- •Anechoic
- •Hypoechoic
- •Hypoechoic
- •Hyperechoic
- •Large Bladder
- •Small Bladder
- •Altered Bladder Shape
- •Intracavitary Mass
- •Hypoechoic
- •Hyperechoic
- •Echogenic
- •Wall Changes
- •Diffuse Wall Thickening
- •Circumscribed Wall Thickening
- •Concavities and Convexities
- •12.1 The Prostate
- •Enlarged Prostate
- •Regular
- •Irregular
- •Small Prostate
- •Regular
- •Echogenic
- •Circumscribed Lesion
- •Anechoic
- •Hypoechoic
- •Echogenic
- •12.2 Seminal Vesicles
- •Diffuse Change
- •Hypoechoic
- •Circumscribed Change
- •Anechoic
- •Echogenic
- •Irregular
- •12.3 Testis, Epididymis
- •Diffuse Change
- •Enlargement
- •Decreased Size
- •Circumscribed Lesion
- •Anechoic or Hypoechoic
- •Irregular/Echogenic
- •Epididymal Lesion
- •Anechoic
- •Hypoechoic
- •Intrascrotal Mass
- •Anechoic or Hypoechoic
- •Echogenic
- •13 Female Genital Tract
- •Masses
- •Abnormalities of Size or Shape
- •Uterus
- •Abnormalities of Size or Shape
- •Myometrial Changes
- •Intracavitary Changes
- •Endometrial Changes
- •Fallopian Tubes
- •Hypoechoic Mass
- •Anechoic Cystic Mass
- •Solid Echogenic or Nonhomogeneous Mass
- •14 Thyroid Gland
- •Diffuse Changes
- •Enlarged Thyroid Gland
- •Small Thyroid Gland
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Circumscribed Changes
- •Anechoic
- •Hypoechoic
- •Isoechoic
- •Hyperechoic
- •Irregular
- •Differential Diagnosis of Hyperthyroidism
- •Types of Autonomy
- •15 Pleura and Chest Wall
- •Chest Wall
- •Masses
- •Parietal Pleura
- •Nodular Masses
- •Diffuse Pleural Thickening
- •Pleural Effusion
- •Anechoic Effusion
- •Echogenic Effusion
- •Complex Effusion
- •16 Lung
- •Masses
- •Anechoic Masses
- •Hypoechoic Masses
- •Complex Masses
- •Index
8 Peritoneal Cavity
Peritoneal Cavity 295
|
|
|
Diffuse Changes |
298 |
||||||
|
|
|
||||||||
|
|
|
|
|
|
Anechoic Structure |
300 |
|||
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
Cirrhosis of the Liver |
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
Heart Failure |
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
Peritonitis |
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
Hypoalbuminemia |
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
Peritoneal Carcinomatosis |
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
Hemoperitoneum |
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
Ruptured Cyst |
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
Urinoma (Intraperitoneal) |
|
|
|
|
|
|
Hypoechoic Structure |
303 |
||||
|
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|
Pancreatitis |
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
Cirrhosis of the Liver with |
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
Spontaneous Bacterial |
|
|
|
|
|
|
|
|
|
|
Peritonitis (SBP) |
|
|
|
|
|
|
|
|
|
|
Peritoneal Carcinomatosis |
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
Purulent Peritonitis |
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
Tuberculosis |
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
Choleperitoneum |
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
Hemoperitoneum |
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
GI Tract Perforation |
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
Chyloperitoneum |
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
Pseudomyxoma Peritonei |
|
|
|
|
|
|
Hyperechoic Structure |
307 |
||||
|
|
|
|
|
|
|
|
|
Pneumoperitoneum |
|
|
|
Localized Changes |
308 |
|||||||
|
|
|||||||||
|
|
|
|
|
Anechoic Structure |
310 |
||||
|
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|
Septated Ascites |
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
Intra-abdominal Abscess |
|
|
|
|
|
|
Hypoechoic Structure |
310 |
||||
|
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|
Abscess |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Bilioma |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Hematoma |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Necrosis after Pancreatitis |
|
|
|
|
|
|
Hyperechoic Structure |
311 |
||||
|
|
|
|
|
|
|
|
|
Localized Perforation |
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
Gas Abscess |
|
|
|
Wall Structures |
312 |
|||||||
|
|
|||||||||
|
|
|
|
|
Smooth Margin |
312 |
||||
|
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|
Right-sided Heart Failure |
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
Cirrhosis |
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
Peritoneal Carcinomatosis |
|
|
|
|
|
|
Irregular Margin |
313 |
||||
|
|
|
|
|
|
|
|
|
Pancreatitis |
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
Peritonitis |
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
Peritoneal Carcinomatosis |
|
|
|
Differentiating Intraand |
|
|||||||
|
|
|
||||||||
|
|
Extraluminal GI Tract Fluid |
316 |
|||||||
|
|
|
|
|
Intragastric Processes |
316 |
||||
|
|
|
|
|
|
|
|
|
Gastric Outlet Obstruction |
|
|
|
|
|
|
Intraintestinal Processes |
317 |
||||
|
|
|
|
|
|
|
|
|
Duodenal Stenosis |
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
Small-bowel Obstruction |
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
Large-bowel Obstruction |
|

8Peritoneal Cavity
D. Nuernberg
Anatomy























































Definition
●Capillary space between the parietal and visceral peritoneum
Synonyms
●Peritoneal cavity
●Greater peritoneal cavity
●Intraperitoneal space
●Abdominal cavity
●Intra-abdominal space
The abdominal organs (viscera) are invested by a thin serous membrane, the so-called visceral peritoneum. Its continuation lining the ab-
dominal wall is known as the parietal peritoneum. The peritoneum continuously transudes serous fluid, thus enabling the organs lined by the visceral peritoneum to glide over each other. Since the peritoneum constantly reabsorbs this peritoneal fluid, imaging modalities cannot demonstrate any significant amount of fluid. Thus, the peritoneal cavity usually exists as a “peritoneal gap” and it is this space that can be visualized sonographically only in pathological conditions. A true space or cavity exists only if fluid or another substrate collects in the gap between the visceral and parietal peritoneum (intraperitoneal position).
Topography 





















































If an organ is completely invested by peritoneum it is called ‘intraperitoneal’ (e. g., stomach, spleen, liver, small intestine, transverse and sigmoid colon, ovaries). Retroperitoneal organs are the kidneys, adrenal glands, aorta, and vena cava. If only the anterior part of an organ is invested by peritoneum and otherwise it is directly fixed to the posterior abdominal wall, it is also regarded as being retroperitoneal (e. g., pancreas, descending part of the duodenum).
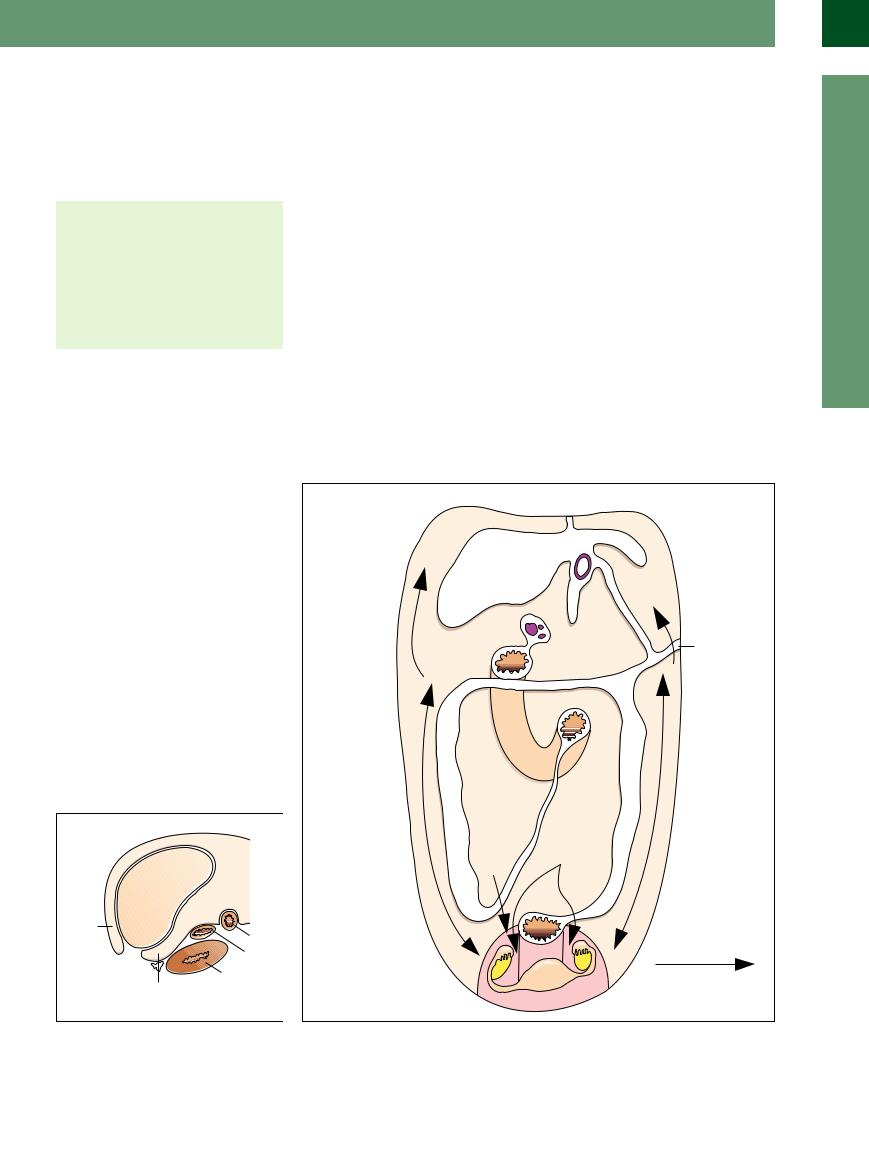
The reflections of the peritoneum divide it into different abdominal compartments (see Figs. 8.1, 8.2, 8.3, 8.4). The significance of these compartments becomes evident when the question arises whether there is diffuse fluid within the peritoneal cavity or if it only involves certain subspaces (e. g., in “trapped” ascites).
Intraperitoneal fluid may stem from hypersecretion or impaired absorption, e. g., when there is inflammation (peritonitis). This intraperitoneal fluid may also arise from injuries of fluid-filled organs, e. g., bleeding (hemoperitoneum) or perforation of the bile system (choleperitoneum) or the gastrointestinal (GI) tract. Another reason for these fluid collections may be pressure changes in the venous system (right-sided heart failure, portal hypertension). The peritoneal cavity may contain not only collections of fluid but also gas and solid matter.
8
Peritoneal Cavity
Fig. 8.2 Delineation and correlation of the longitudinal |
Fig. 8.1 Peritoneal reflections and the recesses thus created.8 |
recesses on the right side.8 |
|
295
8
Peritoneal Cavity
Fig. 8.3 Delineation and correlation of the longitudinal recesses in the midclavicular line.8
fFig. 8.4 Delineation and correlation of the transverse recesses.8
Ultrasound Morphology
Morphology
Ultrasonography of the Peritoneal
Cavity
●Sonographic accessibility
●Preferred localization for fluid and/or gas collections
●Classification as to intraperitoneal, extraperitoneal, and retroperitoneal location
●Retroperitoneal space
The peritoneum itself cannot be demonstrated by ultrasound since it does not have a large enough impedance gradient. However, in ultrasound studies of the viscera it seems to be an integral part of their boundary layers, e. g., the hepatic surfaces, the boundary layer between the liver and the right kidney, the splenic surfaces, and the inner lining of the abdominal wall, and therefore appears as a hyperechoic band investing the capsule of the organ. When the visceral relations change (e. g., between liver and right kidney) the “gliding” motion of the peritoneum becomes quite evident (Fig. 8.5).
Visualization of the peritoneal space implies the presence of pathology, but there is always an exception to the rule: in menstruating young women a scant amount of free fluid can be demonstrated in the retrouterine (Douglas) pouch. The same is true in patients after abdominal surgery.
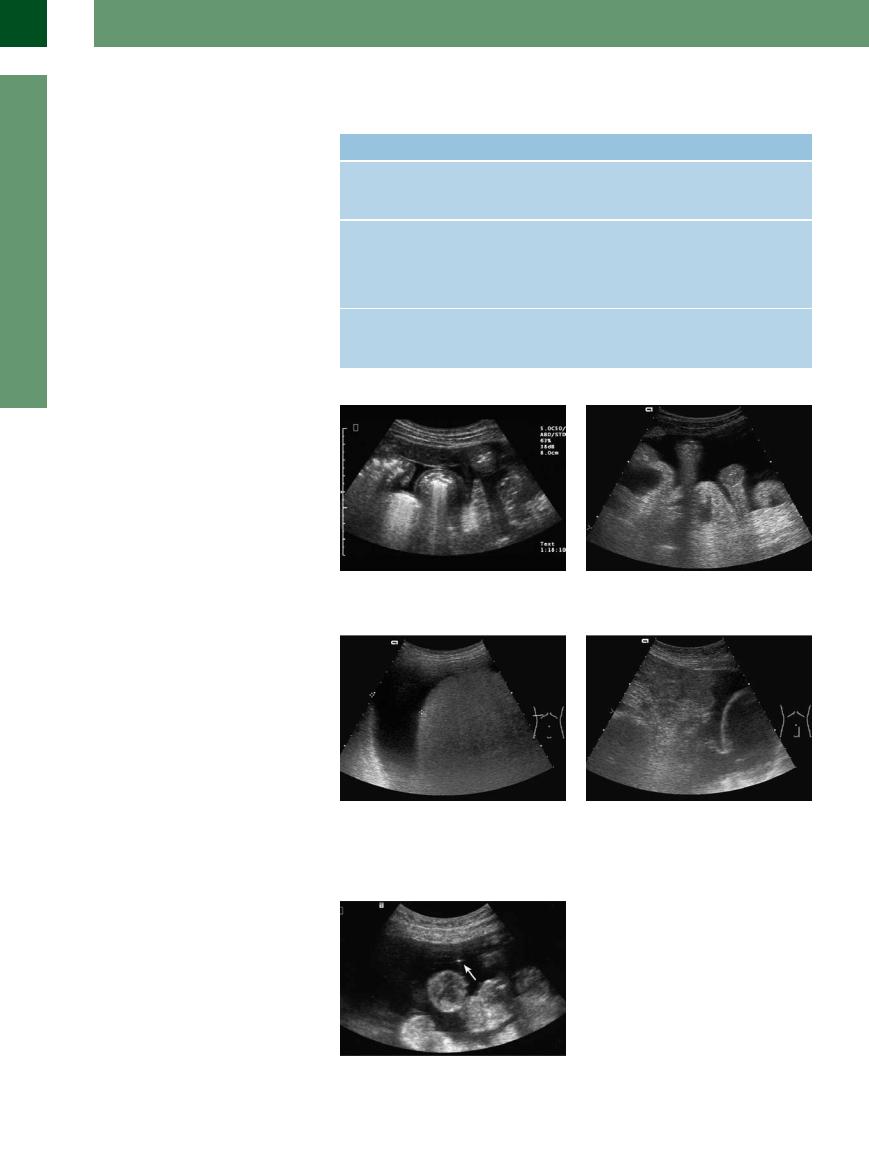
Fluid collections. Fluid collections are seen as anechoic/hypoechoic structures between the abdominal viscera. Owing to gravity, fluid will always collect in the dependent areas, i. e., in the posterior parts of the body while recumbent and in the lower abdomen while upright (Fig. 8.6).
Preferred localizations for fluid (anechoic/ hypoechoic) collections are ( 8.1a–f):
8.1a–f):
●Perihepatic right
●Perihepatic left
●Subhepatic right (between the right lobe of the liver and the right kidney = hepatorenal recess, Morrison’s pouch)
●Subphrenic
●Perisplenic
●Omental bursa
●Retrouterine pouch, perivesical
●Between the bowel loops (characteristic for ascites)
●Pericolic (“paracolic gutter”)
●Below the abdominal wall (knee–elbow position)
Gas collections. The accumulation of free in- tra-abdominal gas may result in the formation of hyperechoic structures. Physics dictates that gas will rise, and therefore it will be found in locations different from those for liquid, i. e., in the more superior regions such as the subphrenic recess (Fig. 8.7; see  8.1 g–i).
8.1 g–i).
Knowledge of these preferred localizations helps to identify substrates and recesses: when the patient is repositioned, liquid will gravitate to the more dependent parts of the abdominal cavity while gases will rise.
Extraperitoneal or intraperitoneal location.
Determination whether a formation is intraperitoneal, extraperitoneal, or retroperitoneal may be quite difficult. Visualization of the organ surfaces is the most decisive factor in this correlation; in the case of fluid collections in the gastrointestinal tract, precise correlation requires demonstration of the stomach or bowel wall.1 Differential diagnosis becomes especially problematic when the liquid or gas does not relocate upon patient repositioning. This repositioning does not produce any significant alterations in extraperitoneal and retroperitoneal formations.
Differentiating intraluminal air within the GI tract from hyperechoic intra-abdominal structures (gas collections) can become rather difficult ( 8.2a,b).
8.2a,b).
Retroperitoneal space. Here too this space as such may only be demonstrated by the organs it contains or by collections of foreign substrates such as fluid, gas, or solid tissue. The retroperitoneal space is delineated by correlating it with the retroperitoneal organs, e. g., the kidneys, large vessels, or pancreas ( 8.2c–h).2
8.2c–h).2
Fig. 8.5 The hyperechoic boundary between the right hepatic lobe and the right kidney (Morrison’s pouch, hepatorenal recess, subhepatic recess) is formed by the surfaces of these two viscera and the investing peritoneum.
Fig. 8.6 Anechoic collection of free fluid (e. g., hepatogenous ascites) within the peritoneal cavity, characterized by the bowel loops floating in the fluid.
Fig. 8.7 Gas collection as sequela of GI tract perforation.9 L = liver; K = kidney; S = spleen.
296
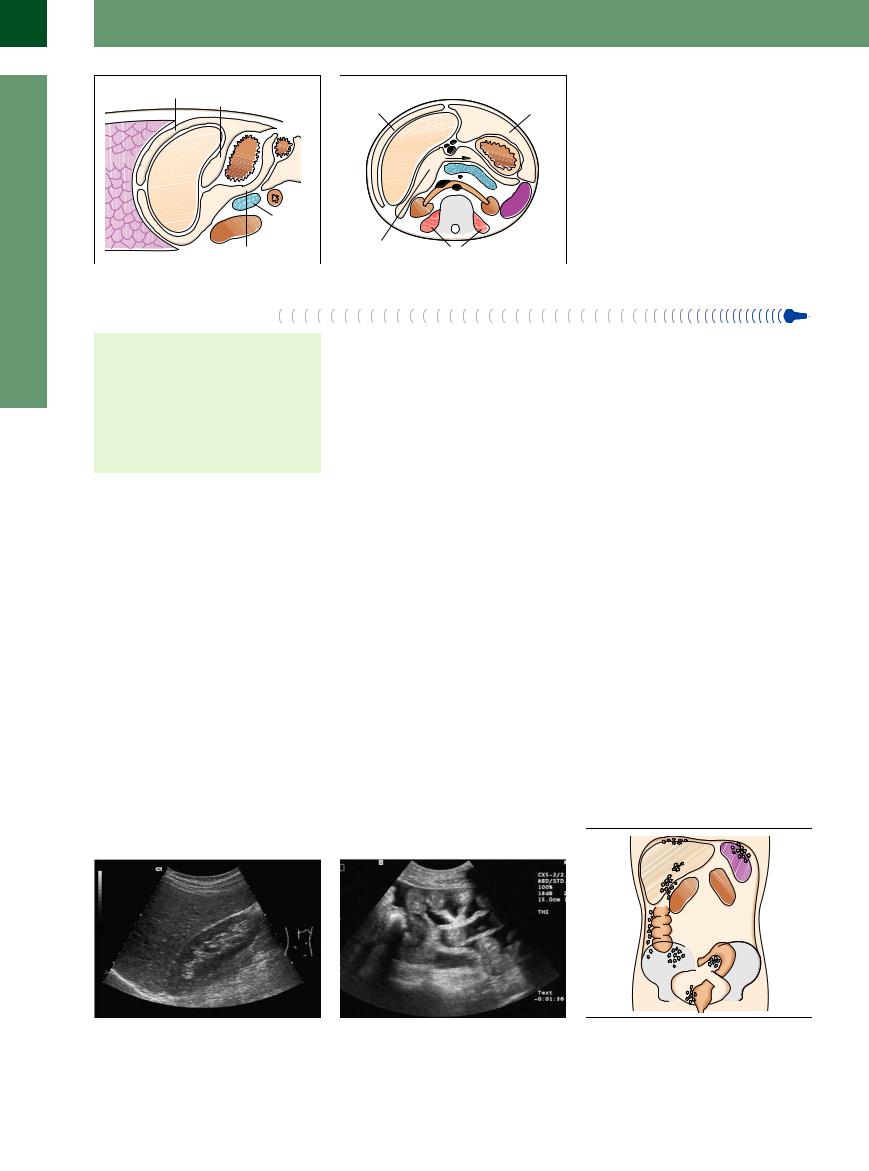
 8.1 Fluid and Gas Collections within the Peritoneal Cavity
8.1 Fluid and Gas Collections within the Peritoneal Cavity
Fluid collections
a Perihepatic: anechoic film anterior and lateral to the right hepatic lobe. Ascites due to alcoholic cirrhosis. The amount of ascites may be estimated by the thickness of the film.
d Perisplenic: anechoic film around the spleen, particularly at the hilum. In the presence of a very small amount of fluid only hypoechoic organ surfaces will be visualized.
b Morrison’s pouch (hepatorenal recess, subhepatic recess): already there is a small amount of free fluid, seen as an anechoic gap between the liver and kidney. Malignant ascites in ovarian cancer.
e Retrouterine pouch: in the lesser pelvis even minute amounts of fluid can be demonstrated. In this longitudinal plane the uterus is bathed by the fluid.
c Subhepatic: free fluid below the liver in the right transverse plane; ascites (transudate) in right cardiac failure. The hyperechoic delineation anterior to the kidney corresponds with the peritoneum plus the renal capsule.
f Interenteric: in the presence of large amounts of free intra-abdominal fluid the bowel loops float in the fluid and weave around like underwater creatures (“sea anemone phenomenon”).
Gas collections
g Hyperechoic intra-abdominal mass |
h Characteristic image of the hyperechoic |
i Gas collection inferior to the left hepatic |
caused by free air. Note the characteristic |
gas collection anterior to the left hepatic |
lobe; visible in the longitudinal plane and |
reverberations. |
lobe in the transverse plane, with the pa- |
posterior to the left hepatic lobe in the |
|
tient supine. The left hepatic lobe can be |
area around the perforation (duodenal |
|
seen between the “curtain” of free air. |
ulcer). |
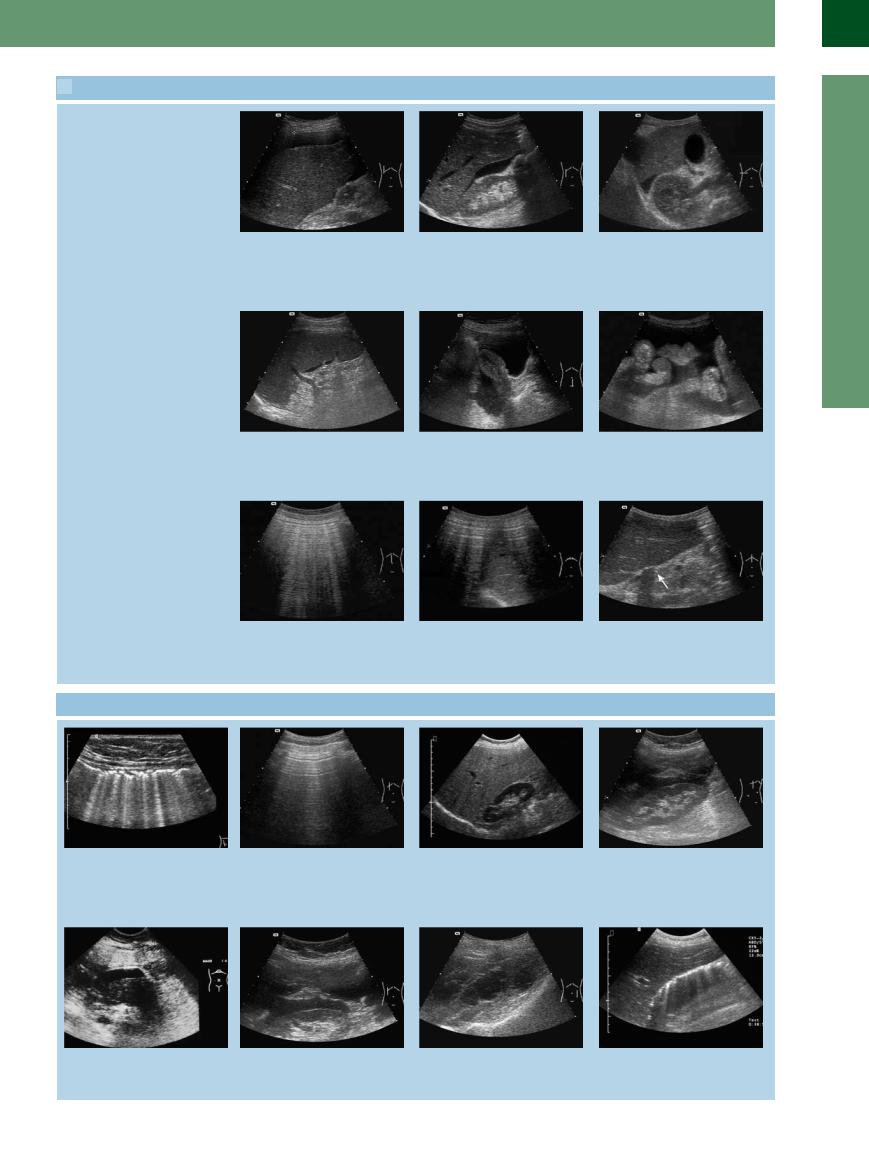
 8.2 Correlation of Extraperitoneal or Intraperitoneal Location
8.2 Correlation of Extraperitoneal or Intraperitoneal Location
8
Peritoneal Cavity
a Intraluminal air within the GI tract. Compared with the free air anterior to the reverberation artifacts, the multilayered bowel wall is demonstrated.
e Peripancreatic hypoechoic mass; fluid collection anterior to the head of the pancreas in acute hemorrhagic pancreatitis.
b In a free perforation, repositioning the patient will not yield any changes and the wall of the GI tract will not be visualized.
f Hypoechoic film enveloping the right kidney in retroperitoneal bile collection due to a lesion during endoscopy of the bile duct.
c The cardinal structures of the retroperitoneal space are its viscera, e. g., the kidneys.
g Inhomogeneous hypoechoic retroperitoneal mass on the left, particularly in the left psoas muscle: hematoma in coumarin anticoagulant overdosage.
d Intraperitoneal and retroperitoneal hypoechoic masses anterior to and around the right kidney in status post rupture of the bile duct, with bile leaking into the peritoneal cavity and the retroperitoneal space.
h Hyperechoic band anterior to the right kidneyandposterior tothegallbladderand duodenum: pneumoperitoneum due to retroperitoneal perforation during ERCP.
297
8
Peritoneal Cavity
■ Diffuse Changes
Diffuse intra-abdominal formations may either be anechoic, hypoechoic (echogenic), or hyperechoic (Table 8.1). Patient repositioning will alter the sonographic image of this diffuse distribution, an almost pathognomonic characteristic. The formation will change its location and can be visualized in different compartments.
Amount. The bigger the collection, the better this flowing effect will be seen. In anechoic substrates (fluid) a small volume of 5–10 mL can already be demonstrated, particularly within the subhepatic recess. Between the bowel loops (preferred localization of ascites) (Fig. 8.8) and within the retrouterine pouch very small amounts may also become visible, whereas an amount of about 700–1000 mL is required to become clinically detectable. When the collection is large (several hundred milliliters, or liters), if not all compartments then at least several compartments will be involved. The loops of the small intestine “floating” in the anechoic fluid are particularly impressive (so-called “sea anemone phenomenon,”
Fig. 8.9).
Determination of the volume involved can be fraught with problems. Some authors rely on the width of the right perihepatic film with the patient supine (1 cm = ca.1 L; 2 cm = 1.5 L; 3 cm = 2 L) (Fig. 8.10). When the patient is sitting or standing, the fluid will gravitate into the retrouterine pouch and the amount can be approximated by the ellipsoid method: 0.5 × h × w × l (Fig. 8.11). Rule-of-thumb approximation is more practicable than attempting to state an exact volume in milliliters or liters. Follow-up studies by one and the same sonographer have proved to be rather helpful and may sometimes determine the course of treatment.
Origin. The origin of peritoneal fluid collections (ascites) may be quite varied (Table 8.2). The rate at which a particular type of ascites is observed depends on the professional training of the sonographer and the patient population studied. In gastroenterology, ascites tends to be hepatogenic in origin; in oncology, malignant ascites prevails; in gynecology, ascites may be due to ovarian cancer or ectopic pregnancy; and in surgical emergencies, hemoperitoneum will be most common. The makeup of a patient population with ascites seen in a typical hospital is listed in Table 8.3.
The most important parameters for the differential diagnosis of intra-abdominal fluid are patient history, clinical signs, distribution of the fluid in the ultrasound study, sonographic morphology, and finally ultrasound-guided fine-needle paracentesis (Fig. 8.12).
Table 8.1 The echogenicity of diffusely distributed substrates |
|
||
Echogenicity |
Substrate |
Contents |
Translucency |
Anechoic |
Fluid |
Transudate |
Good translucency; surroundings |
|
|
Exudates |
can be assessed |
|
|
Blood (early phase) |
|
Hypoechoic |
Fluid |
Exudate |
Good translucency; surroundings |
(echogenic) |
|
Blood (late phase) |
can be assessed |
|
|
Bile |
|
|
|
Pus |
|
|
|
Chyle |
|
Hyperechoic |
Gas |
Gas/air |
No translucency; reverberation |
|
|
(pus + gas) |
artifacts; severely curtailed as- |
|
|
|
sessment of the surroundings |
Fig. 8.8 Minute fluid collection between the bowel loops (several milliliters) resembling an obtuse angle.
Fig. 8.10 When “guesstimating” the amount of free fluid, the distance between the surface of the liver and the lateral abdominal wall is a good marker.
Fig. 8.9 “Sea anemone phenomenon”: in the case of large amounts of diffusely distributed free fluid the bowel loops will float unencumbered in the fluid.
Fig. 8.11 The amount of free fluid in the lesser pelvis (retrouterine pouch) may also be “guesstimated” when viewed in the longitudinal plane. Since this is a dependent region of the body, even minute amounts of fluid can be detected here.
Fig. 8.12 Ultrasound-guided fine-needle paracentesis in the differential diagnosis of ascites. The tip of the needle is visible as a small echogenic structure (arrow) anterior to the bowel loops. Ultrasound guidance will help avoid injuries to intra-abdominal structures.
298
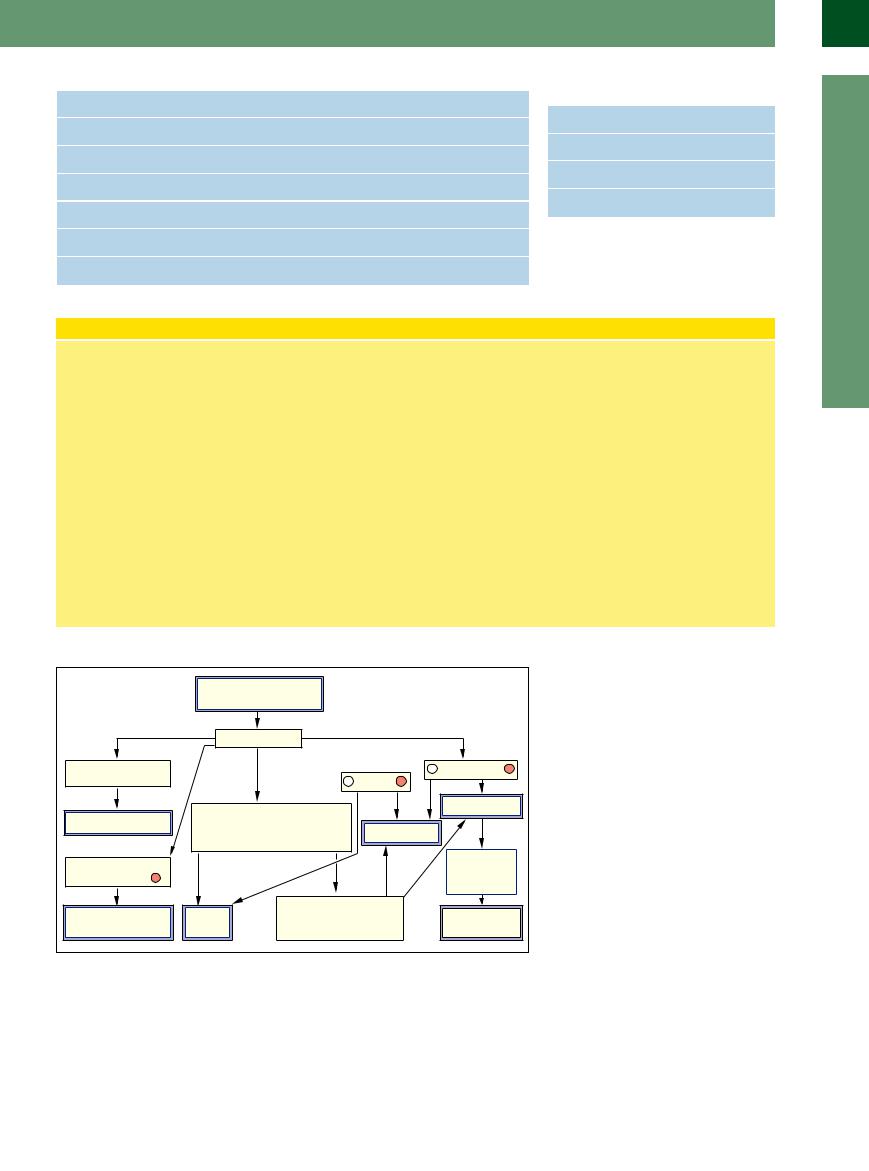
Table 8.2 Origin of intra-abdominal fluid collections (by organ) |
Table 8.3 Frequency of ascites sorted by origin |
||
Hepatogenic/portal |
Cirrhosis, portal vein thrombosis, Budd–Chiari syndrome |
(own patient population) |
|
|
|
||
Peritoneal |
Peritoneal carcinomatosis, peritonitis |
Cirrhosis |
30–50% |
|
|
||
Cardiac |
Right-sided heart failure |
Malignancy |
30–50% |
|
|
||
Pancreatogenous |
Acute/chronic pancreatitis |
Cardiac origin |
10–15% |
|
|
||
Ovarian |
Ectopic pregnancy, ovarian cancer |
Other origins |
10% |
|
|
||
Vascular |
Portal hypertension, ruptured vessel |
|
|
Chylous |
Lymphatic aplasia |
|
|
Ultrasound-guided (Fine-needle) Paracentesis
Quite often the clinical data and the patient’s history, supplemented by ultrasound morphology and the pattern of distribution, are not enough to confirm the precise type of ascites. Ultrasound-guided fine-needle paracentesis is an efficient and proven method with few potential complications that can help ascertain the final diagnosis. For diagnostic purposes it uses needles of up to 3 Fr (1 mm diameter, fine-needle). Larger needles are employed in therapeutic procedures.
Ultrasound targeting. Ultrasound targeting helps to avoid injury to vascular structures on the inside of the abdominal wall (e. g., internal caput medusae, Fig. 8.43b) as well as dry aspiration caused by the tip of the needle adhering to tissue. Furthermore,
it permits atypical needle insertion sites in the left lower quadrant (inverse McBurney’s point). Although any site may be selected, the distance to the target should be as short as possible and also should avoid any obstacles, such as the bowel, omentum, etc.
Laboratory studies. If fluid can be aspirated, thus confirming the suspected ultrasound diagnosis of “free fluid,” it first undergoes gross examination; this will allow the ascites to be classified as transudate/exudate, blood, bile, pus, urine, or chyle. Then the liquid substrate is subjected to additional cytological, bacteriological, and other laboratory studies.
One aspiration is enough for the laboratory panel, but in the case of peritoneal carcino-
matosis cytology sometimes requires several aspirations and work-ups. The sensitivity depends directly on the number of aspirations. If a malignant fluid collection is suspected clinically and the cytology is negative, the fine-needle aspiration has to be repeated. For differential diagnosis, the following laboratory parameters are cardinal
findings:3 |
|
Protein |
↑in exudate |
Amylase, lipase |
↑in pancreatogenous |
|
ascites |
Hemoglobin |
↑in status post bleeding |
Granulocytes |
↑in peritonitis |
Cholesterol |
↑in malignant ascites |
Tumor cells |
↑in malignant ascites |
Bacteria |
↑in peritonitis |
Fig. 8.13 Algorithm for differentiating ascites by diagnostic paracentesis.10
Figure 8.13 illustrates an algorithm for the differential diagnosis in ascites, based on diagnostic paracentesis.
The differential diagnosis of fluid collections within the peritoneal cavity is quite varied; an overview is given in Table 8.4.
8
Diffuse Changes
299
