- •Contents
- •Preface
- •Contributors
- •1 Vessels
- •1.1 Aorta, Vena Cava, and Peripheral Vessels
- •Aorta, Arteries
- •Anomalies and Variant Positions
- •Dilatation
- •Stenosis
- •Wall Thickening
- •Intraluminal Mass
- •Perivascular Mass
- •Vena Cava, Veins
- •Anomalies
- •Dilatation
- •Intraluminal Mass
- •Compression, Infiltration
- •1.2 Portal Vein and Its Tributaries
- •Enlarged Lumen Diameter
- •Portal Hypertension
- •Intraluminal Mass
- •Thrombosis
- •Tumor
- •2 Liver
- •Enlarged Liver
- •Small Liver
- •Homogeneous Hypoechoic Texture
- •Homogeneous Hyperechoic Texture
- •Regionally Inhomogeneous Texture
- •Diffuse Inhomogeneous Texture
- •Anechoic Masses
- •Hypoechoic Masses
- •Isoechoic Masses
- •Hyperechoic Masses
- •Echogenic Masses
- •Irregular Masses
- •Differential Diagnosis of Focal Lesions
- •Diagnostic Methods
- •Suspected Diagnosis
- •3 Biliary Tree and Gallbladder
- •3.1 Biliary Tree
- •Thickening of the Bile Duct Wall
- •Localized and Diffuse
- •Bile Duct Rarefaction
- •Localized and Diffuse
- •Bile Duct Dilatation and Intraductal Pressure
- •Intrahepatic
- •Hilar and Prepancreatic
- •Intrapancreatic
- •Papillary
- •Abnormal Intraluminal Bile Duct Findings
- •Foreign Body
- •The Seven Most Important Questions
- •3.2 Gallbladder
- •Changes in Size
- •Large Gallbladder
- •Small/Missing Gallbladder
- •Wall Changes
- •General Hypoechogenicity
- •General Hyperechogenicity
- •General Tumor
- •Focal Tumor
- •Intraluminal Changes
- •Hyperechoic
- •Hypoechoic
- •Nonvisualized Gallbladder
- •Missing Gallbladder
- •Obscured Gallbladder
- •4 Pancreas
- •Diffuse Pancreatic Change
- •Large Pancreas
- •Small Pancreas
- •Hypoechoic Texture
- •Hyperechoic Texture
- •Focal Changes
- •Anechoic Lesion
- •Hypoechoic Lesion
- •Isoechoic Lesion
- •Hyperechoic Lesion
- •Irregular (Complex Structured) Lesion
- •Dilatation of the Pancreatic Duct
- •Marginal/Mild Dilatation
- •Marked Dilatation
- •5 Spleen
- •Nonfocal Changes of the Spleen
- •Diffuse Parenchymal Changes
- •Large Spleen
- •Small Spleen
- •Focal Changes of the Spleen
- •Anechoic Mass
- •Hypoechoic Mass
- •Hyperechoic Mass
- •Splenic Calcification
- •6 Lymph Nodes
- •Peripheral Lymph Nodes
- •Head/Neck
- •Extremities (Axilla, Groin)
- •Abdominal Lymph Nodes
- •Porta Hepatis
- •Splenic Hilum
- •Mesentery (Celiac, Upper and Lower Mesenteric Station)
- •Stomach
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •Small/Large Intestine
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •8 Peritoneal Cavity
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Wall Structures
- •Smooth Margin
- •Irregular Margin
- •Intragastric Processes
- •Intraintestinal Processes
- •9 Kidneys
- •Anomalies, Malformations
- •Aplasia, Hypoplasia
- •Cystic Malformation
- •Anomalies of Number, Position, or Rotation
- •Fusion Anomaly
- •Anomalies of the Renal Calices
- •Vascular Anomaly
- •Diffuse Changes
- •Large Kidneys
- •Small Kidneys
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Irregular Structure
- •Circumscribed Changes
- •Anechoic Structure
- •Hypoechoic or Isoechoic Structure
- •Complex Structure
- •Hyperechoic Structure
- •10 Adrenal Glands
- •Enlargement
- •Anechoic Structure
- •Hypoechoic Structure
- •Complex Echo Structure
- •Hyperechoic Structure
- •11 Urinary Tract
- •Malformations
- •Duplication Anomalies
- •Dilatations and Stenoses
- •Dilated Renal Pelvis and Ureter
- •Anechoic
- •Hypoechoic
- •Hypoechoic
- •Hyperechoic
- •Large Bladder
- •Small Bladder
- •Altered Bladder Shape
- •Intracavitary Mass
- •Hypoechoic
- •Hyperechoic
- •Echogenic
- •Wall Changes
- •Diffuse Wall Thickening
- •Circumscribed Wall Thickening
- •Concavities and Convexities
- •12.1 The Prostate
- •Enlarged Prostate
- •Regular
- •Irregular
- •Small Prostate
- •Regular
- •Echogenic
- •Circumscribed Lesion
- •Anechoic
- •Hypoechoic
- •Echogenic
- •12.2 Seminal Vesicles
- •Diffuse Change
- •Hypoechoic
- •Circumscribed Change
- •Anechoic
- •Echogenic
- •Irregular
- •12.3 Testis, Epididymis
- •Diffuse Change
- •Enlargement
- •Decreased Size
- •Circumscribed Lesion
- •Anechoic or Hypoechoic
- •Irregular/Echogenic
- •Epididymal Lesion
- •Anechoic
- •Hypoechoic
- •Intrascrotal Mass
- •Anechoic or Hypoechoic
- •Echogenic
- •13 Female Genital Tract
- •Masses
- •Abnormalities of Size or Shape
- •Uterus
- •Abnormalities of Size or Shape
- •Myometrial Changes
- •Intracavitary Changes
- •Endometrial Changes
- •Fallopian Tubes
- •Hypoechoic Mass
- •Anechoic Cystic Mass
- •Solid Echogenic or Nonhomogeneous Mass
- •14 Thyroid Gland
- •Diffuse Changes
- •Enlarged Thyroid Gland
- •Small Thyroid Gland
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Circumscribed Changes
- •Anechoic
- •Hypoechoic
- •Isoechoic
- •Hyperechoic
- •Irregular
- •Differential Diagnosis of Hyperthyroidism
- •Types of Autonomy
- •15 Pleura and Chest Wall
- •Chest Wall
- •Masses
- •Parietal Pleura
- •Nodular Masses
- •Diffuse Pleural Thickening
- •Pleural Effusion
- •Anechoic Effusion
- •Echogenic Effusion
- •Complex Effusion
- •16 Lung
- •Masses
- •Anechoic Masses
- •Hypoechoic Masses
- •Complex Masses
- •Index
Alveolar Hydatid Disease 




Infection with Echinococcus multilocularis yields images similar to invasive tumor growth and cannot be distinguished from a malignancy by sonography alone (Table 2.15).
Table 2.15 Alveolar hydatid disease. Sonographic classification after Wechsler and Kern7
Stage Characteristics
ICircumscribed inhomogeneous changes in the liver; ill-defined margin; mostly hyperechoic with a hypoechoic rim; calcification; no invasion of the portal vein, bile ducts, and hepatic veins
IIAppearance of hypoechoic cystic areas with ill-defined margins; invasion of bile ducts, branches of the portal vein, and hepatic veins; increasing calcification
IIIMarked infiltration of the liver with complications due to invasion of bile ducts and vessels; extensive calcification at the inhomogeneities; increasingly cystic hypoechoic areas
IV Crossing the organ boundary of the liver and invasion of the porta hepatis, diaphragm, retroperitoneum, head of the pancreas, and the duodenum
Liver Injuries in Multiple Trauma
in Multiple Trauma










































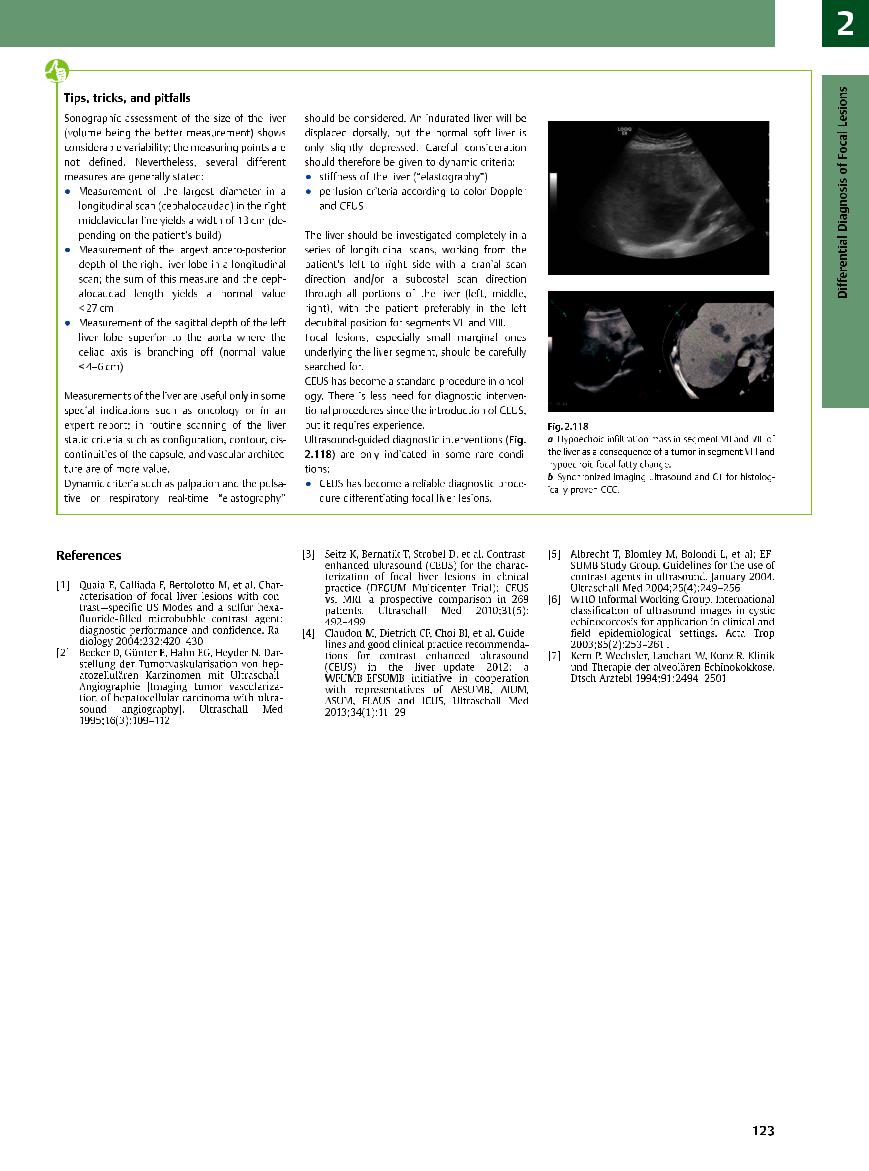
Direct destruction in multiple trauma, fresh and later older bleedings and postoperative results can be seen in the liver. Often only a limited evaluation can be made by B-mode ultrasonography. A further assessment by CEUS is frequently needed (Fig. 2.116, Fig. 2.117).
Fig. 2.116 Polytrauma, 4th postoperative day; patient in |
Fig. 2.117 Same polytrauma patient as in Fig. 2.116, |
intensive care with liver insufficiency. |
CEUS: large areas in the liver demonstrate nonenhance- |
|
ment as a sign of hemorrhage or necrosis. |
■ Differential Diagnosis of Focal Lesions
Diagnostic Methods
Liver

Diffuse Changes in Hepatic
Parenchyma
Localized Changes in Hepatic
Parenchyma
Differential Diagnosis of Focal Lesions
Diagnostic Methods
Suspected Diagnosis
Ultrasonography
CT
MRI
PET
Scintigraphy
Laparoscopy
Needle Biopsy
Angiography
Apart from the patient’s history, clinical findings, and laboratory parameters, the differential diagnosis of focal liver lesions can draw on other technical modalities that permit study of the mass either directly by cytology/histology and function testing, or indirectly by diagnostic imaging. The importance of each modality depends not only on its physical/technical limits
but, owing to rapid technical advances, also on the model of the equipment used, the actual performance of the study, and the personal expertise of the clinician. It is essential to regard the different diagnostic modalities as being complementary rather than rivals, and to employ them as efficiently as possible to maximize the return for the patient. The im-
portance of diagnostic ultrasound increases considerably by using contrast agents.
Undoubtedly, abdominal sonography is the imaging modality of choice in the detection and diagnosis of hepatic disorders. Not only is it the most widely available alternative of all the imaging modalities, but it can be performed at any time, with a high degree of sensitivity
2
Differential Diagnosis of Focal Lesions
119

2
Liver
Alternative Modalities in the Differential Diagnosis of Focal Liver Lesions
Ultrasonography. Routine abdominal sonography may be supplemented by special ultrasound techniques that can help in the further diagnosis of a mass; primarily, this would involve CEUS and qualitative and quantitative studies of the vascularization of the lesion, as well as the various possibilities of guided-needle biopsy and intervention.3 In comparison to competing imaging methods, abdominal sonography has the highest spatial resolution and the advantage of “real-time” imaging.
CT. The primary drawback of abdominal CT scanning is radiation exposure; furthermore, it only permits static cross-sectional images. Its advantages over ultrasonography are in terms of documentation, its standardized presentation of findings in any virtual computed plane, and the imaging of masses in locations that might be hard to study by ultrasound (subphrenic, in massive obesity, etc.). The limits of detection are about the same in both modalities. The sensitivity of each method in detecting focal liver lesions is about 90%, but if both modalities are combined the figure reaches almost 100%.
MRI. The most rapid advances in the imaging of focal liver lesions have taken place in
the field of MRI. Its significance lies in the use of specific contrast agents for analysis, despite its low spatial resolution. Because of the significant cost and resource implications and its lack of widespread availability, MRI is not regarded as a primary imaging modality but rather as an important adjunct in the specific differential diagnosis of lesions detected by routine sonography.3 Suspected hemangiomas lend themselves particularly well to confirmation by MRI.
For detecting focal liver lesions sonography, CT and MRI alone have a sensitivity of over 90%. In combination the sensitivity reaches almost 100%.
PET. The importance of PET in the diagnostic armamentarium remains the subject of clinical studies; at present, it cannot be regarded as a routine measure and is not widely available.
Scintigraphy. Because of the significant logistics and radiation exposure involved, scintigraphic studies are also regarded as second-line options. However, there is an indication for blood-pool scintigraphy when it comes to confirming focal lesions suspected of being hemangiomas. The same holds true for the diagnosis of FNH
by hepatobiliary scintiscan (HIDA scan), which specifically detects the proliferating bile ducts of this disorder.
Laparoscopy. Laparoscopy is a minimally invasive procedure that permits a better assessment of the hepatic surface than any other method, precise guided biopsy of circumscribed lesions, and, with the option of an ultrasound scanner, a high-reso- lution study of the liver. It is used primarily for unknown diffuse disorders of the parenchyma, and in the preoperative work-up of malignant disease when the transabdominal ultrasound finding is negative.
Needle biopsy with cytology/histology/ bacterial culture. Needle biopsy is always an invasive procedure and can only be justified after one of the imaging methods listed above has been used and if it might lead to changes in the treatment—in which case it becomes a necessity.
Angiography. Today, angiography does not play any primary role in the diagnostic work-up of the liver. It is of limited value in the preoperative assessment of hepatic lesions or in transcatheter arterial chemoembolization (TACE).
and specificity, it does not endanger the pa- |
sonographic diagnosis, it has to be supple- |
cost; its invasiveness and the stress/danger |
tient, and it can be repeated as often as needed. |
mented by other specific diagnostic methods. |
for the patient should also be considered. |
With the advent of CEUS, abdominal sonogra- |
The actual application of each modality de- |
Therefore, the differential diagnostic aspects |
phy is at least equal in sensitivity and specific- |
pends not only on the indication and issue at |
of the various modalities summarized above |
ity to other imaging methods such as CT or MRI. |
hand but to a large extent also on its availabil- |
cannot hope to be exhaustive; they are listed |
However, since not all lesions are amenable to |
ity, expenditure of diagnostic resources, and |
only in terms of their importance as supple- |
|
|
mentary measures to diagnostic ultrasound. |
120
Suspected Diagnosis
|
|
|
Diffuse Changes in Hepatic |
|
Liver |
Parenchyma |
|||
|
|
|
||
|
|
|
|
|
|
|
|
Localized Changes in Hepatic |
|
|
|
|
||
|
|
|
Parenchyma |
|
|
|
|
|
Differential Diagnosis of Focal Lesions |
|
|
|
|
|
|
|
|
|
Diagnostic Methods |
|
|
|
|
Suspected Diagnosis |
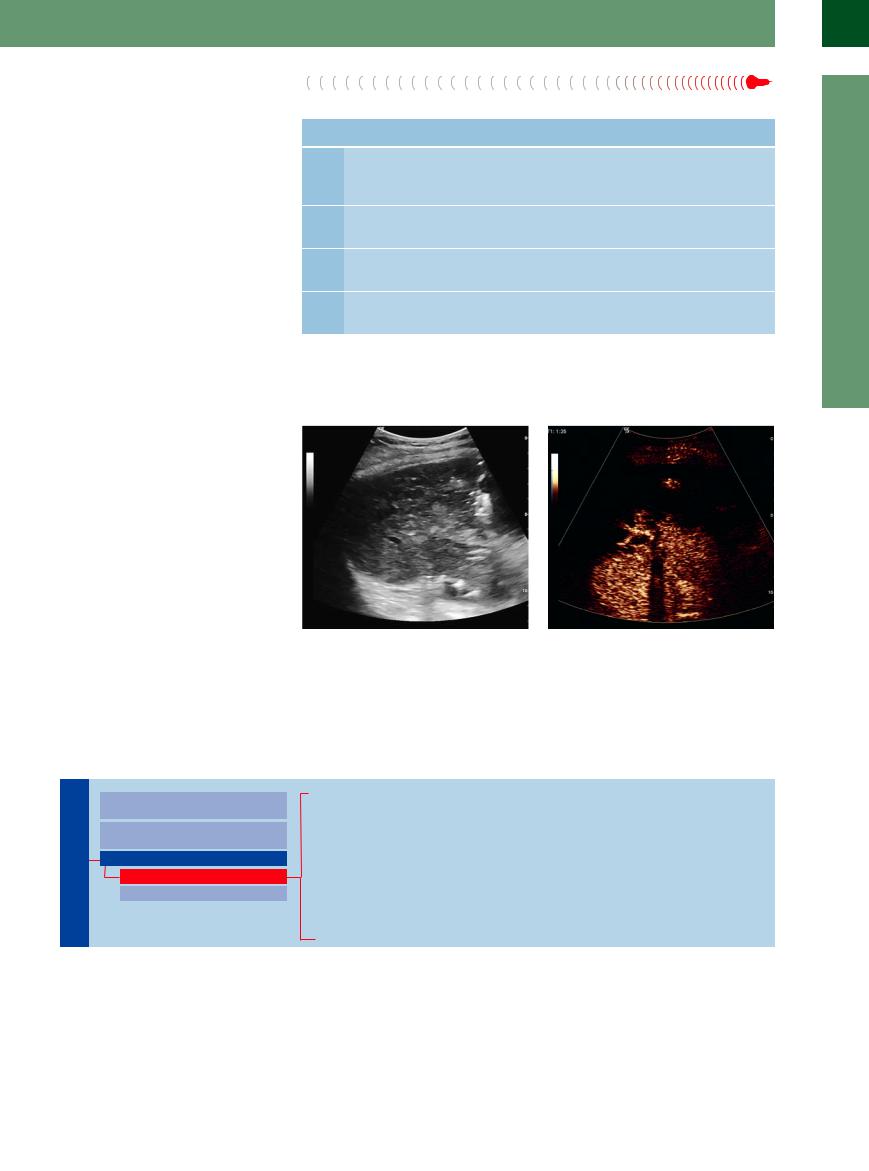
If the sonographic findings are tentative, the sonographer has the following options to confirm or rule out the suspected diagnosis. Table 2.16 summarizes the significance of the various diagnostic modalities.
Hemangioma. If contrast enhancement is available, it can be used during the same study to demonstrate the typical peripheral nodular enhancement and the so-called filling-in phenomenon by color-flow Doppler scanning, or the pooling of the contrast agent within the hemangioma by other imaging techniques (e. g., SAE). The filling-in phenomenon is the basis for detecting hemangiomas by CT angiography as well. In MRI, hemangiomas are characterized by their typical behavior in T1and T2-weighted sequences. The pooling of tracermarked red blood cells is the basis for confirming a hemangioma by blood-pool scintiscanning.
Since hemangiomas are prone to hemorrhaging, they should not be needle-biopsied. Unknown lesions breaking the surface of the liver should be needle-biopsied in such a fashion that the canal passes through a thick enough stretch of normal hepatic parenchyma. One characteristic of hemangiomas is a gush of blood on aspiration.
Focal nodular hyperplasia. The diagnosis of FNH is based on its architecture, with a thick vascular pedicle, central stellate scar and radiating fibrous septa, thick central blood vessel, and radial centrifugal blood flow as well as mulberry-like vascular tree. These characteristics are easily demonstrated by abdominal color-flow Doppler imaging (improved by contrast enhancement), CEUS, CT angiography, and special MRI studies.
FNH is confirmed by HIDA scanning since the tracer is secreted into the bile ducts, whose detectable presence is pathognomonic for this disease (compared to adenoma, HCC, and metastasis).
Needle biopsy requires a tissue cylinder of sufficient diameter; the procedure should allow for the hypervascular nature of this tumor (possible hemorrhage), which is characterized by its firm consistency.
Hemangioma
Focal Nodular Hyperplasia
Hepatocellular Carcinoma
Metastasis
Table 2.16 The importance of additional diagnostic modalities |
|
|
Suspected |
Additional diagnostic modality |
Importance |
sonographic |
|
|
diagnosis |
|
|
Hemangioma |
Contrast-enhanced color-flow Doppler imaging and CEUS |
+++ |
|
MRI |
+++ |
|
Blood-pool scintigraphy |
++ |
|
CT angiography |
++ |
|
Caution: needle biopsy |
|
FNH |
Contrast-enhanced color-flow Doppler imaging and CEUS |
+++ |
|
Hepatobiliary BIDA imaging |
++ |
|
CT |
++ |
|
MRI |
++ |
|
Needle biopsy |
+ |
HCC |
Contrast-enhanced color-flow Doppler imaging and CEUS |
+++ |
|
MRI |
+++ |
|
Needle biopsy |
+++ |
Metastasis |
Contrast-enhanced sonography with contrast harmonic |
+++ |
|
imaging (CHI) |
+++ |
|
Needle biopsy |
|
BIDA = bile intraductal aspiration.
Hepatocellular carcinoma. Any focal mass in a cirrhotic liver should be suspected of HCC and calls for further work-up and confirmation by ultrasound-guided needle biopsy (but only if it results in clinical consequences for the patient).
Noninvasive color-flow Doppler scanning may be able to demonstrate vascular invasion of the tumor or its bizarre irregular hypervascularization. CEUS demonstrates the typical bizarre early arterial vascularization in HCC. In addition, poorly differentiated tumor cells have a rapid wash-out effect compared to the surrounding parenchyma in the parenchymal phase.
After the application of specific contrast agents HCC is delineated by its filling defect on gadolinium-enhanced MRI.
Metastasis ( 2.14). Numerous proven methods can detect hepatic metastases, including transabdominal ultrasound (CEUS is particu-
2.14). Numerous proven methods can detect hepatic metastases, including transabdominal ultrasound (CEUS is particu-
larly effective) and the equally effective modalities of CT and MRI. Laparoscopy is the method of choice in the detection of small superficial metastases since it outperforms all other measures. At this time, typing a metastasis in terms of its primary can only be achieved by cytology/ histology. However, confirmation by ultra- sound-guided needle biopsy after color-flow Doppler study is called for only if it would result in clinical consequences. The canal of the biopsy should always run through a stretch of healthy parenchyma long enough to prevent hemorrhage. Lesions with a sonographic halo sign should be biopsied at the hypoechoic rim.
2
Differential Diagnosis of Focal Lesions
121
2
Liver
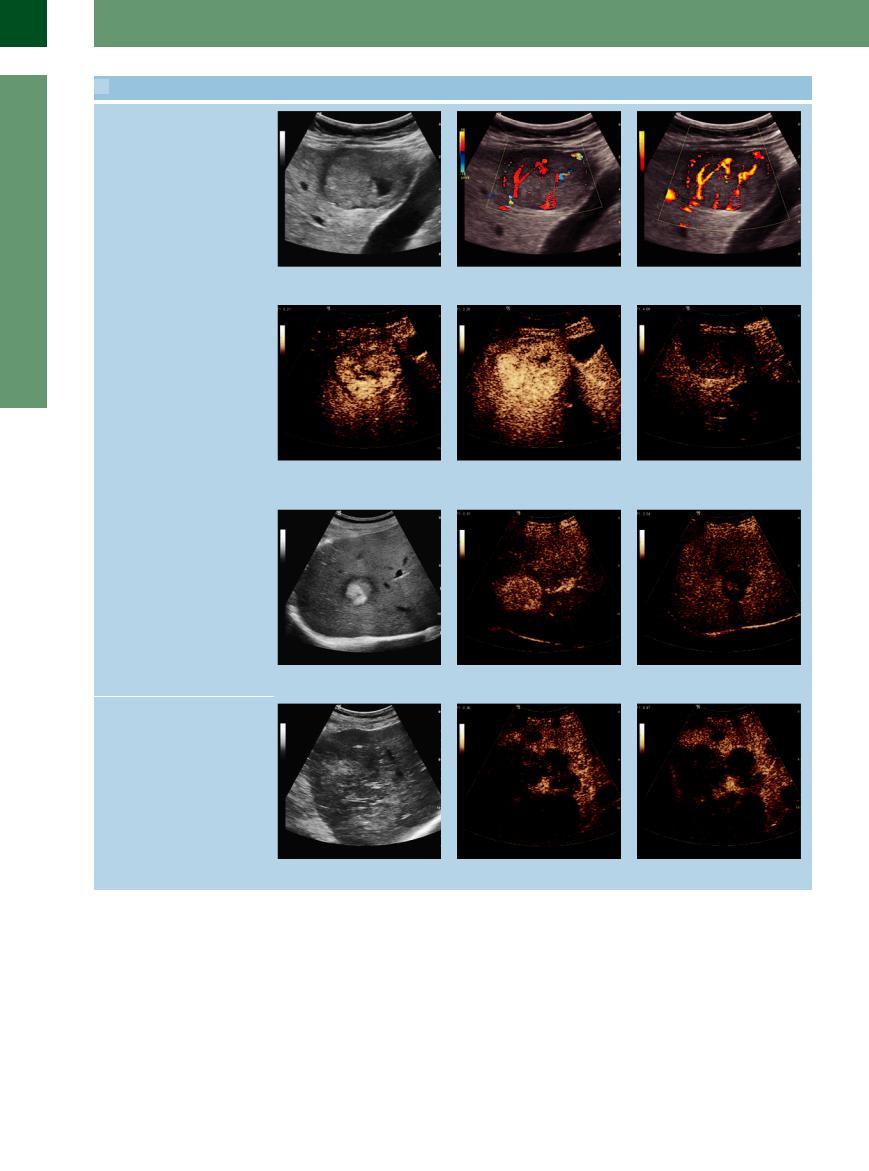
 2.14 Liver Metastases
2.14 Liver Metastases
Liver metastasis of a neuroendocrine carcinoma
a Gray-scale image. |
b Color duplex image. |
c Power Doppler image. |
Neuroendocrine tumors in CEUS
d and e Rapid arterial enhancement. |
f In the late phase, hypoenhancement |
|
(“wash-out”) in contrast to the surround- |
|
ing parenchyma. |
Solitary metastasis of a gastric cancer
g Gray-scale image. |
h Early arterial phase. |
i Late parenchymal phase. |
Metastases of a colonic cancer: hypoenhancement in CEUS
j Gray-scale image. |
k Early arterial phase. |
l Late parenchymal phase. |
122