
- •Contents
- •Preface
- •Contributors
- •1 Vessels
- •1.1 Aorta, Vena Cava, and Peripheral Vessels
- •Aorta, Arteries
- •Anomalies and Variant Positions
- •Dilatation
- •Stenosis
- •Wall Thickening
- •Intraluminal Mass
- •Perivascular Mass
- •Vena Cava, Veins
- •Anomalies
- •Dilatation
- •Intraluminal Mass
- •Compression, Infiltration
- •1.2 Portal Vein and Its Tributaries
- •Enlarged Lumen Diameter
- •Portal Hypertension
- •Intraluminal Mass
- •Thrombosis
- •Tumor
- •2 Liver
- •Enlarged Liver
- •Small Liver
- •Homogeneous Hypoechoic Texture
- •Homogeneous Hyperechoic Texture
- •Regionally Inhomogeneous Texture
- •Diffuse Inhomogeneous Texture
- •Anechoic Masses
- •Hypoechoic Masses
- •Isoechoic Masses
- •Hyperechoic Masses
- •Echogenic Masses
- •Irregular Masses
- •Differential Diagnosis of Focal Lesions
- •Diagnostic Methods
- •Suspected Diagnosis
- •3 Biliary Tree and Gallbladder
- •3.1 Biliary Tree
- •Thickening of the Bile Duct Wall
- •Localized and Diffuse
- •Bile Duct Rarefaction
- •Localized and Diffuse
- •Bile Duct Dilatation and Intraductal Pressure
- •Intrahepatic
- •Hilar and Prepancreatic
- •Intrapancreatic
- •Papillary
- •Abnormal Intraluminal Bile Duct Findings
- •Foreign Body
- •The Seven Most Important Questions
- •3.2 Gallbladder
- •Changes in Size
- •Large Gallbladder
- •Small/Missing Gallbladder
- •Wall Changes
- •General Hypoechogenicity
- •General Hyperechogenicity
- •General Tumor
- •Focal Tumor
- •Intraluminal Changes
- •Hyperechoic
- •Hypoechoic
- •Nonvisualized Gallbladder
- •Missing Gallbladder
- •Obscured Gallbladder
- •4 Pancreas
- •Diffuse Pancreatic Change
- •Large Pancreas
- •Small Pancreas
- •Hypoechoic Texture
- •Hyperechoic Texture
- •Focal Changes
- •Anechoic Lesion
- •Hypoechoic Lesion
- •Isoechoic Lesion
- •Hyperechoic Lesion
- •Irregular (Complex Structured) Lesion
- •Dilatation of the Pancreatic Duct
- •Marginal/Mild Dilatation
- •Marked Dilatation
- •5 Spleen
- •Nonfocal Changes of the Spleen
- •Diffuse Parenchymal Changes
- •Large Spleen
- •Small Spleen
- •Focal Changes of the Spleen
- •Anechoic Mass
- •Hypoechoic Mass
- •Hyperechoic Mass
- •Splenic Calcification
- •6 Lymph Nodes
- •Peripheral Lymph Nodes
- •Head/Neck
- •Extremities (Axilla, Groin)
- •Abdominal Lymph Nodes
- •Porta Hepatis
- •Splenic Hilum
- •Mesentery (Celiac, Upper and Lower Mesenteric Station)
- •Stomach
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •Small/Large Intestine
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •8 Peritoneal Cavity
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Wall Structures
- •Smooth Margin
- •Irregular Margin
- •Intragastric Processes
- •Intraintestinal Processes
- •9 Kidneys
- •Anomalies, Malformations
- •Aplasia, Hypoplasia
- •Cystic Malformation
- •Anomalies of Number, Position, or Rotation
- •Fusion Anomaly
- •Anomalies of the Renal Calices
- •Vascular Anomaly
- •Diffuse Changes
- •Large Kidneys
- •Small Kidneys
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Irregular Structure
- •Circumscribed Changes
- •Anechoic Structure
- •Hypoechoic or Isoechoic Structure
- •Complex Structure
- •Hyperechoic Structure
- •10 Adrenal Glands
- •Enlargement
- •Anechoic Structure
- •Hypoechoic Structure
- •Complex Echo Structure
- •Hyperechoic Structure
- •11 Urinary Tract
- •Malformations
- •Duplication Anomalies
- •Dilatations and Stenoses
- •Dilated Renal Pelvis and Ureter
- •Anechoic
- •Hypoechoic
- •Hypoechoic
- •Hyperechoic
- •Large Bladder
- •Small Bladder
- •Altered Bladder Shape
- •Intracavitary Mass
- •Hypoechoic
- •Hyperechoic
- •Echogenic
- •Wall Changes
- •Diffuse Wall Thickening
- •Circumscribed Wall Thickening
- •Concavities and Convexities
- •12.1 The Prostate
- •Enlarged Prostate
- •Regular
- •Irregular
- •Small Prostate
- •Regular
- •Echogenic
- •Circumscribed Lesion
- •Anechoic
- •Hypoechoic
- •Echogenic
- •12.2 Seminal Vesicles
- •Diffuse Change
- •Hypoechoic
- •Circumscribed Change
- •Anechoic
- •Echogenic
- •Irregular
- •12.3 Testis, Epididymis
- •Diffuse Change
- •Enlargement
- •Decreased Size
- •Circumscribed Lesion
- •Anechoic or Hypoechoic
- •Irregular/Echogenic
- •Epididymal Lesion
- •Anechoic
- •Hypoechoic
- •Intrascrotal Mass
- •Anechoic or Hypoechoic
- •Echogenic
- •13 Female Genital Tract
- •Masses
- •Abnormalities of Size or Shape
- •Uterus
- •Abnormalities of Size or Shape
- •Myometrial Changes
- •Intracavitary Changes
- •Endometrial Changes
- •Fallopian Tubes
- •Hypoechoic Mass
- •Anechoic Cystic Mass
- •Solid Echogenic or Nonhomogeneous Mass
- •14 Thyroid Gland
- •Diffuse Changes
- •Enlarged Thyroid Gland
- •Small Thyroid Gland
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Circumscribed Changes
- •Anechoic
- •Hypoechoic
- •Isoechoic
- •Hyperechoic
- •Irregular
- •Differential Diagnosis of Hyperthyroidism
- •Types of Autonomy
- •15 Pleura and Chest Wall
- •Chest Wall
- •Masses
- •Parietal Pleura
- •Nodular Masses
- •Diffuse Pleural Thickening
- •Pleural Effusion
- •Anechoic Effusion
- •Echogenic Effusion
- •Complex Effusion
- •16 Lung
- •Masses
- •Anechoic Masses
- •Hypoechoic Masses
- •Complex Masses
- •Index
4
Pancreas
Table 4.7 Differentiating pancreatic cancer from focal pancreatitis |
|
||
|
Pancreatic cancer |
Focal pancreatitis |
|
Tumor lesion |
|
|
|
Texture |
Homogeneous to finely mottled |
Lobulated, spotted |
|
|
irregular |
|
|
Delineation |
Polycyclic |
Well defined |
|
Color-flow duplex |
No intrinsic vascularization, infil- |
Normal or marked vascularization |
|
scanning |
trating growth |
|
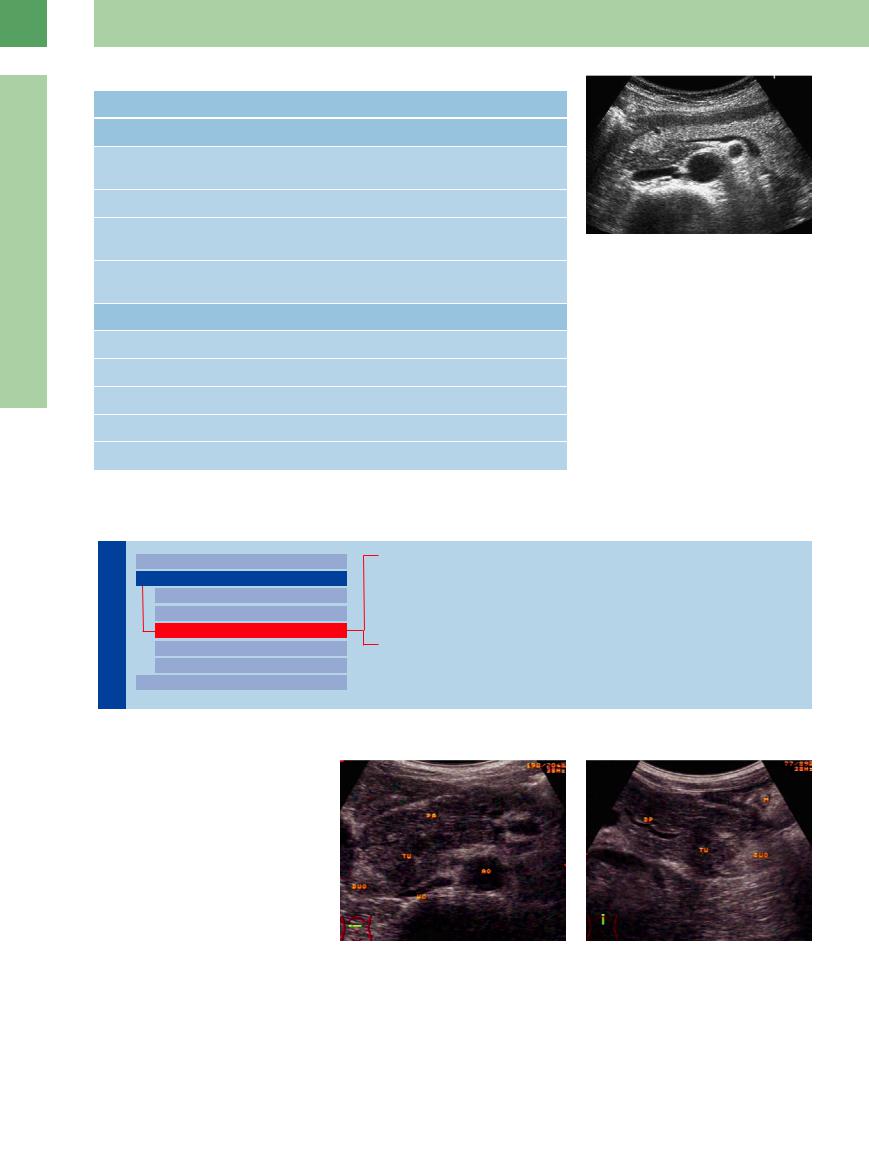
Fig. 4.39 Hypoechoic structure within the pancreatic head |
Contrast-enhanced |
Hypoenhancement |
Similar to the residual parenchyma |
and the uncinate process corresponding to a ventral |
anlage (in pancreatic lipomatosis). |
|||
ultrasound |
|
|
|
Residual organ |
|
|
|
Contour |
Smooth |
Undulating |
|
Parenchyma |
Homogeneous to finely mottled |
Inhomogeneous, coarsely mottled |
|
Pancreatic duct |
Smooth |
Irregular |
|
Calcifications |
(+) |
+++ |
|
Pseudocysts |
(+) |
+++ |
|
Isoechoic Lesion
|
|
|
Diffuse Pancreatic Change |
|
Pancreas |
||||
Hypoechoic Lesion |
||||
|
|
|
Focal Changes |
|
|
|
|
Anechoic Lesion |
|
|
|
|
Isoechoic Lesion |
|
|
|
|
Hyperechoic Lesion |
|
|
|
|
Irregular (Complex Structured) Lesion |
|
|
|
|
Dilatation of the Pancreatic Duct |
|
|
|
|
||
Pancreatic Cancer
Malignant Lymphoma
Focal Pancreatitis
Pancreas Divisum
Annular Pancreas
Pancreatic  Cancer
Cancer


















































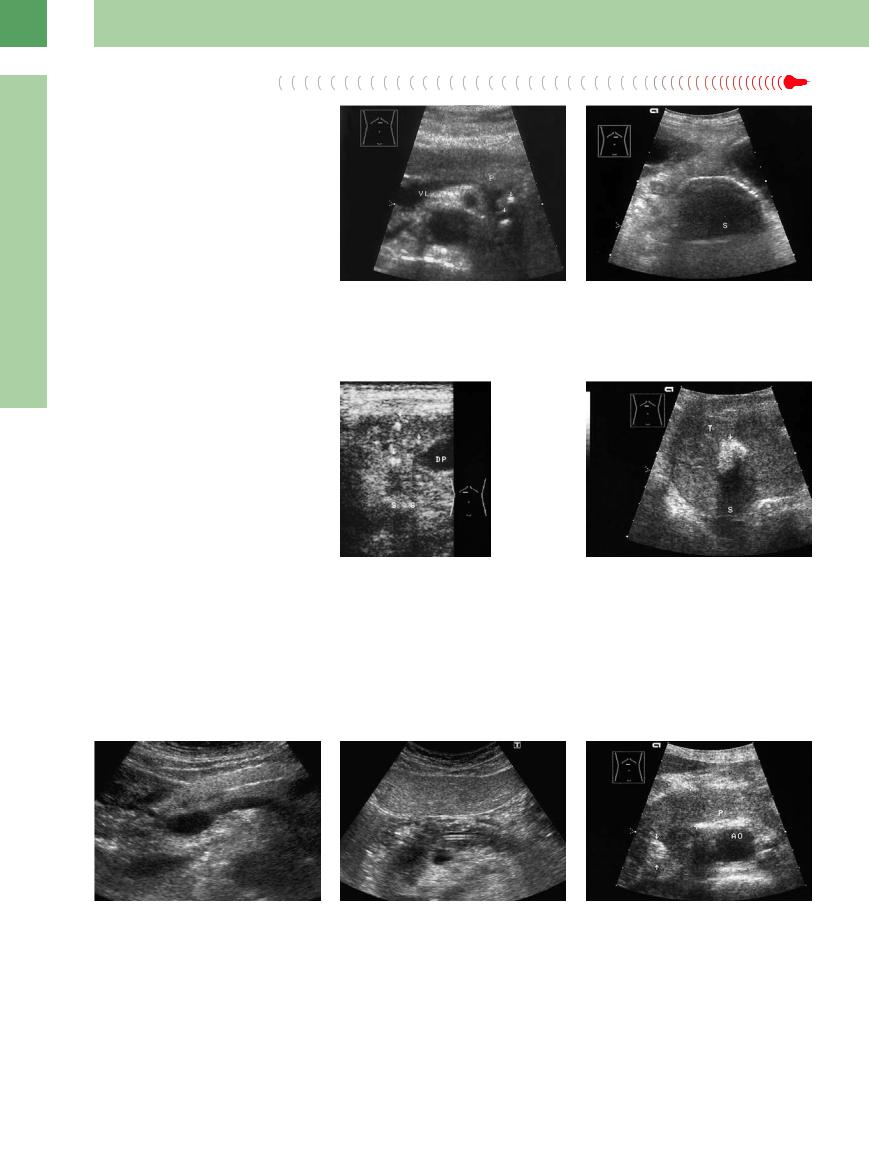
If the texture of the pancreas is hypoechoic, as evidenced in slim young patients, the texture of pancreatic cancer will be isoechoic and can only be differentiated by its bulging contour and any secondary signs. Cancers of the pancreatic tail and uncinate process are also hard to detect, and at that only in the special planes of the oblique/transverse epigastric views: on the right for the head and on the left for the tail of the pancreas. The obstructed pancreatic duct may be a leading sign (Fig. 4.40).
Fig. 4.40 Malignant tumor (TU) of the pancreatic head: texture isoechoic to the rest of the pancreas (PA).
a Transverse scan.
b Longitudinal scan. AO = aorta, WS = vertebral column, AMS = superior mesenteric artery, CF = venous confluence, DUO = duodenum, A = antrum, DP = pancreatic duct.
186
Malignant Lymphoma
















































Malignant lymphoma may also be isoechoic with the pancreas, although its characteristic texture is visualized as markedly hypoechoic (Fig. 4.9a, Fig. 4.36).
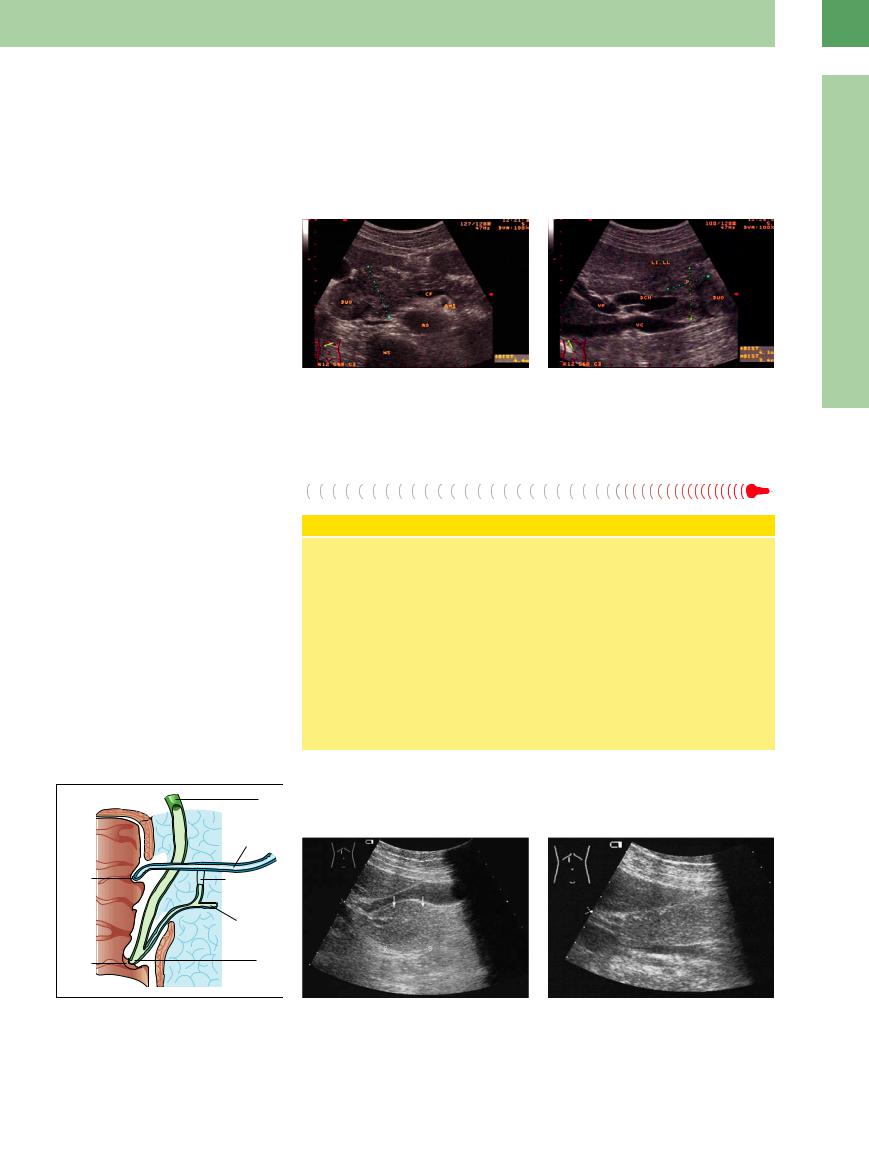
Focal Pancreatitis 


















































While in most cases acute focal pancreatitis appears hypoechoic, chronic focal pancreatitis may be isoechoic with the surrounding pancreatic tissue, and therefore can only be differentiated by focal enlargement and a more macronodular texture. A special form of focal pancreatitis (mainly of the head) is a chronic autoimmune pancreatitis, often characterized by a pancreatic head (or tail12) mass or also by a diffuse pancreatitis. There is a lack of pseudocysts or calculi; the diagnosis is made by antibodies, biopsy, and trial of cortisone therapy (Fig. 4.41, Fig. 4.17b).
Fig. 4.41 Segmental pancreatitis of the head (cursors, P), isoechoic texture.
a Transverse scan.
b Longitudinal scan: Obstruction of the dilated common bile duct (DCH) and cystic duct. DUO = duodenum, WS = vertebral column, AO = aorta, AMS = mesenteric superior artery, VC = vena cava, VP = portal vein, LI LL = left liver lobe, CF = venous confluence.
Pancreas Divisum
Divisum 








Pancreas divisum is characterized by a strikingly enlarged head of the pancreas with normal texture, segmental ductal dilatation in the pancreatic body, and the demonstration of two distinct ductal systems in the pancreatic head (Fig. 4.43, Fig. 4.44).
Congenital Anomaly—Pancreas Divisum
During embryological development, the smaller, originally ventral anlage and the larger dorsal anlage fuse. The ventral anlage constitutes the inferior parts of the head and uncinate process of the pancreas, as well as the main pancreatic duct, while from the dorsal anlage emanate the remainder of the pancreatic head, the entire body and tail, and the anlage for the accessory duct of Santorini. The latter may sometimes persist after fusion and drain the pancreatic juice to the minor papilla, or it may resolve and drain into the main pancreatic duct to the papilla of Vater.
Fusion anomalies (complete or incomplete pancreas divisum) are quite common. The accessory duct of Santorini will drain most of the pancreatic juice via the minor papilla, while the main pancreatic duct (of Wirsung) drains part of the pancreatic head and the uncinate process and displays either no (complete pancreas divisum) or only a thin (incomplete pancreas divisum) communication with the main duct (Fig. 4.42). The relative stenosis upstream of the minor papilla may cause recurrent episodes of pancreatitis.
4
Focal Changes
Fig. 4.42 Schematic drawing of complete and incomplete pancreas divisum.
Fig. 4.43 Enlarged head of pancreas.
a Impressing the posterior wall of the gallbladder (arrow).
b Impressing the vena cava. CT study suspected malignancy. Ultrasound diagnosis: probably pancreas divisum. ERCP: pancreas divisum.
187
4
Pancreas
Annular pancreas is another example of an isoechoic focal lesion with changes in size and shape; only in rare instances is it completely annular. In most patients it is completely or incompletely annular around the pancreatic head, which envelops the descending duodenum and may result in stenosis.
In ultrasonography there is definite compression of the descending duodenum by the enlarged head of the pancreas, which is missing its usual border with the duodenum and extends further to the right, posterior and lateral to the duodenum (Fig. 4.45).13
b Pancreatic tissue (P) unusually far to the right; the |
c Transverse epigastric |
view. The pancreas continues |
descending duodenum (D) is stenosed by the formation |
rather strikingly to the |
right (arrows) posterior to the |
of the pancreas. A = antrum, BD = duodenal bulb, GB = |
dilated (prestenotic) duodenum (BD). VL = splenic vein. |
|
gallbladder, U = uncinate process, VC = vena cava, AO = |
|
|
aorta. |
|
|
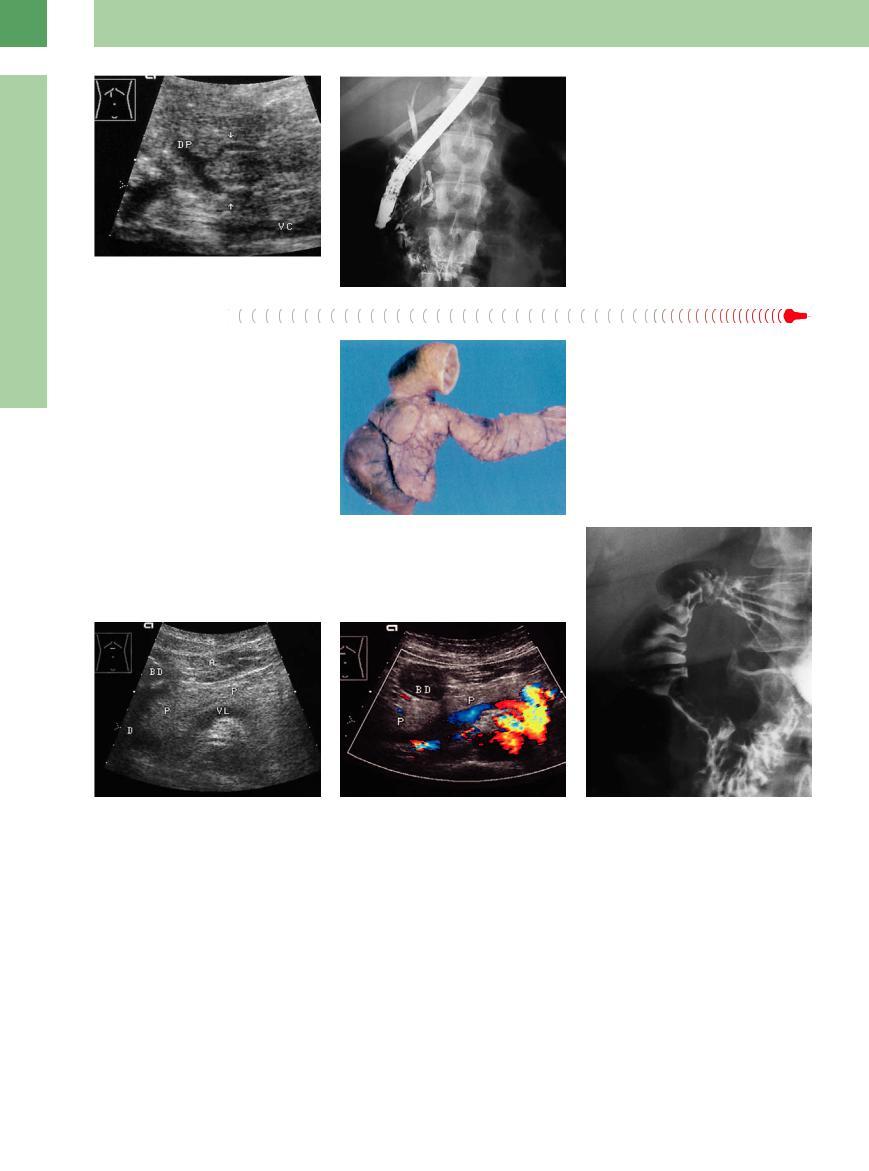
Fig. 4.44 Pancreas divisum, recurrent pancreatitis.
aLongitudinal ultrasound view demonstrating two pancreatic ducts (arrows). The ventral duct is seen to possess
anarrow communication with the main pancreatic duct (DP); the larger posterior duct is the accessory duct of Santorini. VC = vena cava.
b ERCP through the papilla of Vater, with visualization of the CBD and rudiments of the main pancreatic duct (see also  4.1 l).
4.1 l).
Fig. 4.45 Annular pancreas.
a Pathology specimen (from Riede and Werner13).
d Hypotonic duodenogram: stenosis of the descending duodenum.
188
Hyperechoic Lesion
|
|
|
Diffuse Pancreatic Change |
|
Pancreas |
||||
Hypoechoic Lesion |
||||
|
|
|
Focal Changes |
|
|
|
|
Anechoic Lesion |
|
|
|
|
Isoechoic Lesion |
|
|
|
|
Hyperechoic Lesion |
|
|
|
|
Irregular (Complex Structured) Lesion |
|
|
|
|
Dilatation of the Pancreatic Duct |
|
|
|
|
||
Calcification/Intraductal Calculus
Calcified Splenic Artery
Microcalcification, Fat Necrosis
Intraductal Gas/Stent
Focal Fatty Infiltration
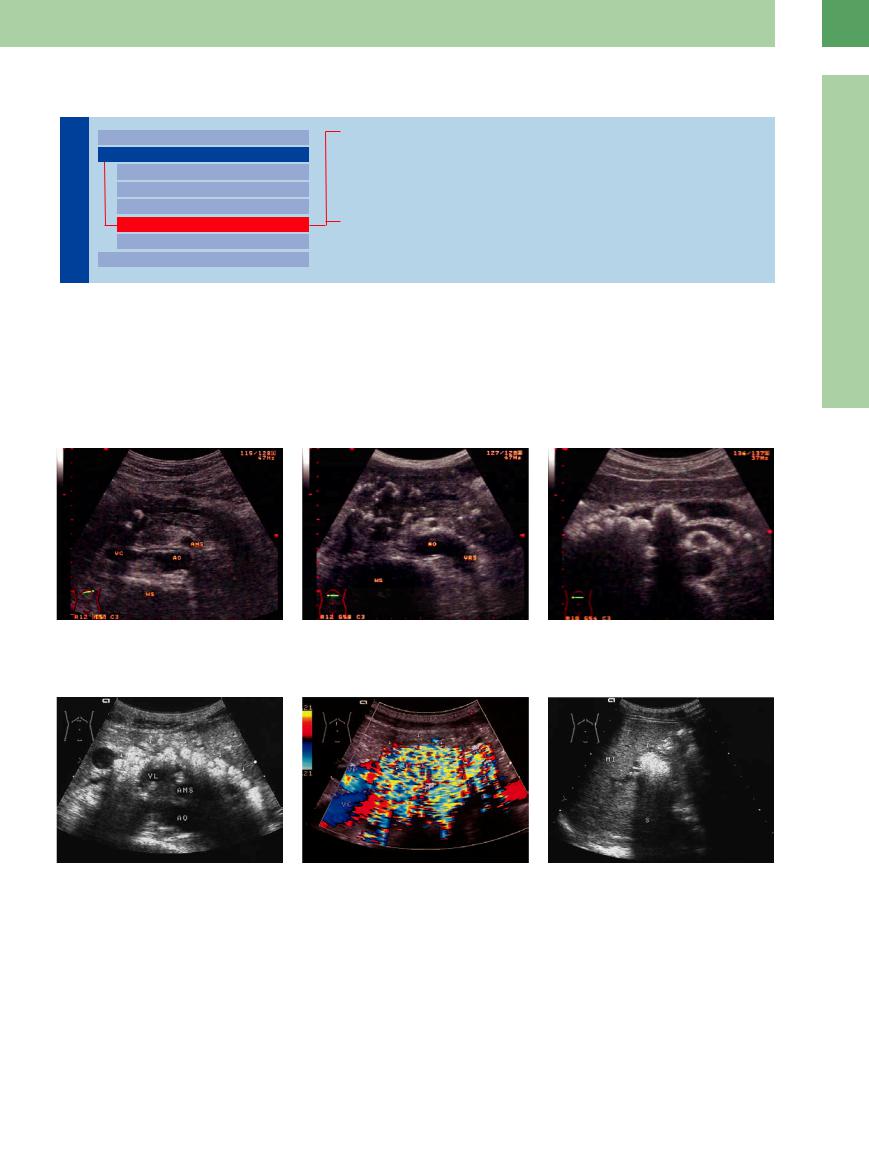
Calcification/Intraductal Calculus










































The most striking, and in addition pathogno- |
calculi) |
and the branching ductules (“paren- |
change of the wave velocity, from phase alter- |
|
monic, criteria for chronic pancreatitis are cal- |
chymal |
calcification”). They appear |
as inten- |
ation or Doppler shifting, and may also be |
cification and intraductal calculi. They consist |
sively hyperechoic structures with |
posterior |
caused by mechanical pulses leading to mini- |
|
of calcium carbonate precipitates and are lo- |
shadowing; the “twinkling artifact” is used as |
mal movements of the calculi (Figs. 4.46, 4.47; |
||
cated in the main pancreatic duct (intraductal |
a diagnostic sign. This probably results from a |
see also Fig. 4.66b). |
||
4
Focal Changes
Fig. 4. 46 Chronic calcifying pancreatitis. a Ductal stones.
Fig. 4.47a–c Chronic calcifying pancreatitis.
a Brightness picture: coarse diffuse echogenic structure with multiple posterior shadowing and summation shadowing. VL = splenic vein; AMS = superior mesenteric vein; AO = aorta.
b Multiple parenchymal calcification, partly with shadowing. WS = vertebral column, AO = aorta, AMS = superior mesenteric artery, VC = vena cava, VRS = left renal vein.
b Color Doppler “twinkling artifact” with confetti phenomenon. VP = portal vein; VC = vena cava.
c Calcifications, stones in the pancreatic duct, atrophy.
c Trans-splenic section. Calcification (arrows) in the tail of the pancreas, shadowing (S). MI = spleen.
189
4
Pancreas
Fig. 4.48
a Echogenic calcified mottling (arrows): calcified splenic artery. VL = splenic vein; P = pancreas.
b Hyperechoic reflection with shadowing (S) overlapping the pancreas: calcified splenic artery.
Microcalcification, Fat
Fat Necrosis
Necrosis











































Microcalcification can be found in chronic pancreatitis, in pancreatic cancer, and as sclerosis in arterial walls. Fat necrosis as part of acute pancreatitis will appear as focal echogenic peripancreatic mottling/bands (Figs. 4.6, 4.49, 4.50).
Fig. 4.49 Echogenic microcalcification with shadowing (S) in pancreatic cancer; cut-off of the pancreatic duct (DP).
Fig. 4.50 Microcalcification and macrocalcification (arrows, shadowing S) in advanced pancreatic cancer (T).
Intraductal Gas/Stent
Gas/Stent 
















































After endoscopic intervention at the papilla or pancreatic duct, gas (after papillotomy) or stents in the pancreatic or intrapancreatic CBD may be evidenced as echogenic foreign
bodies within the duct (Figs. 4.51, 4.52, 4.53). Usually their differential diagnosis becomes self-evident from the patient’s history.
Fig. 4.51 Gas in the pancreatic duct in duodenal diverticulum: hyperechoic band.
Fig. 4.52 Echogenic stent in the pancreatic duct (arrow; DP). P = pancreas; VL = splenic vein; AO = aorta.
Fig. 4.53 Diffuse pancreatic cancer in the head/body of the pancreas (P) (calipers 20 mm); CBD stent (arrows) in place. AO = aorta.
190
