
- •Contents
- •Preface
- •Contributors
- •1 Vessels
- •1.1 Aorta, Vena Cava, and Peripheral Vessels
- •Aorta, Arteries
- •Anomalies and Variant Positions
- •Dilatation
- •Stenosis
- •Wall Thickening
- •Intraluminal Mass
- •Perivascular Mass
- •Vena Cava, Veins
- •Anomalies
- •Dilatation
- •Intraluminal Mass
- •Compression, Infiltration
- •1.2 Portal Vein and Its Tributaries
- •Enlarged Lumen Diameter
- •Portal Hypertension
- •Intraluminal Mass
- •Thrombosis
- •Tumor
- •2 Liver
- •Enlarged Liver
- •Small Liver
- •Homogeneous Hypoechoic Texture
- •Homogeneous Hyperechoic Texture
- •Regionally Inhomogeneous Texture
- •Diffuse Inhomogeneous Texture
- •Anechoic Masses
- •Hypoechoic Masses
- •Isoechoic Masses
- •Hyperechoic Masses
- •Echogenic Masses
- •Irregular Masses
- •Differential Diagnosis of Focal Lesions
- •Diagnostic Methods
- •Suspected Diagnosis
- •3 Biliary Tree and Gallbladder
- •3.1 Biliary Tree
- •Thickening of the Bile Duct Wall
- •Localized and Diffuse
- •Bile Duct Rarefaction
- •Localized and Diffuse
- •Bile Duct Dilatation and Intraductal Pressure
- •Intrahepatic
- •Hilar and Prepancreatic
- •Intrapancreatic
- •Papillary
- •Abnormal Intraluminal Bile Duct Findings
- •Foreign Body
- •The Seven Most Important Questions
- •3.2 Gallbladder
- •Changes in Size
- •Large Gallbladder
- •Small/Missing Gallbladder
- •Wall Changes
- •General Hypoechogenicity
- •General Hyperechogenicity
- •General Tumor
- •Focal Tumor
- •Intraluminal Changes
- •Hyperechoic
- •Hypoechoic
- •Nonvisualized Gallbladder
- •Missing Gallbladder
- •Obscured Gallbladder
- •4 Pancreas
- •Diffuse Pancreatic Change
- •Large Pancreas
- •Small Pancreas
- •Hypoechoic Texture
- •Hyperechoic Texture
- •Focal Changes
- •Anechoic Lesion
- •Hypoechoic Lesion
- •Isoechoic Lesion
- •Hyperechoic Lesion
- •Irregular (Complex Structured) Lesion
- •Dilatation of the Pancreatic Duct
- •Marginal/Mild Dilatation
- •Marked Dilatation
- •5 Spleen
- •Nonfocal Changes of the Spleen
- •Diffuse Parenchymal Changes
- •Large Spleen
- •Small Spleen
- •Focal Changes of the Spleen
- •Anechoic Mass
- •Hypoechoic Mass
- •Hyperechoic Mass
- •Splenic Calcification
- •6 Lymph Nodes
- •Peripheral Lymph Nodes
- •Head/Neck
- •Extremities (Axilla, Groin)
- •Abdominal Lymph Nodes
- •Porta Hepatis
- •Splenic Hilum
- •Mesentery (Celiac, Upper and Lower Mesenteric Station)
- •Stomach
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •Small/Large Intestine
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •8 Peritoneal Cavity
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Wall Structures
- •Smooth Margin
- •Irregular Margin
- •Intragastric Processes
- •Intraintestinal Processes
- •9 Kidneys
- •Anomalies, Malformations
- •Aplasia, Hypoplasia
- •Cystic Malformation
- •Anomalies of Number, Position, or Rotation
- •Fusion Anomaly
- •Anomalies of the Renal Calices
- •Vascular Anomaly
- •Diffuse Changes
- •Large Kidneys
- •Small Kidneys
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Irregular Structure
- •Circumscribed Changes
- •Anechoic Structure
- •Hypoechoic or Isoechoic Structure
- •Complex Structure
- •Hyperechoic Structure
- •10 Adrenal Glands
- •Enlargement
- •Anechoic Structure
- •Hypoechoic Structure
- •Complex Echo Structure
- •Hyperechoic Structure
- •11 Urinary Tract
- •Malformations
- •Duplication Anomalies
- •Dilatations and Stenoses
- •Dilated Renal Pelvis and Ureter
- •Anechoic
- •Hypoechoic
- •Hypoechoic
- •Hyperechoic
- •Large Bladder
- •Small Bladder
- •Altered Bladder Shape
- •Intracavitary Mass
- •Hypoechoic
- •Hyperechoic
- •Echogenic
- •Wall Changes
- •Diffuse Wall Thickening
- •Circumscribed Wall Thickening
- •Concavities and Convexities
- •12.1 The Prostate
- •Enlarged Prostate
- •Regular
- •Irregular
- •Small Prostate
- •Regular
- •Echogenic
- •Circumscribed Lesion
- •Anechoic
- •Hypoechoic
- •Echogenic
- •12.2 Seminal Vesicles
- •Diffuse Change
- •Hypoechoic
- •Circumscribed Change
- •Anechoic
- •Echogenic
- •Irregular
- •12.3 Testis, Epididymis
- •Diffuse Change
- •Enlargement
- •Decreased Size
- •Circumscribed Lesion
- •Anechoic or Hypoechoic
- •Irregular/Echogenic
- •Epididymal Lesion
- •Anechoic
- •Hypoechoic
- •Intrascrotal Mass
- •Anechoic or Hypoechoic
- •Echogenic
- •13 Female Genital Tract
- •Masses
- •Abnormalities of Size or Shape
- •Uterus
- •Abnormalities of Size or Shape
- •Myometrial Changes
- •Intracavitary Changes
- •Endometrial Changes
- •Fallopian Tubes
- •Hypoechoic Mass
- •Anechoic Cystic Mass
- •Solid Echogenic or Nonhomogeneous Mass
- •14 Thyroid Gland
- •Diffuse Changes
- •Enlarged Thyroid Gland
- •Small Thyroid Gland
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Circumscribed Changes
- •Anechoic
- •Hypoechoic
- •Isoechoic
- •Hyperechoic
- •Irregular
- •Differential Diagnosis of Hyperthyroidism
- •Types of Autonomy
- •15 Pleura and Chest Wall
- •Chest Wall
- •Masses
- •Parietal Pleura
- •Nodular Masses
- •Diffuse Pleural Thickening
- •Pleural Effusion
- •Anechoic Effusion
- •Echogenic Effusion
- •Complex Effusion
- •16 Lung
- •Masses
- •Anechoic Masses
- •Hypoechoic Masses
- •Complex Masses
- •Index
1
Vessels
Tumor
Vessels |
Enlarged Lumen Diameter |
|||
|
|
|
||
|
|
|
Intraluminal Mass |
|
|
|
|
||
|
|
|
|
Thrombosis |
|
|
|
|
Tumor |
|
|
|
|
|
Tumor Infiltration
Tumor Infiltration


















































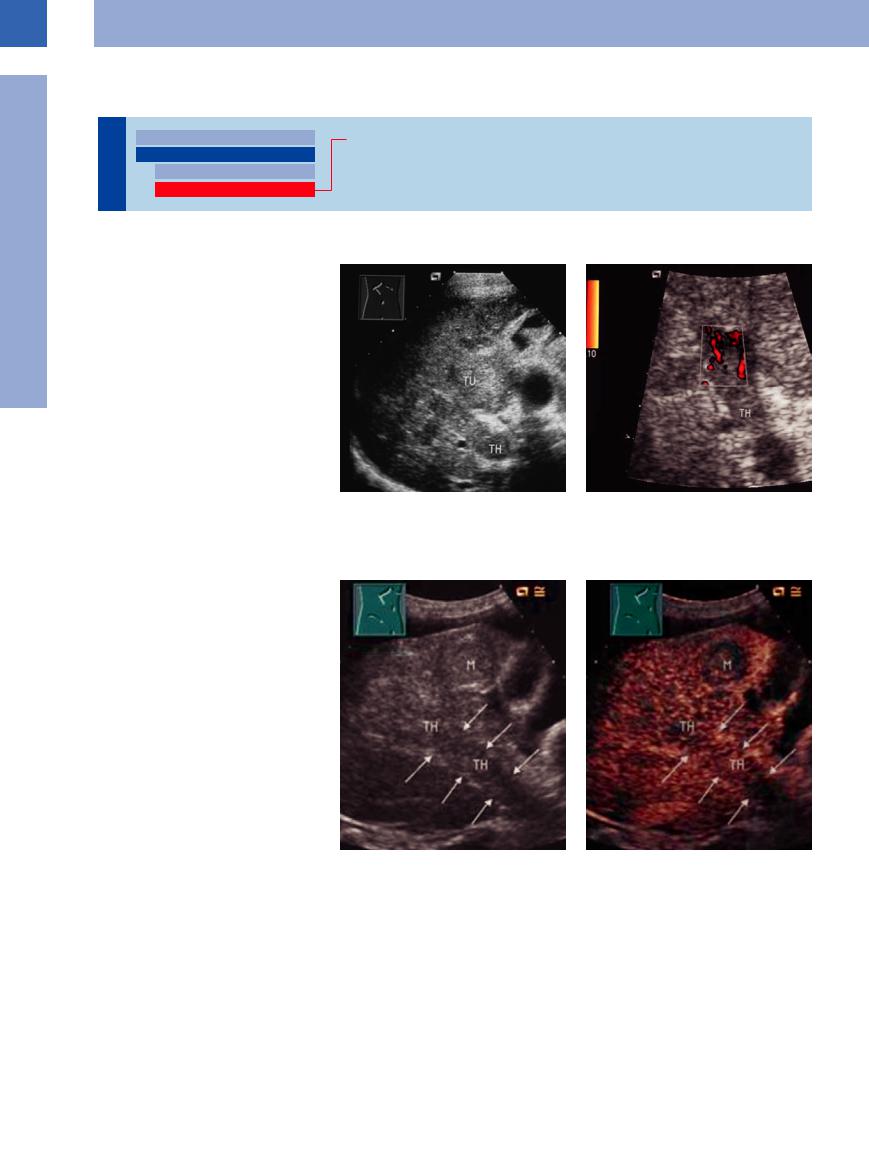
Tumor infiltration into the portovenous system is not infrequent, and in primary hepatic malignancies it is observed quite often at the porta hepatis. Ultrasonography can differentiate between tumor infiltration and thrombosis of the portal vein, but may be difficult to perform for some segments. If color-flow Doppler imaging demonstrates tumor vessels within the “thrombotic material,” this will confirm the diagnosis of tumorous thrombosis (Fig.1.105).
In CEUS, tumor infiltration shows a contrast enhancement (Fig.1.106).
At the confluence and along the splenic vein, tumor infiltration may be one complication of pancreatic cancer, with extensive infiltration of the tumor into the vessel usually being a sign of inoperability. Under good conditions in such cases, ultrasonography may be able to demonstrate direct infiltration of the portal vessels by continuity.18
Fig. 1.105 Patient with hepatocellular carcinoma (TU). TH = thrombosis.
a Demonstration of the tumor and the echogenic portal vein immediately adjacent to it.
Fig. 1.106 Patient with liver cirrhosis and hepatocellular carcinoma.
a Echogenic portal vein (arrows; thrombosis TH) and multiple masses (M).
b Color-flow duplex scanning confirmed the diagnosis of portal vein thrombosis. The discrete flow signals within the thrombotic material raise the suspicion of a tumorous thrombus.
b Contrast-enhanced ultrasound (CEUS) depicts an enhancing within the echogenic portal vein (TH, arrows) as a sign for tumor thrombosis.
52
Tips, tricks, and pitfalls
The dilation of the lumen of the portal vein is not a reliable parameter to diagnose portal hypertension. A better correlation exists between the extent of portal hypertension and the maximal flow rate measured in the portal vein (< 12 cm/s). There can be an overlap between the normal and pathological range of flow rates. This can lead to a false evaluation, if the flow rate is the only value that is considered.
A false normal flow rate can primarily occur due to intrahepatic shunts and an efflux via the paraumbilical veins to the paraumbilical varicose veins (“caput medusae”), which are distinctly
visible in color duplex sonography. Further, a caudal directed efflux via the iliac vein as in a spontaneous portocaval shunt can cause a false normal flow rate. In these cases the flow rate can be elevated up to 40 cm/s. A so-called “Cruvei- lier–Baumgarten syndrome” is present if the umbilical vein is persistently open without the existence of liver cirrhosis.
A transjugular intrahepatic portosystemic shunt (TIPS) is an iatrogenic portosystemic shunt (cf. Chapter 2, Fig. 2.110, p. 116).
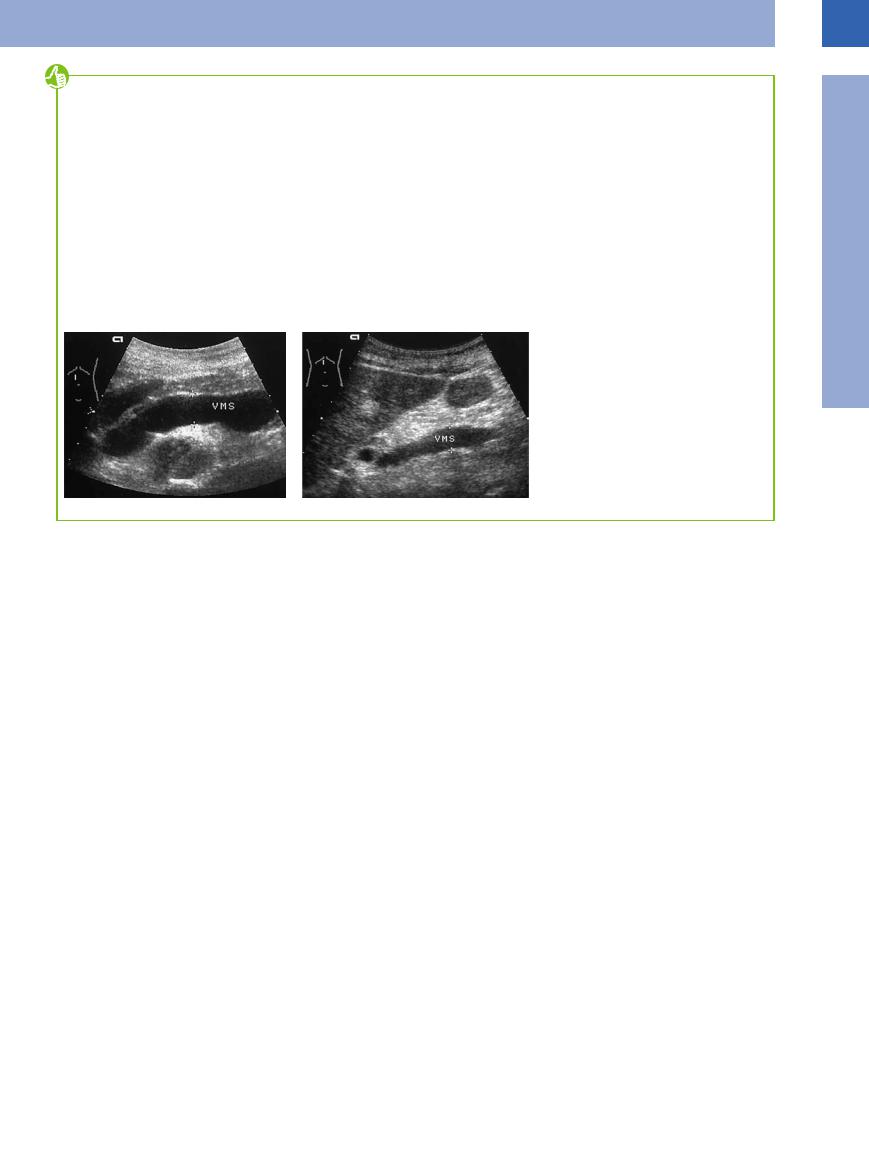
A particular situation is “segmental portal hypertension”. It is based on lack of compression of a
feeder vein. This is mainly caused by tumor compression/ infiltration of the superior mesenteric and splenic vein (infiltration by a pancreatic tumor, lymph node compression in metastasis/ lymphoma). The diagnosis arises from the knowledge of the underlying condition and the particular sonographic findings (Fig. 1.107).
If a conspicuous widening is detected in a feeder vein, especially, if it is the superior mesenteric vein, mesenteric lymph node metastasis should be looked for.
Fig. 1.107
a Extensive enlargement of the superior mesenteric vein up to 17.4 mm caused by intra-abdominal lymphomas (final-stage chronic lymphocytic leukemia (CLL), severe splenomegaly with dilatation of all portal branches).
b Solitary enlargement of the superior mesenteric vein (VMS) in a local metastatic spread of a pancreatic carcinoma.
1
Intraluminal Mass
References
[1]Ludwig M, Kraft K, Rücker W, Hüther AM. Diagnosis of very early arteriosclerosis vascular changes using Duplex sonography. [Article in German] Klin Wochenschr 1989;67(8):442–446
[2]Ludwig M, von Petzinger-Kruthoff A, von Buquoy M, Stumpe KO. Intima-Media-Dicke der Karotisarterien: Früher Indikator für Arteriosklerose und therapeutischer Endpunkt. Ultraschall Med 2003;24(3):162–174
[3]Lorenz MW, Markus HS, Bots M, et al. Prediction of clinical cardiovascular events with carotid intima-media thickness: a systematic review and meta-analysis. Circulation 2007;115:459–467
[4]Heyne JP. Die doppelte Aorta—Rarität oder Artefakt im Ultraschall [The double aorta—r- arity or artifact of ultrasound]. Ultraschall Med 2000;21(3):145–147
[5]Schmidt WA, Kraft HE, Vorpahl K, Völker L, Gromnica-Ihle EJ. Color duplex ultrasonography in the diagnosis of temporal arteritis. N Engl J Med 1997;337(19):1336–1342
[6]Neuerburg-Heusler D, Hennerici M. Gefäßdiagnostik mit Ultraschall. 2nd ed. Stuttgart: Thieme, 1995
[7]Mallek R, Mostbeck G, Walter R, Tscholakow D. Duplexsonographie der Visceralarterien: Angiographische Korrelation. Ultraschall Klin Praxis 1990;5:186
[8]Arning C, et al. Nicht arteriosklerotische Erkrankungen der Halsarterien [Nonarteriosclerotic disease of the cervical arteries]. Ultraschall Med 2008;29:576–599
[9]Widder B, von Reutern GM, Neuerburg-Heus- ler D. Morphologische und dopplersonographische Kriterien zur Bestimmung von Stenosierungsgraden an der A. carotis interna. Ultraschall Med 1986;7:70–75
[10]Janssen A. Pulsatility index is better than an- kle-brachial doppler index for non-invasive detection of critical limb ischaemia in diabetes. Vasa 2005;34(4):235–241
[11]Mörl H, Menges HW. Gefäßkrankheiten in der Praxis. 7th ed. Stuttgart: Thieme 2000
[12]Entelmann M, Sheikhzadeh A. Thromben der Aorta als Emboliequelle. Dtsch Arztebl 2001;98:1968–1970
[13]Clevert DA, Stickel M, Johnson T, et al. Imaging of aortic abnormalities with contrast-en- hanced ultrasound. A pictorial comparison with CT. Eur Radiol 2007;17(11):2991–3000
[14]Fellmeth BD, Roberts AC, Bookstein JJ, et al. Postangiographic femoral artery injuries: nonsurgical repair with US-guided compression. Radiology 1991;178(3):671–675
[15]Habscheid W, Landwehr P. Diagnostik der akuten tiefen Beinvenenthrombose mit der Kompressionssonographie [Diagnosis of acute deep leg vein thrombosis with compression ultrasonography]. Ultraschall Med 1990;11(6):268–273
[16]Hach W, Girth E, Lechner W. Einteilung der Stammvarikose der V. saphena magna in 4 Stadien. Phlebol Proktol 1977;6:116–123
[17]Görg C, Riera-Knorrenschild J. Pictorial review: colour Doppler ultrasound flow patterns in the portal venous system. Br J Radiol 2002;75:919–929
[18]Ochs A. Sonographie der Leber. Freiburg: Falk Foundation Freiburg 2000;1–115
[19]Gaitini D, Thaler I, Kaftori JK. Duplex sonography in the diagnosis of portal vein thrombosis. Rofo 1990;153(6):645–649
[20]Furuse J, Matsutani S, Yoshikawa M, et al. Diagnosis of portal vein tumor thrombus by pulsed Doppler ultrasonography. J Clin Ultrasound 1992;20(7):439–446
[21]Schumacher H, Eckstein HH, Kallinowski F, Allenberg JR. Morphometry and classification in abdominal aortic aneurysms: patient selection for endovascular and open surgery. J Endovasc Surg 1997;4(1):39–44
[22]Schmidt G, Görg C. Kursbuch Ultraschall, 5th ed. Stuttgart, New York: Thieme 2006
[23]Schmidt G, Ed. Checkliste Sonographie. 3. Aufl., Stuttgart, New York: Thieme 2006
[24]Seitz K, Wermke W, Haas K. Sonographie bei portaler Hypertension und TIPPS. Freiburg: Falk Foundation 1997;3–64
53

