
- •Contents
- •Preface
- •Contributors
- •1 Vessels
- •1.1 Aorta, Vena Cava, and Peripheral Vessels
- •Aorta, Arteries
- •Anomalies and Variant Positions
- •Dilatation
- •Stenosis
- •Wall Thickening
- •Intraluminal Mass
- •Perivascular Mass
- •Vena Cava, Veins
- •Anomalies
- •Dilatation
- •Intraluminal Mass
- •Compression, Infiltration
- •1.2 Portal Vein and Its Tributaries
- •Enlarged Lumen Diameter
- •Portal Hypertension
- •Intraluminal Mass
- •Thrombosis
- •Tumor
- •2 Liver
- •Enlarged Liver
- •Small Liver
- •Homogeneous Hypoechoic Texture
- •Homogeneous Hyperechoic Texture
- •Regionally Inhomogeneous Texture
- •Diffuse Inhomogeneous Texture
- •Anechoic Masses
- •Hypoechoic Masses
- •Isoechoic Masses
- •Hyperechoic Masses
- •Echogenic Masses
- •Irregular Masses
- •Differential Diagnosis of Focal Lesions
- •Diagnostic Methods
- •Suspected Diagnosis
- •3 Biliary Tree and Gallbladder
- •3.1 Biliary Tree
- •Thickening of the Bile Duct Wall
- •Localized and Diffuse
- •Bile Duct Rarefaction
- •Localized and Diffuse
- •Bile Duct Dilatation and Intraductal Pressure
- •Intrahepatic
- •Hilar and Prepancreatic
- •Intrapancreatic
- •Papillary
- •Abnormal Intraluminal Bile Duct Findings
- •Foreign Body
- •The Seven Most Important Questions
- •3.2 Gallbladder
- •Changes in Size
- •Large Gallbladder
- •Small/Missing Gallbladder
- •Wall Changes
- •General Hypoechogenicity
- •General Hyperechogenicity
- •General Tumor
- •Focal Tumor
- •Intraluminal Changes
- •Hyperechoic
- •Hypoechoic
- •Nonvisualized Gallbladder
- •Missing Gallbladder
- •Obscured Gallbladder
- •4 Pancreas
- •Diffuse Pancreatic Change
- •Large Pancreas
- •Small Pancreas
- •Hypoechoic Texture
- •Hyperechoic Texture
- •Focal Changes
- •Anechoic Lesion
- •Hypoechoic Lesion
- •Isoechoic Lesion
- •Hyperechoic Lesion
- •Irregular (Complex Structured) Lesion
- •Dilatation of the Pancreatic Duct
- •Marginal/Mild Dilatation
- •Marked Dilatation
- •5 Spleen
- •Nonfocal Changes of the Spleen
- •Diffuse Parenchymal Changes
- •Large Spleen
- •Small Spleen
- •Focal Changes of the Spleen
- •Anechoic Mass
- •Hypoechoic Mass
- •Hyperechoic Mass
- •Splenic Calcification
- •6 Lymph Nodes
- •Peripheral Lymph Nodes
- •Head/Neck
- •Extremities (Axilla, Groin)
- •Abdominal Lymph Nodes
- •Porta Hepatis
- •Splenic Hilum
- •Mesentery (Celiac, Upper and Lower Mesenteric Station)
- •Stomach
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •Small/Large Intestine
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •8 Peritoneal Cavity
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Wall Structures
- •Smooth Margin
- •Irregular Margin
- •Intragastric Processes
- •Intraintestinal Processes
- •9 Kidneys
- •Anomalies, Malformations
- •Aplasia, Hypoplasia
- •Cystic Malformation
- •Anomalies of Number, Position, or Rotation
- •Fusion Anomaly
- •Anomalies of the Renal Calices
- •Vascular Anomaly
- •Diffuse Changes
- •Large Kidneys
- •Small Kidneys
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Irregular Structure
- •Circumscribed Changes
- •Anechoic Structure
- •Hypoechoic or Isoechoic Structure
- •Complex Structure
- •Hyperechoic Structure
- •10 Adrenal Glands
- •Enlargement
- •Anechoic Structure
- •Hypoechoic Structure
- •Complex Echo Structure
- •Hyperechoic Structure
- •11 Urinary Tract
- •Malformations
- •Duplication Anomalies
- •Dilatations and Stenoses
- •Dilated Renal Pelvis and Ureter
- •Anechoic
- •Hypoechoic
- •Hypoechoic
- •Hyperechoic
- •Large Bladder
- •Small Bladder
- •Altered Bladder Shape
- •Intracavitary Mass
- •Hypoechoic
- •Hyperechoic
- •Echogenic
- •Wall Changes
- •Diffuse Wall Thickening
- •Circumscribed Wall Thickening
- •Concavities and Convexities
- •12.1 The Prostate
- •Enlarged Prostate
- •Regular
- •Irregular
- •Small Prostate
- •Regular
- •Echogenic
- •Circumscribed Lesion
- •Anechoic
- •Hypoechoic
- •Echogenic
- •12.2 Seminal Vesicles
- •Diffuse Change
- •Hypoechoic
- •Circumscribed Change
- •Anechoic
- •Echogenic
- •Irregular
- •12.3 Testis, Epididymis
- •Diffuse Change
- •Enlargement
- •Decreased Size
- •Circumscribed Lesion
- •Anechoic or Hypoechoic
- •Irregular/Echogenic
- •Epididymal Lesion
- •Anechoic
- •Hypoechoic
- •Intrascrotal Mass
- •Anechoic or Hypoechoic
- •Echogenic
- •13 Female Genital Tract
- •Masses
- •Abnormalities of Size or Shape
- •Uterus
- •Abnormalities of Size or Shape
- •Myometrial Changes
- •Intracavitary Changes
- •Endometrial Changes
- •Fallopian Tubes
- •Hypoechoic Mass
- •Anechoic Cystic Mass
- •Solid Echogenic or Nonhomogeneous Mass
- •14 Thyroid Gland
- •Diffuse Changes
- •Enlarged Thyroid Gland
- •Small Thyroid Gland
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Circumscribed Changes
- •Anechoic
- •Hypoechoic
- •Isoechoic
- •Hyperechoic
- •Irregular
- •Differential Diagnosis of Hyperthyroidism
- •Types of Autonomy
- •15 Pleura and Chest Wall
- •Chest Wall
- •Masses
- •Parietal Pleura
- •Nodular Masses
- •Diffuse Pleural Thickening
- •Pleural Effusion
- •Anechoic Effusion
- •Echogenic Effusion
- •Complex Effusion
- •16 Lung
- •Masses
- •Anechoic Masses
- •Hypoechoic Masses
- •Complex Masses
- •Index
15
Pleura and Chest Wall
■ Parietal Pleura
Nodular Masses
Wall |
|
|
Chest Wall |
|
|
|
|
||
|
|
|
Parietal Pleura |
|
Chest |
|
|
||
|
|
|
Nodular Masses |
|
|
|
|
||
|
|
|
Diffuse Pleural Thickening |
|
|
|
|
|
|
|
|
|
Pleural Effusion |
|
Pleura and |
|
|||
|
|
|
|
|
Metastases
Pleural Plaque
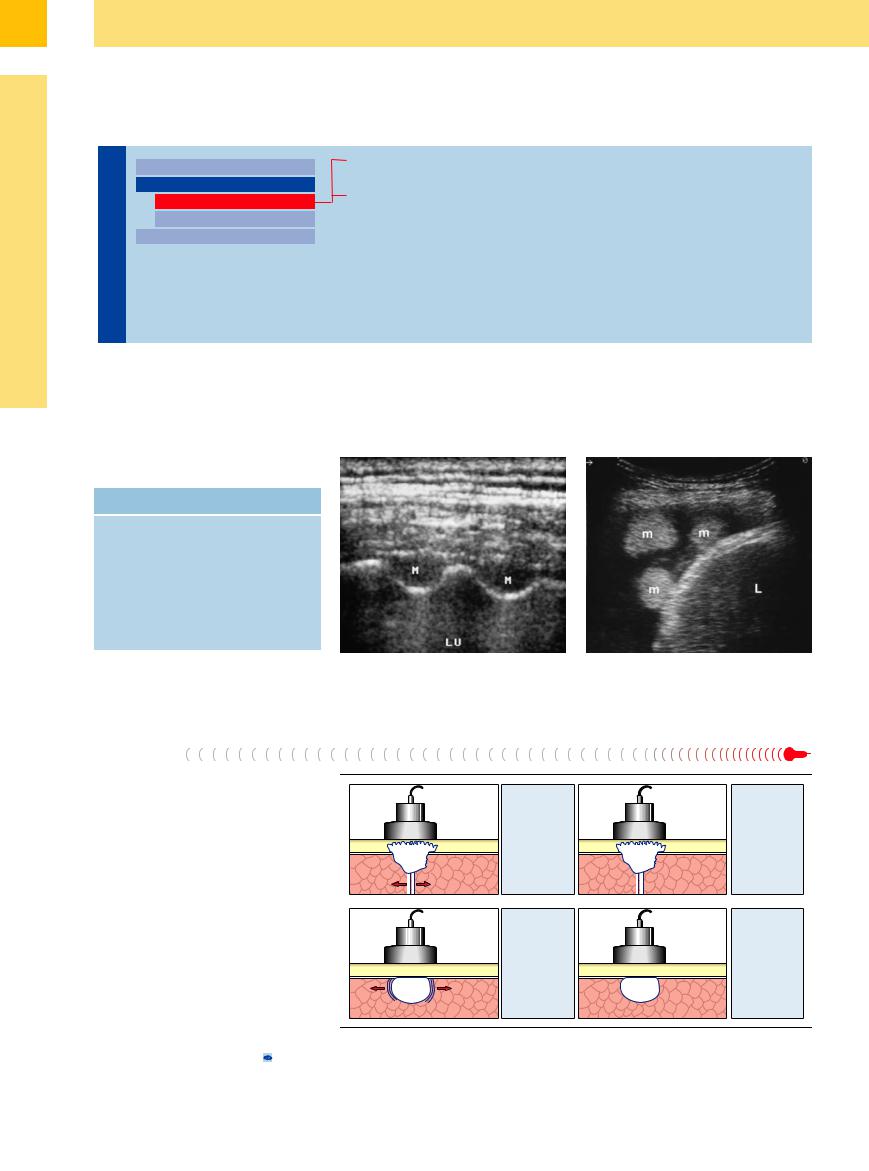
Focal nodular masses of the pleura are localized lesions that either originate from the pleura or are in intimate contact with it (Table 15.3). There may or may not be associated pleural effusion (Fig.15.6). If effusion is absent, the
Table 15.3 Differential diagnosis of focal nodular mass lesions of the pleura
Common |
Less common |
Metastases |
Mesothelioma |
Pleural plaque |
Lipoma |
|
Fibroma |
|
Fibrin bodies |
|
(in pleural e usion) |
|
Neurogenic tumors |
|
Loculated fluid |
|
Organized empyema |
lesions are usually located between the pleural |
A confident benign/malignant discrimina- |
layers. When pleural effusion is present, the |
tion is not possible on the basis of ultrasound |
lesion can be localized to the pleural layers |
findings alone. |
(Fig.15.7).6,7 |
|
Fig. 15.6 Pleural metastases (M) in a 43-year-old man with |
Fig. 15.7 Hypernephroma in a 61-year-old man. Scan |
hypernephroma. LU = lung. |
shows two echogenic round lesions (m) surrounded by |
|
pleural effusion on the right side of the diaphragm. L = |
|
liver. |
Metastases
Metastases are the most common type of focal pleural lesion. The most common primaries are bronchial carcinoma and breast cancer. The lesions may or may not be associated with pleural effusion.
Sonographic features. The lesions usually appear sonographically as round, sharply circumscribed nodules of variable echogenicity. They are frequently in contact with the parietal pleura ( 15.5a–c). Infiltration of the visceral pleura should be assumed if the lesion does not move with respiratory excursions in the absence of pleural effusion (Fig.15.8).3 Even so, differentiation from peripheral lung metastases cannot always be achieved. Subcostal transhepatic scans are best for demonstrating involvement of the diaphragmatic pleura (
15.5a–c). Infiltration of the visceral pleura should be assumed if the lesion does not move with respiratory excursions in the absence of pleural effusion (Fig.15.8).3 Even so, differentiation from peripheral lung metastases cannot always be achieved. Subcostal transhepatic scans are best for demonstrating involvement of the diaphragmatic pleura (
15.5 d–f). Color Doppler ultrasound can differ- |
Fig. 15.8 Technique for differentiating a mobile tumor from a fixed tumor.3 |
entiate between loculated fluid ( 15.5 g–l), |
|
518
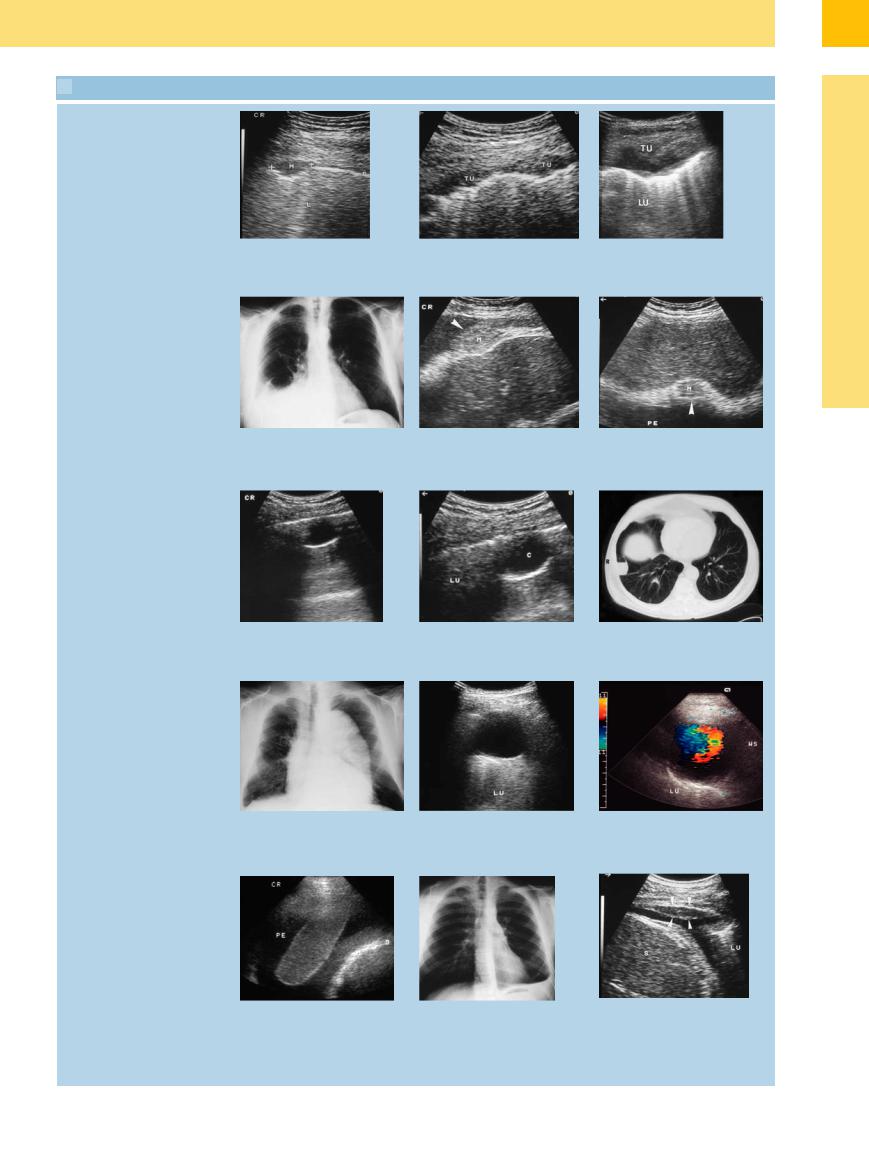
 15.5 Differential Diagnosis of Pleural Metastases
15.5 Differential Diagnosis of Pleural Metastases
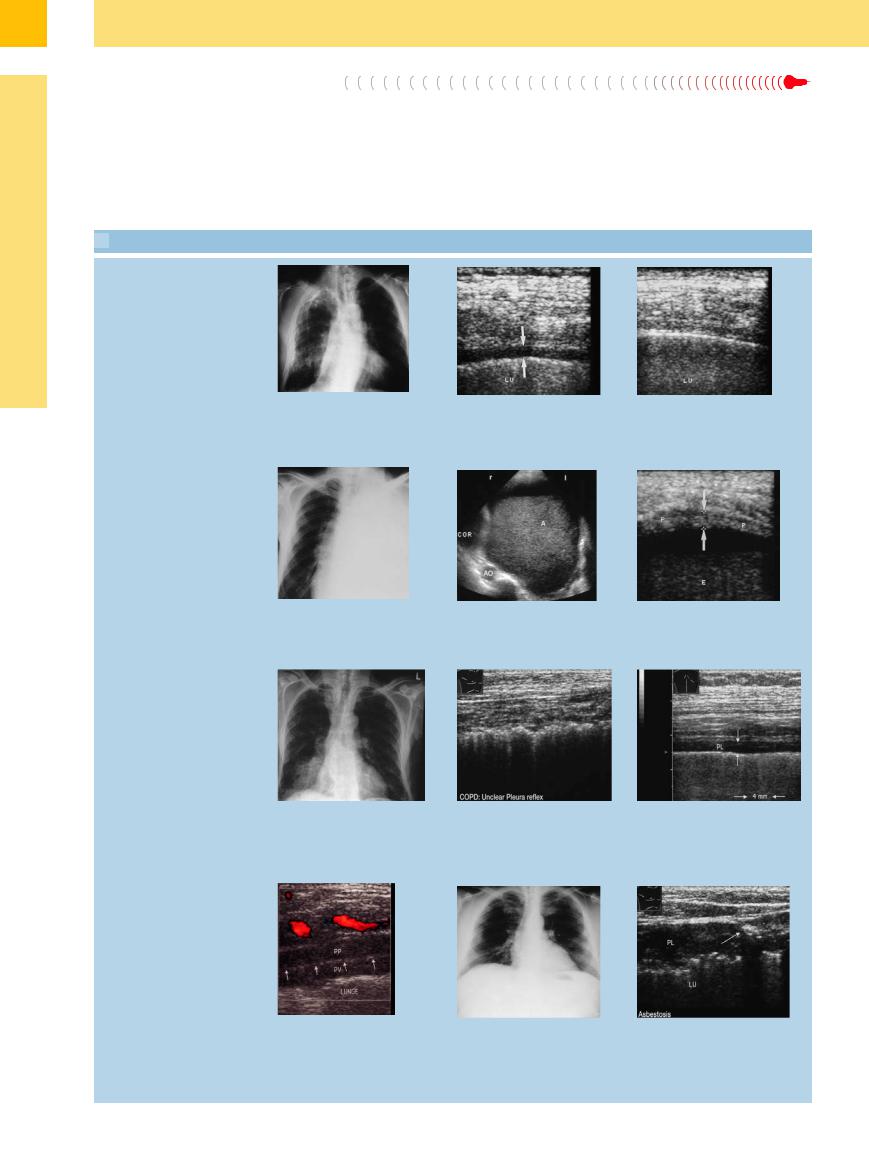
Pleural metastases
a–c Focal mass of the parietal pleura.
a Solitary nodular lesion (M), metastatic to breast carcinoma. L = lung.
Malignant mesothelioma
b Confluent nodular metastases (TU) from breast carcinoma.
c Large focal tumor (TU) invading the chest wall. Metastasis from breast carcinoma. LU = lung.
15
Parietal Pleura
d–f Malignant mesothelioma in a 76-year- old patient.
d Chest radiograph shows moderate pleural e usion on the right side.
e and f Right lateral intercostal scan and subcostal transhepatic scan show an echogenic tumor mass in the diaphragm (arrow). PE = pleural e usion.
Local fluid: pulmonary cyst
g–i Peripheral round lesion in a 64-year-old man. |
i CT appearance of the pulmonary cyst. |
g and h Rounded, sharply circumscribed, echo-free peripheral lesion (C), most likely a |
|
pulmonary cyst. LU = lung. |
|
Local fluid: aortic aneurysm
j–l A 67-year-old patient with mediastinal widening.
j Chest radiograph shows mediastinal widening.
Pleural e usion, fibrin body, pleural thickening
k and l B-mode image shows an elongated, echo-free structure on the pleural wall in the left posterior paravertebral region. Color Doppler image shows zones of arterial turbulence consistent with an aortic aneurysm on the posterior chest wall. The finding was confirmed by MRI. LU = lung; WS = spinal column.
m A 76-year-old man with exudative pleural e usion (PE) on the left side. Fibrin body appears as a homogeneous mass on the pleural wall, mobile in the pleural e usion. D = diaphragm.
n and o A 20-year-old man evaluated for pleural e usion.
n Chest radiograph: small pleural e usion on the left side, diagnostic puncture.
o Ultrasound 2 days after thoracentesis shows pleural thickening in the area of the puncture site (arrows), interpreted as a local reaction to needle insertion. The clinical course was consistent with a parainfectious e usion. LU = lung; S = spleen.
519
15
Pleura and Chest Wall
hematoma, and |
pleural fibrin bodies ( |
In rare cases, malignant mesothelioma can |
15.5 m), which are occasionally seen in fibrin- |
occur as a localized tumor that is indistinguish- |
|
rich exudative pleural effusions. The definitive |
able from pleural metastases or peripheral |
|
diagnosis is established by ultrasound-guided |
bronchial carcinoma by its ultrasound features. |
|
FNA ( 15.5n,o). |
|
|
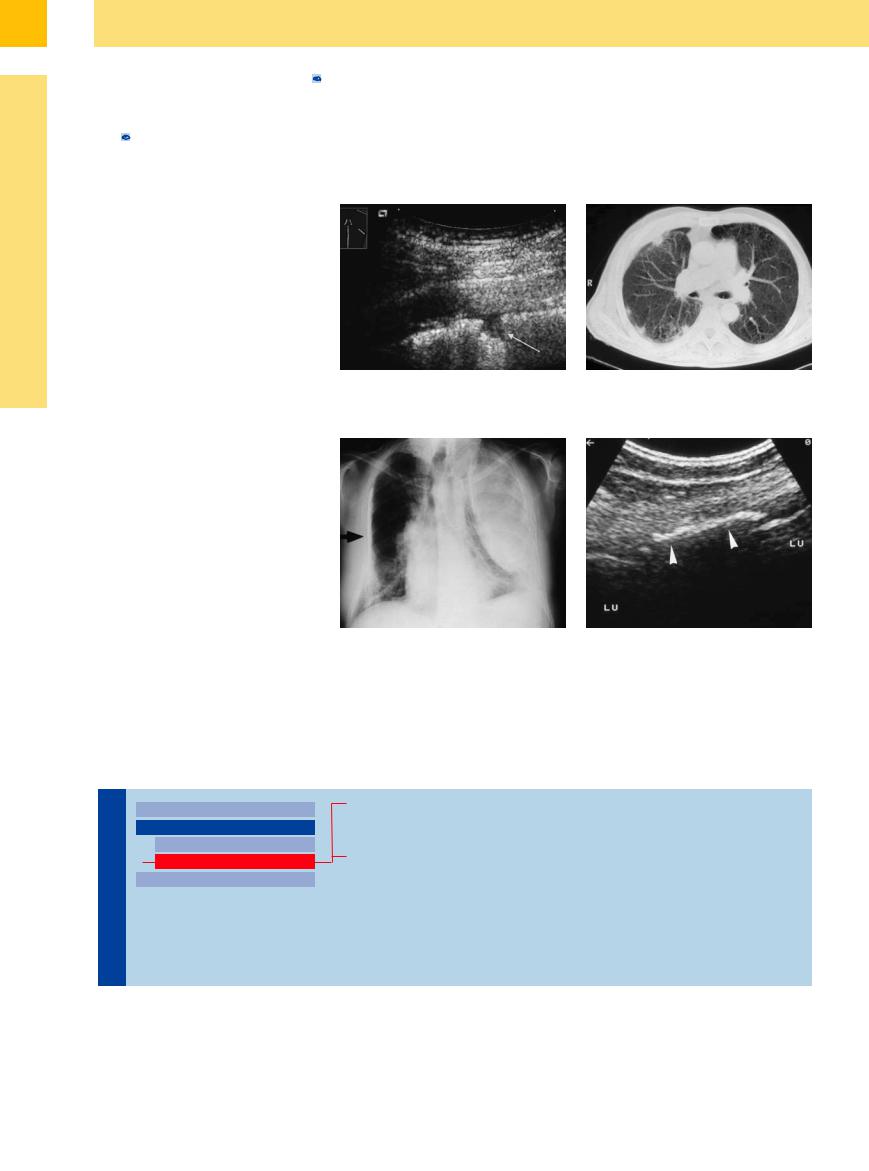
Pleural Plaque




















































Pleural plaques appear as focal hypoechoic lesions that represent the end stage of pneumonia, infarction, empyema, hematoma, tumor irradiation, or chemotherapy. They are also found in the setting of asbestos exposure and other pneumoconioses (Fig.15.9). Not infrequently, the pleural layers are adherent.
Sonographic features. At ultrasound the normally sharp pleural line appears irregular and fragmented. The lesions are mostly hypoechoic and oblong with ill-defined margins. The maximum thickness of the lesions is usually less than 5 mm.
Lesions of the visceral pleura cannot be distinguished from small peripheral pulmonary embolisms or pleurisy by their ultrasound features alone. The focal lesions can be localized to the visceral pleura, however, and the clinical presentation can further narrow the differential diagnosis.8 Differentiation from pleural carcinomatosis is generally difficult.
Calcifications. Localized calcifications are occasionally found on the pleural layers. They are observed after infections (e. g., tuberculosis), after trauma (e. g., fibrothorax), in pneumoconiosis (e. g., asbestosis), and also in hypercalcemia (e. g., renal failure) (Fig.15.10).
Fig. 15.9 A 57-year-old man with a history of asbestosis. a Ultrasound shows plaque-like areas of pleural thickening in addition to pleural nodules (arrow).
b CT appearance of the pleural plaques.
Fig. 15.10 Old pulmonary tuberculosis in a 70-year-old |
b Ultrasound shows localized pleural calcifications (ar- |
man. |
rowheads). LU = lung. |
a Chest radiograph shows a white hemithorax on the left |
|
side following surgical treatment of tuberculosis, with |
|
pleural calcifications on the right side. |
|
Diffuse Pleural Thickening
Pleura and Chest Wall

Chest Wall
Parietal Pleura
Nodular Masses
Diffuse Pleural Thickening
Pleural Effusion
Pleural Carcinomatosis
Pleural Fibrosis
Diffuse Malignant Mesothelioma
520
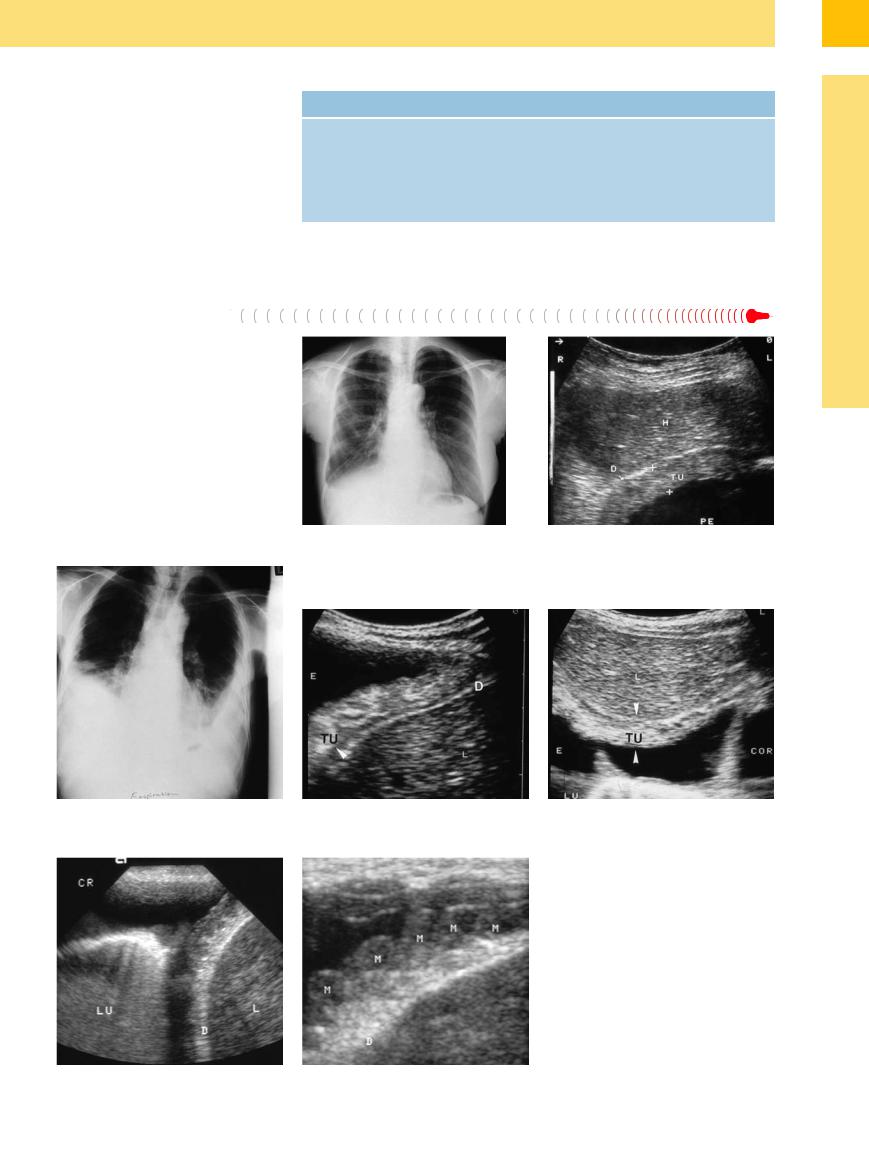
Table 15.4 Differential diagnosis of diffuse pleural thickening
Common |
Less common |
Pleural carcinomatosis |
Localized pleural e usion |
Chronic fibrosing pleurisy |
Asbestosis |
Di use malignant mesothelioma |
Connective tissue diseases |
|
Chronic empyema |
|
Tuberculosis |
|
Aspergillosis |
15
Parietal Pleura
Pleural carcinomatosis may present sonographically with pleural effusion, focal pleural metastases, or diffuse pleural thickening. The latter may occur with or without pleural effusion.
Ultrasound shows a homogeneous, hypoechoic or even hyperechoic, sheet-like tumor mass that is usually distributed along the parietal pleura (Fig.15.11, Fig.15.12). The margins are generally well-defined, but additional nodular lesions may occasionally be seen (Fig.15.13). The diagnosis is established by ul- trasound-guided thoracentesis.6,7
Fig. 15.11 A 38-year-old woman with breast carcinoma. a Chest radiograph shows a small pleural effusion on the right side.
b Subcostal transhepatic scan demonstrates pleural effusion (PE) and diffuse thickening of the parietal pleura (TU) consistent with pleural carcinomatosis. D = diaphragm; L = liver.
Fig. 15.12 A 69-year-old man with an ENT tumor.
a Chest radiograph shows bilateral pleural effusion.
b and c Right lateral intercostal scan (b) and subcostal transhepatic scan (c) show diffuse, hyperechoic thickening of the parietal pleura consistent with pleural carcinomatosis (TU). D = diaphragm; E = effusion; L = liver; LU = lung; COR = heart.
Fig. 15.13a and b Low-grade non-Hodgkin lymphoma in a 78-year-old man. Right lateral intercostal scan shows extensive pleural thickening in a string-of-beads pattern (M), consistent with lymphomatous infiltration. LU = lung; D = diaphragm; L = liver.
521
15
Pleura and Chest Wall
Pleural Fibrosis 









The pleural cavity may become diffusely permeated by fibrotic tissue during or after pneumonia and pleurisy and less commonly after a tuberculous effusion ( 15.6a–c), empyema (
15.6a–c), empyema ( 15.6 d–f), pulmonary fibrosis (
15.6 d–f), pulmonary fibrosis ( 15.6 g–j), asbestosis (
15.6 g–j), asbestosis ( 15.6k,l), or hemothorax. A concomitant exudative effusion is often present.
15.6k,l), or hemothorax. A concomitant exudative effusion is often present.
Sonographic features. Ultrasound usually demonstrates an extended area of hypoechoic pleural thickening. Generally the thickening is less than 5 mm. Typically both the parietal pleura and visceral pleura are thickened and, in the absence of pleural effusion, cannot be defined as separate layers.
 15.6 Various Causes of Pleural Fibrosis
15.6 Various Causes of Pleural Fibrosis
Tuberculosis
Pleural effusion. The pleural layers can be differentiated when pleural effusion is present. The effusion sometimes contains fibrin strands of varying extent ranging to a dense, honey- comb-like structure.
a–c Old pulmonary tuberculosis in a 75-year-old man.
a Chest radiograph shows scar changes in the right lung.
b Extensive pleural thickening (arrows). LU = lung.
c Normal pleura. LU = lung.
Pyothorax
d–f Pyothorax after pneumonectomy.
d Chest radiograph shows a white left hemithorax following pneumonectomy for bronchial carcinoma.
Pulmonary fibrosis
e and f Fluid with a layer of sediment (A). The pleura (P, arrows) shows extensive thickening. Percutaneous aspiration yielded pus consistent with pyothorax. AO = aorta; E = e usion.
gand h A 72-year-old man with chronic obstructive lung disease.
gChest radiograph shows signs of pulmonary emphysema with increased
markings in the right lower lung field.
h The entry echo shows extended irregularity with fine fibrotic changes.
i A 74-year-old man with known pulmonary fibrosis: di use thickening of the pleura (PL) to 4 mm (arrows).
Pulmonary fibrosis, asbestosis
j A 32-year-old woman with left pulmonary fibrosis of undetermined cause. Ultrasound shows di use thickening of the visceral (PV) and parietal (PP) pleura. The lung is immobile. The arrows mark the entry echo at the visceral–parietal interface.
k and l Asbestosis in a 53-year-old man.
k Chest radiograph shows bilateral opacities on the pleural wall.
l Ultrasound shows di use thickening of the pleura (PL) to 10 mm with focal calcifications (arrow). The lung (LU) is fixed.
522
