
- •Contents
- •Preface
- •Contributors
- •1 Vessels
- •1.1 Aorta, Vena Cava, and Peripheral Vessels
- •Aorta, Arteries
- •Anomalies and Variant Positions
- •Dilatation
- •Stenosis
- •Wall Thickening
- •Intraluminal Mass
- •Perivascular Mass
- •Vena Cava, Veins
- •Anomalies
- •Dilatation
- •Intraluminal Mass
- •Compression, Infiltration
- •1.2 Portal Vein and Its Tributaries
- •Enlarged Lumen Diameter
- •Portal Hypertension
- •Intraluminal Mass
- •Thrombosis
- •Tumor
- •2 Liver
- •Enlarged Liver
- •Small Liver
- •Homogeneous Hypoechoic Texture
- •Homogeneous Hyperechoic Texture
- •Regionally Inhomogeneous Texture
- •Diffuse Inhomogeneous Texture
- •Anechoic Masses
- •Hypoechoic Masses
- •Isoechoic Masses
- •Hyperechoic Masses
- •Echogenic Masses
- •Irregular Masses
- •Differential Diagnosis of Focal Lesions
- •Diagnostic Methods
- •Suspected Diagnosis
- •3 Biliary Tree and Gallbladder
- •3.1 Biliary Tree
- •Thickening of the Bile Duct Wall
- •Localized and Diffuse
- •Bile Duct Rarefaction
- •Localized and Diffuse
- •Bile Duct Dilatation and Intraductal Pressure
- •Intrahepatic
- •Hilar and Prepancreatic
- •Intrapancreatic
- •Papillary
- •Abnormal Intraluminal Bile Duct Findings
- •Foreign Body
- •The Seven Most Important Questions
- •3.2 Gallbladder
- •Changes in Size
- •Large Gallbladder
- •Small/Missing Gallbladder
- •Wall Changes
- •General Hypoechogenicity
- •General Hyperechogenicity
- •General Tumor
- •Focal Tumor
- •Intraluminal Changes
- •Hyperechoic
- •Hypoechoic
- •Nonvisualized Gallbladder
- •Missing Gallbladder
- •Obscured Gallbladder
- •4 Pancreas
- •Diffuse Pancreatic Change
- •Large Pancreas
- •Small Pancreas
- •Hypoechoic Texture
- •Hyperechoic Texture
- •Focal Changes
- •Anechoic Lesion
- •Hypoechoic Lesion
- •Isoechoic Lesion
- •Hyperechoic Lesion
- •Irregular (Complex Structured) Lesion
- •Dilatation of the Pancreatic Duct
- •Marginal/Mild Dilatation
- •Marked Dilatation
- •5 Spleen
- •Nonfocal Changes of the Spleen
- •Diffuse Parenchymal Changes
- •Large Spleen
- •Small Spleen
- •Focal Changes of the Spleen
- •Anechoic Mass
- •Hypoechoic Mass
- •Hyperechoic Mass
- •Splenic Calcification
- •6 Lymph Nodes
- •Peripheral Lymph Nodes
- •Head/Neck
- •Extremities (Axilla, Groin)
- •Abdominal Lymph Nodes
- •Porta Hepatis
- •Splenic Hilum
- •Mesentery (Celiac, Upper and Lower Mesenteric Station)
- •Stomach
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •Small/Large Intestine
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •8 Peritoneal Cavity
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Wall Structures
- •Smooth Margin
- •Irregular Margin
- •Intragastric Processes
- •Intraintestinal Processes
- •9 Kidneys
- •Anomalies, Malformations
- •Aplasia, Hypoplasia
- •Cystic Malformation
- •Anomalies of Number, Position, or Rotation
- •Fusion Anomaly
- •Anomalies of the Renal Calices
- •Vascular Anomaly
- •Diffuse Changes
- •Large Kidneys
- •Small Kidneys
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Irregular Structure
- •Circumscribed Changes
- •Anechoic Structure
- •Hypoechoic or Isoechoic Structure
- •Complex Structure
- •Hyperechoic Structure
- •10 Adrenal Glands
- •Enlargement
- •Anechoic Structure
- •Hypoechoic Structure
- •Complex Echo Structure
- •Hyperechoic Structure
- •11 Urinary Tract
- •Malformations
- •Duplication Anomalies
- •Dilatations and Stenoses
- •Dilated Renal Pelvis and Ureter
- •Anechoic
- •Hypoechoic
- •Hypoechoic
- •Hyperechoic
- •Large Bladder
- •Small Bladder
- •Altered Bladder Shape
- •Intracavitary Mass
- •Hypoechoic
- •Hyperechoic
- •Echogenic
- •Wall Changes
- •Diffuse Wall Thickening
- •Circumscribed Wall Thickening
- •Concavities and Convexities
- •12.1 The Prostate
- •Enlarged Prostate
- •Regular
- •Irregular
- •Small Prostate
- •Regular
- •Echogenic
- •Circumscribed Lesion
- •Anechoic
- •Hypoechoic
- •Echogenic
- •12.2 Seminal Vesicles
- •Diffuse Change
- •Hypoechoic
- •Circumscribed Change
- •Anechoic
- •Echogenic
- •Irregular
- •12.3 Testis, Epididymis
- •Diffuse Change
- •Enlargement
- •Decreased Size
- •Circumscribed Lesion
- •Anechoic or Hypoechoic
- •Irregular/Echogenic
- •Epididymal Lesion
- •Anechoic
- •Hypoechoic
- •Intrascrotal Mass
- •Anechoic or Hypoechoic
- •Echogenic
- •13 Female Genital Tract
- •Masses
- •Abnormalities of Size or Shape
- •Uterus
- •Abnormalities of Size or Shape
- •Myometrial Changes
- •Intracavitary Changes
- •Endometrial Changes
- •Fallopian Tubes
- •Hypoechoic Mass
- •Anechoic Cystic Mass
- •Solid Echogenic or Nonhomogeneous Mass
- •14 Thyroid Gland
- •Diffuse Changes
- •Enlarged Thyroid Gland
- •Small Thyroid Gland
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Circumscribed Changes
- •Anechoic
- •Hypoechoic
- •Isoechoic
- •Hyperechoic
- •Irregular
- •Differential Diagnosis of Hyperthyroidism
- •Types of Autonomy
- •15 Pleura and Chest Wall
- •Chest Wall
- •Masses
- •Parietal Pleura
- •Nodular Masses
- •Diffuse Pleural Thickening
- •Pleural Effusion
- •Anechoic Effusion
- •Echogenic Effusion
- •Complex Effusion
- •16 Lung
- •Masses
- •Anechoic Masses
- •Hypoechoic Masses
- •Complex Masses
- •Index
14
Diffuse Changes
b Longitudinal scan on the left side. The inferior thyroid artery has a blurry, rarefied appearance.
c and d Scant color-flow signals at a low PRF setting (same signal pattern seen at 0.05 m/s), indicating a slight decrease in vascularity. AC = common carotid artery; M = muscle.
Hypoechoic Structure
Gland |
|
|
Diffuse Changes |
||
|
|
|
|
||
|
|
|
|
|
Enlarged Thyroid Gland |
Thyroid |
|
|
|
Small Thyroid Gland |
|
|
|
|
Hypoechoic Structure |
||
|
|
|
|||
|
|
|
Hyperechoic Structure |
||
|
|
Circumscribed Changes |
|||
|
|||||
|
|
|
|
Differential Diagnosis of Hyperthyroidism |
|
|
|
|
|||
The diffuse hypoechoic thyroid changes described below are generally associated with a normal-sized thyroid gland.
Chronic Thyroiditis with Transient Hyperthyroidism, Postpartum Thyroiditis
Pregnany-Induced Thyroid Dysfunction Silent (Sporadic) Thyroiditis
Lithiumor Amiodarone-Induced Thyroiditis Interferon-Induced Thyroiditis
Chronic Thyroiditis with Transient  Hyperthyroidism,
Hyperthyroidism, Postpartum Thyroiditis
Postpartum Thyroiditis


















Both chronic thyroiditis with transient hyperthyroidism (juvenile) and postpartum thyroiditis are associated with a brief period of hyperthyroidism, which should not be treated with thyrostatic agents.
Postpartum, the prevalence of autoimmune diseases is increased; it may lead to a relapse of Graves hyperthyroidism or to a postpartum thyroiditis.
Postpartum thyroiditis generally develops during a brief interval after pregnancy, showing an average incidence of 5% (3–17%).8 It is associated with transient but persistent hyperthyroidism or hypothyroidism. Initially, in the first 2–3 months, there is often a hyperthyroidism which is either transient or remains constant, or in 50% of cases it can progress into hypothyroidism. Postpartum thyroiditis is negative for anti-TSH receptor antibodies but positive for anti-TPO antibodies. In most cases it resolves within 1 year.
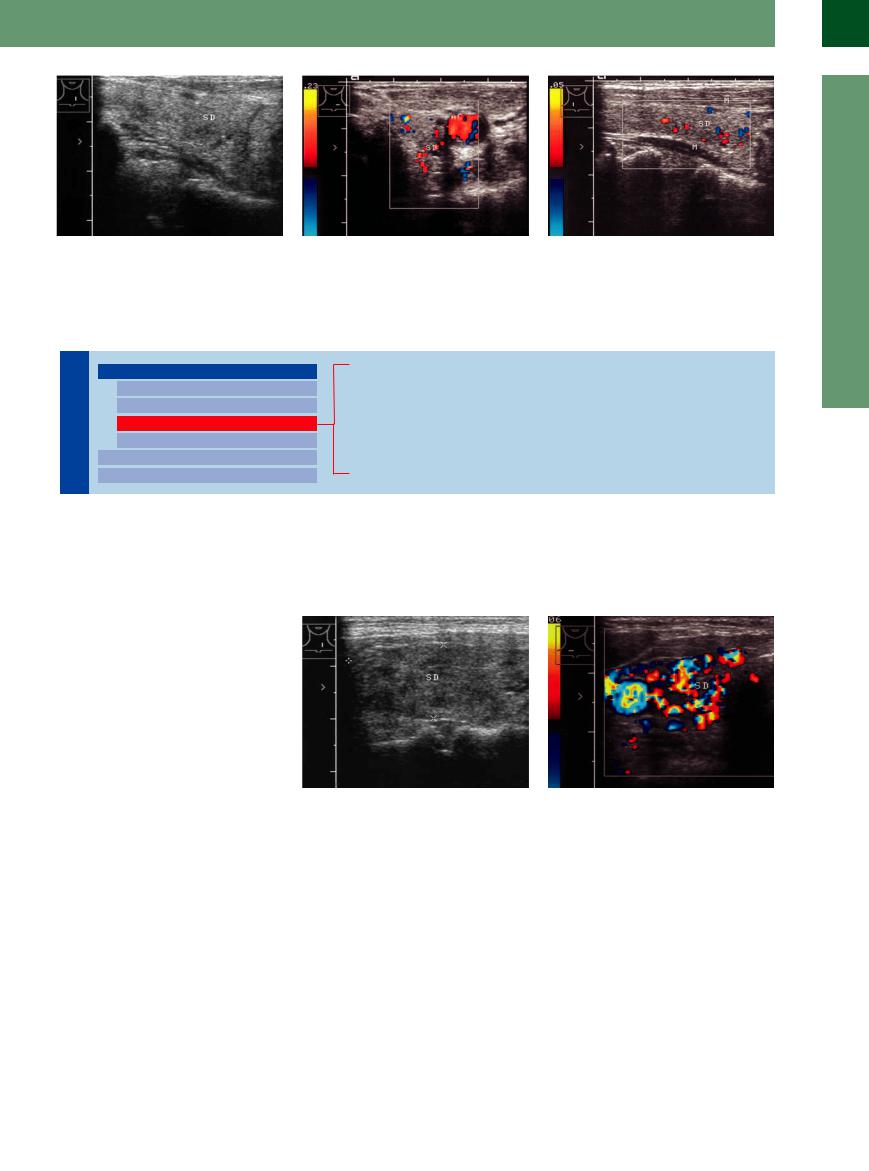
Fig. 14.26 Chronic thyroiditis with transient hyperthyroidism. Patient presented clinically with mild hyperthyroidism and no goiter. Anti-TPO and TRAbs negative, antithyroglobulin antibodies strongly positive.
a Thyroid (TH) with a patchy hypoechoic structure.
Ultrasound in both diseases shows diffuse or patchy hypoechoicity of the thyroid gland. Color duplex examination reveals increased
b Color Doppler: pronounced vascularity.
vascularity as the cause of the low echogenicity (Fig.14.26).
Pregnancy-Induced Thyroid Dysfunction
Dysfunction






































Pregnancy has a profound impact on the thyorid gland (increasing gland) and thyroid function (decreased TSH under human chorionic gonadotropin [hCG]). Postpartum thyroid dysfunction may be caused by a loss of iodine (50% increase in the daily iodine re-
quirement) and the resulting compensatory reaction of the thyroid. In early pregnancy subclinical hypothyroidism occurs in 15% of pregnant women; in hyperemesis gravidarum the TSH value is suppressed. An overintensive thyrostasis in newborns may result in a transitory Graves hyperthyroidism.
The following conditions must be differentiated:
●hCG-induced hyperthyroidism
●Graves hyperthyroidism
●Thyroid autonomy
●(More rarely) AIT
487
14
Thyroid Gland
Silent (Sporadic) Thyroiditis
Thyroiditis 












































This condition runs a subacute or chronic |
toms. Anti-TPO and antithyroglobulin antibod- |
thyroiditis. It is distinguished by low radio- |
course lasting from weeks to several months |
ies are elevated. Silent thyroiditis is also inter- |
tracer uptake in the thyroid. |
(years) with a self-limiting course. It is usually |
preted as a painless variant of de Quervain |
The ultrasound findings are nonspecific, |
associated with hyperthyroidism, rarely with |
thyroiditis, indistinguishable from postpartum |
showing hypoechoic transformation of the |
hypothyroidism, but presents no other symp- |
|
gland (Fig.14.27). |
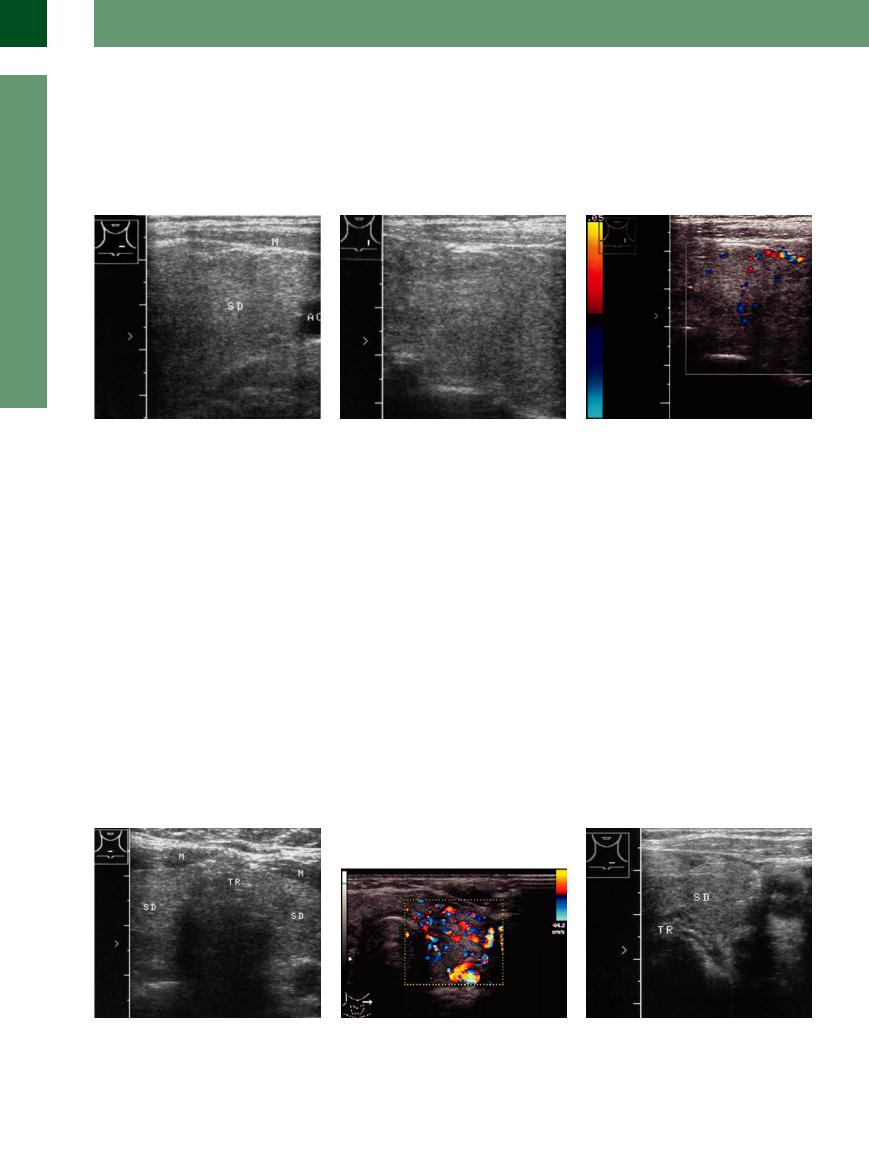
Fig. 14.27 Silent thyroiditis. Patient had mild hyperthyroidism, clinically asymptomatic and unchanged for years. TPO moderately elevated; TRAbs slightly elevated initially, now negative. Thyroid (TH) is slightly enlarged with a homogeneous, moderately hypoechoic structure.
a Transverse scan on the left side.
b Longitudinal scan on the left side.
c Color Doppler shows scant color-flow signals, contrasting with the hypervascularity in Graves disease or autoimmune hyperthyroidism (Fig. 14.13b,  14.1e,f,
14.1e,f,
 14.4q).
14.4q).
Lithiumor Amiodarone-Induced
Amiodarone-Induced Thyroiditis
Thyroiditis




































Lithium. Psychiatric patients who take lithium frequently develop a thyroid disorder. This may take the form of a goiter, hypothyroidism, or both. It is assumed that lithium incites a thyroid autoimmune response. Slight enlargement is relatively common and a frank autoimmune thyroiditis develops in about 10% of cases, but this percentage rises significantly in cases with preexisting thyroid disease. Anti-TPO and antithyroglobulin antibodies are elevated.
Sonographically, the thyroid shows diffuse hypoechoicity that increases if low echogenicity was already present (Fig.14.22, Fig.14.28).10
Amiodarone. Treatment with amiodarone is also commonly followed by hyperthyroidism or hypothyroidism with a (geographically
speaking) highly variable frequency. This may be based on the high iodine content of amiodarone and its structural similarity to the T3 and T4 hormones. Amiodarone has both agonistic and antagonistic effects on thyroid function. The fT4 (free T4) level rises by approximately 40%, while the serum fT3 level falls by about 50%, accompanied by a slight increase in the basal TSH.
Hyperthyroidism type I (with severe progression) is seen in preexisting nodular goiter or autonomy. Color Doppler (CDS) shows increased vascularity; definitive therapy is required.
Hyperthyroidism type II develops in a normal thyroid as well as in preexisting thyroiditis; transition to hypothyroidism is possible.
Amiodarone-induced hyperthyroidism is ultimately caused by an overload of iodine. The ultrasound findings are nonspecific and depend partly on a preexisting thyroid disorder. In Graves disease with latent autonomy, patients frequently develop overt hyperthyroidism. Patients with Hashimoto thyroiditis tend to develop frank hypothyroidism or an exacerbation of existing hypothyroidism. If the thyroid is normal before amiodarone therapy, the drug may trigger an autoimmune thyroiditis, which is also associated with a hypoechoic thyroid (Fig.14.29).
The changes are reversible after the drug is discontinued.
Fig. 14.28 Lithium-induced hypothyroidism. Besides minimal hypoechoicity, even color Doppler shows a normalappearing thyroid gland (TH). TR = trachea; M = muscle.
Fig. 14.29
a Amiodarone-induced hyperthyroidism: hypoechoic thyroid, marked vascularization (identical images also interferone-induced).
b Amiodarone-induced hypothyroidism: small, uniformly hypoechoic thyroid (SD). TR = trachea; AC = common carotid artery.
488
