
- •Contents
- •Preface
- •Contributors
- •1 Vessels
- •1.1 Aorta, Vena Cava, and Peripheral Vessels
- •Aorta, Arteries
- •Anomalies and Variant Positions
- •Dilatation
- •Stenosis
- •Wall Thickening
- •Intraluminal Mass
- •Perivascular Mass
- •Vena Cava, Veins
- •Anomalies
- •Dilatation
- •Intraluminal Mass
- •Compression, Infiltration
- •1.2 Portal Vein and Its Tributaries
- •Enlarged Lumen Diameter
- •Portal Hypertension
- •Intraluminal Mass
- •Thrombosis
- •Tumor
- •2 Liver
- •Enlarged Liver
- •Small Liver
- •Homogeneous Hypoechoic Texture
- •Homogeneous Hyperechoic Texture
- •Regionally Inhomogeneous Texture
- •Diffuse Inhomogeneous Texture
- •Anechoic Masses
- •Hypoechoic Masses
- •Isoechoic Masses
- •Hyperechoic Masses
- •Echogenic Masses
- •Irregular Masses
- •Differential Diagnosis of Focal Lesions
- •Diagnostic Methods
- •Suspected Diagnosis
- •3 Biliary Tree and Gallbladder
- •3.1 Biliary Tree
- •Thickening of the Bile Duct Wall
- •Localized and Diffuse
- •Bile Duct Rarefaction
- •Localized and Diffuse
- •Bile Duct Dilatation and Intraductal Pressure
- •Intrahepatic
- •Hilar and Prepancreatic
- •Intrapancreatic
- •Papillary
- •Abnormal Intraluminal Bile Duct Findings
- •Foreign Body
- •The Seven Most Important Questions
- •3.2 Gallbladder
- •Changes in Size
- •Large Gallbladder
- •Small/Missing Gallbladder
- •Wall Changes
- •General Hypoechogenicity
- •General Hyperechogenicity
- •General Tumor
- •Focal Tumor
- •Intraluminal Changes
- •Hyperechoic
- •Hypoechoic
- •Nonvisualized Gallbladder
- •Missing Gallbladder
- •Obscured Gallbladder
- •4 Pancreas
- •Diffuse Pancreatic Change
- •Large Pancreas
- •Small Pancreas
- •Hypoechoic Texture
- •Hyperechoic Texture
- •Focal Changes
- •Anechoic Lesion
- •Hypoechoic Lesion
- •Isoechoic Lesion
- •Hyperechoic Lesion
- •Irregular (Complex Structured) Lesion
- •Dilatation of the Pancreatic Duct
- •Marginal/Mild Dilatation
- •Marked Dilatation
- •5 Spleen
- •Nonfocal Changes of the Spleen
- •Diffuse Parenchymal Changes
- •Large Spleen
- •Small Spleen
- •Focal Changes of the Spleen
- •Anechoic Mass
- •Hypoechoic Mass
- •Hyperechoic Mass
- •Splenic Calcification
- •6 Lymph Nodes
- •Peripheral Lymph Nodes
- •Head/Neck
- •Extremities (Axilla, Groin)
- •Abdominal Lymph Nodes
- •Porta Hepatis
- •Splenic Hilum
- •Mesentery (Celiac, Upper and Lower Mesenteric Station)
- •Stomach
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •Small/Large Intestine
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •8 Peritoneal Cavity
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Wall Structures
- •Smooth Margin
- •Irregular Margin
- •Intragastric Processes
- •Intraintestinal Processes
- •9 Kidneys
- •Anomalies, Malformations
- •Aplasia, Hypoplasia
- •Cystic Malformation
- •Anomalies of Number, Position, or Rotation
- •Fusion Anomaly
- •Anomalies of the Renal Calices
- •Vascular Anomaly
- •Diffuse Changes
- •Large Kidneys
- •Small Kidneys
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Irregular Structure
- •Circumscribed Changes
- •Anechoic Structure
- •Hypoechoic or Isoechoic Structure
- •Complex Structure
- •Hyperechoic Structure
- •10 Adrenal Glands
- •Enlargement
- •Anechoic Structure
- •Hypoechoic Structure
- •Complex Echo Structure
- •Hyperechoic Structure
- •11 Urinary Tract
- •Malformations
- •Duplication Anomalies
- •Dilatations and Stenoses
- •Dilated Renal Pelvis and Ureter
- •Anechoic
- •Hypoechoic
- •Hypoechoic
- •Hyperechoic
- •Large Bladder
- •Small Bladder
- •Altered Bladder Shape
- •Intracavitary Mass
- •Hypoechoic
- •Hyperechoic
- •Echogenic
- •Wall Changes
- •Diffuse Wall Thickening
- •Circumscribed Wall Thickening
- •Concavities and Convexities
- •12.1 The Prostate
- •Enlarged Prostate
- •Regular
- •Irregular
- •Small Prostate
- •Regular
- •Echogenic
- •Circumscribed Lesion
- •Anechoic
- •Hypoechoic
- •Echogenic
- •12.2 Seminal Vesicles
- •Diffuse Change
- •Hypoechoic
- •Circumscribed Change
- •Anechoic
- •Echogenic
- •Irregular
- •12.3 Testis, Epididymis
- •Diffuse Change
- •Enlargement
- •Decreased Size
- •Circumscribed Lesion
- •Anechoic or Hypoechoic
- •Irregular/Echogenic
- •Epididymal Lesion
- •Anechoic
- •Hypoechoic
- •Intrascrotal Mass
- •Anechoic or Hypoechoic
- •Echogenic
- •13 Female Genital Tract
- •Masses
- •Abnormalities of Size or Shape
- •Uterus
- •Abnormalities of Size or Shape
- •Myometrial Changes
- •Intracavitary Changes
- •Endometrial Changes
- •Fallopian Tubes
- •Hypoechoic Mass
- •Anechoic Cystic Mass
- •Solid Echogenic or Nonhomogeneous Mass
- •14 Thyroid Gland
- •Diffuse Changes
- •Enlarged Thyroid Gland
- •Small Thyroid Gland
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Circumscribed Changes
- •Anechoic
- •Hypoechoic
- •Isoechoic
- •Hyperechoic
- •Irregular
- •Differential Diagnosis of Hyperthyroidism
- •Types of Autonomy
- •15 Pleura and Chest Wall
- •Chest Wall
- •Masses
- •Parietal Pleura
- •Nodular Masses
- •Diffuse Pleural Thickening
- •Pleural Effusion
- •Anechoic Effusion
- •Echogenic Effusion
- •Complex Effusion
- •16 Lung
- •Masses
- •Anechoic Masses
- •Hypoechoic Masses
- •Complex Masses
- •Index
10
Adrenal Glands
Fig. 10.19 Differential diagnosis: small, solid tumor on the upper pole of the left kidney. This lesion is definitely related to the kidney. Renal carcinoma.
Fig. 10.20 A rounded mass having the same echogenicity as the spleen is sometimes found in the splenic hilum or at the inferior border of the spleen. It is not a left adrenal mass but an accessory spleen.
Fig. 10.21 Trans-splenic scan of a large, hypovascular tumor of the pancreatic tail.
Complex Echo Structure
|
|
|
Enlargement |
||
Glands |
|||||
|
Anechoic Structure |
||||
|
Hypoechoic Structure |
||||
Adrenal |
|
Complex Echo Structure |
|||
|
|
|
|
||
|
|
|
|
Hyperechoic Structure |
|
Metastasis
Pheochromocytoma
Carcinoma
Metastasis































Metastases are the adrenal tumors that are |
stases have a complex, nonhomogeneous echo |
most frequently detected by ultrasound. Their |
structure and irregular margins (Figs. 10.22, |
appearance can be very diverse. Some meta- |
10.23, 10.24). The most common primary tu- |
mor is bronchial carcinoma. Other primary tumors have been mentioned above.
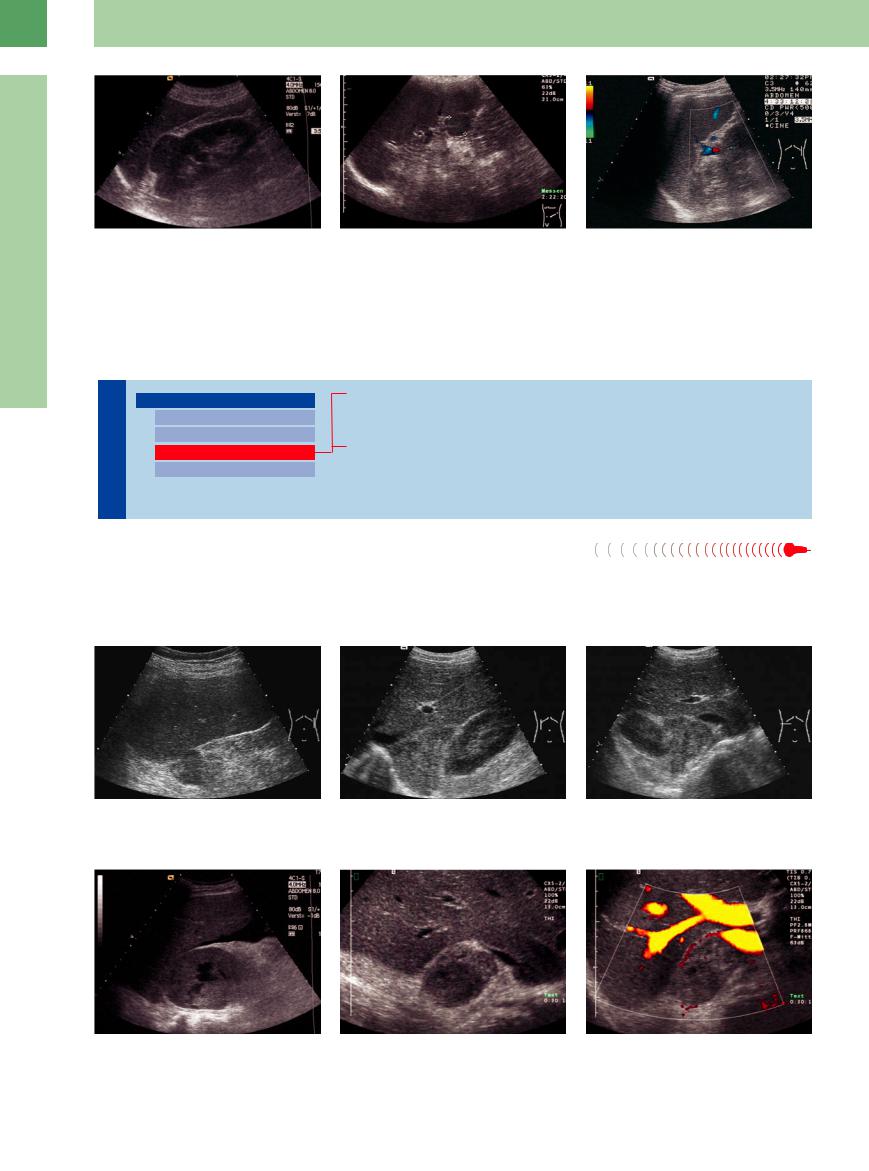
Fig. 10.22 Metastasis from advanced renal cell carcinoma in a left trans-splenic scan. Complex internal structure.
Fig. 10.23 Metastasis from bronchial carcinoma.
a Large, triangular mass with a complex echo structure located above the right kidney.
b Transverse scan shows a metastasis with a complex echo structure “wedged” between the kidney, inferior vena cava, right lobe of the liver, and spinal column.
Fig. 10.24
a Large metastasis from bronchial carcinoma on the right side, with a very nonhomogeneous internal structure. Solid components are seen along with liquid areas.
b and c Sonographically complex metastasis of a right bronchial carcinoma with hypoechoic parts. With color duplex only marginal vascularization is detectable.
374

Pheochromocytoma
Pheochromocytoma is a tumor of the adrenal medulla that is generally detected sonographically (80–90% of cases) following the appearance of clinical symptoms (hypertension and tachycardia caused by increased catecholamine secretion). Most pheochromocytomas are already several centimeters in diameter when diagnosed. They have smooth margins, a round shape, and a nonhomogeneous or complex echo structure. Hypoechoic liquid components
are also observed. A spectrum of appearances may be seen (Fig.10.25, Fig.10.26). Pheochromocytomas are bilateral in approximately 10% of cases and extra-adrenal in 10–20%. The “organ of Zuckerkandl” should be looked for at the level of the origin of the inferior mesenteric artery, anterior to the aorta. Other extra-adre- nal sites are the renal hilum, bladder wall, and thorax. Pheochromocytoma is occasionally
seen posterior to the renal vein in transverse scans.
Rarely, pheochromocytoma is diagnosed in the setting of multiple endocrine neoplasia (MEN). From 2% to 5% of pheochromocytomas are malignant.
Because of the risk of inciting a hypertensive crisis, fine-needle aspiration biopsy should definitely be avoided when a pheochromocytoma is suspected.
10
Enlargement
Fig. 10.25 Pheochromocytoma.
a Nonhomogeneous tumor with hypoechoic central parts (positive endocrine test, increased catecholamine secretion).
b Relative homogeneous echodense pheochromocytoma with hypoechoic margin (image courtesy of Dr. Christian Jenssen, Strausberg, Germany).
Fig. 10.26 Small, functionally active pheochromocytoma only 3 cm in diameter. Typical hyperechoic internal structure.
Carcinoma






















































Adrenal carcinoma is a very rare (1:17 million), highly malignant tumor with a poor prognosis. Carcinomas have a hypoechoic to complex echo structure that is usually nonhomogeneous. The tumors have irregular margins and
may infiltrate their surroundings. Adrenal carcinoma is indistinguishable sonographically from a metastasis, although the visualization of additional tumors can advance the differential diagnosis. Most adrenal carcinomas are
hormone-producing. The tumor is usually detected only after it has reached a considerable size (often > 8 cm). Intratumoral hemorrhage, necrotic foci, and calcifications may occur, adding to the variegated appearance (Fig.10.15).
Hyperechoic Structure
Glands |
Enlargement |
|
Lipoma, Myelolipoma |
|||
|
|
|
|
|||
|
|
|
|
Anechoic Structure |
|
Calcification |
|
|
|
|
Hypoechoic Structure |
|
Metastasis |
Adrenal |
|
Complex Echo Structure |
|
|||
|
|
Pheochromocytoma |
||||
|
|
|
|
|
||
|
|
|
|
Hyperechoic Structure |
|
|
|
|
|
|
|
Neuroblastoma |
|
|
|
|
|
|
||
|
|
|
|
|
|
|
Lipoma, Myelolipoma |
|
|
||||
Lipoma. A pure lipoma of the adrenal glands |
Myelolipoma. Adrenal myelolipoma has |
|||||
has smooth margins and high, homogeneous |
smooth margins and a homogeneous hyper- |
|||||
echogenicity. In contrast to the mixed tissues of |
echoic structure (Fig.10.27, Fig.10.28).12 It re- |
|||||
myolipoma, posterior acoustic shadowing does |
sembles a renal angiomyolipoma in its sono- |
|||||
not occur. Lipoma is rare and shows no prolif- |
graphic features. Posterior acoustic shadowing |
|||||
erative tendency. |
is often present. Malignant transformation is |
|||||
not known to occur. The tumor consists histologically of fat and bone marrow tissue (hematopoietic cells and reticular cells). Intratumoral hemorrhage and calcifications may be seen.
375

10
Adrenal Glands
glands is characterized by a typical echo complex with a posterior acoustic shadow (Fig.10.29). Calcifications can result from a retained intra-adrenal hemorrhage or prior inflammatory process (e. g., tuberculosis). Patients occasionally show the clinical manifestations of Addison disease. Calcifications can also develop in tumors, however (carcinoma, metastases, pheochromocytoma, adenoma).
Fig. 10.27 Homogeneous, sharply circumscribed, hyperechoic tumor adjacent to the right kidney. Classic adrenal lipoma.
fFig. 10.28 Hyperechoic, homogeneous tumor above the right kidney represents a myelolipoma of the adrenal gland. Differentiation is mainly required from a renal angiomyolipoma.
Fig. 10.29 Exactly delineated calcification with acoustic shadow behind the right liver lobe and above the upper kidney pole concurs with a calcification of the adrenal gland as can occur after tuberculosis.
Metastasis































Metastases can have a variety of ultrasound appearances, including high echogenicity. They tend to have irregular margins and a nonhomogeneous internal structure (Figs. 10.30, 10.31, 10.32, 10.33). The most common primary tumor is bronchial carcinoma, which is associated with adrenal metastases in up to 25% of cases.
Fig. 10.30 Hyperechoic, relatively homogeneous metastasis from breast carcinoma (image courtesy of Dr. B. Frentzel-Beyme, Berlin, Germany).
Fig. 10.31 Large, hyperechoic, nonhomogeneous tumor of the right adrenal gland with small calcifications: adrenal gland metastasis of a bronchial carcinoma; a partially visible portal vein in the liver.
Fig. 10.32 Longitudinal scan shows a nonhomogeneous, hyperechoic tumor above the right kidney: metastasis from bronchial carcinoma (image courtesy of Dr. B. Frent- zel-Beyme, Berlin, Germany).
Fig. 10.33 An adrenal metastasis (e. g., bronchial carcinoma) can also appear hyperechoic, but it usually has a nonhomogeneous internal structure with irregular margins.
Pheochromocytoma
Pheochromocytomas typically have a complex echo structure with hypoechoic elements, but some appear hyperechoic. The descriptions given earlier under “Complex Echo Structure” also apply to the hyperechoic variant.
376
Neuroblastoma 









Neuroblastoma, like pheochromocytoma, arises from cells of the adrenal medulla. Next to Wilms tumor, it is the most common malignant abdominal tumor in children. Approximately 70% of neuroblastomas are located in the adrenal glands, the rest occurring at other sites in the sympathetic chain. Most neuroblas-
tomas are very large and predominantly hyperechoic. Some may have cystic elements (due to hemorrhage) and calcifications. Laboratory tests usually show an increase in catecholamine secretion.
Considerably less common are benign neural tumors such as ganglioneuromas. They have
been described only sporadically in the adrenal glands, occurring more commonly in the posterior mediastinum and at paravertebral sites.
Tips, tricks, and pitfalls
Most anatomic depictions place the adrenal gland close to the upper pole of the kidney, slightly tilted to the medial side. This, however, applies only to newborns and children. In adults, they are more or less distinguishable from the fatty tissue of the kidney and the surrounding fat
References
[1]Dietrich CF, Wehrmann T, Hoffmann C, Herrmann G, Caspary WF, Seifert H. Detection of the adrenal glands by endoscopic or transabdominal ultrasound. Endoscopy 1997; 29(9):859–864
[2]Frentzel-Beyme B, Nürnberg D. Sonographie der Nebenschilddrüse und der Nebenniere [Sonography of parathyroid and adrenal gland]. Praxis (Bern 1994) 2006;95:737–740
[3]Jenssen C, Dietrich CF. Sonografie und Endosonografie der Nebennieren [Ultrasound and endoscopic ultrasound of the adrenal glands]. Ultraschall Med 2010;31(3):228–250
[4]Braun B. Nebennieren. In: Braun B, Günther R, Schwerk WB. Ultraschalldiagnostik. Lehrbuch und Atlas. Landshut: Ecomed, 1983
[5]Schmidt G. Thieme Clinical Companions: Ultrasound. Stuttgart: Thieme, 2006
of the gland itself. Further important information in locating the glands, especially if they are enlarged, is that the right gland extends below the inferior vena cava and the left gland is between the upper kidney hilum and the aorta. The enlarged left adrenal gland can be mistaken for a
[6]Trojan J, Schwarz W, Sarrazin C, Thalhammer A, Vogl TJ, Dietrich CF. Role of ultrasonography in the detection of small adrenal masses. Ultraschall Med 2002;23(2):96–100
[7]Burton S, Ros PR. Adrenal Glands. In: Stark D, Bradley WG (eds.). Magnetic Resonance Imaging. Philadelphia: Mosby, 1999
[8]Allolio B, Schulte HM. Praktische Endokrinologie. Munich: Urban & Schwarzenberg, 1996
[9]Lam KY, Lo CY. Metastatic tumours of the adrenal glands: a 30-year experience in a teaching hospital. Clin Endocrinol (Oxf) 2002;56(1):95–101
[10]Allolio B. Adrenal incidentalomas. In: Margio-
ris AN, Chrousos CG, Eds. Adrenal Disorders. Totowa, NJ: Humana Press, 2001:
pp. 249–261
[11]Görg C, Schwerk WB, Bittinger A, et al. Sonographisch gesteuerte Feinnadelpunktion von Nebennierentumoren [Sonographically guided fine-needle puncture of adrenal tumors]. Dtsch Med Wochenschr 1992;117: 448–454
para-aortic lymph node. With this knowledge, the glands are easy to locate in the respective sections. It is essential to demonstrate the adrenal glands as part of a tumor staging or in a follow-up examination in metastasized lung and bronchial carcinomas as well as breast cancer.
[12]Fröhlich E, Rufle W, Strunk H, Stuckmann G, Seeliger H. Stellenwert der Feinnadelpunktion bei Nebennierentumoren [The value of fine needle puncture in adrenal gland tumors]. Ultraschall Med 1995;16(2):90–93
[13]Reincke M, Allolio B. Das Nebenniereninzidentalom: Die Kunst der Beschränkung in Diagnostik und Therapie. Dtsch Ärztebl 1995;92:A764–A770
[14]Nürnberg D. Sonographie von Nebennieren- tumoren—wann ist die Punktion indiziert? [Ultrasound of adrenal gland tumours and indications for fine needle biopsy (uFNB)]. Ultraschall Med 2005;26:458–469
[15]Mantero F, Arnaldi G. Management approaches to adrenal incidentalomas. A view from Ancona, Italy. Endocrinol Metab Clin North Am 2000;29(1):107–125, ix
10
Enlargement
377

