
- •Contents
- •Preface
- •Contributors
- •1 Vessels
- •1.1 Aorta, Vena Cava, and Peripheral Vessels
- •Aorta, Arteries
- •Anomalies and Variant Positions
- •Dilatation
- •Stenosis
- •Wall Thickening
- •Intraluminal Mass
- •Perivascular Mass
- •Vena Cava, Veins
- •Anomalies
- •Dilatation
- •Intraluminal Mass
- •Compression, Infiltration
- •1.2 Portal Vein and Its Tributaries
- •Enlarged Lumen Diameter
- •Portal Hypertension
- •Intraluminal Mass
- •Thrombosis
- •Tumor
- •2 Liver
- •Enlarged Liver
- •Small Liver
- •Homogeneous Hypoechoic Texture
- •Homogeneous Hyperechoic Texture
- •Regionally Inhomogeneous Texture
- •Diffuse Inhomogeneous Texture
- •Anechoic Masses
- •Hypoechoic Masses
- •Isoechoic Masses
- •Hyperechoic Masses
- •Echogenic Masses
- •Irregular Masses
- •Differential Diagnosis of Focal Lesions
- •Diagnostic Methods
- •Suspected Diagnosis
- •3 Biliary Tree and Gallbladder
- •3.1 Biliary Tree
- •Thickening of the Bile Duct Wall
- •Localized and Diffuse
- •Bile Duct Rarefaction
- •Localized and Diffuse
- •Bile Duct Dilatation and Intraductal Pressure
- •Intrahepatic
- •Hilar and Prepancreatic
- •Intrapancreatic
- •Papillary
- •Abnormal Intraluminal Bile Duct Findings
- •Foreign Body
- •The Seven Most Important Questions
- •3.2 Gallbladder
- •Changes in Size
- •Large Gallbladder
- •Small/Missing Gallbladder
- •Wall Changes
- •General Hypoechogenicity
- •General Hyperechogenicity
- •General Tumor
- •Focal Tumor
- •Intraluminal Changes
- •Hyperechoic
- •Hypoechoic
- •Nonvisualized Gallbladder
- •Missing Gallbladder
- •Obscured Gallbladder
- •4 Pancreas
- •Diffuse Pancreatic Change
- •Large Pancreas
- •Small Pancreas
- •Hypoechoic Texture
- •Hyperechoic Texture
- •Focal Changes
- •Anechoic Lesion
- •Hypoechoic Lesion
- •Isoechoic Lesion
- •Hyperechoic Lesion
- •Irregular (Complex Structured) Lesion
- •Dilatation of the Pancreatic Duct
- •Marginal/Mild Dilatation
- •Marked Dilatation
- •5 Spleen
- •Nonfocal Changes of the Spleen
- •Diffuse Parenchymal Changes
- •Large Spleen
- •Small Spleen
- •Focal Changes of the Spleen
- •Anechoic Mass
- •Hypoechoic Mass
- •Hyperechoic Mass
- •Splenic Calcification
- •6 Lymph Nodes
- •Peripheral Lymph Nodes
- •Head/Neck
- •Extremities (Axilla, Groin)
- •Abdominal Lymph Nodes
- •Porta Hepatis
- •Splenic Hilum
- •Mesentery (Celiac, Upper and Lower Mesenteric Station)
- •Stomach
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •Small/Large Intestine
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •8 Peritoneal Cavity
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Wall Structures
- •Smooth Margin
- •Irregular Margin
- •Intragastric Processes
- •Intraintestinal Processes
- •9 Kidneys
- •Anomalies, Malformations
- •Aplasia, Hypoplasia
- •Cystic Malformation
- •Anomalies of Number, Position, or Rotation
- •Fusion Anomaly
- •Anomalies of the Renal Calices
- •Vascular Anomaly
- •Diffuse Changes
- •Large Kidneys
- •Small Kidneys
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Irregular Structure
- •Circumscribed Changes
- •Anechoic Structure
- •Hypoechoic or Isoechoic Structure
- •Complex Structure
- •Hyperechoic Structure
- •10 Adrenal Glands
- •Enlargement
- •Anechoic Structure
- •Hypoechoic Structure
- •Complex Echo Structure
- •Hyperechoic Structure
- •11 Urinary Tract
- •Malformations
- •Duplication Anomalies
- •Dilatations and Stenoses
- •Dilated Renal Pelvis and Ureter
- •Anechoic
- •Hypoechoic
- •Hypoechoic
- •Hyperechoic
- •Large Bladder
- •Small Bladder
- •Altered Bladder Shape
- •Intracavitary Mass
- •Hypoechoic
- •Hyperechoic
- •Echogenic
- •Wall Changes
- •Diffuse Wall Thickening
- •Circumscribed Wall Thickening
- •Concavities and Convexities
- •12.1 The Prostate
- •Enlarged Prostate
- •Regular
- •Irregular
- •Small Prostate
- •Regular
- •Echogenic
- •Circumscribed Lesion
- •Anechoic
- •Hypoechoic
- •Echogenic
- •12.2 Seminal Vesicles
- •Diffuse Change
- •Hypoechoic
- •Circumscribed Change
- •Anechoic
- •Echogenic
- •Irregular
- •12.3 Testis, Epididymis
- •Diffuse Change
- •Enlargement
- •Decreased Size
- •Circumscribed Lesion
- •Anechoic or Hypoechoic
- •Irregular/Echogenic
- •Epididymal Lesion
- •Anechoic
- •Hypoechoic
- •Intrascrotal Mass
- •Anechoic or Hypoechoic
- •Echogenic
- •13 Female Genital Tract
- •Masses
- •Abnormalities of Size or Shape
- •Uterus
- •Abnormalities of Size or Shape
- •Myometrial Changes
- •Intracavitary Changes
- •Endometrial Changes
- •Fallopian Tubes
- •Hypoechoic Mass
- •Anechoic Cystic Mass
- •Solid Echogenic or Nonhomogeneous Mass
- •14 Thyroid Gland
- •Diffuse Changes
- •Enlarged Thyroid Gland
- •Small Thyroid Gland
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Circumscribed Changes
- •Anechoic
- •Hypoechoic
- •Isoechoic
- •Hyperechoic
- •Irregular
- •Differential Diagnosis of Hyperthyroidism
- •Types of Autonomy
- •15 Pleura and Chest Wall
- •Chest Wall
- •Masses
- •Parietal Pleura
- •Nodular Masses
- •Diffuse Pleural Thickening
- •Pleural Effusion
- •Anechoic Effusion
- •Echogenic Effusion
- •Complex Effusion
- •16 Lung
- •Masses
- •Anechoic Masses
- •Hypoechoic Masses
- •Complex Masses
- •Index
11
Urinary Tract
■ Wall Changes
Diffuse Wall Thickening
Tract |
|
|
Malformations |
|
|
|
|
|
|
|
Dilated Renal Pelvis and Ureter |
|
|
|
|
|
|
|
Renal Pelvic Mass, Ureteral Mass |
Urinary |
|
|
|
|
|
Changes in Bladder Size or Shape |
|
|
|
|
|
|
|
|
Intracavitary Mass |
|
|
|
|
|
|
|
Wall Changes |
|
|
||
|
|
|
Diffuse Wall Thickening |
|
|
|
Circumscribed Wall Thickening |
|
|
|
Concavities and Convexities |
Bladder-Wall Hypertrophy
Flat Bladder Tumor
Bladder-Wall Hypertrophy
Hypertrophy 













































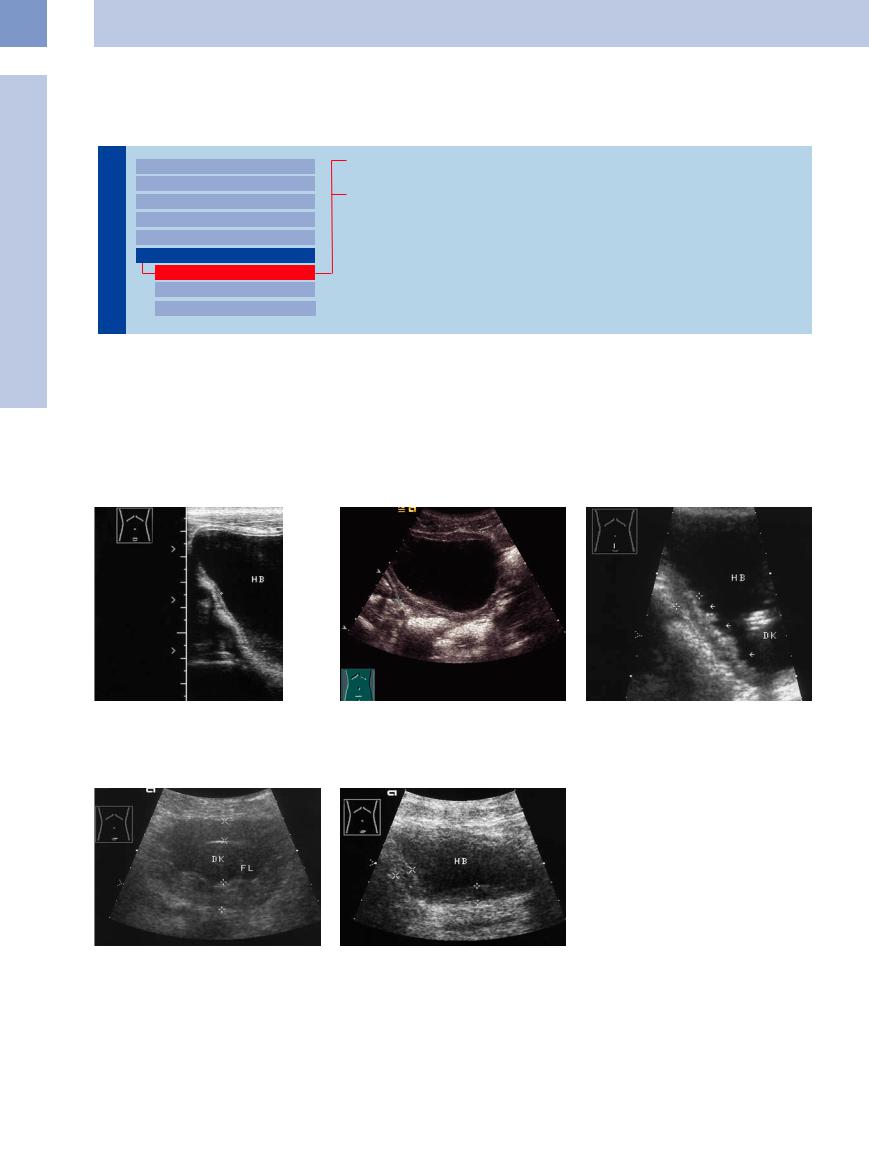
The normal wall thickness of a distended blad- |
inflammations (e. g., after prolonged catheter- |
distension may be misinterpreted as diffuse |
der is 1–3 mm and does not exceed 5 mm |
ization) or schistosomiasis in some regions, but |
wall thickening (Fig.11.94). In children, ure- |
(Fig.11.91). |
it most commonly results from infravesical ob- |
thral valves may also cause wall thickening |
Diffuse bladder-wall hypertrophy greater |
struction, often combined with pseudodiverti- |
and urinary stasis by subvesical stenosis. |
than 5 mm may be found in association with |
cula (Fig.11.92, Fig.11.93). Inadequate bladder |
|
Fig. 11.91 Normal three-layered wall (cursors) of a welldistended bladder (HB).
Fig. 11.92 Diffuse bladder-wall thickening secondary to an infravesical prostatic obstruction.
a Bladder-wall thickening without a pseudodiverticulum (cursors).
b Diffuse wall thickening with pseudodiverticulum (arrows). DK = echogenic indwelling catheter.
Fig. 11.93 Massive wall thickening, measuring up to 20 mm at some sites and exceeding the wall thickness of an empty bladder (compare with Fig. 11.94). IC = indwelling catheter. FL = urinary fluid.
f Fig. 11.94 Apparent diffuse wall thickening (cursors) in a partially distended bladder (HB).
410
Flat Bladder Tumor 

















































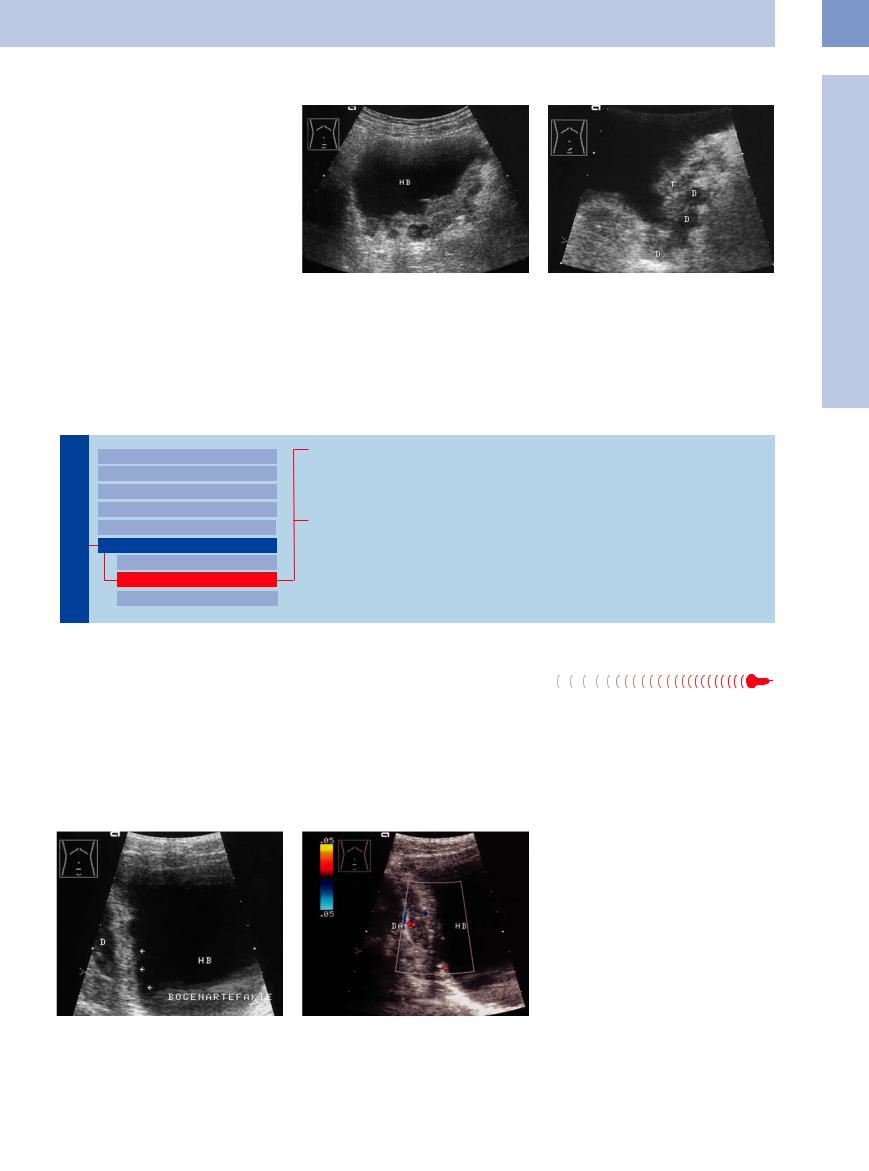
It can be difficult or impossible to distinguish diffuse bladder-wall hypertrophy from a carcinoma, sarcoma, or lymphoma that has formed a plaque-like growth on the bladder wall.
If ultrasound raises suspicion of a flat carcinoma on the bladder wall, further tests such as cystoscopy, radiography, and CT should be carried out (Fig.11.95).
Fig. 11.95 Plaque-like bladder tumor (histology: papillary |
b Tumor-encased diverticula (D). The internal echoes are |
urothelial carcinoma, probably a diverticular tumor). |
caused by tumor tissue inside the diverticula. T = tumor. |
a Tumor has spread over the bladder floor and (in other |
|
planes) into both sidewalls, almost extending to the blad- |
|
der roof on the left side. HB = bladder. |
|
Circumscribed Wall Thickening
Urinary Tract
Malformations
Dilated Renal Pelvis and Ureter Renal Pelvic Mass, Ureteral Mass Changes in Bladder Size or Shape Intracavitary Mass
Wall Changes
Diffuse Wall Thickening Circumscribed Wall Thickening Concavities and Convexities
Bladder-Wall Hypertrophy
Bladder-Wall Edema
Bladder Carcinoma
Blood Clots
Bladder-Wall Hypertrophy
Hypertrophy 






















Bladder-wall hypertrophy is the most frequent |
They most commonly occur on the bladder |
cause of circumscribed bladder-wall thickening |
floor and sidewalls, rarely affecting the bladder |
demonstrated by ultrasound. The wall thick- |
roof (Fig.11.96, Fig.11.97). |
ness often exceeds 7 mm in cases due to infra- |
Sites of inflammatory wall thickening due to |
vesical obstruction. Pseudodiverticula gener- |
infiltration from adjacent organs, as in Crohn |
ally appear as anechoic, usually multiple, sharp |
disease of the terminal ileum or peridiverticu- |
or rounded protrusions of the bladder wall. |
litis, are not uncommon. |
The differential diagnosis should include clots or sludge adherent to the bladder wall, a flat circumscribed tumor, and especially a faulty examination technique with inadequate bladder filling.
Fig. 11.96 Wall hypertrophy in a trabeculated bladder with incipient pseudodiverticula. HB = bladder.
a B-mode image, lower abdominal transverse scan: relatively long, serrated area of circumscribed wall thickening (arrows) with adherent, fluid-filled bowel segment (D). Tumor was excluded by cystoscopy. Side-lobe artifacts are also visible.
b Color Doppler shows scattered vascular spots but no tumor vascularity. DA = bowel wall.
11
Wall Changes
411
11
Urinary Tract
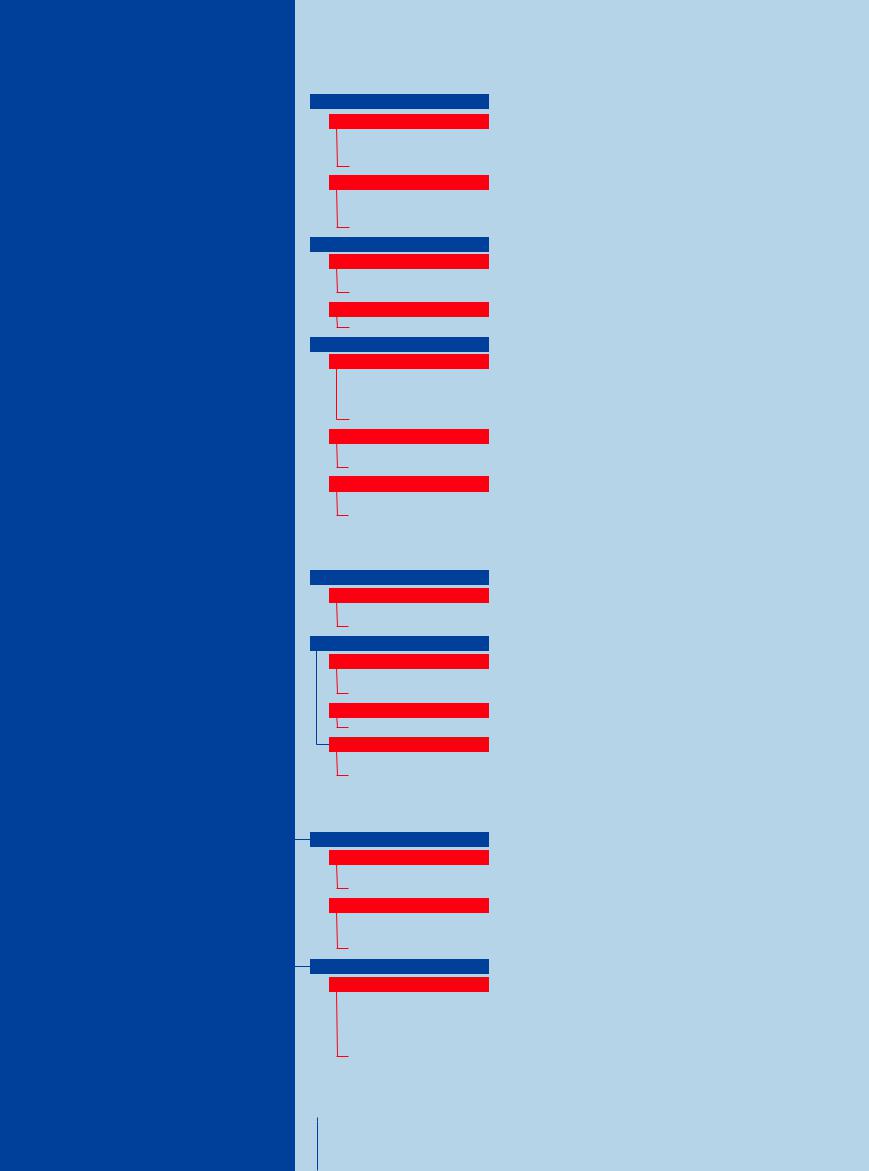
Fig. 11.97 Circumscribed wall thickening on the bladder floor, raising suspicion of a tumor. HB = bladder.
a Lower abdominal transverse scan. Color Doppler shows no vessels. PR = prostate.
b Longitudinal scan shows a polypoid tumor mass (arrow). P = prostate. Cystoscopy showed a trabeculated bladder due to BPH.
Bladder-Wall Edema
Edema

















































Circumscribed bladder-wall edema is usually based on mechanical irritation and inflammation from a bladder catheter, and so generally the cause is apparent.
Bladder Carcinoma 

















































The most important sonographic diagnosis is a flat, circumscribed carcinoma of the bladder wall. It is occasionally difficult to distinguish from bladder-wall hypertrophy. Tumor spread through the bladder wall to neighboring organs, especially adjacent bowel segments (e. g., the sigmoid colon), and the presence of lymph node metastases prove that the lesion is a malignant process. Conversely, it is not uncommon to find bladder invasion by tumors in adjacent organs, such as ovarian or rectosigmoid cancer.
Flat, circumscribed bladder carcinoma most commonly occurs on the bladder floor in the
area of the trigone and ureteral orifices, leading to ureteral obstruction (Figs. 11.99, 11.100, 11.101).
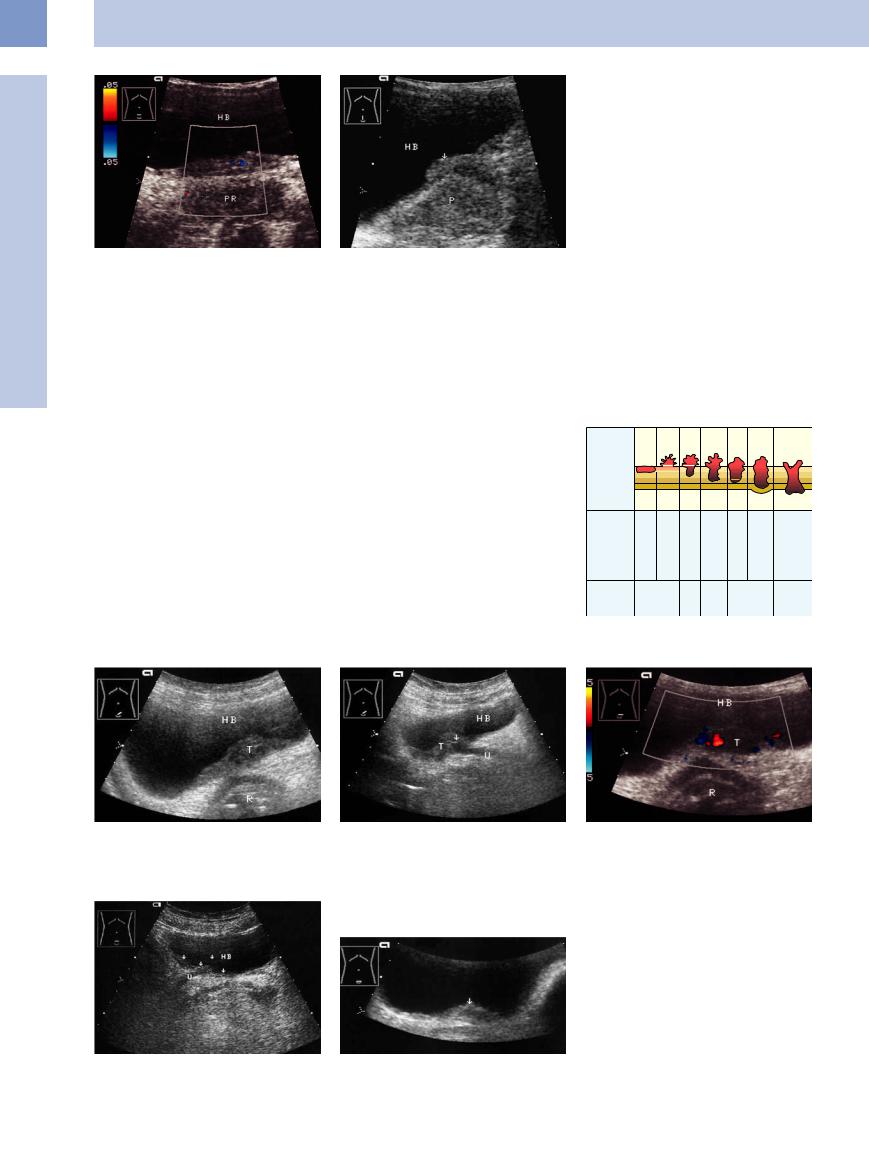
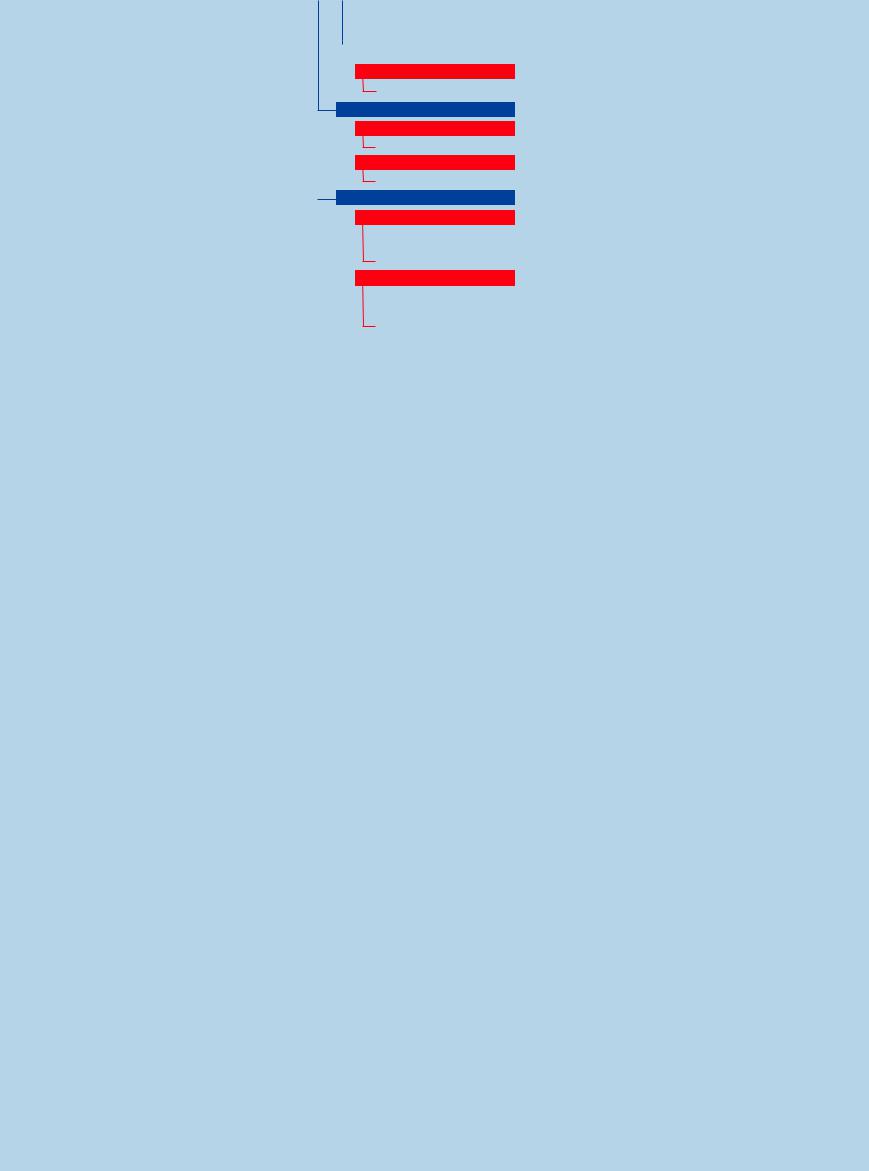
Sonographic tumor staging is of limited accuracy in transabdominal ultrasound, but transurethral scanning is more reliable. The system for staging bladder tumors is shown in
Fig.11.98.
Bladder carcinoma is isoechoic to the rest of the bladder wall. Its outline is usually wavy but occasionally smooth. Sites of wall thickening near diverticula are always suspicious for carcinoma, as they are considered premalignant lesions (see Fig.11.105).
TNM In- |
Tis |
Ta |
T1 |
T2 |
T3a |
T3b |
T4 |
volvement |
|
|
|
|
|
|
|
of urothel- |
|
|
|
|
|
|
|
ium, lamina |
|
|
|
|
|
|
|
propria, |
|
|
|
|
|
|
|
muscle lay- |
|
|
|
|
|
|
|
ers, adventitia |
|
|
|
|
|
|
|
Involve- |
|
|
|
|
|
|
Prostate, |
ment |
|
|
|
|
|
|
uterus, |
outside the |
|
|
|
|
|
|
vagina, |
bladder |
|
|
|
|
|
|
abdomi- |
|
|
|
|
|
|
|
nal wall, |
|
|
|
|
|
|
|
pelvis |
New TNM |
|
0 |
I |
II |
|
III |
IV |
stage |
|
|
|||||
|
|
|
|
|
|
|
|
(1992) |
|
|
|
|
|
|
|
Fig. 11.98 Staging of bladder carcinoma.12
Fig. 11.99 Carcinoma involving the left side of the bladder floor. HB = bladder. R = rectum.
a Hypoechoic, slightly nonhomogeneous mass (T) spread over the bladder floor.
b Shifting the probe slightly shows involvement of the left ureteral orifice (arrow) causing ureteral obstruction
(U).
c Color Doppler: atypical spotty vascularity.
fFig. 11.100 Tumor spread over the bladder floor (arrows), with ureteral obstruction (U). HB = bladder.
Fig. 11.101 Recurrent urothelial carcinoma (arrow) in an 87-year-old woman 2 years after transurethral resection: flat, circumscribed, hypoechoic mass on the bladder floor.
412
Blood Clots 





















































Blood clots or viscous sludge adherent to the bladder wall may be confused with real tumors (see above).
Concavities and Convexities
Urinary Tract
Malformations
Dilated Renal Pelvis and Ureter Renal Pelvic Mass, Ureteral Mass Changes in Bladder Size or Shape Intracavitary Mass
Wall Changes
Diffuse Wall Thickening Circumscribed Wall Thickening Concavities and Convexities
Ureteroceles
Diverticula
Ureteroceles





















































Protrusions from the bladder floor near the |
Fig. 11.102 Ureterocele: elliptical, hyperechoic ureteral |
|
wall herniating into the bladder from the area of the right |
||
ureteral orifices are ureteroceles. Their ultra- |
||
ureteral orifice. The wall layers can be identified. |
||
sound appearance is described above |
|
|
(Fig.11.102). |
|
11
Wall Changes
Diverticula






















































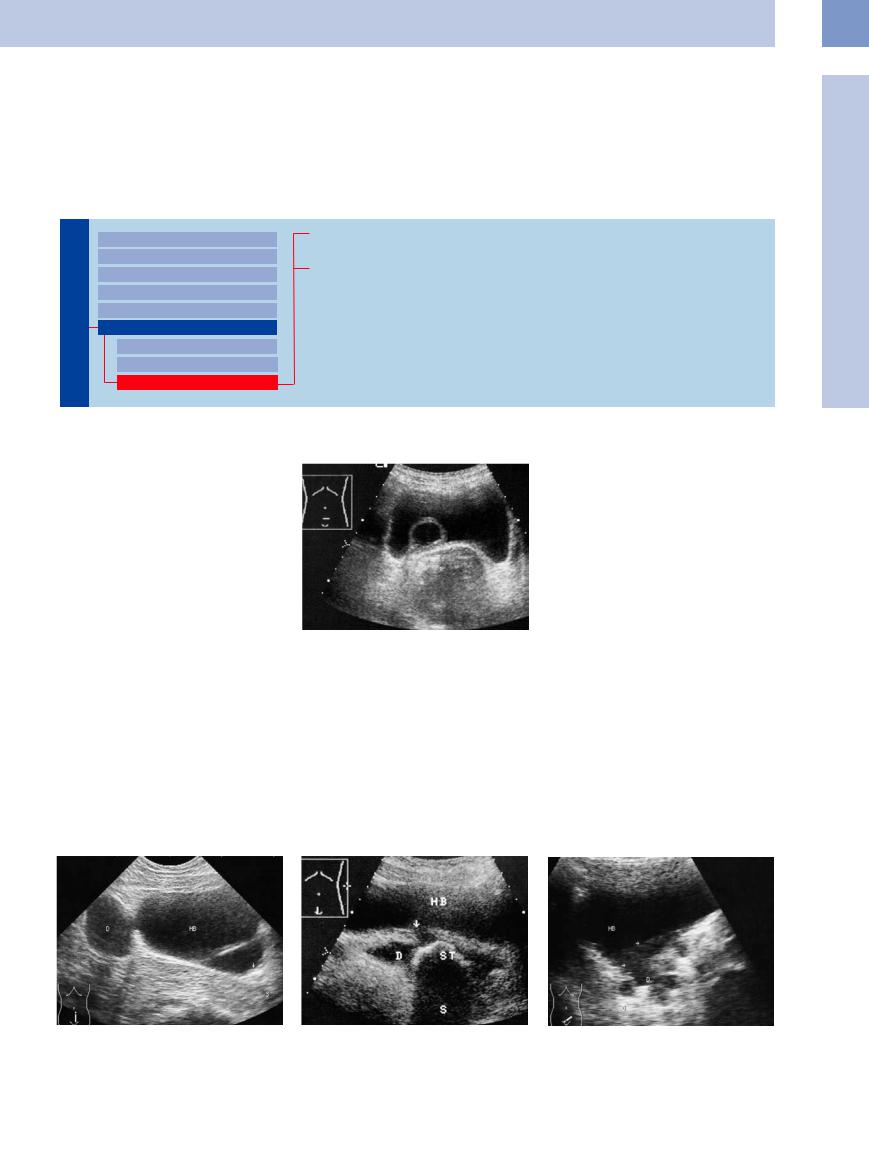
Congenital bladder diverticula are based on a congenital weakness in the bladder wall, allowing a localized full-thickness herniation of the wall. They may be solitary or multiple and range in size from very small to extremely large. Diverticula predispose to stone formation and diverticular carcinoma (Fig.11.105),
which is why they should be surgically removed.
At ultrasound, diverticula typically appear as anechoic round or oval masses located outside the bladder wall. Most diverticula are connected to the bladder lumen by a neck or stalk. The wall of the diverticulum is thinner than the rest of the bladder wall. Diverticula may reach
a size exceeding that of the bladder, often causing them to be mistaken for cysts or the bladder itself. The diagnosis of diverticula is facilitated by examining the bladder in various degrees of distension (Figs. 11.103, 11.104, 11.105).
Pseudodiverticula are secondary reactions to subvesical obstructions, and so they are usually associated with wall hypertrophy,
Fig. 11.103 Large bladder diverticula: one located cranially (D) with a well-defined diverticular neck, and one located in the bladder floor, separated from the main lumen by an echogenic wall and containing a stone (arrow; acoustic shadow S). HB = bladder.
Fig. 11.104 Diverticulum (D) in the bladder floor, with a narrow neck (arrow). The sac contains a large stone (ST) with a wide acoustic shadow (S). HB = bladder.
Fig. 11.105 Extensive diverticular tumor (arrows): hypoechoic mass spread over the bladder floor and occupying the diverticula (D). HB = bladder.
413
11
Urinary Tract
producing a trabeculated bladder (Fig.11.106). |
Fig. 11.106 Bladder-wall hypertrophy with numerous |
They represent protrusions of the bladder mu- |
pseudodiverticula, young man with BPH. |
cosa between bundles of hypertrophied |
|
muscle. |
|
Tips, tricks, and pitfalls
●Bladder polyps and tumors are among the most common accidental findings. Therefore, always pay attention to the bladder and minor pelvis (“sono-optic window”, which is more effective with a fully filled bladder).
●Masses in the bladder present great difficulties in differentiating blood clots from solid tumors. Detectable vessels inside of a mass
may exclude sediments and clots. CEUS improves the differential diagnosis of intraluminal echoic masses, allowing the detection of tumors, which are vascularized and thus enhance, while clots do not enhance (Fig. 11.107).7
References
[1]Hohenfellner R, Walz RH. Primärer und sekundärer Megaureter. In: Hohenfellner R, Thüroff JW, Schulte-Wissermann H. Kinderurologie in Klinik und Praxis. Stuttgart: Thieme, 1986; p. 268
[2]Kröpfl D. Harnleiteranomalien. In: Jocham D, Miller H (eds.). Praxis der Urologie. Stuttgart: Thieme, 1995; p. 377
[3]Tuma J, Schwarzenbach HR. Die Sonographie bei Nierenkolik [Ultrasound for renal colic]. Praxis (Bern 1994) 2004;93:1767–1774
[4]Gladisch R. Praxis der abdominellen Ultraschalldiagnostik. 2nd ed. Stuttgart: Schattauer, 1992
An obstructed–dilated urinary tract is readily differentiable:
●Always examine the region of the occlusion (Fig. 11.107). Small calculi are optimally diagnosable in the ureterovesical junction.
●Ureteral calculi are detectable in a high percentage of cases (up to 98%3) by considering all of the clinical and sonographic diagnostic possibilities (color Doppler, twinkling artifact, compression, and observing the course of the ureter).
●In case of urinary stasis the cause of obstruction should always be diagnosed: in acute stasis it is usually calculi, and in chronic stasis more often a tumor (ovary, prostate, colorectal.
[5]Jequier S, Paltiel H, Lafortune M. Ureterovesical jets in infants and children: duplex and color Doppler US studies. Radiology 1990;175(2):349–353
[6]Riedmiller H, Köhl U. Vesikoureteraler und vesikorenaler Reflux. In: Jocham D, Miller H (eds.). Praxis der Urologie. Stuttgart: Thieme, 1995; pp. 384–388
[7]Piscaglia F Nolsøe C, Dietrich CF, et al. The EFSUMB Guidelines and Recommendations on the Clinical Practice of Contrast Enhanced Ultrasound (CEUS): Update 2011 on non-hep- atic applications. Ultraschall Med 2012; 33(1):33–59
[8]Eble JN, Sauter G, Epstein JI, Sesterhenn IA (eds.). World Health Organization Classifica-
Fig 11.107 Ectated renal pelvis (P) caused by a cyst in the lower pole compressing the upper ureter (arrow).
tion of Tumours. Pathology and Genetics of Tumours of the Urinary System and Male Genital Organs. Lyon: IARC Press, 2004
[9]Gottfried HW. Ultraschall in der Urologie. In: Jocham D, Miller H (eds.). Praxis der Urologie. Stuttgart: Thieme, 1995; pp. 55–75
[10]Jocham D. Maligne Tumoren der Harnblase. In: Jocham D, Miller H (eds.). Praxis der Urologie. Stuttgart: Thieme, 1995; pp. 49–115
[11]Malone PR, Weston-Anderwood J, Aron PM. Transcutaneous ultrasound in the detection of superficial bladder cancer. Br J Urol 1985;58 (6):664–667
[12]Wilmanns W, Huhn D, Wilms K. Internistische Onkologie. Stuttgart: Thieme, 2000; p. 534
414
Prostate, Seminal |
Testis, Epididymis |
12 |
Vesicles, |
The Prostate 417
|
|
|
Enlarged Prostate |
418 |
|||||
|
|
|
|||||||
|
|
|
|
|
|
Regular |
418 |
||
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
Benign Prostatic Hyperplasia |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Prostatic Carcinoma |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Acute Prostatitis |
|
|
|
|
|
|
|
Irregular |
421 |
||
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
Benign Prostatic Hyperplasia |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Prostatic Carcinoma |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Chronic Prostatitis |
|
|
|
|
Small Prostate |
422 |
|||||
|
|
|
|||||||
|
|
|
|
|
Regular |
422 |
|||
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
Operated Prostate |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Radiation Therapy |
|
|
|
|
|
|
|
Echogenic |
423 |
||
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
Chronic Prostatitis |
|
|
|
Circumscribed Lesion |
423 |
||||||
|
|
||||||||
|
|
|
|
|
Anechoic |
423 |
|||
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
Abscess, Cavity |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Utricular Cyst, |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Ectopic Ureter |
|
|
|
|
|
|
|
|
|
After Transurethral Resection |
|
|
|
|
|
|
Hypoechoic |
424 |
|||
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
Benign Prostatic Hyperplasia |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Prostatic Carcinoma |
|
|
|
|
|
|
|
Echogenic |
426 |
||
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
Stones, Calcifications |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
“Surgical Capsule” |
|
Seminal Vesicles |
426 |
|||||||
|
|
|
Diffuse Change |
426 |
||||
|
||||||||
|
|
|||||||
|
|
|
|
|
Hypoechoic |
426 |
||
|
|
|
|
|
||||
|
|
|
|
|
|
|
Vesiculitis |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Tumor Infiltration |
|
|
Circumscribed Change |
427 |
||||||
|
||||||||
|
|
|
|
Anechoic |
427 |
|||
|
|
|
|
|||||
|
|
|
|
|
|
|
Dilatation, Cyst |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Abscess |
|
|
|
|
|
Echogenic |
428 |
|||
|
|
|
|
|||||
|
|
|
|
|
|
|
Stones, Calcifications |
|
|
|
|
|
Irregular |
428 |
|||
|
|
|
|
|
|
|
Chronic Vesiculitis |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Tumor Infiltration |
|
Testis, Epididymis 429
|
Diffuse Change |
430 |
||||||
|
|
Enlargement |
430 |
|||||
|
|
|||||||
|
|
|
|
|
|
|
Orchitis |
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
Testicular Torsion |
|
|
|
|
Decreased Size |
431 |
||||
|
|
|
||||||
|
|
|
|
|
|
|
Anorchism, Cryptorchidism |
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
Hypogonadism |
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
Atrophy |
|
Circumscribed Lesion |
431 |
|||||||
|
|
Anechoic or Hypoechoic |
431 |
|||||
|
|
|||||||
|
|
|
|
|
|
|
Testicular Cyst |
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
Hematoma |
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
Abscess |
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
Testicular Infarction |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Testicular Tumor |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Irregular/Echogenic |
433 |
|||
|
|
|
|
|||||
|
|
|
|
|
|
|
Testicular Microlithiasis |
|
Epididymal Lesion |
434 |
|||||||
|
|
|
|
Anechoic |
434 |
|||
|
|
|
|
|||||
|
|
|
|
|
|
|
Spermatocele, Epididymal Cyst |
|
|
|
|
|
|
Hypoechoic |
434 |
||
|
|
|
|
|
||||
|
|
|
|
|
|
|
Epididymitis |
|
|
|
Intrascrotal Mass |
435 |
|||||
|
||||||||
|
|
|
|
Anechoic or Hypoechoic |
435 |
|||
|
|
|
|
|
|
|
Hydrocele |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Varicocele |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Hematocele |
|
|
|
|
|
|
Echogenic |
436 |
||
|
|
|
|
|
||||
|
|
|
|
|
|
|
Fibroma of the Tunica/ |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Corpus Librum |
|
Scrotal Hernia
