
- •Contents
- •Preface
- •Contributors
- •1 Vessels
- •1.1 Aorta, Vena Cava, and Peripheral Vessels
- •Aorta, Arteries
- •Anomalies and Variant Positions
- •Dilatation
- •Stenosis
- •Wall Thickening
- •Intraluminal Mass
- •Perivascular Mass
- •Vena Cava, Veins
- •Anomalies
- •Dilatation
- •Intraluminal Mass
- •Compression, Infiltration
- •1.2 Portal Vein and Its Tributaries
- •Enlarged Lumen Diameter
- •Portal Hypertension
- •Intraluminal Mass
- •Thrombosis
- •Tumor
- •2 Liver
- •Enlarged Liver
- •Small Liver
- •Homogeneous Hypoechoic Texture
- •Homogeneous Hyperechoic Texture
- •Regionally Inhomogeneous Texture
- •Diffuse Inhomogeneous Texture
- •Anechoic Masses
- •Hypoechoic Masses
- •Isoechoic Masses
- •Hyperechoic Masses
- •Echogenic Masses
- •Irregular Masses
- •Differential Diagnosis of Focal Lesions
- •Diagnostic Methods
- •Suspected Diagnosis
- •3 Biliary Tree and Gallbladder
- •3.1 Biliary Tree
- •Thickening of the Bile Duct Wall
- •Localized and Diffuse
- •Bile Duct Rarefaction
- •Localized and Diffuse
- •Bile Duct Dilatation and Intraductal Pressure
- •Intrahepatic
- •Hilar and Prepancreatic
- •Intrapancreatic
- •Papillary
- •Abnormal Intraluminal Bile Duct Findings
- •Foreign Body
- •The Seven Most Important Questions
- •3.2 Gallbladder
- •Changes in Size
- •Large Gallbladder
- •Small/Missing Gallbladder
- •Wall Changes
- •General Hypoechogenicity
- •General Hyperechogenicity
- •General Tumor
- •Focal Tumor
- •Intraluminal Changes
- •Hyperechoic
- •Hypoechoic
- •Nonvisualized Gallbladder
- •Missing Gallbladder
- •Obscured Gallbladder
- •4 Pancreas
- •Diffuse Pancreatic Change
- •Large Pancreas
- •Small Pancreas
- •Hypoechoic Texture
- •Hyperechoic Texture
- •Focal Changes
- •Anechoic Lesion
- •Hypoechoic Lesion
- •Isoechoic Lesion
- •Hyperechoic Lesion
- •Irregular (Complex Structured) Lesion
- •Dilatation of the Pancreatic Duct
- •Marginal/Mild Dilatation
- •Marked Dilatation
- •5 Spleen
- •Nonfocal Changes of the Spleen
- •Diffuse Parenchymal Changes
- •Large Spleen
- •Small Spleen
- •Focal Changes of the Spleen
- •Anechoic Mass
- •Hypoechoic Mass
- •Hyperechoic Mass
- •Splenic Calcification
- •6 Lymph Nodes
- •Peripheral Lymph Nodes
- •Head/Neck
- •Extremities (Axilla, Groin)
- •Abdominal Lymph Nodes
- •Porta Hepatis
- •Splenic Hilum
- •Mesentery (Celiac, Upper and Lower Mesenteric Station)
- •Stomach
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •Small/Large Intestine
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •8 Peritoneal Cavity
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Wall Structures
- •Smooth Margin
- •Irregular Margin
- •Intragastric Processes
- •Intraintestinal Processes
- •9 Kidneys
- •Anomalies, Malformations
- •Aplasia, Hypoplasia
- •Cystic Malformation
- •Anomalies of Number, Position, or Rotation
- •Fusion Anomaly
- •Anomalies of the Renal Calices
- •Vascular Anomaly
- •Diffuse Changes
- •Large Kidneys
- •Small Kidneys
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Irregular Structure
- •Circumscribed Changes
- •Anechoic Structure
- •Hypoechoic or Isoechoic Structure
- •Complex Structure
- •Hyperechoic Structure
- •10 Adrenal Glands
- •Enlargement
- •Anechoic Structure
- •Hypoechoic Structure
- •Complex Echo Structure
- •Hyperechoic Structure
- •11 Urinary Tract
- •Malformations
- •Duplication Anomalies
- •Dilatations and Stenoses
- •Dilated Renal Pelvis and Ureter
- •Anechoic
- •Hypoechoic
- •Hypoechoic
- •Hyperechoic
- •Large Bladder
- •Small Bladder
- •Altered Bladder Shape
- •Intracavitary Mass
- •Hypoechoic
- •Hyperechoic
- •Echogenic
- •Wall Changes
- •Diffuse Wall Thickening
- •Circumscribed Wall Thickening
- •Concavities and Convexities
- •12.1 The Prostate
- •Enlarged Prostate
- •Regular
- •Irregular
- •Small Prostate
- •Regular
- •Echogenic
- •Circumscribed Lesion
- •Anechoic
- •Hypoechoic
- •Echogenic
- •12.2 Seminal Vesicles
- •Diffuse Change
- •Hypoechoic
- •Circumscribed Change
- •Anechoic
- •Echogenic
- •Irregular
- •12.3 Testis, Epididymis
- •Diffuse Change
- •Enlargement
- •Decreased Size
- •Circumscribed Lesion
- •Anechoic or Hypoechoic
- •Irregular/Echogenic
- •Epididymal Lesion
- •Anechoic
- •Hypoechoic
- •Intrascrotal Mass
- •Anechoic or Hypoechoic
- •Echogenic
- •13 Female Genital Tract
- •Masses
- •Abnormalities of Size or Shape
- •Uterus
- •Abnormalities of Size or Shape
- •Myometrial Changes
- •Intracavitary Changes
- •Endometrial Changes
- •Fallopian Tubes
- •Hypoechoic Mass
- •Anechoic Cystic Mass
- •Solid Echogenic or Nonhomogeneous Mass
- •14 Thyroid Gland
- •Diffuse Changes
- •Enlarged Thyroid Gland
- •Small Thyroid Gland
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Circumscribed Changes
- •Anechoic
- •Hypoechoic
- •Isoechoic
- •Hyperechoic
- •Irregular
- •Differential Diagnosis of Hyperthyroidism
- •Types of Autonomy
- •15 Pleura and Chest Wall
- •Chest Wall
- •Masses
- •Parietal Pleura
- •Nodular Masses
- •Diffuse Pleural Thickening
- •Pleural Effusion
- •Anechoic Effusion
- •Echogenic Effusion
- •Complex Effusion
- •16 Lung
- •Masses
- •Anechoic Masses
- •Hypoechoic Masses
- •Complex Masses
- •Index
Staging in Abdominal Lymph Node Involvement
Solid gastrointestinal tumors. Ultrasound cannot differentiate reliably between lymph nodes with metastatic invasion and those with benign lymphadenopathy. Frequently the lymph nodes are located within the drainage region of the tumor. Lymph node involvement has great prognostic significance in tumor staging (TNM system). When removing the tumor and the regional lymph nodes, the number of metastatic lymph nodes and their distance from the primary tumor are of additional prognostic importance (Fig. 6.9). In most cases, exact staging is possible only after pathological work-up since the mesenteric and parietal lymph nodes are superimposed on each other and thus defy precise demonstration. Endosonography is the imaging modality of choice when staging gastrointestinal tumors (except in the large and small intestines). In solid tumors the primary pattern of lymph node invasion is diffuse and micronodular as well as focal lymphadenopathy (micro and macro). “Bulky” formations are infrequent findings.
Malignant lymphoma. In the staging of malignant lymphoma, possible involvement of the abdominal lymph nodes carries with it far-reaching therapeutic consequences. If ultrasound cannot resolve the issue, additional CT studies are warranted. In patients with Hodgkin disease, staging laparotomy becomes necessary in only a few cases and is done only if the outcome has consequences for the treatment regimen. The sonographic image of abdominal lymph node involvement in malignant lymphoma covers a broad spectrum. Focal lymphadenopathy is most prevalent, with the lymphomas being well defined or confluent. Extremely “bulky” formations with concomitant displacement phenomena are not especially rare. If there is concurrent lymphoma, involvement of parenchymal organs of the gastrointestinal tract with an invasion pattern characteristic of lymphoma ultrasound will often be the first finding to raise the suspected diagnosis of malignant lymphoma.
In localized, primarily gastrointestinal lymphomas, any additional splanchnic (regional) lymph node involvement implies stage IIE1, while parietal (nonregional) in-
volvement would indicate stage IIE2 (according to the Musshoff staging system). Sometimes this situation is difficult to differentiate from primary lymph node involvement with organ involvement by direct extension.
Low-grade and high-grade non-Hodgkin lymphoma (NHL). The most common manifestation of low-grade NHL is systemic lymphadenopathy (the clinical symptoms frequently being rather mild), but highgrade NHL often manifests itself by enlarged lymph nodes in localized anatomical regions, and also by “bulky” formation. The diagnosis has to be confirmed by histology (also needed for subtyping of the lymphoma). Ultrasound-guided fine-needle aspiration biopsy will be able to distinguish benign lymphadenopathy from cancer metastasis or malignant lymphoma; however, typing of malignant lymphoma usually requires substantially more material, which often can only be obtained by laparotomy (unless there are peripheral lymph nodes easily accessible for excision).
Fig. 6.9 Schematic illustration of the splanchnic and parietal lymph nodes. TR = celiac axis; VC = vena cava; N = kidney; M = stomach; AO = aorta; AMS = superior mesenteric artery; AMI = inferior mesenteric artery.
6
Peripheral Lymph Nodes
■ Peripheral Lymph Nodes
Head/Neck
Lymph Nodes

Peripheral Lymph Nodes
Head/Neck
Extremities (Axilla, Groin)
Abdominal Lymph Nodes
Inflammatory Lymph Nodes
Metastases
Malignant Lymphoma
Other Structures
241
6
Lymph Nodes
Inflammatory Lymph Nodes 












































About 300 of the about 1000 lymph nodes in the human body are located in the cervical region. During childhood and adolescence, more than 80% of all enlarged lymph nodes are reactive in nature, depending on age. Posterocervical nuchal lymph nodes tend to be benign, whereas the lymph nodes of the supraclavicular fossa are often malignant.
Acute inflammatory lymphadenopathy ( 6.3c,d) has to be differentiated from chronic inflammatory (regressive) lymph node enlargement (Fig. 6.4). Usually, acutely inflamed lymph nodes are small (<1.5 cm), the hilar sign is present, and the length:width ratio (L/W) is greater than 2; they are not caked together and mostly display a homogeneous parenchyma (note: liquefying suppurating lymph node). Acute lymphadenitis is characterized by homogeneous hyperperfusion (
6.3c,d) has to be differentiated from chronic inflammatory (regressive) lymph node enlargement (Fig. 6.4). Usually, acutely inflamed lymph nodes are small (<1.5 cm), the hilar sign is present, and the length:width ratio (L/W) is greater than 2; they are not caked together and mostly display a homogeneous parenchyma (note: liquefying suppurating lymph node). Acute lymphadenitis is characterized by homogeneous hyperperfusion ( 6.3e,f), but lowlevel perfusion, or even lack of it, does not rule out reactive lymph node enlargement (Fig. 6.10). It has been suggested that horizon-
6.3e,f), but lowlevel perfusion, or even lack of it, does not rule out reactive lymph node enlargement (Fig. 6.10). It has been suggested that horizon-
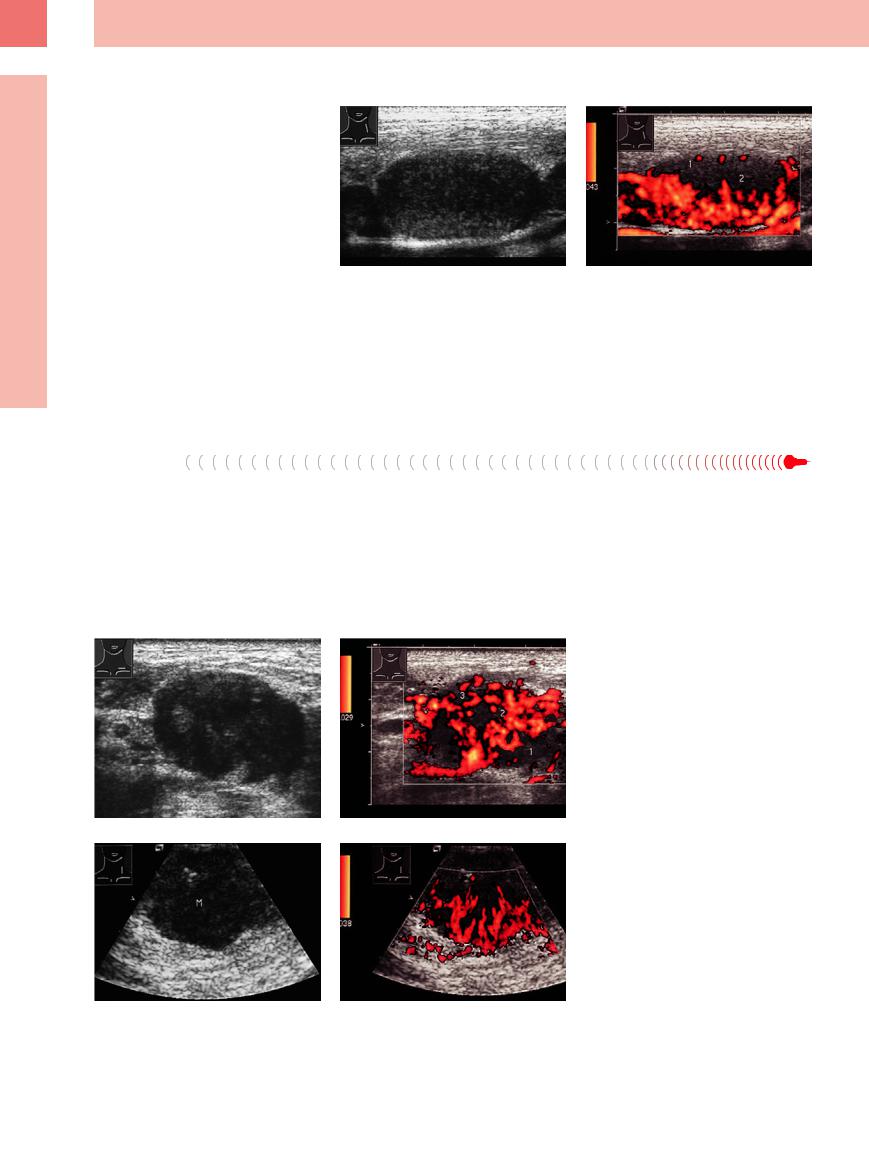
Fig. 6.10 A 13-year-old girl with fever and cervical lymphadenopathy.
a Enlarged homogeneous hypoechoic lymph node.
tal hilar vessels, longitudinal branches, and homogeneous vascular branching seen on colorflow Doppler scanning of the vascular supply of the lymph nodes are indicative of reactive lymphadenopathy ( 6.3i,j).
6.3i,j).
b Subcapsular vessels (1) and a focal lack of blood vessels
(2) on color-flow Doppler imaging. The initial findings raised a high suspicion of malignancy, while the followup indicated reactive lymphadenopathy.
In regressive lymph nodes, parenchymal calcification is possible ( 6.2j–l). On color-flow Doppler imaging, chronic inflammatory lymph nodes are characterized by a lack of flow.
6.2j–l). On color-flow Doppler imaging, chronic inflammatory lymph nodes are characterized by a lack of flow.
Metastases
In metastasis, size is not a typical parameter and usually the hilar sign is missing ( 6.3 g,h). This type of lymph node tends to be round and hyperechoic (
6.3 g,h). This type of lymph node tends to be round and hyperechoic ( 6.1a,b). Sometimes invasive growth can be demonstrated, necrosis is possible, and calcification of the parenchyma has also been observed (
6.1a,b). Sometimes invasive growth can be demonstrated, necrosis is possible, and calcification of the parenchyma has also been observed ( 6.2n,o). The concentration of blood vessels varies on color-flow Doppler scanning. The vascular supply of the lymph
6.2n,o). The concentration of blood vessels varies on color-flow Doppler scanning. The vascular supply of the lymph
nodes has been said to indicate malignancy if color-flow Doppler imaging visualizes vascular displacement, aberrant vessels, and regions lacking any vascularization, and capsular vessels ( 6.3 m,n). Metastases exhibiting rapid growth have been shown to display a pathological vascularization with corkscrew-like vessels (Fig. 6.11). It is important to determine before surgery whether the metastatic cervical
6.3 m,n). Metastases exhibiting rapid growth have been shown to display a pathological vascularization with corkscrew-like vessels (Fig. 6.11). It is important to determine before surgery whether the metastatic cervical
lymph nodes can be delineated from the large blood vessels of the neck or whether there is vascular invasion. Contact between tumor and vessel wall over a distance of more than 3.5 cm, or over more than half the circumference, suggests vascular invasion (Fig. 6.12).
Fig. 6.11 A 72-year-old patient with malignant lymphoma and cervical lymph node metastasis.
a Hypoechoic lymph node.
b Corkscrew-like neovascularization. 1 = focal lack of vessels; 2 = aberrant vessels; 3 = subcapsular vessels.
c Hypoechoic lymph node. M = metastasis.
d Marked neovascularization in metastases with rapid clinical growth.
242
Malignant Lymphoma

























In many cases the lymph nodes will be visual- |
like fashion. Color-flow Doppler scanning will |
ized as being large, hypoechoic, and in multi- |
show them to be characterized by a homoge- |
ples. The normal length:width ratio is less than |
neous increase in the vascular images ( |
2. Their texture is mostly homogeneous and |
6.5a,b). Not only will they decrease in size |
they are clustered like grapes or in festoon- |
during treatment but the flow phenomena ob- |
 6.5 Lymph Nodes in Hodgkin Disease
6.5 Lymph Nodes in Hodgkin Disease
Color Doppler (power mode)
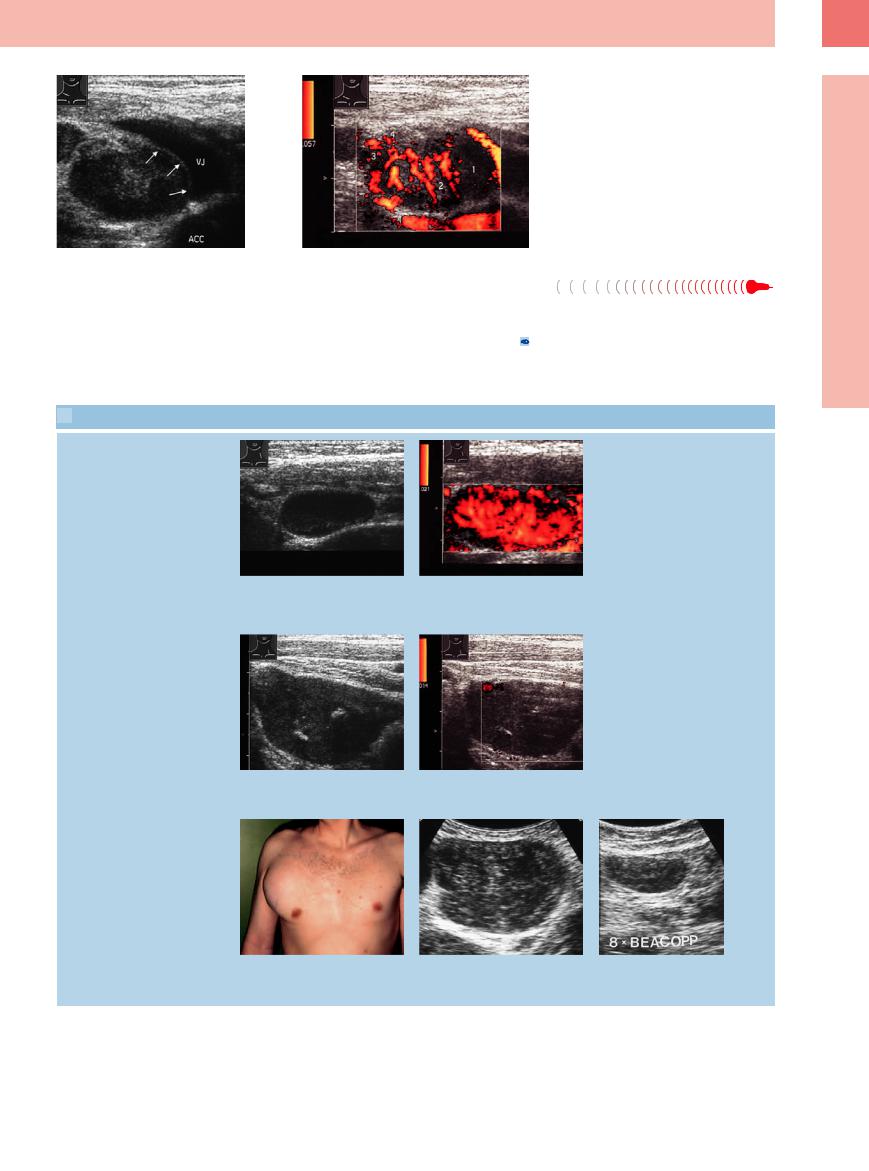
Fig. 6.12 Lymph node invaded by an ENT tumor.
a The lymph node covers the vessel wall over more than one-quarter of the circumference (vessel contact over 90 °). ACC = common carotid artery; VJ = jugular vein.
b Color-flow Doppler imaging demonstrates a lack of blood vessels (1), aberrant vessels (2), “paint spots” (3), and subcapsular vessels (4).
served on color-flow Doppler scanning will also diminish ( 6.5c,d,
6.5c,d,  6.5e–i). Sometimes the end stage will be an echogenic lymph node, varying in size, with hyperechoic capsule and no discernible flow signals.
6.5e–i). Sometimes the end stage will be an echogenic lymph node, varying in size, with hyperechoic capsule and no discernible flow signals.
6
Peripheral Lymph Nodes
a and b A 32-year-old patient with Hodgkin disease 4 years previously, presenting with an acutely enlarged lymph node.
a Homogeneous hypoechoic lymph node.
c and d A 33-year-old patient with Hodgkin disease.
c Persistently enlarged lymph node.
b Hypervascularization on color-flow Doppler scanning. Follow-up indicated reactive lymphadenopathy.
d Lack of any flow signals on color-flow Doppler scanning. Follow-up indicated reactive lymphadenopathy.
Follow-up studies post treatment
e–g Lymph node in Hodgkin disease.
e A 25-year-old patient with a large tumor in the right axilla.
f and g Large hypoechoic lymphoma that resolved under treatment.
243
6
Lymph Nodes
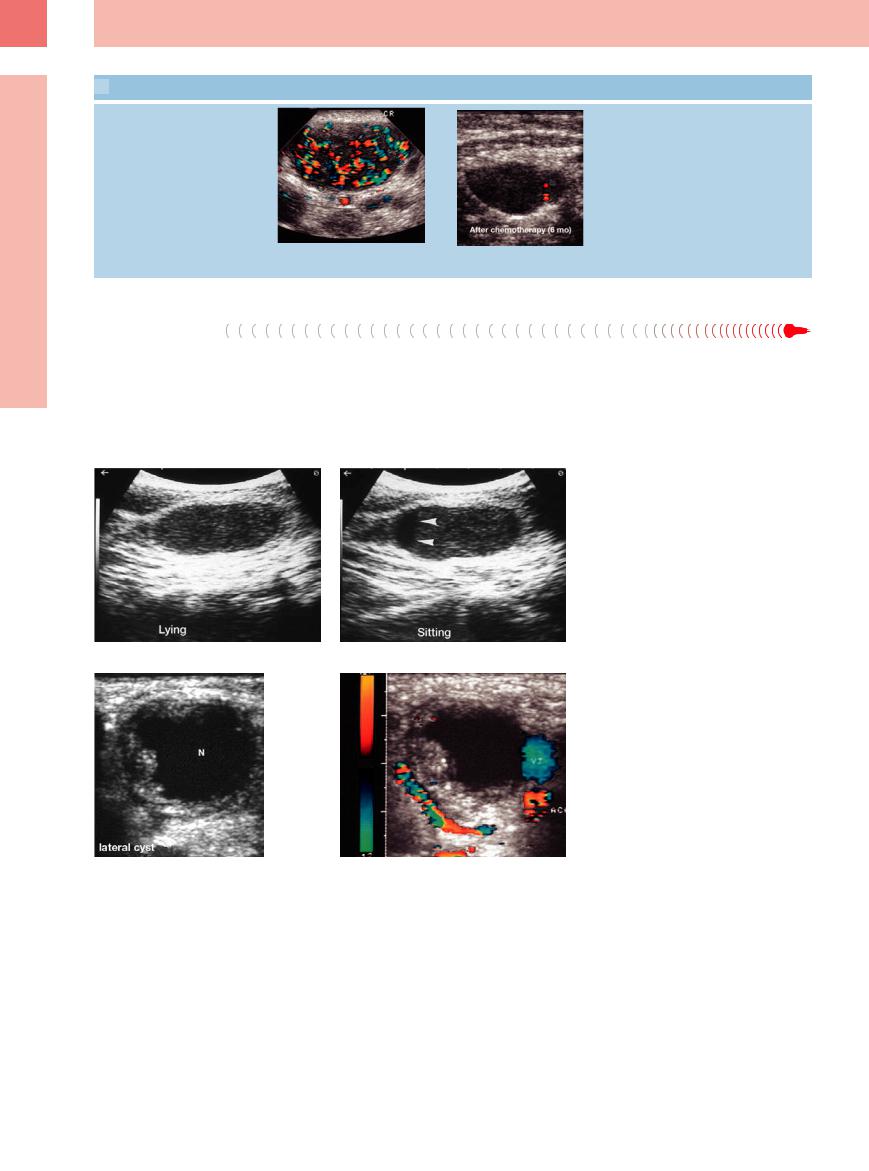
 6.5 Lymph Nodes in Hodgkin Disease (Continued)
6.5 Lymph Nodes in Hodgkin Disease (Continued)
h and i Intensified vascularization on color-flow Doppler scanning before therapy; after chemotherapy no more flow signals are detected (further resolution during follow-up).
Other Structures
●Head/neck. Tumor of the parotid gland, lymphangiomatosis, abscess, hemorrhage, carotid artery aneurysm, branchial cyst (Fig. 6.13, Fig. 6.14), parathyroid adenoma.
●Supraclavicular. Pancoast tumor, bone tumor, abscess.
Fig. 6.13a and b Formation in the right lateral neck with sedimentation phenomena, compatible with a branchial cyst.
Fig. 6.14a and b Formation in the right lateral neck with liquefied center (N). The diagnosis of a branchial cyst was made only after surgery. ACC = common carotid artery; VJ = jugular vein.
244
