
- •Contents
- •Preface
- •Contributors
- •1 Vessels
- •1.1 Aorta, Vena Cava, and Peripheral Vessels
- •Aorta, Arteries
- •Anomalies and Variant Positions
- •Dilatation
- •Stenosis
- •Wall Thickening
- •Intraluminal Mass
- •Perivascular Mass
- •Vena Cava, Veins
- •Anomalies
- •Dilatation
- •Intraluminal Mass
- •Compression, Infiltration
- •1.2 Portal Vein and Its Tributaries
- •Enlarged Lumen Diameter
- •Portal Hypertension
- •Intraluminal Mass
- •Thrombosis
- •Tumor
- •2 Liver
- •Enlarged Liver
- •Small Liver
- •Homogeneous Hypoechoic Texture
- •Homogeneous Hyperechoic Texture
- •Regionally Inhomogeneous Texture
- •Diffuse Inhomogeneous Texture
- •Anechoic Masses
- •Hypoechoic Masses
- •Isoechoic Masses
- •Hyperechoic Masses
- •Echogenic Masses
- •Irregular Masses
- •Differential Diagnosis of Focal Lesions
- •Diagnostic Methods
- •Suspected Diagnosis
- •3 Biliary Tree and Gallbladder
- •3.1 Biliary Tree
- •Thickening of the Bile Duct Wall
- •Localized and Diffuse
- •Bile Duct Rarefaction
- •Localized and Diffuse
- •Bile Duct Dilatation and Intraductal Pressure
- •Intrahepatic
- •Hilar and Prepancreatic
- •Intrapancreatic
- •Papillary
- •Abnormal Intraluminal Bile Duct Findings
- •Foreign Body
- •The Seven Most Important Questions
- •3.2 Gallbladder
- •Changes in Size
- •Large Gallbladder
- •Small/Missing Gallbladder
- •Wall Changes
- •General Hypoechogenicity
- •General Hyperechogenicity
- •General Tumor
- •Focal Tumor
- •Intraluminal Changes
- •Hyperechoic
- •Hypoechoic
- •Nonvisualized Gallbladder
- •Missing Gallbladder
- •Obscured Gallbladder
- •4 Pancreas
- •Diffuse Pancreatic Change
- •Large Pancreas
- •Small Pancreas
- •Hypoechoic Texture
- •Hyperechoic Texture
- •Focal Changes
- •Anechoic Lesion
- •Hypoechoic Lesion
- •Isoechoic Lesion
- •Hyperechoic Lesion
- •Irregular (Complex Structured) Lesion
- •Dilatation of the Pancreatic Duct
- •Marginal/Mild Dilatation
- •Marked Dilatation
- •5 Spleen
- •Nonfocal Changes of the Spleen
- •Diffuse Parenchymal Changes
- •Large Spleen
- •Small Spleen
- •Focal Changes of the Spleen
- •Anechoic Mass
- •Hypoechoic Mass
- •Hyperechoic Mass
- •Splenic Calcification
- •6 Lymph Nodes
- •Peripheral Lymph Nodes
- •Head/Neck
- •Extremities (Axilla, Groin)
- •Abdominal Lymph Nodes
- •Porta Hepatis
- •Splenic Hilum
- •Mesentery (Celiac, Upper and Lower Mesenteric Station)
- •Stomach
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •Small/Large Intestine
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •8 Peritoneal Cavity
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Wall Structures
- •Smooth Margin
- •Irregular Margin
- •Intragastric Processes
- •Intraintestinal Processes
- •9 Kidneys
- •Anomalies, Malformations
- •Aplasia, Hypoplasia
- •Cystic Malformation
- •Anomalies of Number, Position, or Rotation
- •Fusion Anomaly
- •Anomalies of the Renal Calices
- •Vascular Anomaly
- •Diffuse Changes
- •Large Kidneys
- •Small Kidneys
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Irregular Structure
- •Circumscribed Changes
- •Anechoic Structure
- •Hypoechoic or Isoechoic Structure
- •Complex Structure
- •Hyperechoic Structure
- •10 Adrenal Glands
- •Enlargement
- •Anechoic Structure
- •Hypoechoic Structure
- •Complex Echo Structure
- •Hyperechoic Structure
- •11 Urinary Tract
- •Malformations
- •Duplication Anomalies
- •Dilatations and Stenoses
- •Dilated Renal Pelvis and Ureter
- •Anechoic
- •Hypoechoic
- •Hypoechoic
- •Hyperechoic
- •Large Bladder
- •Small Bladder
- •Altered Bladder Shape
- •Intracavitary Mass
- •Hypoechoic
- •Hyperechoic
- •Echogenic
- •Wall Changes
- •Diffuse Wall Thickening
- •Circumscribed Wall Thickening
- •Concavities and Convexities
- •12.1 The Prostate
- •Enlarged Prostate
- •Regular
- •Irregular
- •Small Prostate
- •Regular
- •Echogenic
- •Circumscribed Lesion
- •Anechoic
- •Hypoechoic
- •Echogenic
- •12.2 Seminal Vesicles
- •Diffuse Change
- •Hypoechoic
- •Circumscribed Change
- •Anechoic
- •Echogenic
- •Irregular
- •12.3 Testis, Epididymis
- •Diffuse Change
- •Enlargement
- •Decreased Size
- •Circumscribed Lesion
- •Anechoic or Hypoechoic
- •Irregular/Echogenic
- •Epididymal Lesion
- •Anechoic
- •Hypoechoic
- •Intrascrotal Mass
- •Anechoic or Hypoechoic
- •Echogenic
- •13 Female Genital Tract
- •Masses
- •Abnormalities of Size or Shape
- •Uterus
- •Abnormalities of Size or Shape
- •Myometrial Changes
- •Intracavitary Changes
- •Endometrial Changes
- •Fallopian Tubes
- •Hypoechoic Mass
- •Anechoic Cystic Mass
- •Solid Echogenic or Nonhomogeneous Mass
- •14 Thyroid Gland
- •Diffuse Changes
- •Enlarged Thyroid Gland
- •Small Thyroid Gland
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Circumscribed Changes
- •Anechoic
- •Hypoechoic
- •Isoechoic
- •Hyperechoic
- •Irregular
- •Differential Diagnosis of Hyperthyroidism
- •Types of Autonomy
- •15 Pleura and Chest Wall
- •Chest Wall
- •Masses
- •Parietal Pleura
- •Nodular Masses
- •Diffuse Pleural Thickening
- •Pleural Effusion
- •Anechoic Effusion
- •Echogenic Effusion
- •Complex Effusion
- •16 Lung
- •Masses
- •Anechoic Masses
- •Hypoechoic Masses
- •Complex Masses
- •Index
9
Kidneys
Topography 





















































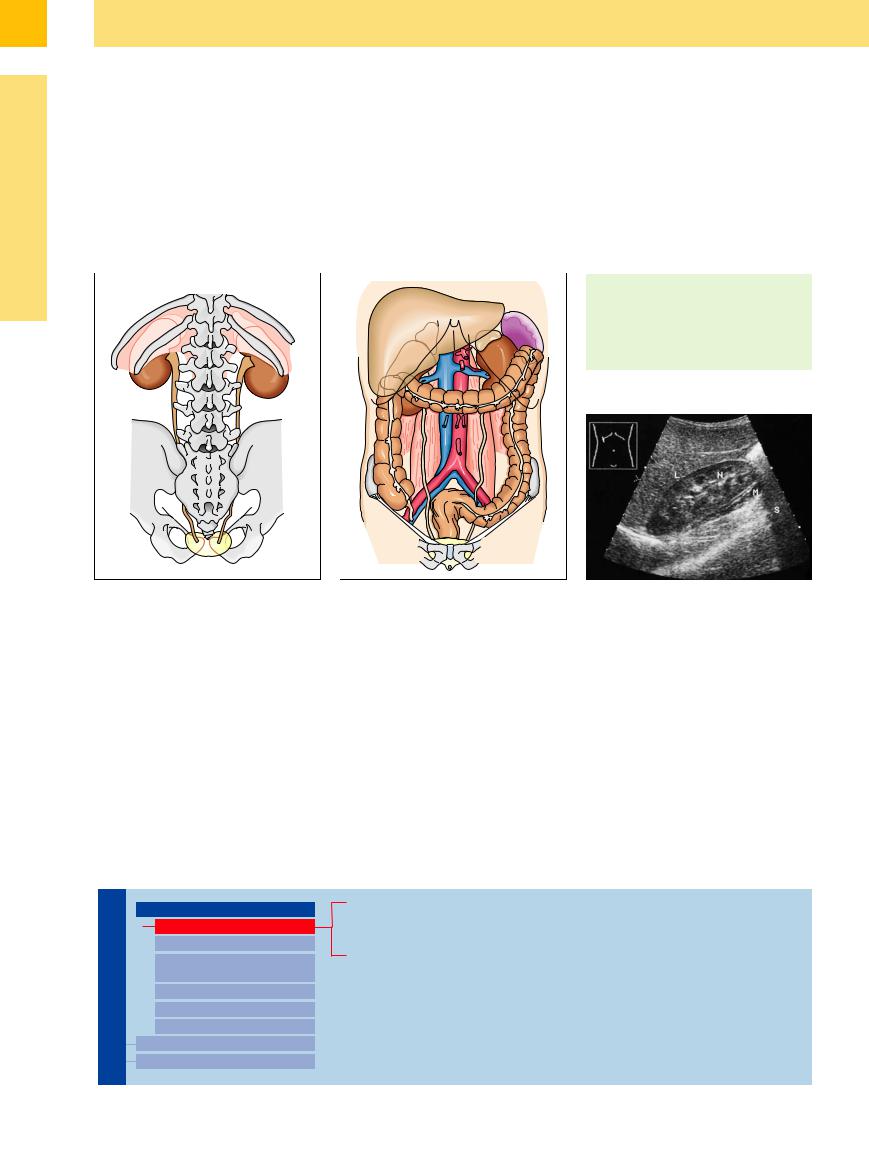
The spleen and pancreatic tail are in contact with the upper pole of the left kidney. Both kidneys are located in the retroperitoneal space, one on either side of the spinal column, and are anterior to the lumbar muscles (psoas major, quadratus lumborum, and transversus abdominis). They project past the 12th rib into the last intercostal space, so that part of the kidneys extends into the chest between the diaphragm and chest wall. The central portion
of each kidney is anterior to the diaphragm at the level of the lateral part of the 12th rib, and the lower portion extends down past the 12th rib (Fig. 9.4a).
At the medial concave border of the kidney is the hilum with the renal vessels. The vein is anterior, the artery is behind it, and the upper ureter is posterior. In the right kidney, this region borders on the descending part of the duodenum. The anterior surface of the kidney
forms the renal impression in the right lobe of the liver. The right and left colic flexures overlie the lower renal poles (Fig. 9.4b, Fig. 9.5). The upper portion of the left kidney borders on the spleen, while the tail of the pancreas and the posterosuperior gastric surface overlie it. Cystic areas arising from the spleen, kidney, or tail of the pancreas may be found in the renal–splenic angle; they are difficult to localize to a specific organ in ultrasonography (see  9.2h).
9.2h).
Fig. 9.4 Relations of the kidney to neighboring structures. a Ribs and spinal column (from a dorsal point of view).
b Organs in the upper and lower abdomen. |
Relations
●The kidneys are retroperitoneal, lying anterior to the lumbar muscles.
●Colic flexures overlie the lower renal poles; liver and stomach overlie the upper poles.
Fig. 9.5 Topography of the right kidney (N). The organ is retroperitoneal, lying anterior to the musculature (M). Its anterior surface is related to the liver (L), which bears the renal impression. The lower pole of the kidney extends anteriorly downward and is partially obscured by highlevel echoes from the right colic flexure, which casts an acoustic shadow (S).
■ Anomalies, Malformations
Anomalies and malformations are based on a |
teric bud (agenesis) to the fully formed kidney |
dromedary hump in the lateral border of the |
congenital disturbance of fetal renal develop- |
(postrenal urinary tract anomaly). |
left kidney (see Fig. 9.66b). |
ment. Their severity depends on the timing of |
Not every presumed malformation is ac- |
|
their occurrence, i. e., the period ranging from |
tually classified as such. A number of “malfor- |
|
the metanephrogenic blastema and the ure- |
mations” are actually normal variants, such as a |
|
Aplasia, Hypoplasia
Kidneys

Anomalies, Malformations
Aplasia, Hypoplasia
Cystic Malformation
Anomalies of Number, Position, or Rotation
Fusion Anomaly
Anomalies of the Renal Calices Vascular Anomaly
Diffuse Changes Circumscribed Changes
Renal Agenesis
Hypoplasia
Dysplasia
322
9
looking caudally to the “normal location” along the line of ascent (pelvic, lumbar, abdominal dysplasia). Renal agenesis in one-third of patients is associated with cystic seminal vesicles or unilateral seminal vesicle agenesis.
Anomalies, Malformations
Fig. 9.6 Aplasia of the right kidney with compensatory |
b Left kidney with two parapelvic cysts. P = renal pelvis. |
enlargement of the left kidney (N). |
|
a The right renal fossa is empty. L = liver, S = shadowing |
|
from gas in the colon. |
|
Hypoplasia































A hypoplastic kidney appears sonographically as an abnormal development of the renal tissue, which is usually of less than normal size, but with a normal structure. In dysplasia there are additional disturbances of normal renal architecture, with the kidney presenting as small or very small: some hypoplastic kidneys are too small to be defined with ultrasound. Differentiation from an atrophic kidney is not always possible, but most hypoplastic kidneys exhibit normal parenchyma and normal central hilar echoes. Calcifications or multicystic changes may be found (Fig. 9.7).
Dysplasia
Because of the common association of dysplastic kidneys with a urinary tract obstruction and other extrarenal syndromes, they are found more often in children than in adults. In ultrasound imaging the kidney is small and shows a dysplastic parenchyma with single or multiple small or large cysts and a dissolved corticomedullar differentiation without a regular architecture.
Fig. 9.7 Renal hypoplasia. The apparent “missing left kidney” is probably a tiny hypoplastic kidney (cursors).
323
9
Kidneys
Cystic Malformation
Kidneys |
Anomalies, Malformations |
|||
|
|
|
||
|
|
|
|
Aplasia, Hypoplasia |
|
|
|
|
Cystic Malformation |
|
|
|
|
|
|
|
|
|
Anomalies of Number, |
|
|
|
|
Position, or Rotation |
|
|
|
|
Fusion Anomaly |
|
|
|
|
Anomalies of the Renal Calices |
|
|
|
|
Vascular Anomaly |
|
|
|
Diffuse Changes |
|
|
|
|
||
|
|
|
Circumscribed Changes |
|
|
|
|
||
The most common benign masses of the kidney are cysts. About 50% of the population have renal cysts, which appear more often and are larger in advanced age.
Between 45 and 59 years of age renal cysts are more common in men than in women. A specific pathologic explanation for this has not yet been established; however, ischemic changes, interstitial medullary fibrosis, and tubular obstruction at the basal membrane of
Autosomal Dominant Polycystic Kidney Disease (ADPKD)
the distal tubulus are all under discussion. The following list shows a differential synopsis of the diverse renal diseases accompanied by cysts:
●Unilateral cystic dysplastic kidney
●Dysplasia with cysts
●Idiopathic renal cyst
●Genetic polycystic kidney disease:
–Autosomal recessive polycystic kidney disease (ARPKD) in neonates (Potter syndrome type I)
–Autosomal dominant polycystic kidney disease (ADPKD), manifestation in adults (Potter syndrome type III)
●Secondary cysts
●Cysts associated with tumors
●Cysts in obstructive uropathy
Autosomal Dominant
Dominant Polycystic Kidney
Polycystic Kidney Disease (ADPKD)
Disease (ADPKD) 




























Polycystic kidney diseases, associated with cystic liver and with cystic lesions of other organs and cerebral aneurysms, fall into the category of ontogenic renal lesions. Renal and often liver and splenic cysts can also be commonly found in parents of affected children, especially in the father. They are caused by increased intratubular pressure due to distal tubular obstructions and by tubular epithelial dysplasia. The cystic lesions thus represent tubular retention cysts. Because the cysts are small in infancy and only later become increasingly larger, it is difficult to make a diagnosis in children. Renal cysts in children aged 6 years and older should indicate an examination of the parents (as the mother can often have multiple renal cysts). If the cysts are bilateral and multiple, ADPKD may be present. In the infantile form (autosomal recessive polycystic kidney disease, ARPKD), one can find cystically transformed pyramids.
Cysts located in the area of the renal sinus are generally lymphatic cysts. Secondary cysts (involutional cysts) may be found in chronic renal diseases (see below), especially in terminal kidney insufficiency, which is frequently associated with renal cancer. The various types of renal cysts are reviewed in Table 9.1.
Table 9.1 Types of renal cysts |
|
|
|
Type of cystic kidney |
Age at symptom |
Morphology |
Complications, |
(Potter) |
onset, location |
|
associated disorders |
Infantile polycystic |
Newborn, infants, |
Kidneys greatly en- |
Renal failure, hepatic |
nephropathy (type I) |
bilateral |
larged, with collecting |
fibrosis |
|
|
ducts 1–2 mm in size |
|
Dysplastic cystic |
Infants, small children, |
Polycystic kidneys, |
Obstructive ureteral |
kidney (type II) |
unilateral or bilateral |
cortical cysts |
or bladder anomalies, |
|
|
|
recurrent urinary |
|
|
|
tract infections |
Adult polycystic |
20–40 years of age, |
Kidneys greatly en- |
Frequent hepatic |
nephropathy (type III) |
bilateral |
larged, with cysts in all |
cysts, pyelonephritis, |
|
|
nephrons |
hypertension, uremia |
Familial nephronoph- |
Adolescents, adults, |
Small kidneys, |
Mental deficiency, |
thisis |
bilateral |
sclerosing interstitial |
hepatic fibrosis, |
|
|
nephropathy with |
ataxia, uremia |
|
|
distal tubular cysts |
|
Medullary sponge |
Adults, 80% bilateral |
Collecting-duct cysts |
Recurrent urinary |
kidney |
|
in the papillae with |
tract infections, |
|
|
calculi |
urolithiasis |
Simple renal cysts |
Any age, unilateral or |
Solitary or multiple |
Rarely, pyelonephritis |
|
bilateral |
cysts up to 5 cm in size |
|
324
9
Anomalies, Malformations
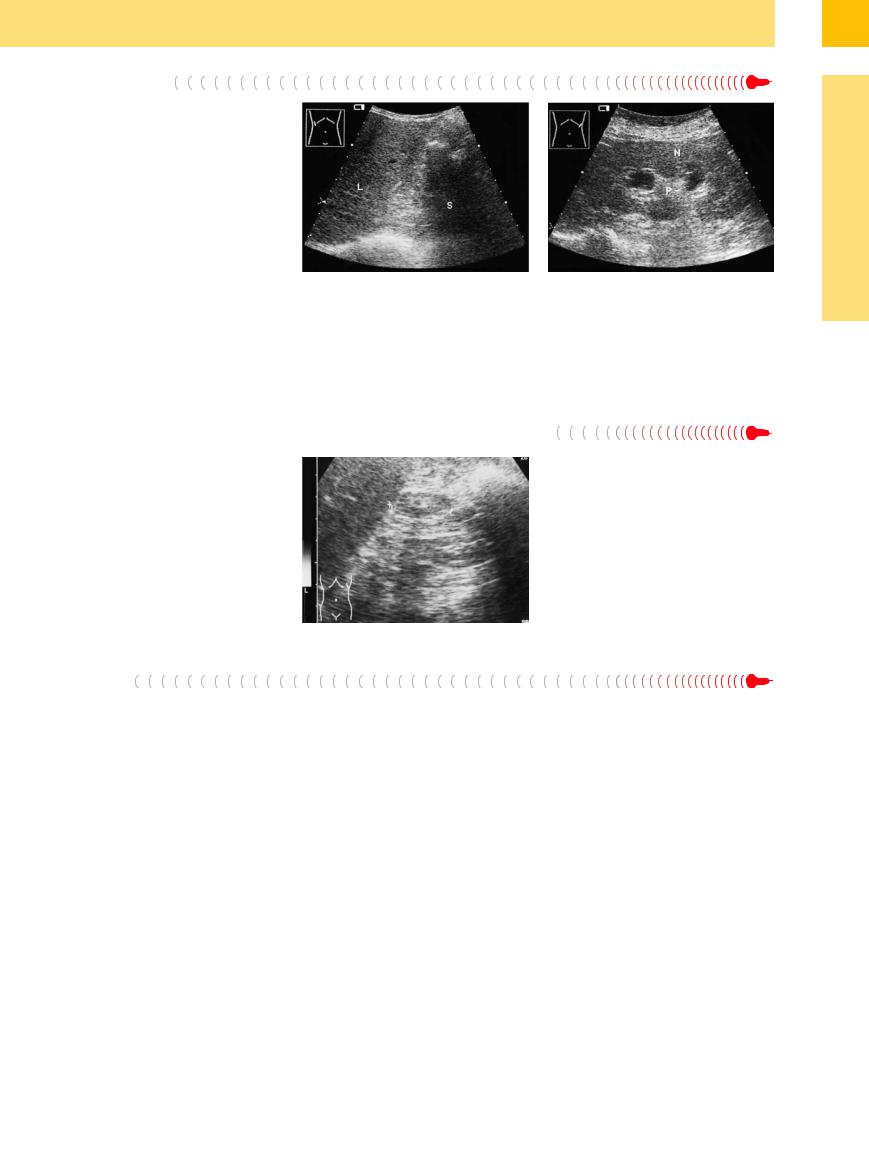
Fig. 9.8 Polycystic renal degeneration (Potter type III adult polycystic disease). Cystic renal degeneration (N). The parenchyma is difficult to identify because of the many anechoic spaces.
a Macrocystic-bullous form, 72-year-old man: macrocystic conglomerate with still detectable residual parenchyma (N).
b Predominantly microcystic form in a 21-year-old man: multiple fine cysts (Z) with relatively well preserved parenchyma.
Fig. 9.9 Multiple renal cysts (Z). The kidney is still of normal size, and the parenchyma is clearly visible; dialysis.
Sonographic features. Renal cysts appear sonographically as round, anechoic, smooth-bor- dered masses that are lined with epithelium, forming a cyst wall. For physical reasons, they cause posterior acoustic enhancement. Simple solitary or multiple cysts and adult-type polycystic kidneys (Potter type III) are of particular interest for routine scanning in internal medicine.
Polycystic kidneys contain multiple anechoic masses of varying size, usually causing considerable organ enlargement. The cysts produce an undulating renal outline with no discernible capsule, causing poor delineation of the kidney. Large bullous cysts obscure the residually intact parenchyma through a “blooming effect,” so that the kidney appears to consist almost entirely of cystic areas. Microcystic kidneys still display numerous areas of
Anomalies of Number, Position, or Rotation
renal parenchyma. This pattern requires differentiation from multiple renal cysts. In this case the parenchyma is still clearly visible and generally the kidneys are not enlarged (Fig. 9.8, Fig. 9.9; see also “Circumscribed Changes”, p. 344).
Kidneys

Anomalies, Malformations
Aplasia, Hypoplasia
Cystic Malformation
Anomalies of Number, Position, or Rotation
Fusion Anomaly
Anomalies of the Renal Calices Vascular Anomaly
Diffuse Changes Circumscribed Changes
Duplex Kidney
Ectopic Kidney
Malrotation
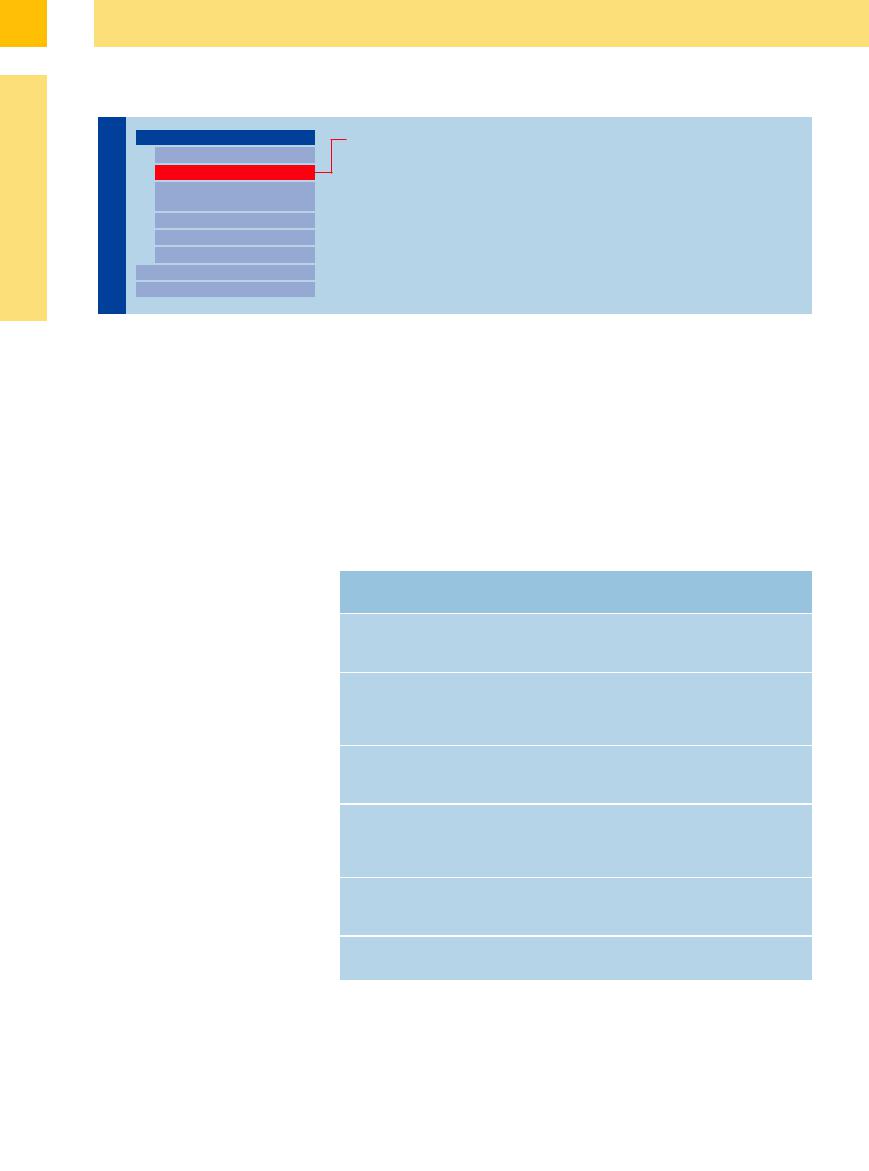
Duplex Kidney




















































Duplex kidney is the most common renal anomaly, occurring in 1% of the general population. It is characterized by duplicated renal pelvises and two ureters that unite somewhere between the kidney and bladder. The duplex kidney is also enlarged. When the ureters have different insertions, the ureter with the more distal insertion belongs to the upper moiety, according to the Meyer–Weigert rule. The ureter belonging to the lower moiety consistently empties proximate to that site. In a duplex kidney with hydronephrosis, then, the upper
ureter (e. g., megaureter, see Chapter 11) and associated pelvis will be obstructed owing to the ectopic insertion (caution: upper-pole cyst). But if the lower ureter is affected, the obstruction is due not to an ectopic insertion but to some other obstructive process.
It is common to find an ectopic insertion of the lower moiety with an associated ureterocele, leading to vesicorenal reflux or ureteral obstruction that again affects the upper moiety. (In the case of a ureterocele, it cannot be de-
termined with ultrasound whether the ureter runs within or outside the detrusor muscle.)
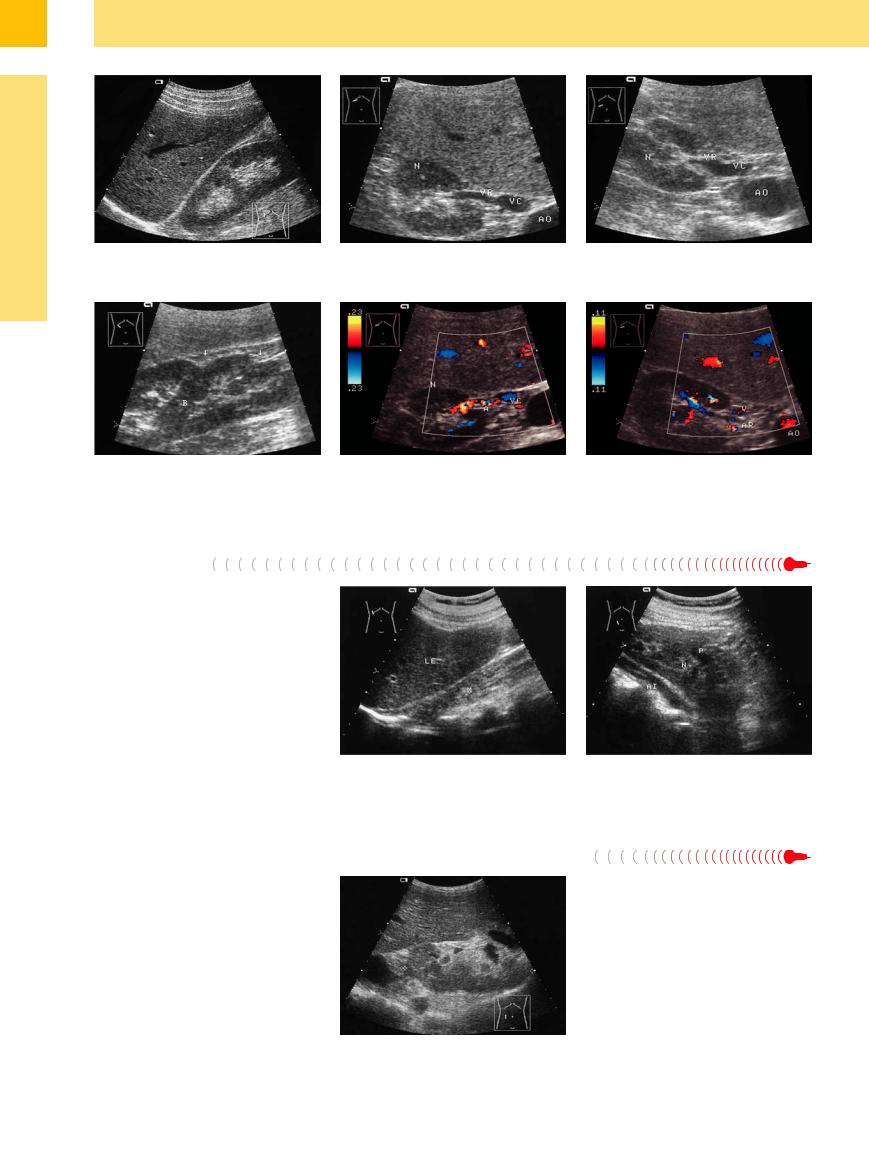
The ultrasound features of a duplex kidney are (Figs. 9.10, 9.11, 9.12, 9.13):
●Longitudinal enlargement with a normal organ thickness
●A parenchymal bridge separating the upper and lower collecting systems
●Usually, a notch at the level of the parenchymal bridge
●Duplication of the renal hilum
325
9
Kidneys
Fig. 9.10 Duplex kidney: 12 cm long kidney with two pelvises separated by a band of parenchyma.
Fig. 9.12 Duplex kidney. The two moieties are separated by a parenchymal band (B), where a notch is visible in the renal outline (arrows; the lower arrow marks the hilum of the lower renal segment).
Fig. 9.11 Duplicated renal hilum. VC = vena cava; AO = aorta; N = kidney; VR = renal vein.
a Upper renal vein.
Fig. 9.13 CDS image showing two renal pelvises. N = kidney; VC = vena cava.
a Upper renal artery (A).
b Lower renal vein, demonstrated by a lower transverse scan.
b Lower renal artery (AR).
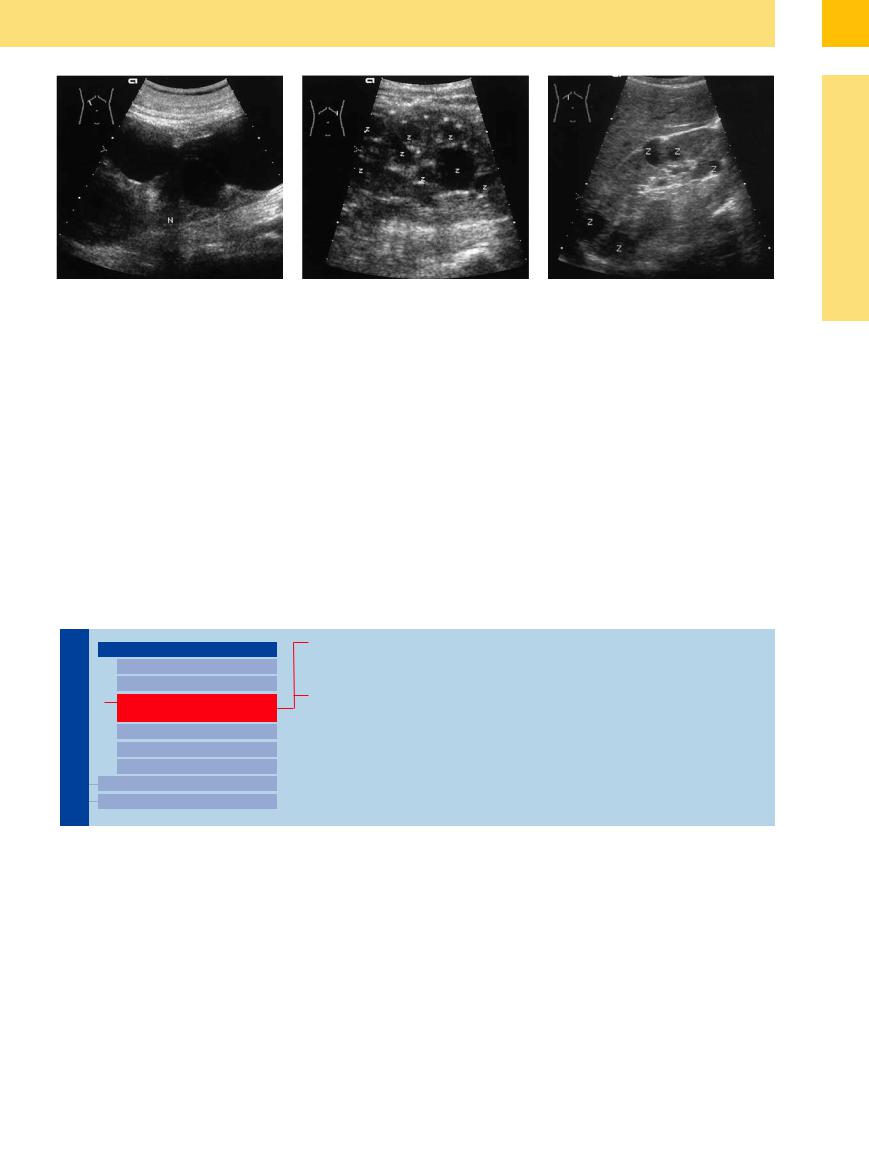
Ectopic Kidney
A lumbar kidney is the most common form of renal ectopia, with ultrasound revealing the ectopic kidney in the anterior iliac fossa. The key sonographic landmark is the iliac artery— the ectopic kidney will generally be found anterior to that vessel. The less common pelvic kidney lies anterior to the sacrum and below the aortic bifurcation. Abdominal ectopia is the easiest form to detect, as the affected kidney is markedly lower than its counterpart; but in contrast to the lumbar and pelvic forms, usually the kidney is not small or malrotated (Fig. 9.14).
Fig. 9.14 Ectopic right kidney in the lesser pelvis (renal pelvic dysplasia).
a The right kidney is not found at its usual site posterior to the liver (LE) (no renal impression). M = lumbar muscle.
b The dysplastic right kidney (N) is located in the lesser pelvis on the right side along the iliac artery (AI). P = renal pelvis.
Malrotation 






























Malrotation is an anomaly in which the renal hilum faces anteriorly (caution: this makes the vessels vulnerable to a percutaneous needle). Otherwise difficult to detect, a malrotated kidney can be positively identified by the location of its hilum (Fig. 9.15).
Fig. 9.15 Malrotated kidney in a slightly ectopic location (cursors). The renal hilum faces anteriorly.
326
