
- •Contents
- •Preface
- •Contributors
- •1 Vessels
- •1.1 Aorta, Vena Cava, and Peripheral Vessels
- •Aorta, Arteries
- •Anomalies and Variant Positions
- •Dilatation
- •Stenosis
- •Wall Thickening
- •Intraluminal Mass
- •Perivascular Mass
- •Vena Cava, Veins
- •Anomalies
- •Dilatation
- •Intraluminal Mass
- •Compression, Infiltration
- •1.2 Portal Vein and Its Tributaries
- •Enlarged Lumen Diameter
- •Portal Hypertension
- •Intraluminal Mass
- •Thrombosis
- •Tumor
- •2 Liver
- •Enlarged Liver
- •Small Liver
- •Homogeneous Hypoechoic Texture
- •Homogeneous Hyperechoic Texture
- •Regionally Inhomogeneous Texture
- •Diffuse Inhomogeneous Texture
- •Anechoic Masses
- •Hypoechoic Masses
- •Isoechoic Masses
- •Hyperechoic Masses
- •Echogenic Masses
- •Irregular Masses
- •Differential Diagnosis of Focal Lesions
- •Diagnostic Methods
- •Suspected Diagnosis
- •3 Biliary Tree and Gallbladder
- •3.1 Biliary Tree
- •Thickening of the Bile Duct Wall
- •Localized and Diffuse
- •Bile Duct Rarefaction
- •Localized and Diffuse
- •Bile Duct Dilatation and Intraductal Pressure
- •Intrahepatic
- •Hilar and Prepancreatic
- •Intrapancreatic
- •Papillary
- •Abnormal Intraluminal Bile Duct Findings
- •Foreign Body
- •The Seven Most Important Questions
- •3.2 Gallbladder
- •Changes in Size
- •Large Gallbladder
- •Small/Missing Gallbladder
- •Wall Changes
- •General Hypoechogenicity
- •General Hyperechogenicity
- •General Tumor
- •Focal Tumor
- •Intraluminal Changes
- •Hyperechoic
- •Hypoechoic
- •Nonvisualized Gallbladder
- •Missing Gallbladder
- •Obscured Gallbladder
- •4 Pancreas
- •Diffuse Pancreatic Change
- •Large Pancreas
- •Small Pancreas
- •Hypoechoic Texture
- •Hyperechoic Texture
- •Focal Changes
- •Anechoic Lesion
- •Hypoechoic Lesion
- •Isoechoic Lesion
- •Hyperechoic Lesion
- •Irregular (Complex Structured) Lesion
- •Dilatation of the Pancreatic Duct
- •Marginal/Mild Dilatation
- •Marked Dilatation
- •5 Spleen
- •Nonfocal Changes of the Spleen
- •Diffuse Parenchymal Changes
- •Large Spleen
- •Small Spleen
- •Focal Changes of the Spleen
- •Anechoic Mass
- •Hypoechoic Mass
- •Hyperechoic Mass
- •Splenic Calcification
- •6 Lymph Nodes
- •Peripheral Lymph Nodes
- •Head/Neck
- •Extremities (Axilla, Groin)
- •Abdominal Lymph Nodes
- •Porta Hepatis
- •Splenic Hilum
- •Mesentery (Celiac, Upper and Lower Mesenteric Station)
- •Stomach
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •Small/Large Intestine
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •8 Peritoneal Cavity
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Wall Structures
- •Smooth Margin
- •Irregular Margin
- •Intragastric Processes
- •Intraintestinal Processes
- •9 Kidneys
- •Anomalies, Malformations
- •Aplasia, Hypoplasia
- •Cystic Malformation
- •Anomalies of Number, Position, or Rotation
- •Fusion Anomaly
- •Anomalies of the Renal Calices
- •Vascular Anomaly
- •Diffuse Changes
- •Large Kidneys
- •Small Kidneys
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Irregular Structure
- •Circumscribed Changes
- •Anechoic Structure
- •Hypoechoic or Isoechoic Structure
- •Complex Structure
- •Hyperechoic Structure
- •10 Adrenal Glands
- •Enlargement
- •Anechoic Structure
- •Hypoechoic Structure
- •Complex Echo Structure
- •Hyperechoic Structure
- •11 Urinary Tract
- •Malformations
- •Duplication Anomalies
- •Dilatations and Stenoses
- •Dilated Renal Pelvis and Ureter
- •Anechoic
- •Hypoechoic
- •Hypoechoic
- •Hyperechoic
- •Large Bladder
- •Small Bladder
- •Altered Bladder Shape
- •Intracavitary Mass
- •Hypoechoic
- •Hyperechoic
- •Echogenic
- •Wall Changes
- •Diffuse Wall Thickening
- •Circumscribed Wall Thickening
- •Concavities and Convexities
- •12.1 The Prostate
- •Enlarged Prostate
- •Regular
- •Irregular
- •Small Prostate
- •Regular
- •Echogenic
- •Circumscribed Lesion
- •Anechoic
- •Hypoechoic
- •Echogenic
- •12.2 Seminal Vesicles
- •Diffuse Change
- •Hypoechoic
- •Circumscribed Change
- •Anechoic
- •Echogenic
- •Irregular
- •12.3 Testis, Epididymis
- •Diffuse Change
- •Enlargement
- •Decreased Size
- •Circumscribed Lesion
- •Anechoic or Hypoechoic
- •Irregular/Echogenic
- •Epididymal Lesion
- •Anechoic
- •Hypoechoic
- •Intrascrotal Mass
- •Anechoic or Hypoechoic
- •Echogenic
- •13 Female Genital Tract
- •Masses
- •Abnormalities of Size or Shape
- •Uterus
- •Abnormalities of Size or Shape
- •Myometrial Changes
- •Intracavitary Changes
- •Endometrial Changes
- •Fallopian Tubes
- •Hypoechoic Mass
- •Anechoic Cystic Mass
- •Solid Echogenic or Nonhomogeneous Mass
- •14 Thyroid Gland
- •Diffuse Changes
- •Enlarged Thyroid Gland
- •Small Thyroid Gland
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Circumscribed Changes
- •Anechoic
- •Hypoechoic
- •Isoechoic
- •Hyperechoic
- •Irregular
- •Differential Diagnosis of Hyperthyroidism
- •Types of Autonomy
- •15 Pleura and Chest Wall
- •Chest Wall
- •Masses
- •Parietal Pleura
- •Nodular Masses
- •Diffuse Pleural Thickening
- •Pleural Effusion
- •Anechoic Effusion
- •Echogenic Effusion
- •Complex Effusion
- •16 Lung
- •Masses
- •Anechoic Masses
- •Hypoechoic Masses
- •Complex Masses
- •Index
7
Gastrointestinal Tract
■ Stomach
Although the stomach is not part of a routine transabdominal ultrasound study, except for some special cases, it quite often produces typical findings that have to be interpreted correctly. This calls not only for a systematic analysis of the above criteria but also for the use of a
5 MHz probe, which will improve the diagnostic interpretation (differentiation of the wall layers).
Assessment of any sonographic findings at the stomach has to consider quite precisely the time of the patient’s last ingestion. Interpreta-
tion may be facilitated and improved by oral fluid intake (with an antifoaming agent added). Specific sonomorphologic analysis of the gastric wall requires endoscopic/bioptic and endosonographic procedures.
Focal Wall Changes
|
|
|
|
Stomach |
|
|
Gastric Polyps |
|
Tract |
|
|||||||
|
|
Focal Wall Changes |
|
|
Stromal Tumor |
|||
|
|
|
||||||
Gastrointestinal |
|
|
Extended Wall Changes |
|
|
Carcinoma |
||
|
|
Dilated Lumen |
|
|
||||
|
|
|
|
Lymphoma |
||||
|
|
|
|
|
|
|
||
|
|
|
|
|
Narrowed Lumen |
|
|
|
|
|
|
|
|
|
|
Gastric Varices |
|
|
|
|
|
Small/Large Intestine |
|
|
||
|
|
|
|
|
|
GAVE |
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Ulceration |
|
|
|
|
|
|
|
|
Diverticula, Mucosal Folds |
|
|
|
|
|
|
|
|
Hypertrophic Pyloric Stenosis |
Gastric Polyps 











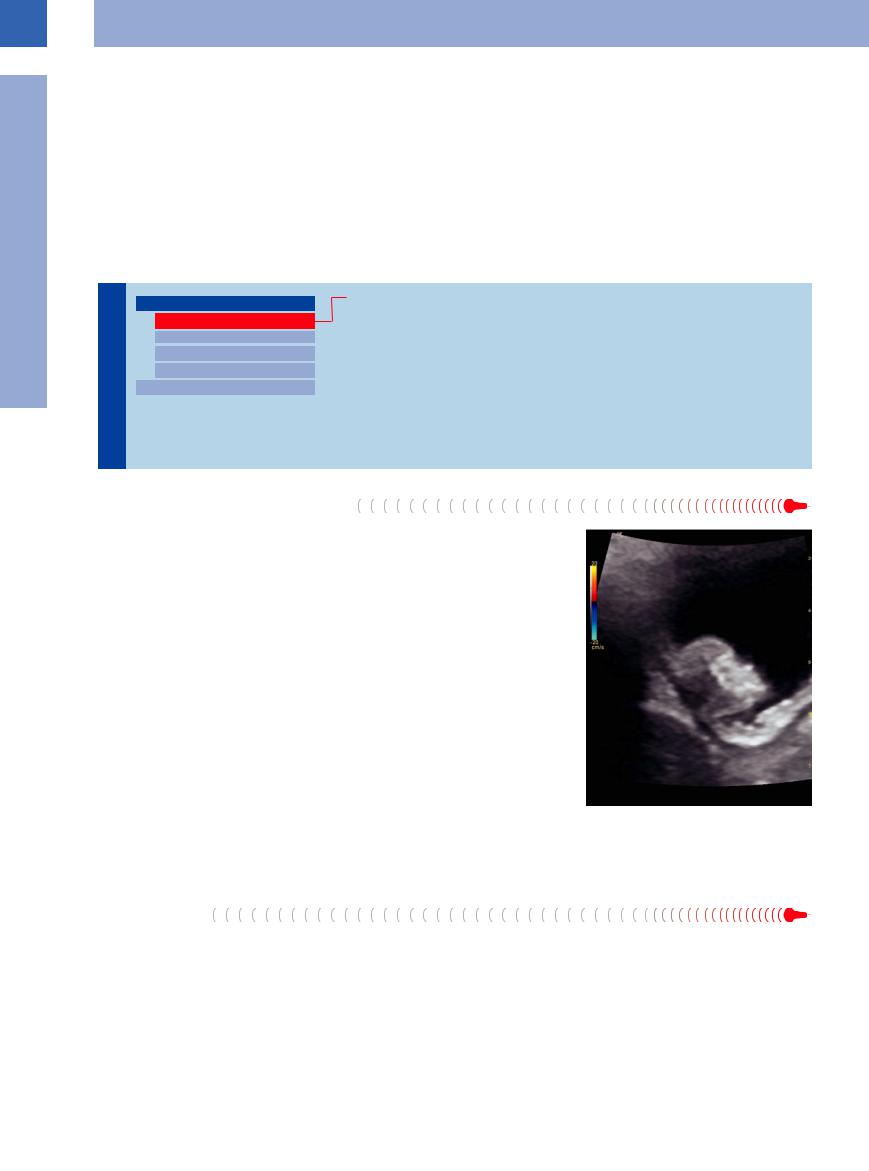
Polypoid changes of the gastric wall are purely incidental findings and are best visualized with the stomach containing only very little fluid (Fig. 7.2). The polyp will appear as a sessile focal mass protruding into the gastric lumen and presenting as an atypical (off-center) pathological gut signature. Polyps arise from certain layers of the gastric wall, most often the mucosa and submucosa, but may also involve the deeper layers of the wall. A more precise analysis of the wall layers would require the use of high-frequency probes or
even endoscopic/endosonographic procedures. In larger polyps, color flow Doppler imaging may be able to demonstrate the intravascular blood flow. Polyps do not affect the outer delineation of the gastric gut signature. Being subjected to the peristaltic movement of the stomach wall, the sessile polyp will move passively and thus can be better differentiated from the mucosal folds. Since ultrasound cannot distinguish between benign and malignant polyps, it is impossible to differentiate a benign polyp from gastric adenocarcinoma type I.
Fig. 7.2 Polypoid gastric tumor. In US, demonstration of a circumscribed thickening of the muscularis propria and over that the edematous submucosa and mucosa (here, GIST).
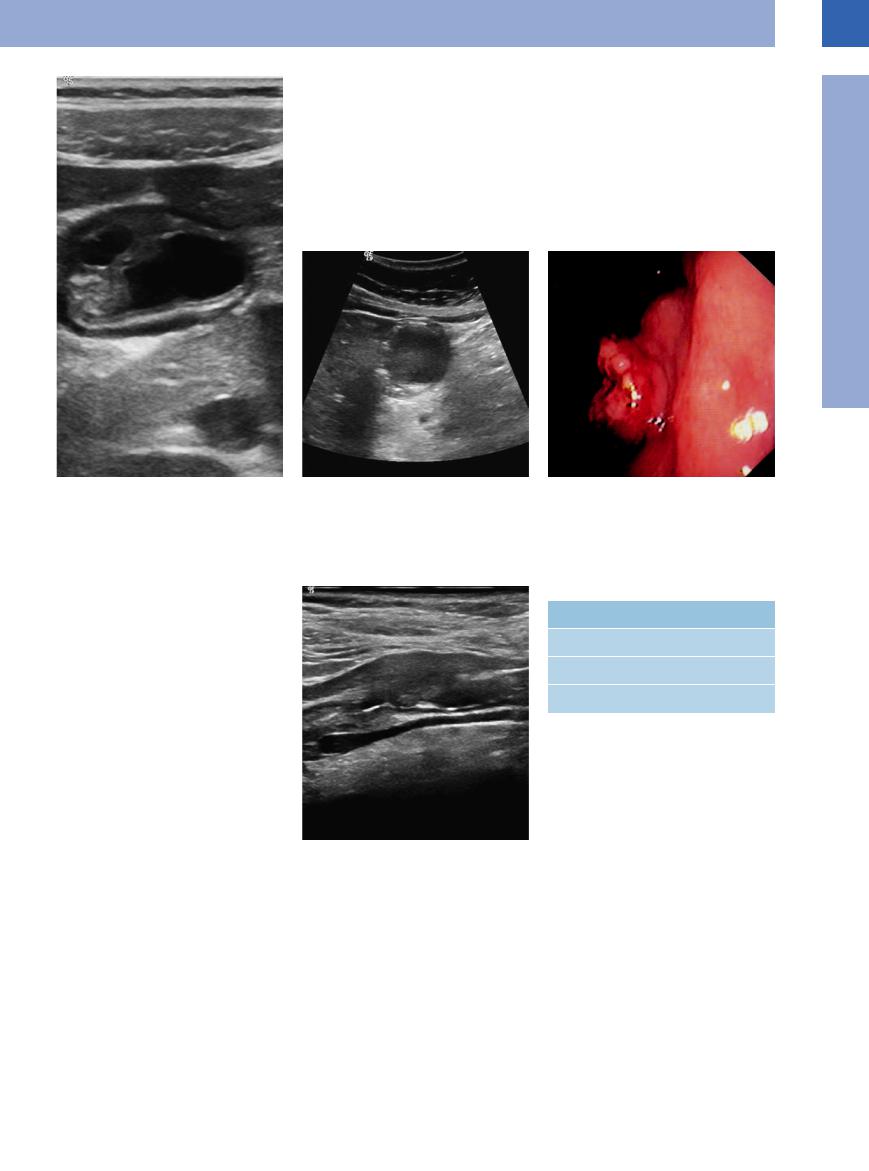
Stromal Tumor
Gastrointestinal stromal tumors (GIST) are rare tumors of mesenchymal origin. They are normally related to a layer of the gastointestinal wall, but can also occur beyond the gastrointestinal wall and without a connection to it (eGIST). The most common location is the gas-
tric wall (ca. 60% occurrence). These tumors have smooth margins, are found in the layered wall of the stomach, quite often relate to one of the central layers, and are well vascularized. They exhibit interstitial growth and may reach a size of several centimeters (0.5–40 cm). Pos-
sible malignancy increases with size. Although these firm, elastic tumors display a somewhat varied echogenicity, they are mostly hypoechoic. In large tumors central necrosis can be detected (Figs. 7.3, 7.4, 7.5).
266
7
Stomach
Fig. 7.3 Gastrointestinal stromal tumor (GIST). Hypoechoic tumor (leiomyoma) in the wall of the stomach.
Fig. 7.4 Gastrointestinal stromal tumor (GIST). Hypo- |
Fig. 7.5 Gastrointestinal stromal tumor (GIST). Endo- |
echoic tumor in the wall of the stomach. |
scopic view; the biopsies were negative. |
Carcinoma






















































Focal adenocarcinoma may arise anywhere within the stomach (Table 7.3). Frequently, sonography will demonstrate a pathological concentric gut signature limited to the gastric antrum or cardia, while focal pathological atypical (off-center) gut signatures are more common in the corpus and rare in the fundus of the stomach. The typical lesion is visualized as a pathological thickening of the gastric wall with loss of the usual layering. Quite often the lesion is poorly delineated at the gastric lumen, and in case of concentric tumors it is not uncommon to encounter a stenotic lumen; in such cases there will be retention of food proximal to the stenosis. The immediate vicinity of the tumor shows a characteristic loss of peristalsis, while the pathological gut signature is hard and not compliant. The surface of the tumor may either be smooth or irregular. In advanced gastric carcinoma, there may be free fluid as well as lymphadenopathy around the pancreas, the porta hepatis, and/or the celiac axis (Figs. 7.6, 7.7, 7.8).
Fig. 7.6 Pathological gut signature with eccentric loss of wall layering, irregular and clearly thickened wall, ill-de- fined inner margin, and narrowed lumen.
Table 7.3 The sites of gastric adenocarcinoma
Site |
Frequency (%) |
Antrum |
50–80 |
Corpus/fundus |
20–30 |
Cardia |
10–20 |
267
7
Gastrointestinal Tract
Fig. 7.7 Carcinoma of the gastric cardia. Irregular, abnormal target sign.
fFig. 7.8 Gastric carcinoma. Thickened, ovoid, pathological gut signature of the gastric antrum in the longitudinal plane; caudally, an enlarged pathologic lymph node.
Lymphoma































Gastric lymphoma may be visible on ultrasound as a focal hypoechoic mass involving the wall of the stomach, with clearly evident hypervascularity and loss of its typical layered appearance.
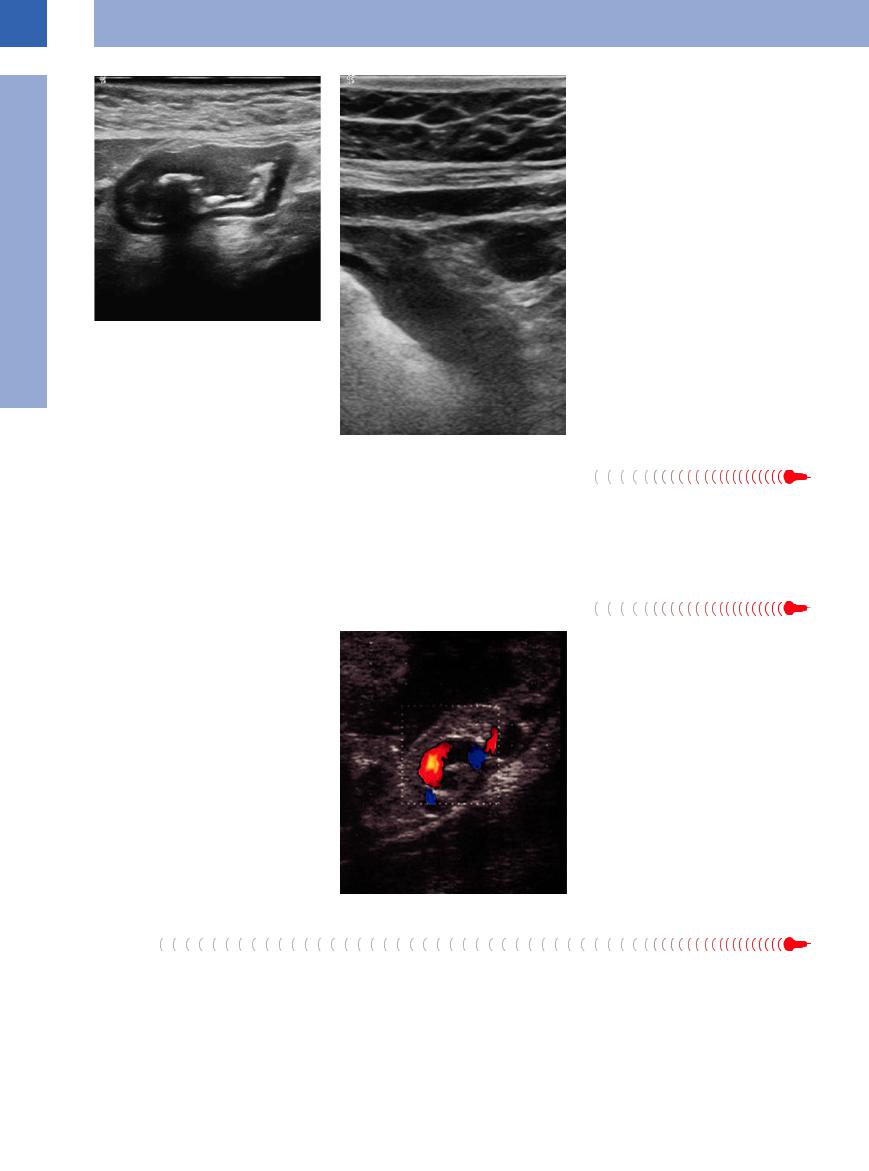
Gastric Varices





























Varices of the gastric wall are quite common in portal hypertension; owing to their tortuous course, sectional views of these varices will appear as small anechoic/hypoechoic cystoid structures on the outside of the gastric wall (Fig. 7.9). At the gastric fundus and cardia, as well as at the distal esophagus, they may protrude transmurally into the lumen of the stomach as esophageal or fundic varices. Color flow Doppler scanning will demonstrate a ribbonlike hepatofugal portovenous blood flow.
Fig. 7.9 Gastric varices. Endosonography demonstrating varices in the gastric wall in portal hypertension.
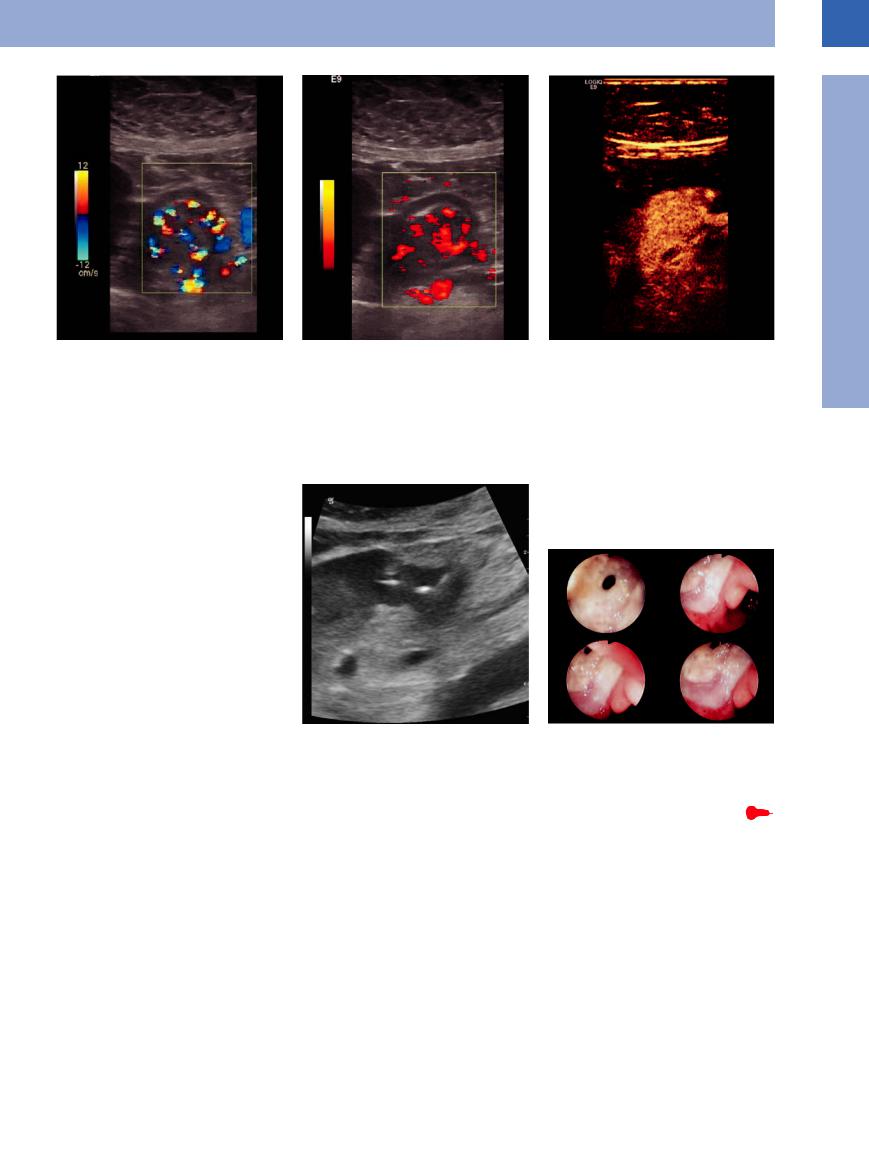
GAVE
Gastric antral vascular ectasia (GAVE syndrome) is a rare disease and is mainly seen in older women with autoimmune diseases or in portal hypertension. Pathomorphologically, it is a focal arteriovenous malformation, more pre-
cisely a vascular ectasia in the antrum of the stomach. This malformation can be seen by color Doppler sonography and by contrast-en- hanced ultrasonography (CEUS; Fig. 7.10a–c).
268
7
Stomach
Fig. 7.10 GAVE syndrome. Demonstration of a thick |
b Power Doppler. |
pathologic hypervascularity of the gastric antrum like |
|
an arteriovenous malformation. |
|
a CDS. |
|
c CEUS, 14 s after injection; demonstration of the feeding artery branching off the gastroduodenal artery.
Ulceration 






















































Most gastric ulcers are far too small to be visualized on transabdominal ultrasound. At the ulceration, the gastric wall is thinned out and has lost its layered appearance; trapped air or food particles will often be seen within the cavity of the ulcer, resulting in a coarse echo. Peristalsis will spare the area of the lesion. The liver, pancreas, or greater omentum may wall off any possible penetration, and in other cases there may be free fluid, while free air can sometimes be demonstrated in frank perforation (Fig. 7.11, Fig. 7.12).
Fig. 7.11 Gastric ulcer perforation. Pathologic gut signature of the antrum with covered gas at the outer margin.
Fig. 7.12 Gastric ulcer perforation. Endoscopic view.
Diverticula, Mucosal Folds 













































Diverticulum-like sacculation in the gastric wall is rare; when looking at all wall layers there will be focal excavation of the lumen.
Transverse sections through rugal hypertrophy at the gastric body may mimic focal polypoid wall lesions.
269
