
- •Contents
- •Preface
- •Contributors
- •1 Vessels
- •1.1 Aorta, Vena Cava, and Peripheral Vessels
- •Aorta, Arteries
- •Anomalies and Variant Positions
- •Dilatation
- •Stenosis
- •Wall Thickening
- •Intraluminal Mass
- •Perivascular Mass
- •Vena Cava, Veins
- •Anomalies
- •Dilatation
- •Intraluminal Mass
- •Compression, Infiltration
- •1.2 Portal Vein and Its Tributaries
- •Enlarged Lumen Diameter
- •Portal Hypertension
- •Intraluminal Mass
- •Thrombosis
- •Tumor
- •2 Liver
- •Enlarged Liver
- •Small Liver
- •Homogeneous Hypoechoic Texture
- •Homogeneous Hyperechoic Texture
- •Regionally Inhomogeneous Texture
- •Diffuse Inhomogeneous Texture
- •Anechoic Masses
- •Hypoechoic Masses
- •Isoechoic Masses
- •Hyperechoic Masses
- •Echogenic Masses
- •Irregular Masses
- •Differential Diagnosis of Focal Lesions
- •Diagnostic Methods
- •Suspected Diagnosis
- •3 Biliary Tree and Gallbladder
- •3.1 Biliary Tree
- •Thickening of the Bile Duct Wall
- •Localized and Diffuse
- •Bile Duct Rarefaction
- •Localized and Diffuse
- •Bile Duct Dilatation and Intraductal Pressure
- •Intrahepatic
- •Hilar and Prepancreatic
- •Intrapancreatic
- •Papillary
- •Abnormal Intraluminal Bile Duct Findings
- •Foreign Body
- •The Seven Most Important Questions
- •3.2 Gallbladder
- •Changes in Size
- •Large Gallbladder
- •Small/Missing Gallbladder
- •Wall Changes
- •General Hypoechogenicity
- •General Hyperechogenicity
- •General Tumor
- •Focal Tumor
- •Intraluminal Changes
- •Hyperechoic
- •Hypoechoic
- •Nonvisualized Gallbladder
- •Missing Gallbladder
- •Obscured Gallbladder
- •4 Pancreas
- •Diffuse Pancreatic Change
- •Large Pancreas
- •Small Pancreas
- •Hypoechoic Texture
- •Hyperechoic Texture
- •Focal Changes
- •Anechoic Lesion
- •Hypoechoic Lesion
- •Isoechoic Lesion
- •Hyperechoic Lesion
- •Irregular (Complex Structured) Lesion
- •Dilatation of the Pancreatic Duct
- •Marginal/Mild Dilatation
- •Marked Dilatation
- •5 Spleen
- •Nonfocal Changes of the Spleen
- •Diffuse Parenchymal Changes
- •Large Spleen
- •Small Spleen
- •Focal Changes of the Spleen
- •Anechoic Mass
- •Hypoechoic Mass
- •Hyperechoic Mass
- •Splenic Calcification
- •6 Lymph Nodes
- •Peripheral Lymph Nodes
- •Head/Neck
- •Extremities (Axilla, Groin)
- •Abdominal Lymph Nodes
- •Porta Hepatis
- •Splenic Hilum
- •Mesentery (Celiac, Upper and Lower Mesenteric Station)
- •Stomach
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •Small/Large Intestine
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •8 Peritoneal Cavity
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Wall Structures
- •Smooth Margin
- •Irregular Margin
- •Intragastric Processes
- •Intraintestinal Processes
- •9 Kidneys
- •Anomalies, Malformations
- •Aplasia, Hypoplasia
- •Cystic Malformation
- •Anomalies of Number, Position, or Rotation
- •Fusion Anomaly
- •Anomalies of the Renal Calices
- •Vascular Anomaly
- •Diffuse Changes
- •Large Kidneys
- •Small Kidneys
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Irregular Structure
- •Circumscribed Changes
- •Anechoic Structure
- •Hypoechoic or Isoechoic Structure
- •Complex Structure
- •Hyperechoic Structure
- •10 Adrenal Glands
- •Enlargement
- •Anechoic Structure
- •Hypoechoic Structure
- •Complex Echo Structure
- •Hyperechoic Structure
- •11 Urinary Tract
- •Malformations
- •Duplication Anomalies
- •Dilatations and Stenoses
- •Dilated Renal Pelvis and Ureter
- •Anechoic
- •Hypoechoic
- •Hypoechoic
- •Hyperechoic
- •Large Bladder
- •Small Bladder
- •Altered Bladder Shape
- •Intracavitary Mass
- •Hypoechoic
- •Hyperechoic
- •Echogenic
- •Wall Changes
- •Diffuse Wall Thickening
- •Circumscribed Wall Thickening
- •Concavities and Convexities
- •12.1 The Prostate
- •Enlarged Prostate
- •Regular
- •Irregular
- •Small Prostate
- •Regular
- •Echogenic
- •Circumscribed Lesion
- •Anechoic
- •Hypoechoic
- •Echogenic
- •12.2 Seminal Vesicles
- •Diffuse Change
- •Hypoechoic
- •Circumscribed Change
- •Anechoic
- •Echogenic
- •Irregular
- •12.3 Testis, Epididymis
- •Diffuse Change
- •Enlargement
- •Decreased Size
- •Circumscribed Lesion
- •Anechoic or Hypoechoic
- •Irregular/Echogenic
- •Epididymal Lesion
- •Anechoic
- •Hypoechoic
- •Intrascrotal Mass
- •Anechoic or Hypoechoic
- •Echogenic
- •13 Female Genital Tract
- •Masses
- •Abnormalities of Size or Shape
- •Uterus
- •Abnormalities of Size or Shape
- •Myometrial Changes
- •Intracavitary Changes
- •Endometrial Changes
- •Fallopian Tubes
- •Hypoechoic Mass
- •Anechoic Cystic Mass
- •Solid Echogenic or Nonhomogeneous Mass
- •14 Thyroid Gland
- •Diffuse Changes
- •Enlarged Thyroid Gland
- •Small Thyroid Gland
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Circumscribed Changes
- •Anechoic
- •Hypoechoic
- •Isoechoic
- •Hyperechoic
- •Irregular
- •Differential Diagnosis of Hyperthyroidism
- •Types of Autonomy
- •15 Pleura and Chest Wall
- •Chest Wall
- •Masses
- •Parietal Pleura
- •Nodular Masses
- •Diffuse Pleural Thickening
- •Pleural Effusion
- •Anechoic Effusion
- •Echogenic Effusion
- •Complex Effusion
- •16 Lung
- •Masses
- •Anechoic Masses
- •Hypoechoic Masses
- •Complex Masses
- •Index
3
Biliary Tree and Gallbladder
■ Thickening of the Bile Duct Wall
Localized and Diffuse
|
|
|
|
Thickening of the Bile Duct Wall |
|
|
Benign Thickening of the Bile Duct Wall |
||
Tree |
|
||||||||
|
|
|
Localized and Diffuse |
|
|
Malignant Thickening of the Bile Duct Wall |
|||
|
|
|
|
||||||
|
|
|
|
Bile Duct Rarefaction |
|
|
|
||
Biliary |
|
|
|
|
|||||
|
Bile Duct Dilatation and Intraductal Pressure |
|
|
|
|||||
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Abnormal Intraluminal Bile Duct Findings |
|
|
|
||
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
||
|
|
|
|
|
Differential Diagnosis of Sonographic |
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
Cholestasis |
|
|
|
||
Benign Thickening of the
of the Bile Duct
Bile Duct Wall
Wall






































Transcutaneous ultrasonography can assess localized benign thickening of the bile duct wall in two disorders of the biliary system: intrahepatic and extrahepatic presentation of primary sclerosing cholangitis (PSC) (Fig. 3.6), and the solely extrahepatic manifestation of (severe) suppurative cholangitis (Fig. 3.7). Except for a few cases, in both instances the sonographic morphology cannot be considered as primary proof but rather “suggests” the suspected diagnosis, with a greater or lesser degree of probability, which then will have to be confirmed by other means (clinical findings,
blood chemistry, and endoscopic retrograde cholangiography).
The prolonged course of chronic inflammatory bowel disease (Crohn disease, ulcerative colitis) is often accompanied by the sonographic telltale signs of PSC, from segmental diffuse bile duct wall thickening all the way to complete obstruction of the lumen, alternating with dilated/ectatic bile duct segments; ducts may also appear simply to break off, and intraductal sludge is a frequent finding (Fig. 3.6a,b). It is not possible to rule out early cholangiocellular carcinoma (CCC), and even fine-needle aspiration cytology has its prob-
lems. PSC-like changes have been described for HIV infections with manifest AIDS symptoms.
Acute suppurative cholangitis may result in thickening of the common duct wall, which can be demonstrated for the extrahepatic segment. This thickening of the wall becomes particularly evident if endoscopic intervention (endoscopic papillotomy, EPT) has provided pressure relief by removing or bypassing the biliary obstruction: the dilated bile duct walls, originally thinned out by their distension, collapse and their inflamed and swollen true structure becomes exceptionally well visualized (Fig. 3.7a).
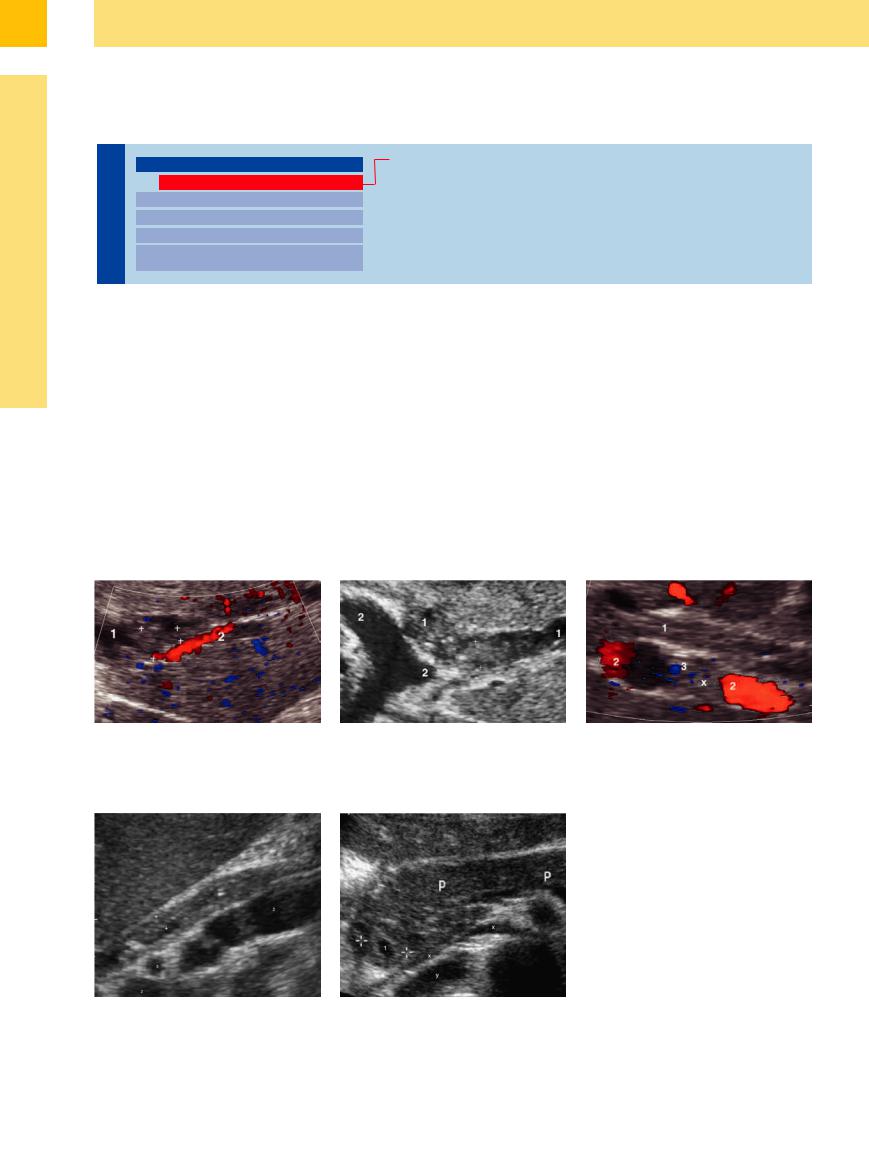
Fig. 3.6 Primary sclerosing cholangitis.
a Dilatation and wall thickening (calipers) of the intrahepatic bile duct (1) in segment III. Accompanying branch of the portal vein (2).
b Dilation and thickening of the wall of the intrahepatic branch of a bile duct (1) in segment III and II, rudimentary also (ventral) second intrahepatic branching of a portal vessel (2).
c Wall thickening (“sclerosis”) of the common duct (1); hepatic artery (3) crossing in between.
Fig. 3.7
a Suppurative cholangitis, subsiding after endoscopic papillotomy and extraction of calculi, with thickened wall (calipers) of the common duct (1); portal vein (2); hepatic artery (3) crossing in between.
b Wall thickening of the prepapillar intrahepatic CBD (cursors) after stent delivery – accentuated lumen (1); pancreas (P), left renal artery and collapsed caval vein (x), right renal artery (y).
130

Malignant Thickening of the Bile
of the Bile Duct
Duct Wall
Wall




































Malignant bile duct wall thickening may be localized as in CCC or infiltrating as in hepatocellular carcinoma (HCC), and in both cases ultrasound detects these changes solely in terms of the resulting biliary obstruction with its subsequent prestenotic dilatation of the duct. Consequently, these entities are discussed
in the section on pressure-induced bile duct dilatation.
One rare special case is mucinous biliary papillomatosis with its fluent transition to well-differentiated cholangiocarcinoma (Fig. 3.8). The ultrasound findings show a nonexpansile solid mass originating in the surrounding bile duct wall, which it dilates to
sometimes bizarre shapes, but well defined and demarcated from the bile duct wall itself; complete biliary obstruction tends to occur late in the disease. It has a rather indolent course (over many years), and treatment is characterized by effective long-term interventional endoscopy (stenting, removal of the tumor masses).
3
Thickening of the Bile Duct Wall
Fig. 3.8
a Obstruction of the common duct (1) in intraductal spread of cholangiocarcinoma (xx); portal vein (2); hepatic artery (3).
b Tumor invasion into the CBD.
d Biliary obstruction of the left liver lobe—increased (biliary) fluid content of the left lobe in contrast to the right lobe (therefore only under this condition is there exact differentiation of both liver lobes).
c Klatskin tumor (CCC) involving the hepatic duct bifurcation (arrows) and infiltrating the right (1) and left (2) hepatic duct. Middle: Corresponding ERC with tumor stenosis of the right (1) and left (2) hepatic duct. Right: After double stent implantation (x,y): diminished stasis of the hepatic ducts (1, 2).
131
