
- •Contents
- •Preface
- •Contributors
- •1 Vessels
- •1.1 Aorta, Vena Cava, and Peripheral Vessels
- •Aorta, Arteries
- •Anomalies and Variant Positions
- •Dilatation
- •Stenosis
- •Wall Thickening
- •Intraluminal Mass
- •Perivascular Mass
- •Vena Cava, Veins
- •Anomalies
- •Dilatation
- •Intraluminal Mass
- •Compression, Infiltration
- •1.2 Portal Vein and Its Tributaries
- •Enlarged Lumen Diameter
- •Portal Hypertension
- •Intraluminal Mass
- •Thrombosis
- •Tumor
- •2 Liver
- •Enlarged Liver
- •Small Liver
- •Homogeneous Hypoechoic Texture
- •Homogeneous Hyperechoic Texture
- •Regionally Inhomogeneous Texture
- •Diffuse Inhomogeneous Texture
- •Anechoic Masses
- •Hypoechoic Masses
- •Isoechoic Masses
- •Hyperechoic Masses
- •Echogenic Masses
- •Irregular Masses
- •Differential Diagnosis of Focal Lesions
- •Diagnostic Methods
- •Suspected Diagnosis
- •3 Biliary Tree and Gallbladder
- •3.1 Biliary Tree
- •Thickening of the Bile Duct Wall
- •Localized and Diffuse
- •Bile Duct Rarefaction
- •Localized and Diffuse
- •Bile Duct Dilatation and Intraductal Pressure
- •Intrahepatic
- •Hilar and Prepancreatic
- •Intrapancreatic
- •Papillary
- •Abnormal Intraluminal Bile Duct Findings
- •Foreign Body
- •The Seven Most Important Questions
- •3.2 Gallbladder
- •Changes in Size
- •Large Gallbladder
- •Small/Missing Gallbladder
- •Wall Changes
- •General Hypoechogenicity
- •General Hyperechogenicity
- •General Tumor
- •Focal Tumor
- •Intraluminal Changes
- •Hyperechoic
- •Hypoechoic
- •Nonvisualized Gallbladder
- •Missing Gallbladder
- •Obscured Gallbladder
- •4 Pancreas
- •Diffuse Pancreatic Change
- •Large Pancreas
- •Small Pancreas
- •Hypoechoic Texture
- •Hyperechoic Texture
- •Focal Changes
- •Anechoic Lesion
- •Hypoechoic Lesion
- •Isoechoic Lesion
- •Hyperechoic Lesion
- •Irregular (Complex Structured) Lesion
- •Dilatation of the Pancreatic Duct
- •Marginal/Mild Dilatation
- •Marked Dilatation
- •5 Spleen
- •Nonfocal Changes of the Spleen
- •Diffuse Parenchymal Changes
- •Large Spleen
- •Small Spleen
- •Focal Changes of the Spleen
- •Anechoic Mass
- •Hypoechoic Mass
- •Hyperechoic Mass
- •Splenic Calcification
- •6 Lymph Nodes
- •Peripheral Lymph Nodes
- •Head/Neck
- •Extremities (Axilla, Groin)
- •Abdominal Lymph Nodes
- •Porta Hepatis
- •Splenic Hilum
- •Mesentery (Celiac, Upper and Lower Mesenteric Station)
- •Stomach
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •Small/Large Intestine
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •8 Peritoneal Cavity
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Wall Structures
- •Smooth Margin
- •Irregular Margin
- •Intragastric Processes
- •Intraintestinal Processes
- •9 Kidneys
- •Anomalies, Malformations
- •Aplasia, Hypoplasia
- •Cystic Malformation
- •Anomalies of Number, Position, or Rotation
- •Fusion Anomaly
- •Anomalies of the Renal Calices
- •Vascular Anomaly
- •Diffuse Changes
- •Large Kidneys
- •Small Kidneys
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Irregular Structure
- •Circumscribed Changes
- •Anechoic Structure
- •Hypoechoic or Isoechoic Structure
- •Complex Structure
- •Hyperechoic Structure
- •10 Adrenal Glands
- •Enlargement
- •Anechoic Structure
- •Hypoechoic Structure
- •Complex Echo Structure
- •Hyperechoic Structure
- •11 Urinary Tract
- •Malformations
- •Duplication Anomalies
- •Dilatations and Stenoses
- •Dilated Renal Pelvis and Ureter
- •Anechoic
- •Hypoechoic
- •Hypoechoic
- •Hyperechoic
- •Large Bladder
- •Small Bladder
- •Altered Bladder Shape
- •Intracavitary Mass
- •Hypoechoic
- •Hyperechoic
- •Echogenic
- •Wall Changes
- •Diffuse Wall Thickening
- •Circumscribed Wall Thickening
- •Concavities and Convexities
- •12.1 The Prostate
- •Enlarged Prostate
- •Regular
- •Irregular
- •Small Prostate
- •Regular
- •Echogenic
- •Circumscribed Lesion
- •Anechoic
- •Hypoechoic
- •Echogenic
- •12.2 Seminal Vesicles
- •Diffuse Change
- •Hypoechoic
- •Circumscribed Change
- •Anechoic
- •Echogenic
- •Irregular
- •12.3 Testis, Epididymis
- •Diffuse Change
- •Enlargement
- •Decreased Size
- •Circumscribed Lesion
- •Anechoic or Hypoechoic
- •Irregular/Echogenic
- •Epididymal Lesion
- •Anechoic
- •Hypoechoic
- •Intrascrotal Mass
- •Anechoic or Hypoechoic
- •Echogenic
- •13 Female Genital Tract
- •Masses
- •Abnormalities of Size or Shape
- •Uterus
- •Abnormalities of Size or Shape
- •Myometrial Changes
- •Intracavitary Changes
- •Endometrial Changes
- •Fallopian Tubes
- •Hypoechoic Mass
- •Anechoic Cystic Mass
- •Solid Echogenic or Nonhomogeneous Mass
- •14 Thyroid Gland
- •Diffuse Changes
- •Enlarged Thyroid Gland
- •Small Thyroid Gland
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Circumscribed Changes
- •Anechoic
- •Hypoechoic
- •Isoechoic
- •Hyperechoic
- •Irregular
- •Differential Diagnosis of Hyperthyroidism
- •Types of Autonomy
- •15 Pleura and Chest Wall
- •Chest Wall
- •Masses
- •Parietal Pleura
- •Nodular Masses
- •Diffuse Pleural Thickening
- •Pleural Effusion
- •Anechoic Effusion
- •Echogenic Effusion
- •Complex Effusion
- •16 Lung
- •Masses
- •Anechoic Masses
- •Hypoechoic Masses
- •Complex Masses
- •Index
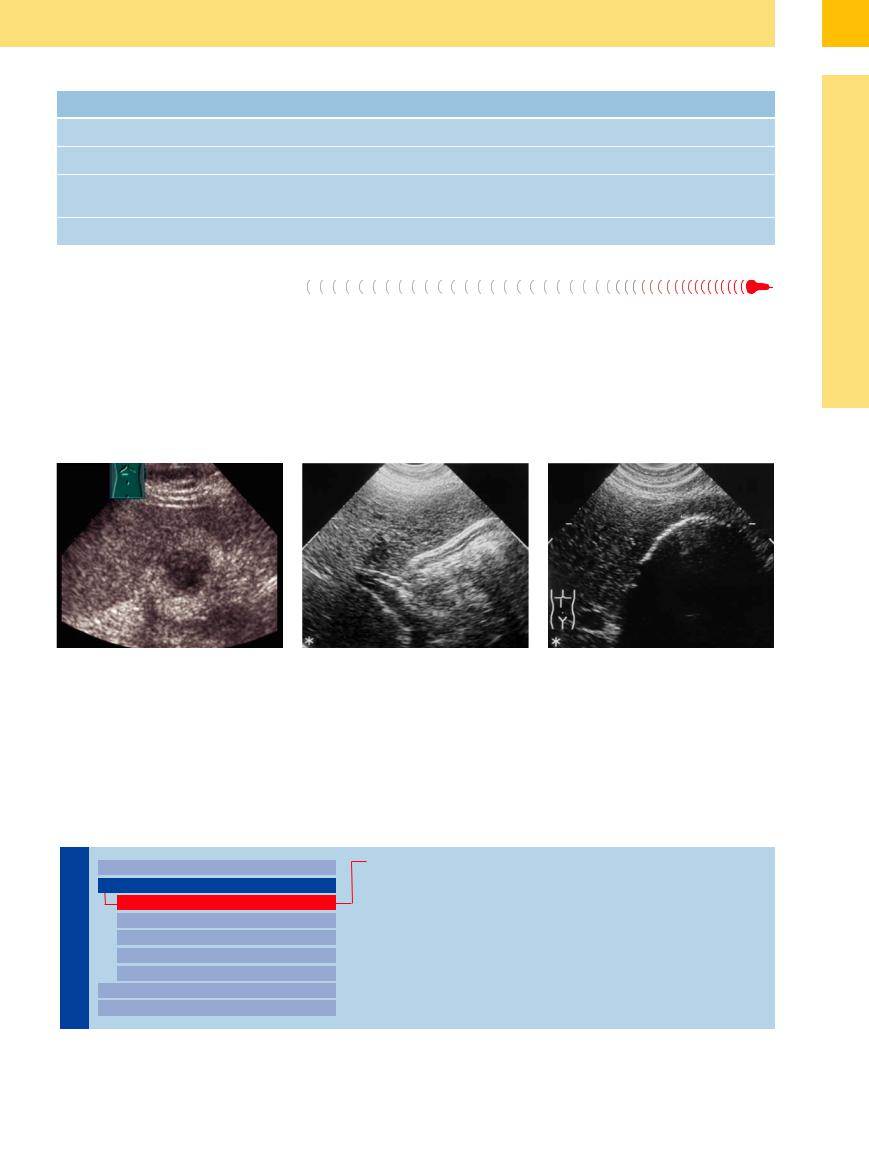
Table 3.1 Gallbladder changes in nonbiliary disorders |
|
|
||
|
Right-sided heart failure |
Cirrhosis of the liver |
Severe malabsorption |
Acute hepatitis |
Size |
Normal or enlarged |
More likely small |
Normal or enlarged |
More likely small |
Shape |
Normal or little fluid |
Normal or little fluid |
Smooth or rippled |
Ovoid, little fluid |
Wall |
Smooth hypoechoic wall thick- |
Smooth hypoechoic wall thick- |
Wall thickening of mixed |
Smooth hypoor hyperechoic |
|
ening |
ening, possibly varicose veins |
echogenicity |
wall thickening |
Surroundings |
Signs of cardiac congestion |
Ascites |
Edema of the intestinal wall |
Lymph nodes |
Symptomatic (Pathological) 


Most fasting gallbladders with low or no fluid levels result from cystic duct obstruction (Fig. 3.43).
Inflammatory atrophy of the gallbladder with its lack of fluid is usually caused by chronic cholecystitis, where the shape of the gallbladder is irregular and its wall thickened and inhomogeneous (hyperechoic) (Fig. 3.45, Fig. 3.46). During acute exacerbation, hypo-
echoic areas in the wall may also be visualized. A typical finding would be several, sometimes even encrusted, intraluminal gallstones. In the end the atrophic gallbladder can only be identified by the encrusted calculi within the scar tissue.
This contracted gallbladder with its gallstones is characterized by a crescent-shaped band of echoes without demonstration of the
posterior wall. Sometimes even the anterior wall with its scar contraction may hardly be delimited from the gallstone echoes (Fig. 3.46). In these patients, differentiation of a possible concurrent gallbladder carcinoma can be problematic.
Fig. 3.45 Inflammatory atrophic gallbladder. Atrophied |
b Completely folded-over gallbladder wall; the underly- |
Fig. 3.46 The contracted gallbladder with low levels of |
gallbladder (GB) void of any fluid. |
ing gallstone obstructing the cystic duct is not depicted |
liquid and filled with gallstones is characterized by a |
a Calculous atrophied gallbladder. The atrophied gall- |
in this image. |
crescent-shaped band of echoes at the base and a blurry |
bladder is visualized as a crescent-shaped band of echoes |
|
ventral wall. The demonstration of the posterior wall |
in the hepatic fossa with ill-defined contour of the anterior |
|
often is impossible due to the gallstone echoes. |
wall. Usually, the posterior wall cannot be demonstrated |
|
|
due to posterior shadowing (S) of the gallstones. |
|
|
■ Wall Changes
General Hypoechogenicity
Gallbladder |
|
|
|
Changes in Size |
|
|
Acute Cholecystitis |
|
|
||||||
|
|
|
Wall Changes |
|
|
Special Cases |
|
|
|
|
|
|
|
||
|
|
|
|
General Hypoechogenicity |
|
|
Wall Thickening in Hepatic/ |
|
|
|
|
|
|||
|
|
|
|
General Hyperechogenicity |
|
|
Pancreatic Disorders and Trauma |
|
|
|
|
Focal Hypoechogenicity/Hyperechogenicity |
|
|
|
|
|
|
|
General Tumor |
|
|
|
|
|
|
|
Focal Tumor |
|
|
|
|
|
|
|
Intraluminal Changes |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Nonvisualized Gallbladder |
|
|
|
|
|
|
|
|
|
|
3
Wall Changes
151
3
Biliary Tree and Gallbladder
Acute Cholecystitis 







Acute and chronic cholecystitis is characterized by uneven thickening of the gallbladder wall with irregular echo pattern. The typical finding in acute cholecystitis is the tensely distended afunctional/dysfunctional gallbladder with its hypoechoic wall that is tender on palpation (positive Murphy’s sign). Another sign is the ill-defined intraluminal and extraluminal contour of the wall, accompanied by hypoechoic inflammation of the surrounding tissue (pericholecystitis). Ultrasound morphology of the gallbladder wall spans the spectrum from diffuse hypoechoic thickening with poorly delim-
ited contour of the wall ( 3.6a,b) through hypoechoic necrosis all the way to complete destruction of the wall (
3.6a,b) through hypoechoic necrosis all the way to complete destruction of the wall ( 3.6c; see Table 3.2).9 Intraluminal hyperechoic or inhomogeneously echogenic material can point the way to the diagnosis of cholecystic empyema.
3.6c; see Table 3.2).9 Intraluminal hyperechoic or inhomogeneously echogenic material can point the way to the diagnosis of cholecystic empyema.
Advanced and severe courses of acute cholecystitis may result in necrosis of the mucosa and filiform detachment of the tunica mucosa ( 3.6e). Usually, these cases present with hyperechoic inhomogeneous necrotic debris within the gallbladder. A pericholecystic film is typical of localized perforation (
3.6e). Usually, these cases present with hyperechoic inhomogeneous necrotic debris within the gallbladder. A pericholecystic film is typical of localized perforation ( 3.6 d,e).
3.6 d,e).
Lacelike structures with hypoechoic necrotic areas are infrequent findings.
Imminent perforation may be preceded by ascites, ulcers of the gallbladder wall, or pericholecystic infiltrates/abscesses ( 3.6f). Hypervascularization of the gallbladder wall in color-flow duplex scanning of cholecystitis is by no means mandatory. The histological grading of edematous, phlegmonous, and gangrenous cholecystitis cannot be differentiated very well by ultrasound.
3.6f). Hypervascularization of the gallbladder wall in color-flow duplex scanning of cholecystitis is by no means mandatory. The histological grading of edematous, phlegmonous, and gangrenous cholecystitis cannot be differentiated very well by ultrasound.
Special Cases 




















































Emphysematous cholecystitis. The characteristic sign of emphysematous cholecystitis is intraluminal and intramural gas (from infection by gas-producing pathogens) ( 3.6 g,h).
3.6 g,h).
Acalculous and xanthogranulomatous cholecystitis. Other special cases are acalculous ( 3.6i) and xanthogranulomatous (
3.6i) and xanthogranulomatous ( 3.6j,k) cholecystitis. Acalculous cholecystitis is a typical disorder in the immune-compromised patient in the intensive care unit or after chemotherapy. It is characterized by a nonfunctional gallbladder that is tender on palpation, with edema of the wall and possible sludge. In large hydropic gallbladders, ultrasound may only demonstrate slight thickening of the wall despite the presence of phlegmon. Xanthogranu-
3.6j,k) cholecystitis. Acalculous cholecystitis is a typical disorder in the immune-compromised patient in the intensive care unit or after chemotherapy. It is characterized by a nonfunctional gallbladder that is tender on palpation, with edema of the wall and possible sludge. In large hydropic gallbladders, ultrasound may only demonstrate slight thickening of the wall despite the presence of phlegmon. Xanthogranu-
Table 3.2 Differentiating cholecystitis
|
Acute cholecystitis |
Size |
Large |
Shape |
Irregular |
Echogenicity |
Hypoechoic—layered |
Lumen |
Large, calculi |
Wall |
Thickened |
lomatous cholecystitis, on the other hand, is characterized by pseudotumorous thickening of the wall with loss of the usual layering.
Chronic cholecystitis
Normal or atrophied
Round
Hyperechoic
Small or lacking
Thickened
This entity is almost impossible to differentiate from gallbladder carcinoma on the basis of sonographic morphology alone.
Wall Thickening in Hepatic/Pancreatic
in Hepatic/Pancreatic Disorders and
Disorders and Trauma
Trauma 


























The differential diagnosis of cholecystic wall changes has to include not only calculous cholecystitis but also wall thickening secondary to acute hepatitis, decompensated cirrhosis of the liver, and acute episodes of (chronic) pancreatitis ( 3.6 m–p).
3.6 m–p).
152

 3.6 Acute Cholecystitis: Complications and Special Cases
3.6 Acute Cholecystitis: Complications and Special Cases
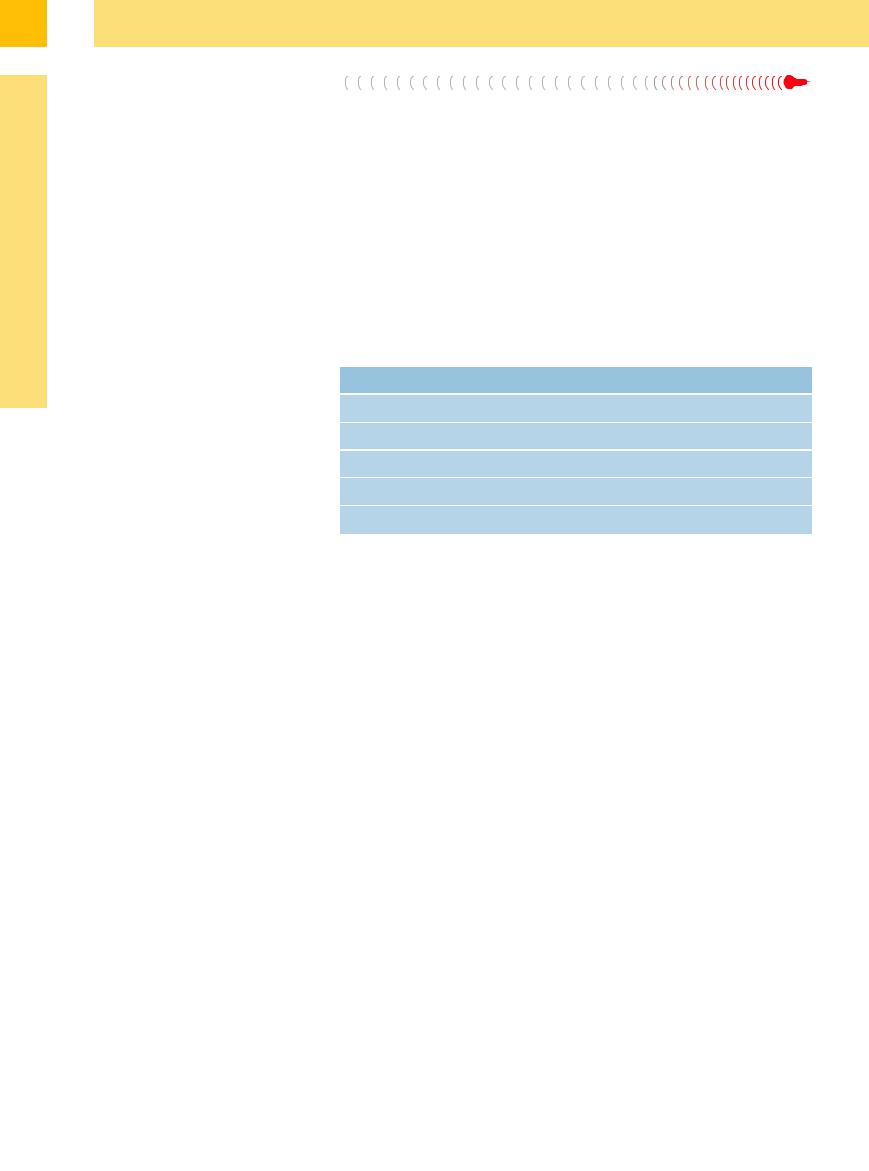
a Acute cholecystitis in cholecystolithia- |
b Acute phlegmonous cholecystitis: en- |
c Necrotizing cholecystitis: complete sep- |
d Perforated gallbladder with intrahepatic |
sis: irregularly thickened gallbladder wall |
larged gallbladder with painful palpation: |
aration of the wall layering; fistula to the |
bile leak (bilioma); phlegmonous gall- |
with positive Murphy’s sign. |
ill-defined (hypoechoic) wall and small |
abdomen wall (x). |
bladder with sludge in the lumen, peri- |
|
amount of sludge in the lumen; side-lobe |
|
cholecystic bile leak with fluid (bile). |
|
artifact. |
|
|
3
Wall Changes
e Perforated gallbladder: phlegmonous gallbladder with filiform desquamation and extensive pericholecystic intraperitoneal fluid (bile).
f Empyema of the gallbladder with extensive cholecystitis and pericholecystic abscess.
g Emphysematous cholecystitis: extensive intramural gas collection in emphysematous cholecystitis.
h Emphysematous cholecystitis with mild gas formation: difficult study conditions may render the diagnosis more problematic (image courtesy of Dr. W.B. Stelzel, Frankfurt, Germany).
i Acalculous cholecystitis in an ICU patient with total parenteral nutrition: gallbladder tender on palpation, with or without sludge and wall edema.
j and k Xanthogranulomatous cholecystitis: rare special case with tumor-like thickening of the gallbladder wall and complete loss of normal wall layering (images courtesy of Dr. W.B. Stelzel, Frankfurt, Germany).
l Differentiation of the chronic cholecystitis: hyperechoic (callous) irregular wall thickening.
m Intensive complex thickening of the gallbladder wall without fluid in acute hepatitis and AIDS.
n Hypoechoic swelling of the wall (cursors) in decompensated toxic liver cirrhosis.
o Concurrent inflammatory wall thickening in an acute episode of chronic pancreatitis; perihepatic fluid film (arrows); surgery did not yield any gallstones.
p Traumatic wall thickening (with initial obstruction of the lumen) as part of a contusion; sparse vascularization in colorflow Doppler scanning.
153
3
Biliary Tree and Gallbladder
General Hyperechogenicity
Gallbladder |
|
|
|
Changes in Size |
|
Chronic Cholecystitis |
|
|
|||||
|
|
|
Wall Changes |
|
Porcelain Gallbladder |
|
|
|
|
|
|
||
|
|
|
|
General Hypoechogenicity |
|
|
|
|
|
|
|
|
|
|
|
|
|
General Hyperechogenicity |
|
|
|
|
|
|
|
|
|
|
|
|
|
Focal Hypoechogenicity/Hyperechogenicity |
|
|
|
|
|
|
General Tumor |
|
|
|
|
|
|
Focal Tumor |
|
|
|
|
|
|
Intraluminal Changes |
|
|
|
|
|
|
|
|
|
|
|
|
|
Nonvisualized Gallbladder |
|
|
|
|
|
|
|
|
Chronic Cholecystitis 
















































Chronic cholecystitis is accompanied by hyperechoic thickening of the gallbladder wall, ranging from barely noticeable to pronounced callous thickening ( 3.6 l). After oral intake these gallbladders present as dysfunctional or even nonfunctional organs. In the early stages of chronic inflammation the luminal wall displays not only areas of scarred hyperechoic thickening but also acutely inflamed (hypoechoic) lesions of the mucosa. The terminal stage of chronic scarred cholecystitis is characterized by extensive callous (hyperechoic) thickening of the wall with complete loss of layering. The
3.6 l). After oral intake these gallbladders present as dysfunctional or even nonfunctional organs. In the early stages of chronic inflammation the luminal wall displays not only areas of scarred hyperechoic thickening but also acutely inflamed (hypoechoic) lesions of the mucosa. The terminal stage of chronic scarred cholecystitis is characterized by extensive callous (hyperechoic) thickening of the wall with complete loss of layering. The
differentiation between acute and chronic cholecystitis is listed in Table 3.2.
Mirizzi syndrome. If the inflammatory changes induced by a stone impacted in the neck of the gallbladder spread beyond the border of the gallbladder on to the porta hepatis, leading to obstruction of the CBD, this may result in Mirizzi syndrome (Fig. 3.47).
Cholelithic gallbladder perforation. Spontaneous perforation of calculi into the gastrointestinal tract is a rare complication of chronic cholecystitis. Fecal studies have demonstrated
spontaneous passage of stones up to 5.7 cm in diameter. Most often the stones perforate from the gallbladder into the duodenum (52%); perforation into the stomach occurs rather infrequently (ca. 3%), while the remainder of the gastrointestinal tract is affected in 45% of cases. The ultrasound signs of a perforated stone are its atypical anatomical location, gas echoes (pneumobilia) (Fig. 3.49b) within the lumen of the gallbladder (may not be present in case of fistulas), demonstration of a fistula, and atrophic gallbladder with visualization of calculi (Fig. 3.48, Fig. 3.49).
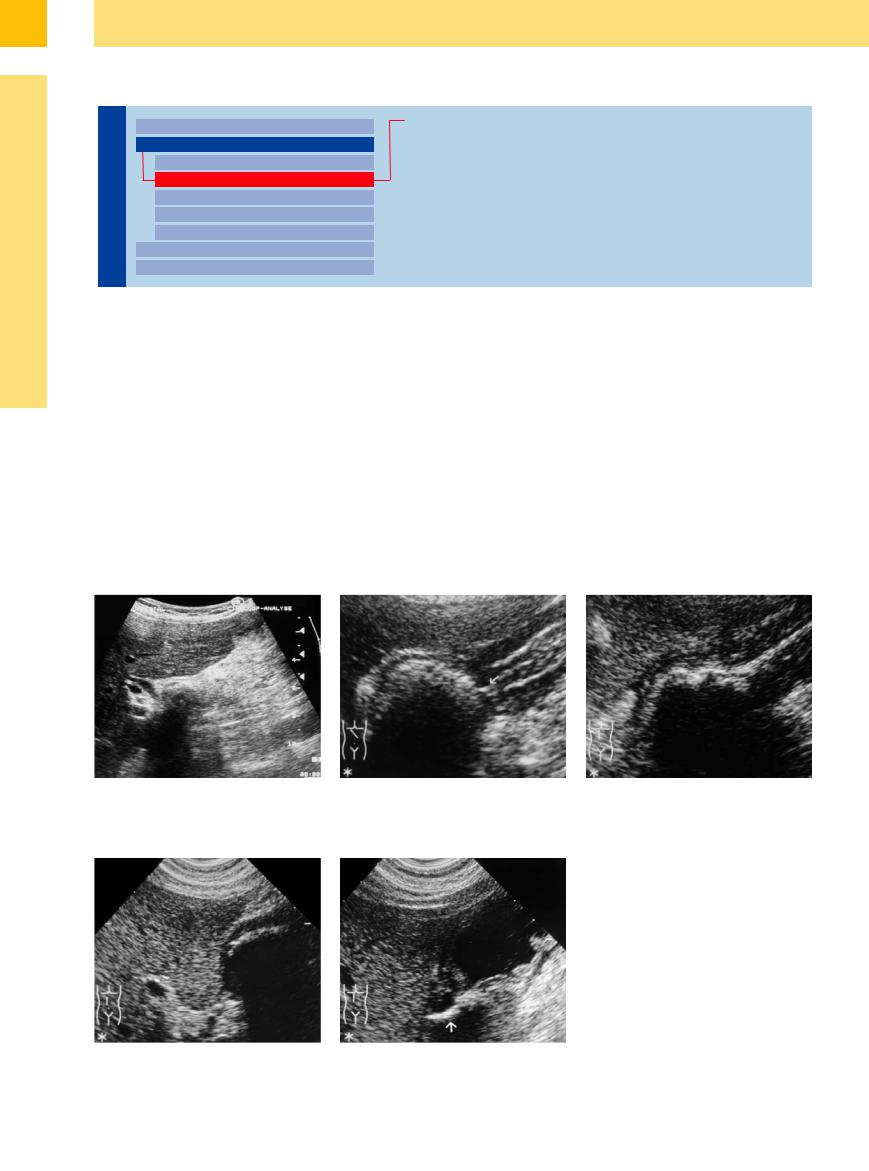
Fig. 3.47 Mirizzi syndrome: calculus impacted in the neck of the gallbladder, with adjacent inflammation and dilatation of the CBD.
Fig. 3.48 Gallstone perforation from the gallbladder into the gastric antrum.
a Barrel-shaped gallstone impacted in a fistula (arrow) between gallbladder and gastric antrum.
b Successful disintegration of the calculus into multiple fragments after extracorporeal shock-wave lithotripsy.
Fig. 3.49 Cholecystoduodenal gallstone perforation.
a Barrel-shaped gallstone impacted in the duodenal bulb after perforation through the gallbladder wall.
b Successful shock-wave lithotripsy with spontaneous passage of the fragments, now with demonstration of a wide hyperechoic fistula (arrow) between the atrophied gallbladder and the duodenal bulb (fluid-filled gastric antrum).
154
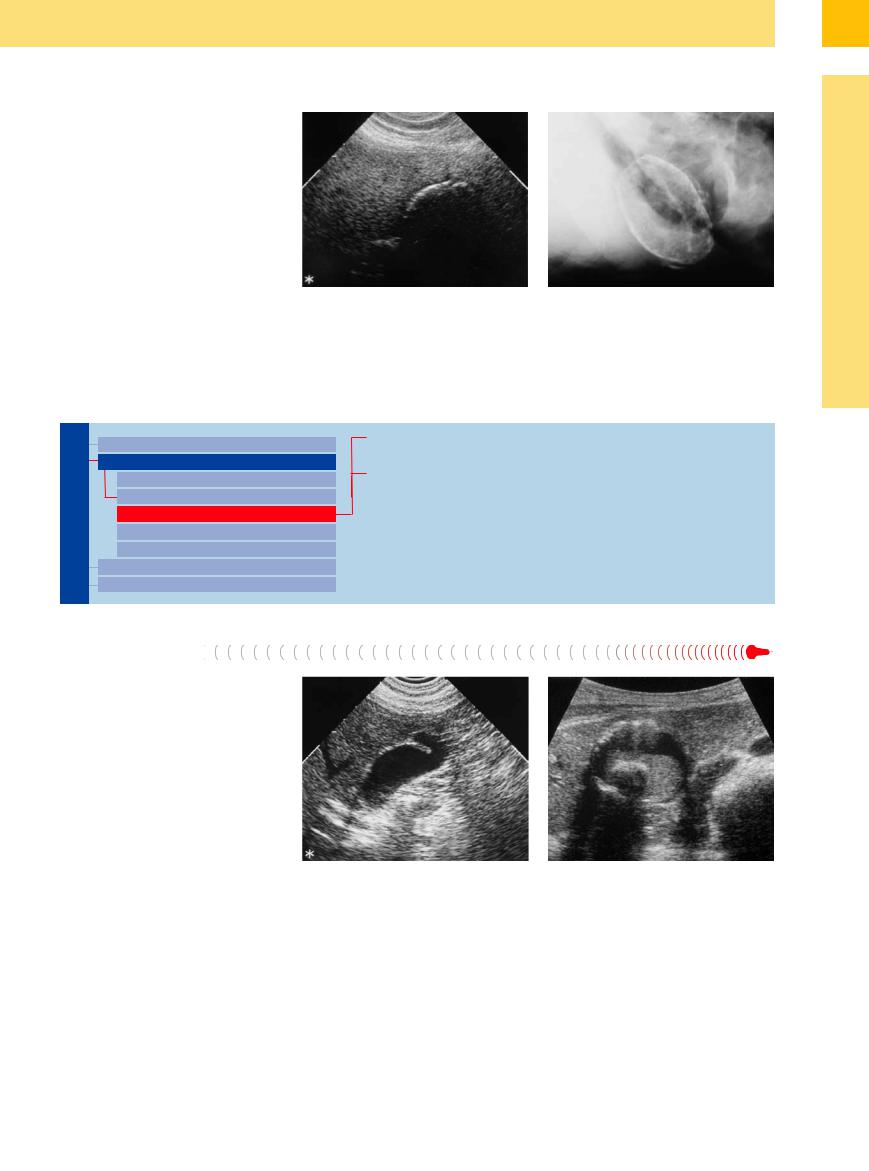
Porcelain Gallbladder
Gallbladder 
















































Porcelain gallbladder is considered a precancerous condition because in 10–60% of all cases gallbladder carcinoma will develop. Porcelain gallbladder is characterized by intramural shell-like calcification that may affect the entire wall or (more commonly) just parts of it (e. g., the fundus) (Fig. 3.50a,b, Fig. 3.52). Depending on the thickness of the calcified layer, the gallbladder wall may be sonolucent. In cases of severe calcification, any ultrasound differentiation of possible malignancy may prove to be infeasible. In the diffuse type there is complete calcification of the gallbladder wall, which may not be penetrated by the ultrasound beam in severe cases. If porcelain gallbladder is suspected, a plain radiograph of the gallbladder should be obtained (Fig. 3.50b).
Fig. 3.50
a Classic diffuse porcelain gallbladder: visualization of a broad calcified intramural crescent.
b Plain film of the gallbladder: typical radiographic image of diffuse porcelain gallbladder.
Focal Hypoechogenicity/Hyperechogenicity
Gallbladder |
Changes in Size |
Focal Inflammation |
|
Wall Changes |
Gallbladder Varicosity |
||
|
|||
|
General Hypoechogenicity |
|
|
|
General Hyperechogenicity |
|
|
|
Focal Hypoechogenicity/Hyperechogenicity |
|
|
|
General Tumor |
|
|
|
Focal Tumor |
|
|
|
Intraluminal Changes |
|
|
|
Nonvisualized Gallbladder |
|
|
Focal Inflammation |
|
||
Based on the morphology of the outflow obstruction in gallbladder anomalies, the inflammatory changes of the gallbladder wall may be focal (e. g., inflammation of the fundus in Phrygian cap). The sonographic morphology of focal inflammatory lesions resembles that of the diffuse changes (Fig. 3.51). Just as in diffuse calcification, focal calcium deposits are classified as porcelain gallbladders (see above) (Fig. 3.52). Cholecystitis in focal porcelain gallbladder may be hard to differentiate.
Fig. 3.51 Focal cholecystitis (in Phrygian cap).
Fig. 3.52 Porcelain gallbladder with sonolucent wall: fine focal calcification of the fundus wall with translucent lumen of the gallbladder and identifiable cholecystolithiasis (with sludge) (image courtesy of Dr. W.B. Stelzel, Frankfurt, Germany).
3
Wall Changes
155
