
- •Contents
- •Preface
- •Contributors
- •1 Vessels
- •1.1 Aorta, Vena Cava, and Peripheral Vessels
- •Aorta, Arteries
- •Anomalies and Variant Positions
- •Dilatation
- •Stenosis
- •Wall Thickening
- •Intraluminal Mass
- •Perivascular Mass
- •Vena Cava, Veins
- •Anomalies
- •Dilatation
- •Intraluminal Mass
- •Compression, Infiltration
- •1.2 Portal Vein and Its Tributaries
- •Enlarged Lumen Diameter
- •Portal Hypertension
- •Intraluminal Mass
- •Thrombosis
- •Tumor
- •2 Liver
- •Enlarged Liver
- •Small Liver
- •Homogeneous Hypoechoic Texture
- •Homogeneous Hyperechoic Texture
- •Regionally Inhomogeneous Texture
- •Diffuse Inhomogeneous Texture
- •Anechoic Masses
- •Hypoechoic Masses
- •Isoechoic Masses
- •Hyperechoic Masses
- •Echogenic Masses
- •Irregular Masses
- •Differential Diagnosis of Focal Lesions
- •Diagnostic Methods
- •Suspected Diagnosis
- •3 Biliary Tree and Gallbladder
- •3.1 Biliary Tree
- •Thickening of the Bile Duct Wall
- •Localized and Diffuse
- •Bile Duct Rarefaction
- •Localized and Diffuse
- •Bile Duct Dilatation and Intraductal Pressure
- •Intrahepatic
- •Hilar and Prepancreatic
- •Intrapancreatic
- •Papillary
- •Abnormal Intraluminal Bile Duct Findings
- •Foreign Body
- •The Seven Most Important Questions
- •3.2 Gallbladder
- •Changes in Size
- •Large Gallbladder
- •Small/Missing Gallbladder
- •Wall Changes
- •General Hypoechogenicity
- •General Hyperechogenicity
- •General Tumor
- •Focal Tumor
- •Intraluminal Changes
- •Hyperechoic
- •Hypoechoic
- •Nonvisualized Gallbladder
- •Missing Gallbladder
- •Obscured Gallbladder
- •4 Pancreas
- •Diffuse Pancreatic Change
- •Large Pancreas
- •Small Pancreas
- •Hypoechoic Texture
- •Hyperechoic Texture
- •Focal Changes
- •Anechoic Lesion
- •Hypoechoic Lesion
- •Isoechoic Lesion
- •Hyperechoic Lesion
- •Irregular (Complex Structured) Lesion
- •Dilatation of the Pancreatic Duct
- •Marginal/Mild Dilatation
- •Marked Dilatation
- •5 Spleen
- •Nonfocal Changes of the Spleen
- •Diffuse Parenchymal Changes
- •Large Spleen
- •Small Spleen
- •Focal Changes of the Spleen
- •Anechoic Mass
- •Hypoechoic Mass
- •Hyperechoic Mass
- •Splenic Calcification
- •6 Lymph Nodes
- •Peripheral Lymph Nodes
- •Head/Neck
- •Extremities (Axilla, Groin)
- •Abdominal Lymph Nodes
- •Porta Hepatis
- •Splenic Hilum
- •Mesentery (Celiac, Upper and Lower Mesenteric Station)
- •Stomach
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •Small/Large Intestine
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •8 Peritoneal Cavity
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Wall Structures
- •Smooth Margin
- •Irregular Margin
- •Intragastric Processes
- •Intraintestinal Processes
- •9 Kidneys
- •Anomalies, Malformations
- •Aplasia, Hypoplasia
- •Cystic Malformation
- •Anomalies of Number, Position, or Rotation
- •Fusion Anomaly
- •Anomalies of the Renal Calices
- •Vascular Anomaly
- •Diffuse Changes
- •Large Kidneys
- •Small Kidneys
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Irregular Structure
- •Circumscribed Changes
- •Anechoic Structure
- •Hypoechoic or Isoechoic Structure
- •Complex Structure
- •Hyperechoic Structure
- •10 Adrenal Glands
- •Enlargement
- •Anechoic Structure
- •Hypoechoic Structure
- •Complex Echo Structure
- •Hyperechoic Structure
- •11 Urinary Tract
- •Malformations
- •Duplication Anomalies
- •Dilatations and Stenoses
- •Dilated Renal Pelvis and Ureter
- •Anechoic
- •Hypoechoic
- •Hypoechoic
- •Hyperechoic
- •Large Bladder
- •Small Bladder
- •Altered Bladder Shape
- •Intracavitary Mass
- •Hypoechoic
- •Hyperechoic
- •Echogenic
- •Wall Changes
- •Diffuse Wall Thickening
- •Circumscribed Wall Thickening
- •Concavities and Convexities
- •12.1 The Prostate
- •Enlarged Prostate
- •Regular
- •Irregular
- •Small Prostate
- •Regular
- •Echogenic
- •Circumscribed Lesion
- •Anechoic
- •Hypoechoic
- •Echogenic
- •12.2 Seminal Vesicles
- •Diffuse Change
- •Hypoechoic
- •Circumscribed Change
- •Anechoic
- •Echogenic
- •Irregular
- •12.3 Testis, Epididymis
- •Diffuse Change
- •Enlargement
- •Decreased Size
- •Circumscribed Lesion
- •Anechoic or Hypoechoic
- •Irregular/Echogenic
- •Epididymal Lesion
- •Anechoic
- •Hypoechoic
- •Intrascrotal Mass
- •Anechoic or Hypoechoic
- •Echogenic
- •13 Female Genital Tract
- •Masses
- •Abnormalities of Size or Shape
- •Uterus
- •Abnormalities of Size or Shape
- •Myometrial Changes
- •Intracavitary Changes
- •Endometrial Changes
- •Fallopian Tubes
- •Hypoechoic Mass
- •Anechoic Cystic Mass
- •Solid Echogenic or Nonhomogeneous Mass
- •14 Thyroid Gland
- •Diffuse Changes
- •Enlarged Thyroid Gland
- •Small Thyroid Gland
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Circumscribed Changes
- •Anechoic
- •Hypoechoic
- •Isoechoic
- •Hyperechoic
- •Irregular
- •Differential Diagnosis of Hyperthyroidism
- •Types of Autonomy
- •15 Pleura and Chest Wall
- •Chest Wall
- •Masses
- •Parietal Pleura
- •Nodular Masses
- •Diffuse Pleural Thickening
- •Pleural Effusion
- •Anechoic Effusion
- •Echogenic Effusion
- •Complex Effusion
- •16 Lung
- •Masses
- •Anechoic Masses
- •Hypoechoic Masses
- •Complex Masses
- •Index
3
Biliary Tree and Gallbladder
Topography 





















































Landmark structures
●In the paramedian view: porta hepatis and the edge of the right hepatic lobe
●In the subcostal oblique view: interlobar fissure
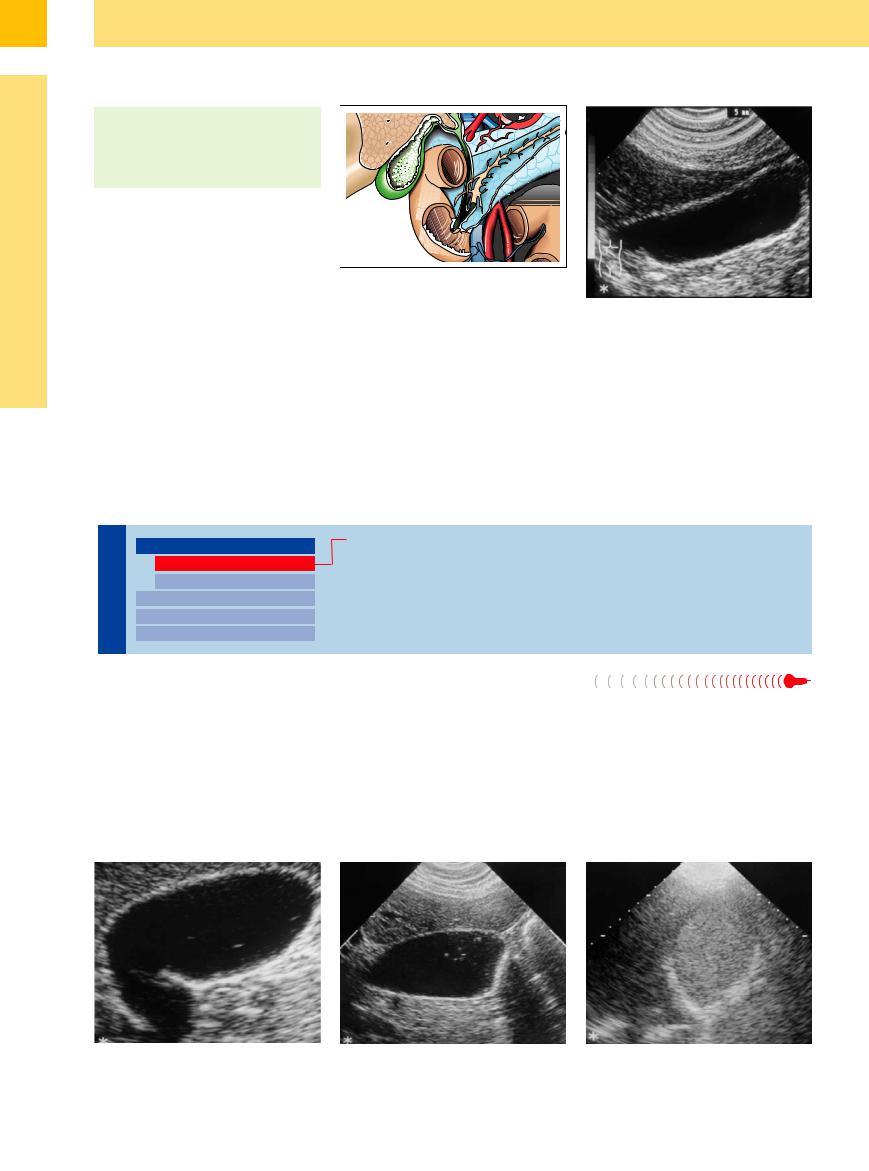
When looking for the gallbladder, useful landmarks are the porta hepatis and the edge of the right hepatic lobe (paramedian view) (Fig. 3.34, Fig. 3.35). During deep inspiration the gallbladder may easily be demonstrated anterior to the vena cava (the probe being tilted somewhat to the median plane). In the subcostal oblique view the landmark structure to be used is the interlobar fissure, which can be visualized in almost all patients; the gallbladder will be found by aligning the probe with the fissure and then tilting it caudad. The gallbladder will be located inferior or lateral to the fissure (between liver segments IV and V).
Fig. 3.34 Schematic illustration of the relationship between the gallbladder and its adjacent organs.
If the liver is small and the gallbladder is situated deep in the liver, access via the lateral intercostal spaces may be the best way to demonstrate the gallbladder. The landmark struc-
Fig. 3.35 Gallbladder in a longitudinal scan direction.
ture to locate the gallbladder is the portal vein in the porta hepatis. The probe is tilted caudal.
■ Changes in Size
Large Gallbladder
|
|
|
Changes in Size |
|
Asymptomatic (Functional) |
|||
Gallbladder |
||||||||
|
|
Large Gallbladder |
|
Asymptomatic (Pathological) |
||||
|
|
|
|
|
|
|||
|
|
|
|
|
Small/Missing Gallbladder |
|
Symptomatic (Pathological) |
|
|
|
|
Wall Changes |
|
|
|||
|
|
|
|
|
||||
|
|
|
|
|
|
|||
|
|
|
|
Intraluminal Changes |
|
|
||
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|||
|
|
|
|
Nonvisualized Gallbladder |
|
|
||
|
|
|
|
|
|
|||
Asymptomatic (Functional)
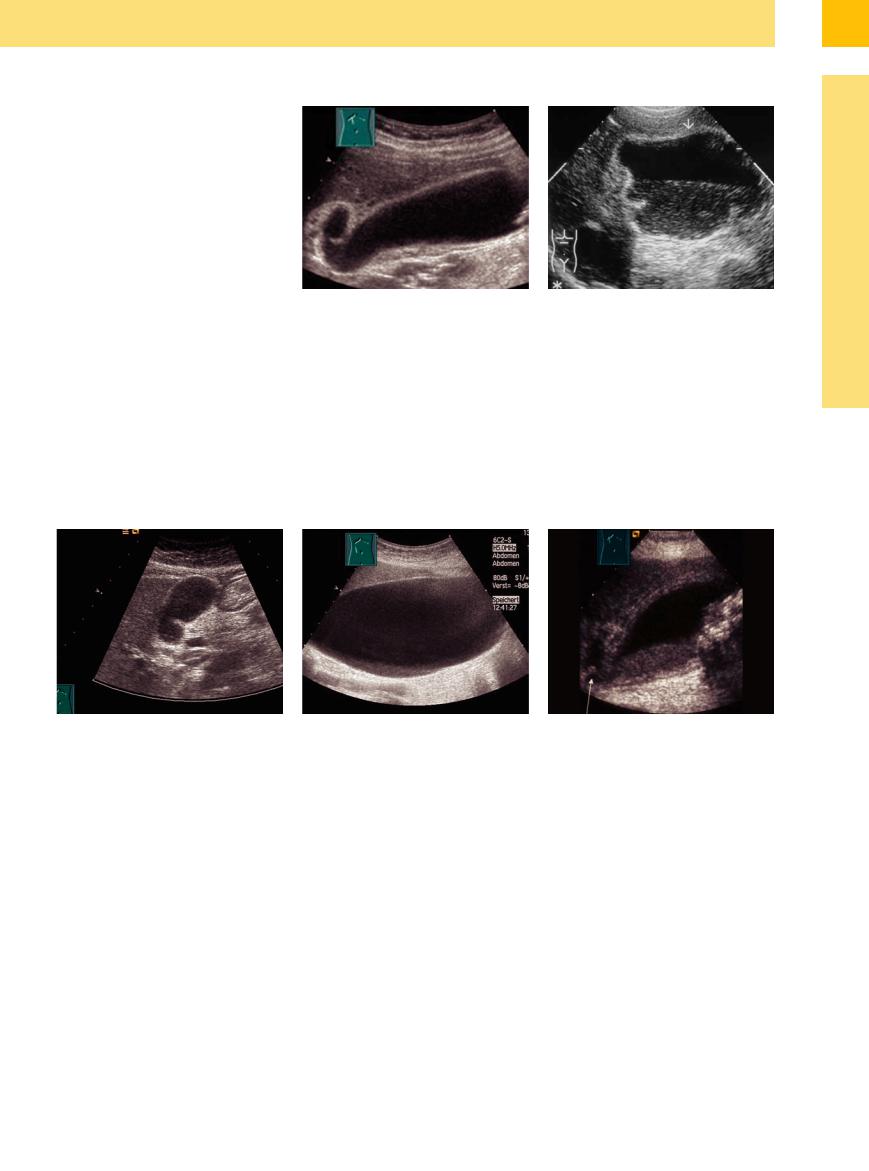
(Functional)






















A large (> 10 cm) flaccid gallbladder with normal wall (and a large volume of fluid) may be demonstrated as a variant in the asthenic patient or as an atonic sequel of long-term total parenteral nutrition (Fig. 3.36). Long periods of fasting may also result in a large, functionally flaccid gallbladder, not infrequently with intraluminal sludge (viscous bile or microliths) (Fig. 3.37a). Transient, and in case of permanent dysfunction of the gallbladder even per-
sistent, sludge formation may be demonstrated in patients with atonic/hypotonic gallbladder function after abdominal surgery as well as in abdominal disorders accompanied by various organ dysfunctions (e. g., gastrointestinal tract infection, hepatitis, pancreatitis, peritonitis, ileus). Metabolic disorders with abdominal manifestation (e. g., diabetes mellitus, polyneuropathy) may also effect large atonic gallbladders with or without sludge (Fig. 3.37b). In
contrast to inflammatory gallbladder disease, here the gallbladder does not exhibit any tenderness on palpation (negative ultrasonic Murphy’s sign), and on ultrasound the wall appears normal. Another important criterion for differentiation from cholecystitis is the lack of tense gallbladder distension (hydrops). Cholecystomegaly can be an indication of acromegaly.
Fig. 3.36 Large flaccid gallbladder (congenital variant). |
Fig. 3.37 Flaccid gallbladder. |
b Flaccid gallbladder in diabetes mellitus with concurrent |
Characteristic: normal wall and texture, anechoic intra- |
a After parenteral nutrition: normal wall, possibly intra- |
polyneuropathy. Nonfunctional gallbladder filled with |
luminal material. |
luminal sludge. |
sludge (“hepatized gallbladder”). |
148
Asymptomatic (Pathological)
(Pathological)












































The large but still functional gallbladder has to be differentiated from the large pathological specimen. Gallbladder size alone is insufficient to differentiate between dysfunction and pathological outflow obstruction. One such classic criterion in this differential diagnosis is the tense distension of the gallbladder, or hydrops. The nature of the outflow obstruction (obstruction of the cystic duct due to, e. g., calculus or tumor of the cystic duct, CBD, or pancreas) with enlarged palpable hydropic gallbladder (Courvoisier’s sign) can be differentiated by subtle ultrasound study (Fig. 3.38, Fig. 3.39). For optimum visualization of the cystic duct the patient should be supine, while the proximal CBD is best demonstrated in the left lateral decubitus position.
Fig. 3.38 Hydropic gallbladder (with dependent sedimentation in cystic duct obstruction. Gallbladder wall normal.
Symptomatic (Pathological) 












































Symptomatic hydrops of the gallbladder is one |
duct obstruction, the concurrent cholecystitis |
of the main criteria in cystic duct obstruction |
may not be manifest (Fig. 3.40). However, the |
due to gallstones and is characterized by a |
classic case does exhibit the combination of |
tensely distended gallbladder tender on palpa- |
cholecystolithiasis and cholecystitis (Fig. 3.41). |
tion. In the early phase of acute calculous cystic |
The sonographic Murphy’s sign (gallbladder |
Fig. 3.39 Gallbladder hydrops associated with a tumor of the cystic duct/common bile duct. The Courvoisier’s sign is typical: palpable, tense, nontender gallbladder.
tender on palpation under ultrasonic guidance during inspiration) is quite characteristic. After oral intake the gallbladder does not contract.
3
Changes in Size
Fig. 3.40 Hydropic gallbladder without cholecystitis in calculous obstruction of the cystic duct/CBD.
a Gallbladder hydrops with increased echogenicity: empyema, no wall thickening.
b Gallbladder hydrops caused by choledocholithiasis; normal gallbladder wall, gallbladder tensely distended, round, tender on palpation, sludge on the bottom.
Fig. 3.41 Hydropic gallbladder with cholecystitis (laminated wall) in cholecystolithiasis/cholangiolithiasis. Typical sonographic Murphy’s sign: distended gallbladder tender on ultrasound-guided palpation. Detection of sedimentation and stones.
149
3
Biliary Tree and Gallbladder
Small/Missing Gallbladder
|
|
|
Changes in Size |
|
|
Asymptomatic (Functional) |
|||
Gallbladder |
|||||||||
|
|
Large Gallbladder |
|
|
Asymptomatic (Pathological) |
||||
|
|
|
|
|
|
|
|||
|
|
|
|
|
Small/Missing Gallbladder |
|
|
Symptomatic (Pathological) |
|
|
|
|
|
|
|
||||
|
|
|
Wall Changes |
|
|
|
|||
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|||
|
|
|
|
Intraluminal Changes |
|
|
|
||
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
||
|
|
|
|
Nonvisualized Gallbladder |
|
|
|
||
|
|
|
|
|
|
|
|||
Asymptomatic (Functional)
(Functional)













































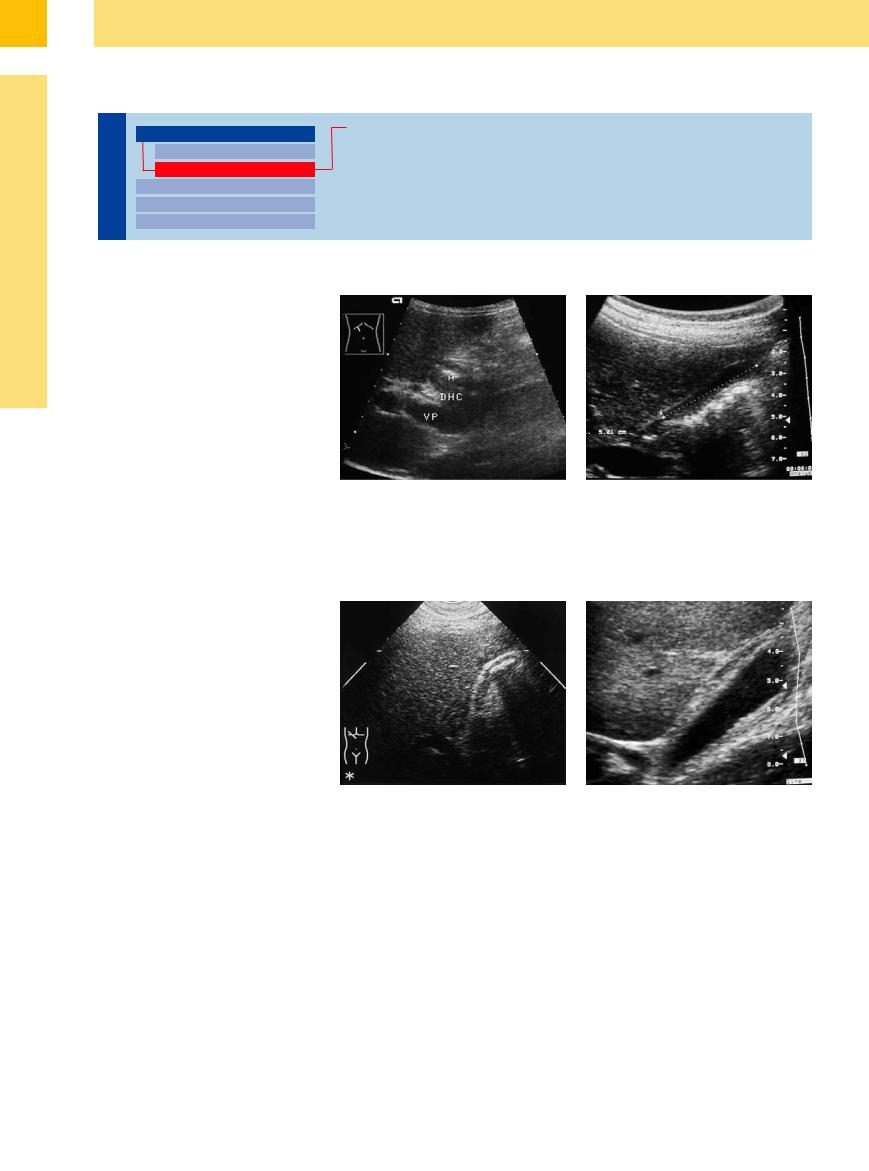
Agenesis of the gallbladder is an extremely rare finding (<0.1%) (Fig. 3.42a). Congenital hypoplasia of the gallbladder is also rather rare. If agenesis of the gallbladder is suspected, one should assiduously look for a dystopic gallbladder (e. g., an atypical intrahepatic gallbladder or one hyperextending all the way into the minor pelvis). A completely empty postprandial (or intrahepatic gallbladder) may also be quite hard to visualize (see “Nonvisualized Gallbladder,” p. 163). A gallbladder completely void of fluid is characterized by homogeneous triplelayering of the wall (Fig. 3.42b).
Fig. 3.42 a Agenesis of the gallbladder. Previous ultra- |
b Postprandial gallbladder with minimum fluid. After oral |
sound and CT studies diagnosed an atrophic gallblad- |
intake the gallbladder may be void of any fluid. This state |
der; surgery demonstrated agenesis of the gallbladder. |
is characterized by a smooth wall echo with homogene- |
A = antrum, DHC = common bile duct, VP = portal vein. |
ous triple-layered foldover. |
Asymptomatic (Pathological)
(Pathological)












































The postprandial contracted gallbladder should be differentiated from the asymptomatic cystic duct obstruction with a gallbladder persistently void of any fluid (Fig. 3.43).
Gallbladders with low fluid levels and concurrent wall edema are found in severe nonbiliary disorders (Table 3.1). They are characterized by a diffuse swelling in the wall, sometimes more pronounced in the fundus, which is hypoechoic or mixed hypoechoic and hyperechoic, and cleanly demarcated from the lumen as well as the exterior. If these criteria are demonstrated, the ultrasound study should concentrate on the underlying disease; typical examples are cirrhosis of the liver, right-sided heart failure, acute hepatitis, or severe renal failure. Severe hepatic dysfunction with insufficient bile secretion (e. g., in cirrhosis) may decrease the filling volume of the gallbladder and result in wall edema due to hypoalbuminemia (Fig. 3.44). Inflammatory lymph nodes along the hepatoduodenal ligament are fre-
Fig. 3.43 Gallbladder void of liquid in CBD obstruction. Gallbladder appears permanently contracted irrespective of food intake.
quent findings in acute chronic hepatitis. Hypoechoic increases in the wall thickness accompanied by loss of fluid are characteristic of severe hypoalbuminemia in renal failure or
Fig. 3.44 Gallbladder with little fluid and edema of the wall in cirrhosis of the liver with dysproteinemia. In nonbiliary disorders the hypoechoic increase in wall thickness with decreased fluid level is a typical phenomenon.
intestinal protein loss as well as for massive chronic cardiac congestion. In these cases hepatomegaly is another regular finding.
150
