
- •Contents
- •Preface
- •Contributors
- •1 Vessels
- •1.1 Aorta, Vena Cava, and Peripheral Vessels
- •Aorta, Arteries
- •Anomalies and Variant Positions
- •Dilatation
- •Stenosis
- •Wall Thickening
- •Intraluminal Mass
- •Perivascular Mass
- •Vena Cava, Veins
- •Anomalies
- •Dilatation
- •Intraluminal Mass
- •Compression, Infiltration
- •1.2 Portal Vein and Its Tributaries
- •Enlarged Lumen Diameter
- •Portal Hypertension
- •Intraluminal Mass
- •Thrombosis
- •Tumor
- •2 Liver
- •Enlarged Liver
- •Small Liver
- •Homogeneous Hypoechoic Texture
- •Homogeneous Hyperechoic Texture
- •Regionally Inhomogeneous Texture
- •Diffuse Inhomogeneous Texture
- •Anechoic Masses
- •Hypoechoic Masses
- •Isoechoic Masses
- •Hyperechoic Masses
- •Echogenic Masses
- •Irregular Masses
- •Differential Diagnosis of Focal Lesions
- •Diagnostic Methods
- •Suspected Diagnosis
- •3 Biliary Tree and Gallbladder
- •3.1 Biliary Tree
- •Thickening of the Bile Duct Wall
- •Localized and Diffuse
- •Bile Duct Rarefaction
- •Localized and Diffuse
- •Bile Duct Dilatation and Intraductal Pressure
- •Intrahepatic
- •Hilar and Prepancreatic
- •Intrapancreatic
- •Papillary
- •Abnormal Intraluminal Bile Duct Findings
- •Foreign Body
- •The Seven Most Important Questions
- •3.2 Gallbladder
- •Changes in Size
- •Large Gallbladder
- •Small/Missing Gallbladder
- •Wall Changes
- •General Hypoechogenicity
- •General Hyperechogenicity
- •General Tumor
- •Focal Tumor
- •Intraluminal Changes
- •Hyperechoic
- •Hypoechoic
- •Nonvisualized Gallbladder
- •Missing Gallbladder
- •Obscured Gallbladder
- •4 Pancreas
- •Diffuse Pancreatic Change
- •Large Pancreas
- •Small Pancreas
- •Hypoechoic Texture
- •Hyperechoic Texture
- •Focal Changes
- •Anechoic Lesion
- •Hypoechoic Lesion
- •Isoechoic Lesion
- •Hyperechoic Lesion
- •Irregular (Complex Structured) Lesion
- •Dilatation of the Pancreatic Duct
- •Marginal/Mild Dilatation
- •Marked Dilatation
- •5 Spleen
- •Nonfocal Changes of the Spleen
- •Diffuse Parenchymal Changes
- •Large Spleen
- •Small Spleen
- •Focal Changes of the Spleen
- •Anechoic Mass
- •Hypoechoic Mass
- •Hyperechoic Mass
- •Splenic Calcification
- •6 Lymph Nodes
- •Peripheral Lymph Nodes
- •Head/Neck
- •Extremities (Axilla, Groin)
- •Abdominal Lymph Nodes
- •Porta Hepatis
- •Splenic Hilum
- •Mesentery (Celiac, Upper and Lower Mesenteric Station)
- •Stomach
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •Small/Large Intestine
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •8 Peritoneal Cavity
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Wall Structures
- •Smooth Margin
- •Irregular Margin
- •Intragastric Processes
- •Intraintestinal Processes
- •9 Kidneys
- •Anomalies, Malformations
- •Aplasia, Hypoplasia
- •Cystic Malformation
- •Anomalies of Number, Position, or Rotation
- •Fusion Anomaly
- •Anomalies of the Renal Calices
- •Vascular Anomaly
- •Diffuse Changes
- •Large Kidneys
- •Small Kidneys
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Irregular Structure
- •Circumscribed Changes
- •Anechoic Structure
- •Hypoechoic or Isoechoic Structure
- •Complex Structure
- •Hyperechoic Structure
- •10 Adrenal Glands
- •Enlargement
- •Anechoic Structure
- •Hypoechoic Structure
- •Complex Echo Structure
- •Hyperechoic Structure
- •11 Urinary Tract
- •Malformations
- •Duplication Anomalies
- •Dilatations and Stenoses
- •Dilated Renal Pelvis and Ureter
- •Anechoic
- •Hypoechoic
- •Hypoechoic
- •Hyperechoic
- •Large Bladder
- •Small Bladder
- •Altered Bladder Shape
- •Intracavitary Mass
- •Hypoechoic
- •Hyperechoic
- •Echogenic
- •Wall Changes
- •Diffuse Wall Thickening
- •Circumscribed Wall Thickening
- •Concavities and Convexities
- •12.1 The Prostate
- •Enlarged Prostate
- •Regular
- •Irregular
- •Small Prostate
- •Regular
- •Echogenic
- •Circumscribed Lesion
- •Anechoic
- •Hypoechoic
- •Echogenic
- •12.2 Seminal Vesicles
- •Diffuse Change
- •Hypoechoic
- •Circumscribed Change
- •Anechoic
- •Echogenic
- •Irregular
- •12.3 Testis, Epididymis
- •Diffuse Change
- •Enlargement
- •Decreased Size
- •Circumscribed Lesion
- •Anechoic or Hypoechoic
- •Irregular/Echogenic
- •Epididymal Lesion
- •Anechoic
- •Hypoechoic
- •Intrascrotal Mass
- •Anechoic or Hypoechoic
- •Echogenic
- •13 Female Genital Tract
- •Masses
- •Abnormalities of Size or Shape
- •Uterus
- •Abnormalities of Size or Shape
- •Myometrial Changes
- •Intracavitary Changes
- •Endometrial Changes
- •Fallopian Tubes
- •Hypoechoic Mass
- •Anechoic Cystic Mass
- •Solid Echogenic or Nonhomogeneous Mass
- •14 Thyroid Gland
- •Diffuse Changes
- •Enlarged Thyroid Gland
- •Small Thyroid Gland
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Circumscribed Changes
- •Anechoic
- •Hypoechoic
- •Isoechoic
- •Hyperechoic
- •Irregular
- •Differential Diagnosis of Hyperthyroidism
- •Types of Autonomy
- •15 Pleura and Chest Wall
- •Chest Wall
- •Masses
- •Parietal Pleura
- •Nodular Masses
- •Diffuse Pleural Thickening
- •Pleural Effusion
- •Anechoic Effusion
- •Echogenic Effusion
- •Complex Effusion
- •16 Lung
- •Masses
- •Anechoic Masses
- •Hypoechoic Masses
- •Complex Masses
- •Index
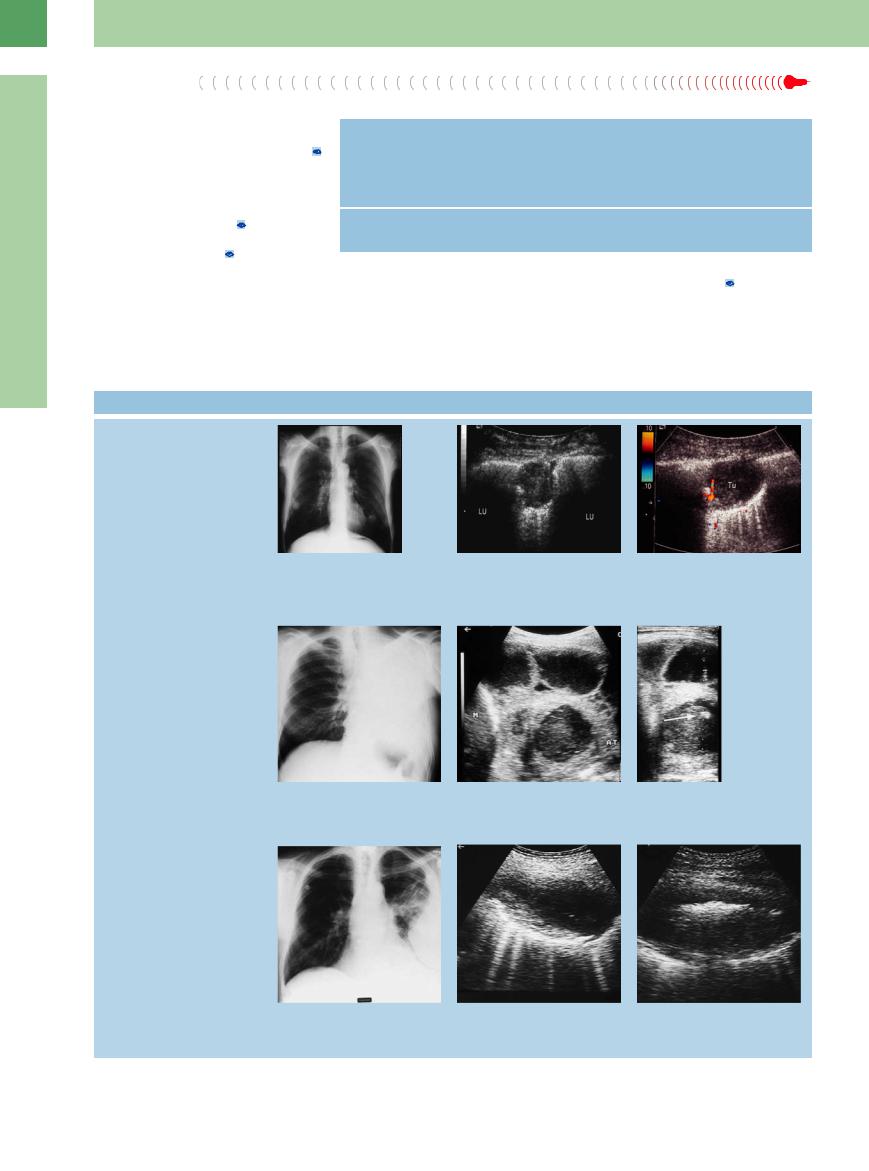
16
Lung
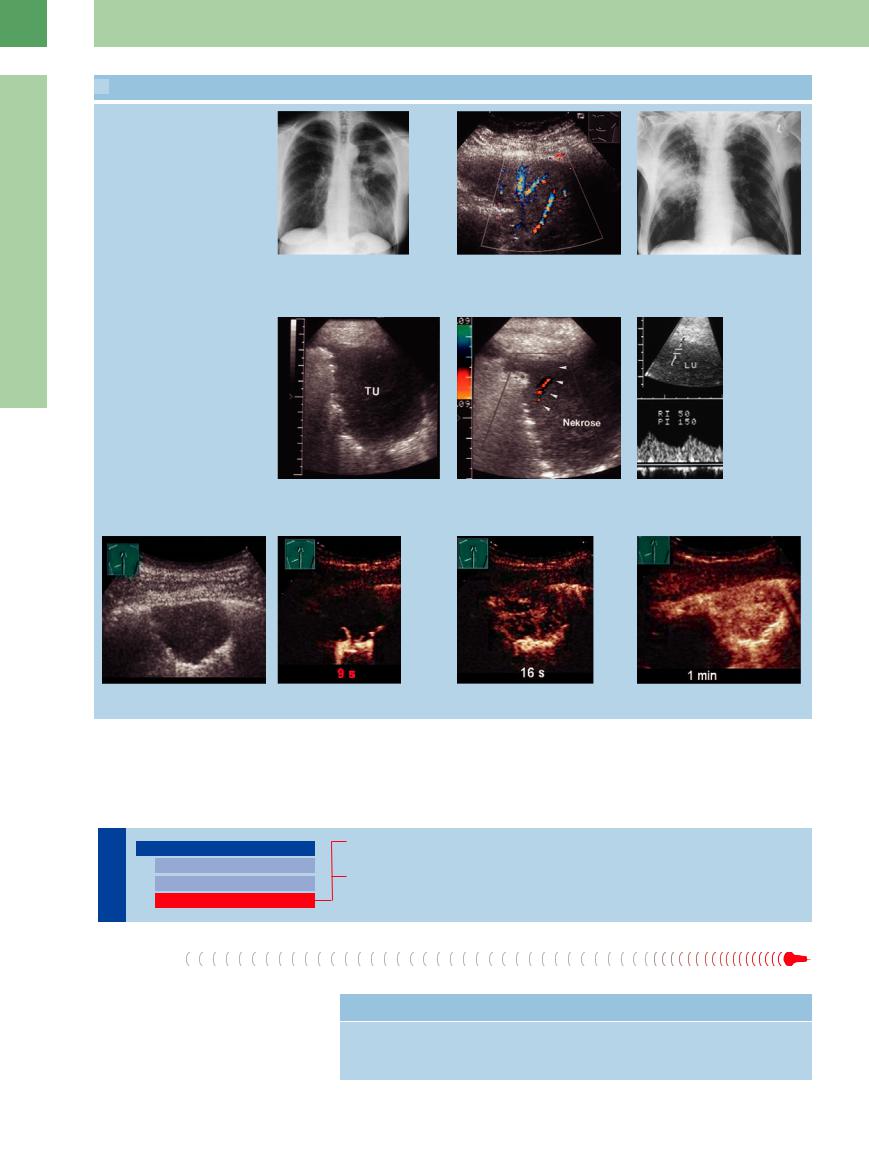
 16.6 Pulmonary Tumors and Metastases (Continued)
16.6 Pulmonary Tumors and Metastases (Continued)
Color Doppler findings in bronchoalveolar carcinoma
p and q Bronchoalveolar carcinoma in a 53-year-old woman.
p Chest radiograph shows di use shadowing in the left middle and upper zones.
High diastolic flow in color Doppler
q Homogeneous hypoechoic transformation of lung tissue. Color Doppler records prominent flow signals in the tumor.
r–u Bronchial carcinoma in a 77-year-old man.
r Chest radiograph shows di use shadowing in the right mid zone.
s–u Hypoechoic tumor mass (TU) in a right lateral intercostal scan. Color Doppler waveforms are recorded at the tumor periphery. The high diastolic flow (“parenchymal artery” pattern) is characteristic of tumor vessels. LU = lung.
Flow profile in color Doppler and CEUS
v–y Peripheral lung cancer in CEUS. The vascularization of the tumor begins after 8 s, indicating a bronchial arterial vascularization. The diagnosis of a bronchial carcinoma was made by punch biopsy.
Complex Masses
Lung |
Masses |
|||
|
|
|
||
|
|
|
|
Anechoic Masses |
|
|
|
|
Hypoechoic Masses |
|
|
|
|
Complex Masses |
|
|
|
|
|
Pneumonia
Lung Abscess
Pneumonia
Ultrasound is of limited value in the diagnosis of pneumonia ( 16.7). It can show a more or less pronounced replacement of alveolar air, depending on the degree of pneumonic changes (
16.7). It can show a more or less pronounced replacement of alveolar air, depending on the degree of pneumonic changes ( 16.7a–c). But the majority of inflammatory lung changes (especially central and interstitial) cannot be visualized with ul-
16.7a–c). But the majority of inflammatory lung changes (especially central and interstitial) cannot be visualized with ul-
Table 16.5 Differential diagnosis of complex masses
Common |
Less common |
Pneumonia |
Liquefying tumor |
Lung abscess |
Liquefying atelectasis |
|
Compression atelectasis |
546
trasound ( 16.7 d–f). Table 16.6 reviews the sonographic findings that may be seen in pneumonia.
16.7 d–f). Table 16.6 reviews the sonographic findings that may be seen in pneumonia.
Lobar pneumonia. True lobar pneumonia produces a homogeneous, hypoechoic structural transformation in its early stage. The echo texture of affected lung resembles that of the liver ( 16.7 g,h). Color Doppler shows increased vascular color-flow signals in the infiltrated lung area (
16.7 g,h). Color Doppler shows increased vascular color-flow signals in the infiltrated lung area ( 16.8c). Lobar pneumonia often shows a bronchial arterial vascularization in CEUS (
16.8c). Lobar pneumonia often shows a bronchial arterial vascularization in CEUS ( 16.8 m).
16.8 m).
Aerated bronchi may appear as prominent echogenic bands, similar to the bronchogram seen on radiographs ( 16.7j,k). They may have a branched, string-of-beads appearance or may present as focal echogenic zones with irregular margins. The consolidated areas are usually irregular but may show segmental boundaries. The healing stage is marked by
16.7j,k). They may have a branched, string-of-beads appearance or may present as focal echogenic zones with irregular margins. The consolidated areas are usually irregular but may show segmental boundaries. The healing stage is marked by
Table 16.6 Possible sonographic findings in pneumonia
B-mode ultrasound
●Frequent hypoechoic transformation of lung tissue
●Tends to be poorly demarcated from aerated lung
●Frequent positive air bronchogram
●Aeration often increases during inspiration
●Possible concomitant e usion
Color Doppler ultrasound
●Increased color flow in relation to the liver
●Triphasic Doppler spectrum of pulmonary artery waveforms (“extremity artery” pattern)
re-aeration with an increase in echogenicity. |
Ultrasound is not a substitute for chest ra- |
Concomitant effusion is often present. The |
diography in pneumonia, but it is helpful as a |
complication of cavitating pneumonia usually |
follow-up study in detecting complications, re- |
appears as a hypoechoic to anechoic area |
ducing radiation exposure, and advancing the |
within the consolidated lung ( 16.8). |
differential diagnosis (Table 16.5).8 |
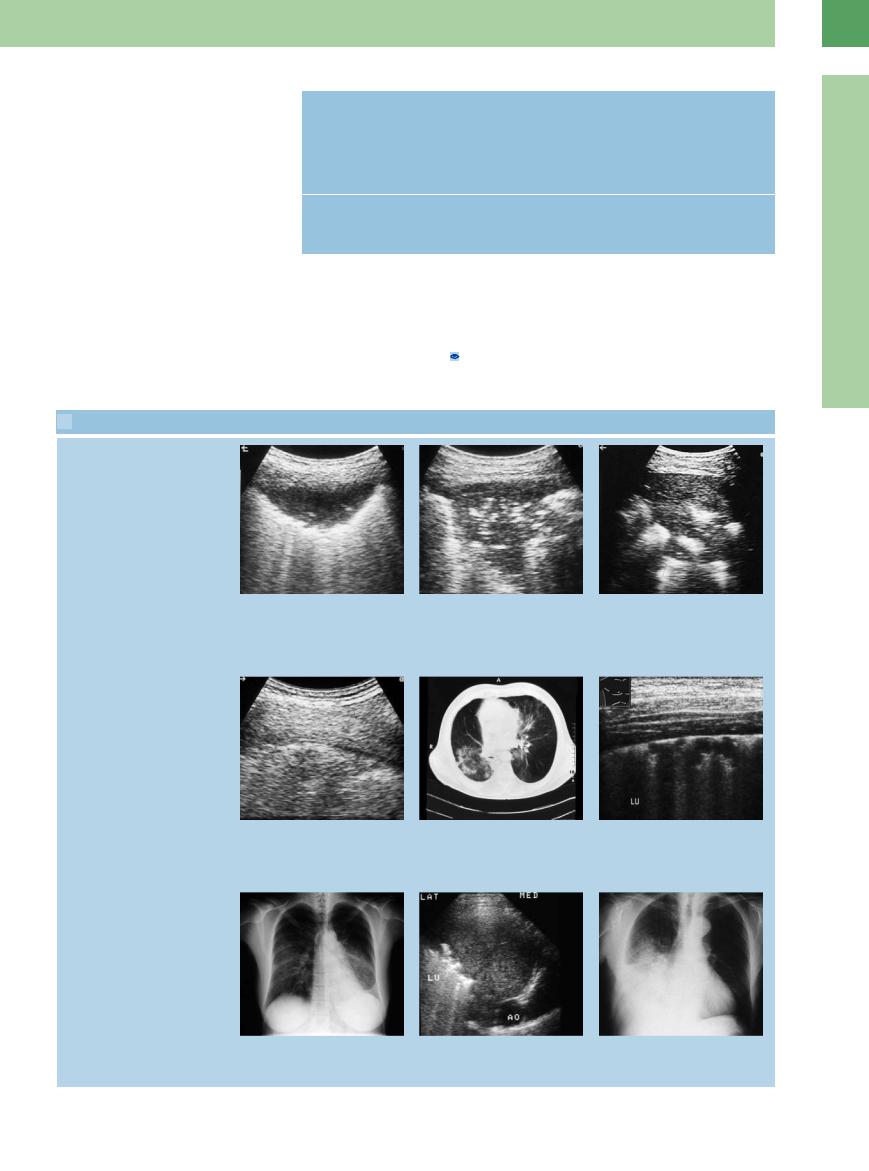
 16.7 Interstitial and Lobar Pneumonia
16.7 Interstitial and Lobar Pneumonia
Lobar pneumonia: air bronchogram
16
Masses
a–c Types of air bronchogram that may be seen in pneumonia. The pattern of air echoes depends partly on the course of the pneumonia.
a Di use air bronchogram. LU = lung; S = spleen.
Interstitial pneumonia
d–f Bronchial carcinoma and interstitial pneumonia in a 60-year-old man.
d The pleural line is fragmented, with partial sound transmission in the lung tissue.
Lobar pneumonia
g and h Early form of lobar pneumonia.
g Chest radiograph shows opacity in the lower left lung field.
b Branched air bronchogram.
e CT: interstitial pneumonia.
h Left posterior intercostal scan shows a largely homogeneous hypoechoic transformation of lung tissue.
c Patchy air bronchogram.
f Interstitial pneumonia in a 20-year-old woman. Ultrasound shows slight disruption of the pleural line; partial sound transmission in the lung tissue.
i–o Pneumonia in a 73-year-old man.
i Chest radiograph shows opacity in the lower right lung field.
547
16
Lung
 16.7 Interstitial and Lobar Pneumonia (Continued)
16.7 Interstitial and Lobar Pneumonia (Continued)
j and k Hypoechoic transformation of lung tissue. A branched air bronchogram is seen |
l Color Doppler image defines the course |
in the magnified view. |
of blood vessels along the bronchial |
|
system. LA = lung artery; LV = lung vein; |
|
BR = air bronchogram. |
Pulmonary artery and pulmonary vein
m–o The pulmonary artery (n) and pulmonary vein (o) can be identified by their color-flow image and spectral waveforms.
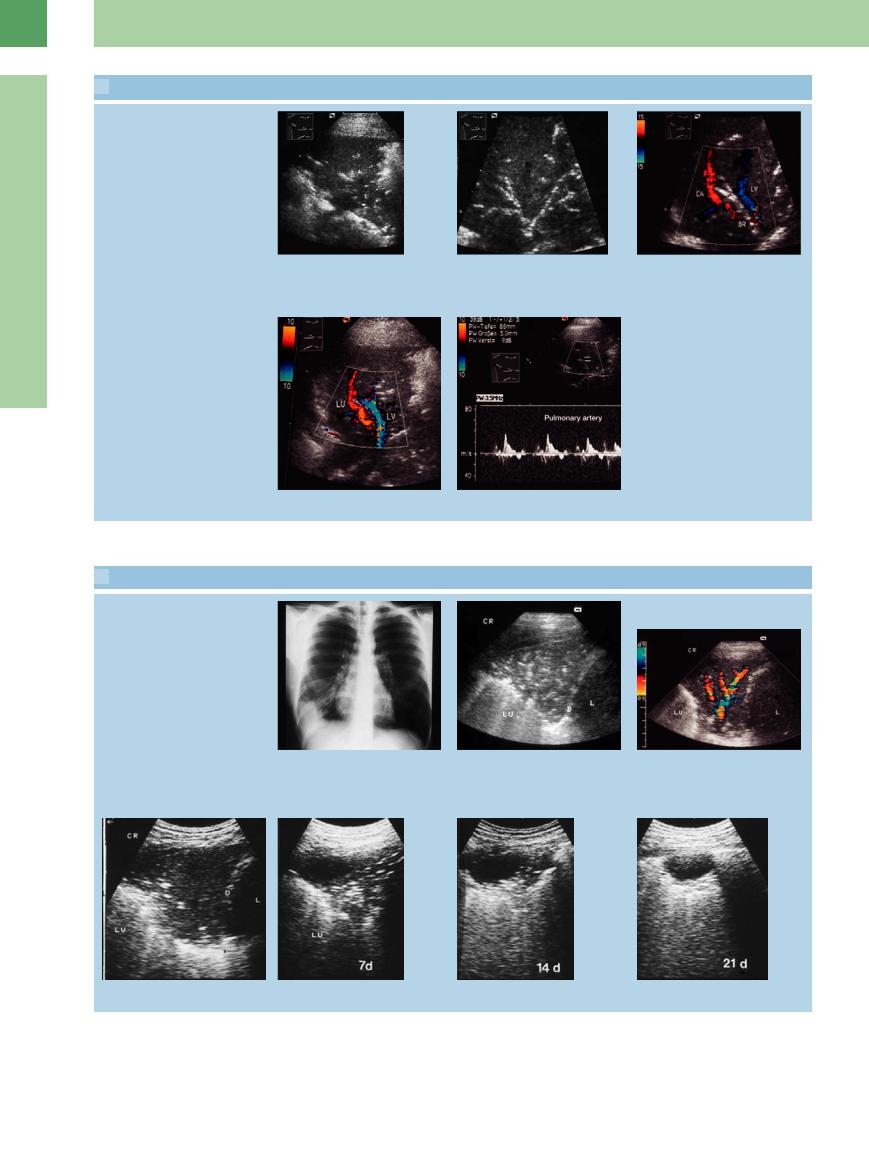
 16.8 Complications of Pneumonia
16.8 Complications of Pneumonia
Lobar pneumonia with liquefied interior over time
a–g Pneumonia in a 31-year-old man.
a Chest radiograph shows di use shadowing in the area of the right costophrenic angle.
b Right lateral intercostal scan shows a small e usion and a triangular area of hypoechoic lung tissue. A subtle, speckled air bronchogram is present.
c Prominent flow signals are observed with color Doppler.
d–g Serial scans document progressive aeration over a 3-week period. A small fluid collection persisted as a complication (still visible at 21 days).
548
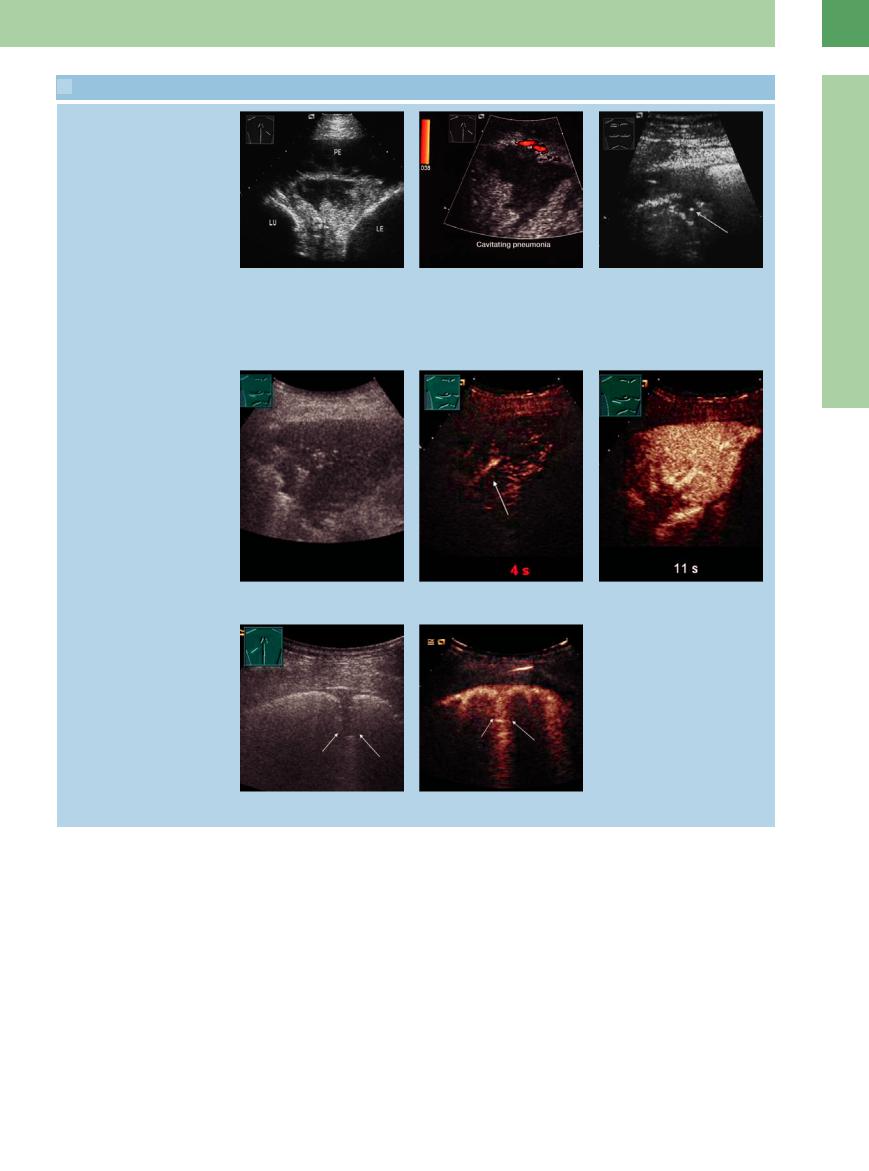
 16.8 Complications of Pneumonia (Continued)
16.8 Complications of Pneumonia (Continued)
Pneumonia with liquefaction
h and i Pneumonia in a 72-year-old man.
h Pleural e usion (PE) and a wedgeshaped area of complex lung transformation. LE = liver; LU = lung.
CEUS
i Color Doppler shows peripheral flow signals. The central echo-free structure is an area of cavitating pneumonia.
j Open pulmonary tuberculosis in a 60- year-old man. Ultrasound scans show hypoechoic transformation of peripheral lung tissue. The echo-free round lesion with a central air echo in the lung parenchyma (arrow) is caused by liquefaction.
16
Masses
k–m Pneumonia in CEUS. The homogenous enhancement of the pneumonia begins after 4 s, indicating a pulmonary arterial vascularization.
n and o Pleurisy in CEUS. The pleurisy caused by inflammation shows a distinct enhancement.
Pleuropneumonia, pleurisy. There is a continuum between pleuropneumonia and pleurisy. The latter appears sonographically as a break in the sharp pleural line, usually combined with pleural effusion. The parenchymal defects that
can be defined with ultrasound are often less than 1 cm in size and cannot be detected radiographically in the absence of pleural effusion.
Pleurisy caused by inflammation shows a bronchial arterial vascularization in CEUS,
which is not common in pleurisy caused by infarctions ( 16.8n).
16.8n).
When combined with physical examination, ultrasonography is the method of choice in the diagnosis of pleurisy.
549
16
Lung
Table 16.7 Possible sonographic findings in lung abscess/empyema
B-mode ultrasound
● Complex transformation of lung tissue
●Sharp limitation to the ventilated pulmonary parenchyma
●Echogenic margins of the mass
●Possible detection of intralesional gas and movable echoes (liquefaction)
Color Doppler ultrasound
● Lack of flow signals
the mass. This creates a more or less conspic- |
Ultrasound-guided FNA is useful for con- |
a fine needle5 (viscous contents). |
uous hyperechoic boundary consisting of the |
firming the diagnosis, sampling material, and |
|
 16.9 Lung Abscess
16.9 Lung Abscess
Lobar pneumonia with liquefied interior over time
a–c Septic lung abscesses in a 54-year-old man.
a Chest radiograph shows multiple pulmonary nodules.
|
d–f Patient with bronchial carcinoma and |
|
septic temperatures. |
|
d Chest radiograph shows di use opacifi- |
Lobar pneumonia with liquefaction |
cation of the left lung. |
|
g–i Di erential diagnosis: pleural empyema.
g Chest radiograph shows a large opacity bordering the chest wall on the left side.
b Ultrasound shows a homogeneous hypoechoic peripheral lung mass (LU).
e Loculated pleural e usion and complete lower lobe atelectasis (AT) with a central hypoechoic area of retained fluid. M = spleen.
h Scan at a higher level shows bright air echoes in the upper part of the mass.
c Color Doppler shows flow signals only at the periphery of the mass (Tu). An abscess was diagnosed by ultrasoundguided core biopsy (which yielded streptococci).
f Diagnostic needle aspiration yielded purulent fluid consistent with a lung abscess. The arrow indicates the needle tip echo.
i The lower part of the lesion contains echogenic material. The margins of the lesion are relatively smooth.
550

 16.9 Lung Abscess (Continued)
16.9 Lung Abscess (Continued)
j–l Sepsis and peripheral lung lesion in CEUS. The lesions shows an early arterial (pulmonary arterial) enhancement, while the more central lesions do not accumulate contrast agent, indicating that they are caused by septic embolisms.
m–o Patient with acute myeloid leukemia (AML) and chronic pneumonia in CEUS. The lesion shows a peripheral enhancement, while the central parts do not accumulate contrast agent, indicating nonvital tissue. A punch biopsy of the central parts confirmed the diagnosis of necrotic tissue.
Tips, tricks, and pitfalls
Most helpful and easily answered are questions for pneumonia, embolism, and pneumothorax in patients who are confined to bed or on artificial respiration:
●Pneumonia
–investigation of the dorsobasal parts
–look for sound transmission
References
[1]Mathis G. Lungenund Pleurasonographie. 2nd ed. Berlin: Springer, 1996
[2]Görg C, Schwerk WB. Pleura und Lunge, Teil 1. In: Braun G, Schwerk WB (Hrsg.). Ultraschalldiagnostik. Landsberg: ECO-Med, 2006, 33. Erg.Lfg. III 2.2., pp.1–72
[3]Görg C, Schwerk WB. Pleura und Lunge, Teil 2. In: Braun G, Schwerk WB (Hrsg.). Ultraschalldiagnostik. Landsberg: ECO-Med, 2007, 34. Erg.Lfg. III 2.2., pp. 72–188
–look for aerobronchogram
–look for (small) effusions
●Subpleural areas of infarction
–look for pleural bands of enhanced reflectivity for embolism (easily done)
–also look for sources of embolism (popliteal and femoral veins)
[4]Yang PC. Color Doppler ultrasound of pulmonary consolidation. Eur J Ultrasound 1996; 3:169–178
[5]Blank W. Sonographisch gesteuerte Punktionen und Drainagen. In: Braun G, Schwerk WB (eds.). Ultraschalldiagnostik. Landsberg: ECO-Med, 1994, III.II., pp. 5–12
[6]Kroschel U, Seitz K, Reuss J, Rettenmaier G. Sonographische Darstellung von Lungenmbolien. Ergebnisse einer prospektiven Studie [Sonographic imaging of lung emboli. Results of a prospective study]. Ultraschall Med 1991;12(6):263–268
●Pneumothorax
–lack of visualized pleural band reflexes and/or of pulmonary entrance echoes
–no sign of pleural reflectibility
–lack of comet-tail artifacts, and of colored moving artifacts (in B- or in M-mode)
[7]Mathis G, Dirschmid K. Pulmonary infarction: sonographic appearance with pathologic correlation. Eur J Radiol 1993;17(3):170–174
[8]Gehmacher O. Ultrasound pictures of pneumonia. Eur J Ultrasound 1996;3:161–167
[9]Görg C, Bert T, Kring R, Dempfle A. Transcutaneous contrast enhanced sonography of the chest for evaluation of pleural based pulmonary lesions: experience in 137 patients. Ultraschall Med 2006;27(5):437–444
16
Masses
551

