
- •Contents
- •Preface
- •Contributors
- •1 Vessels
- •1.1 Aorta, Vena Cava, and Peripheral Vessels
- •Aorta, Arteries
- •Anomalies and Variant Positions
- •Dilatation
- •Stenosis
- •Wall Thickening
- •Intraluminal Mass
- •Perivascular Mass
- •Vena Cava, Veins
- •Anomalies
- •Dilatation
- •Intraluminal Mass
- •Compression, Infiltration
- •1.2 Portal Vein and Its Tributaries
- •Enlarged Lumen Diameter
- •Portal Hypertension
- •Intraluminal Mass
- •Thrombosis
- •Tumor
- •2 Liver
- •Enlarged Liver
- •Small Liver
- •Homogeneous Hypoechoic Texture
- •Homogeneous Hyperechoic Texture
- •Regionally Inhomogeneous Texture
- •Diffuse Inhomogeneous Texture
- •Anechoic Masses
- •Hypoechoic Masses
- •Isoechoic Masses
- •Hyperechoic Masses
- •Echogenic Masses
- •Irregular Masses
- •Differential Diagnosis of Focal Lesions
- •Diagnostic Methods
- •Suspected Diagnosis
- •3 Biliary Tree and Gallbladder
- •3.1 Biliary Tree
- •Thickening of the Bile Duct Wall
- •Localized and Diffuse
- •Bile Duct Rarefaction
- •Localized and Diffuse
- •Bile Duct Dilatation and Intraductal Pressure
- •Intrahepatic
- •Hilar and Prepancreatic
- •Intrapancreatic
- •Papillary
- •Abnormal Intraluminal Bile Duct Findings
- •Foreign Body
- •The Seven Most Important Questions
- •3.2 Gallbladder
- •Changes in Size
- •Large Gallbladder
- •Small/Missing Gallbladder
- •Wall Changes
- •General Hypoechogenicity
- •General Hyperechogenicity
- •General Tumor
- •Focal Tumor
- •Intraluminal Changes
- •Hyperechoic
- •Hypoechoic
- •Nonvisualized Gallbladder
- •Missing Gallbladder
- •Obscured Gallbladder
- •4 Pancreas
- •Diffuse Pancreatic Change
- •Large Pancreas
- •Small Pancreas
- •Hypoechoic Texture
- •Hyperechoic Texture
- •Focal Changes
- •Anechoic Lesion
- •Hypoechoic Lesion
- •Isoechoic Lesion
- •Hyperechoic Lesion
- •Irregular (Complex Structured) Lesion
- •Dilatation of the Pancreatic Duct
- •Marginal/Mild Dilatation
- •Marked Dilatation
- •5 Spleen
- •Nonfocal Changes of the Spleen
- •Diffuse Parenchymal Changes
- •Large Spleen
- •Small Spleen
- •Focal Changes of the Spleen
- •Anechoic Mass
- •Hypoechoic Mass
- •Hyperechoic Mass
- •Splenic Calcification
- •6 Lymph Nodes
- •Peripheral Lymph Nodes
- •Head/Neck
- •Extremities (Axilla, Groin)
- •Abdominal Lymph Nodes
- •Porta Hepatis
- •Splenic Hilum
- •Mesentery (Celiac, Upper and Lower Mesenteric Station)
- •Stomach
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •Small/Large Intestine
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •8 Peritoneal Cavity
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Wall Structures
- •Smooth Margin
- •Irregular Margin
- •Intragastric Processes
- •Intraintestinal Processes
- •9 Kidneys
- •Anomalies, Malformations
- •Aplasia, Hypoplasia
- •Cystic Malformation
- •Anomalies of Number, Position, or Rotation
- •Fusion Anomaly
- •Anomalies of the Renal Calices
- •Vascular Anomaly
- •Diffuse Changes
- •Large Kidneys
- •Small Kidneys
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Irregular Structure
- •Circumscribed Changes
- •Anechoic Structure
- •Hypoechoic or Isoechoic Structure
- •Complex Structure
- •Hyperechoic Structure
- •10 Adrenal Glands
- •Enlargement
- •Anechoic Structure
- •Hypoechoic Structure
- •Complex Echo Structure
- •Hyperechoic Structure
- •11 Urinary Tract
- •Malformations
- •Duplication Anomalies
- •Dilatations and Stenoses
- •Dilated Renal Pelvis and Ureter
- •Anechoic
- •Hypoechoic
- •Hypoechoic
- •Hyperechoic
- •Large Bladder
- •Small Bladder
- •Altered Bladder Shape
- •Intracavitary Mass
- •Hypoechoic
- •Hyperechoic
- •Echogenic
- •Wall Changes
- •Diffuse Wall Thickening
- •Circumscribed Wall Thickening
- •Concavities and Convexities
- •12.1 The Prostate
- •Enlarged Prostate
- •Regular
- •Irregular
- •Small Prostate
- •Regular
- •Echogenic
- •Circumscribed Lesion
- •Anechoic
- •Hypoechoic
- •Echogenic
- •12.2 Seminal Vesicles
- •Diffuse Change
- •Hypoechoic
- •Circumscribed Change
- •Anechoic
- •Echogenic
- •Irregular
- •12.3 Testis, Epididymis
- •Diffuse Change
- •Enlargement
- •Decreased Size
- •Circumscribed Lesion
- •Anechoic or Hypoechoic
- •Irregular/Echogenic
- •Epididymal Lesion
- •Anechoic
- •Hypoechoic
- •Intrascrotal Mass
- •Anechoic or Hypoechoic
- •Echogenic
- •13 Female Genital Tract
- •Masses
- •Abnormalities of Size or Shape
- •Uterus
- •Abnormalities of Size or Shape
- •Myometrial Changes
- •Intracavitary Changes
- •Endometrial Changes
- •Fallopian Tubes
- •Hypoechoic Mass
- •Anechoic Cystic Mass
- •Solid Echogenic or Nonhomogeneous Mass
- •14 Thyroid Gland
- •Diffuse Changes
- •Enlarged Thyroid Gland
- •Small Thyroid Gland
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Circumscribed Changes
- •Anechoic
- •Hypoechoic
- •Isoechoic
- •Hyperechoic
- •Irregular
- •Differential Diagnosis of Hyperthyroidism
- •Types of Autonomy
- •15 Pleura and Chest Wall
- •Chest Wall
- •Masses
- •Parietal Pleura
- •Nodular Masses
- •Diffuse Pleural Thickening
- •Pleural Effusion
- •Anechoic Effusion
- •Echogenic Effusion
- •Complex Effusion
- •16 Lung
- •Masses
- •Anechoic Masses
- •Hypoechoic Masses
- •Complex Masses
- •Index
3Biliary Tree and Gallbladder
3.1Biliary Tree
L. Greiner
The intrahepatic and extrahepatic bile ducts are delicate tubular structures without the stratified appearance so typical of smoothmuscle walls—the epithelium of the bile ducts lies directly adjacent to the outermost connective tissue layer. Any increase in pressure within the ducts results in immediate dilatation of those parts of the ducts (and possibly also of the gallbladder and/or cystic duct) up-
stream of the obstruction. This facet of dilatation may be detected quite easily by ultrasound and is the most important aspect in the differential diagnosis of (obstructive) cholestasis (with or without jaundice). The changes in wall thickness, intraluminal matter, and adjacent structures form the basis for the sonographic assessment of the level and cause (benign or malignant) of biliary obstruction.
Anatomy























































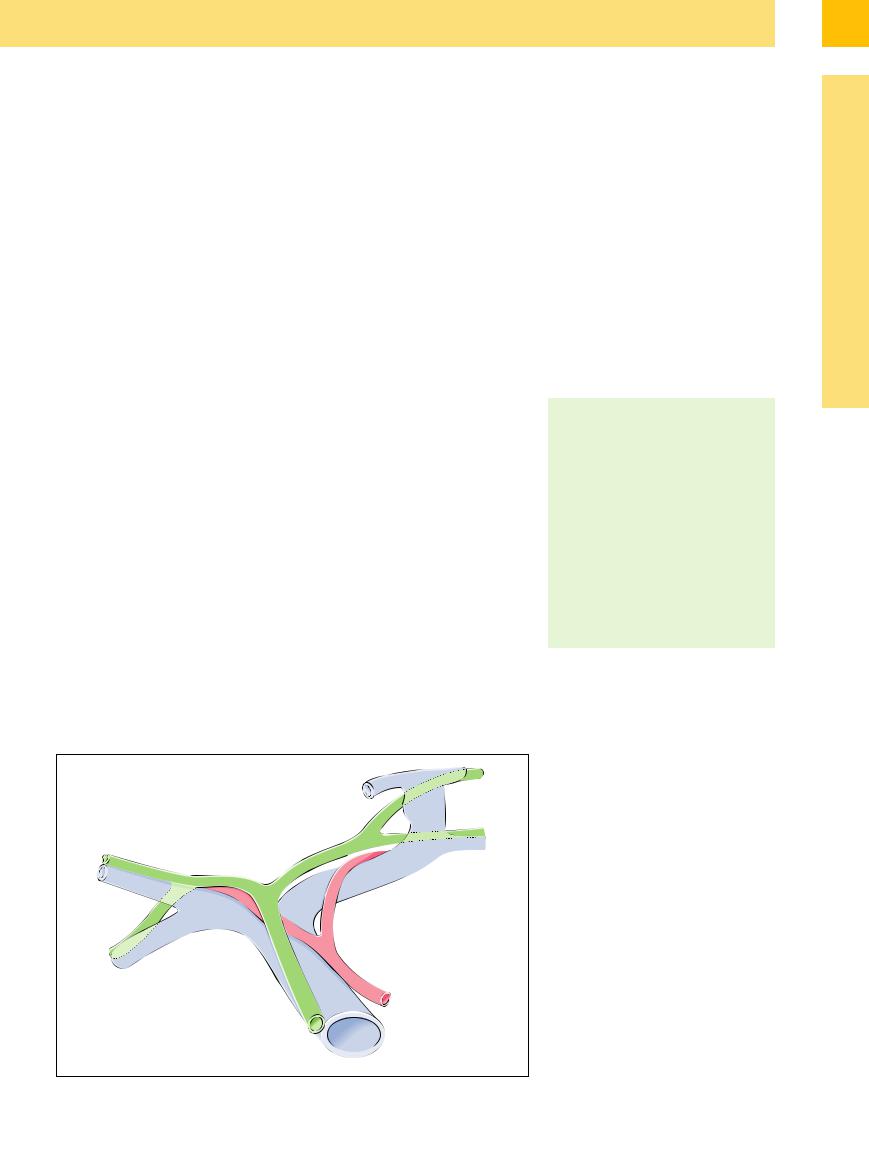
When viewed in the direction of bile flow, the anatomy of the biliary tree may be subdivided into an intrahepatic as well as an extrahepatic compartment (Fig. 3.1), the gallbladder appearing to be “just” a dilated dead end. The extrahepatic course of the bile ducts can be broken down further into the hilar, prepancreatic, and intrapancreatic segments (ultrasound cannot differentiate between a (rare) true intrapancreatic course and the duct running in a “groove”). Only in rare instances does another anatomical landmark become visible by sonography—the union of the cystic duct with the common hepatic duct. In ultrasound nomenclature this then becomes the common hepatic and hepatocystic ducts, i. e., the common bile duct (CBD).
Diameter. Differential diagnosis in the ultrasound of the biliary tree relies much more on the shape of the ducts than their “actual” or “identifiable” diameter, since the precise measurement of biological structures is character-
ized by numerous variables: the definition of the distances to be measured—which diameter at which organ/tubule border and at which position—is arbitrary and therefore not precise. In addition, this issue becomes even more complex when taking into account the typical changes seen in the extrahepatic biliary tree, where the diameter of the ducts increases with advancing age. Localized increases in the prepancreatic duct diameter without a concomitant rise in the intraductal pressure (“cholangiectasia”) do not depend on age and are a frequent finding (see Fig. 3.4). Careful studies have not been able to confirm the prevailing concept that the diameter of the common duct increases regularly after cholecystectomy; agerelated cholangiectasia is the main cause.
There are no systematic ultrasound studies correlating bile duct diameter and patient position, and neither have there been any studies on the (possible) changes in bile duct diameter after meals or pressure relief, e. g., by
To discern the level (intraor extrahepatic) as well as the cause (benign or malignant) of biliary obstruction, other criteria such as luminal content (concretion, sludge, solid masses), thickening of bile duct wall and compression by neighboring pathological structures are of great importance.1
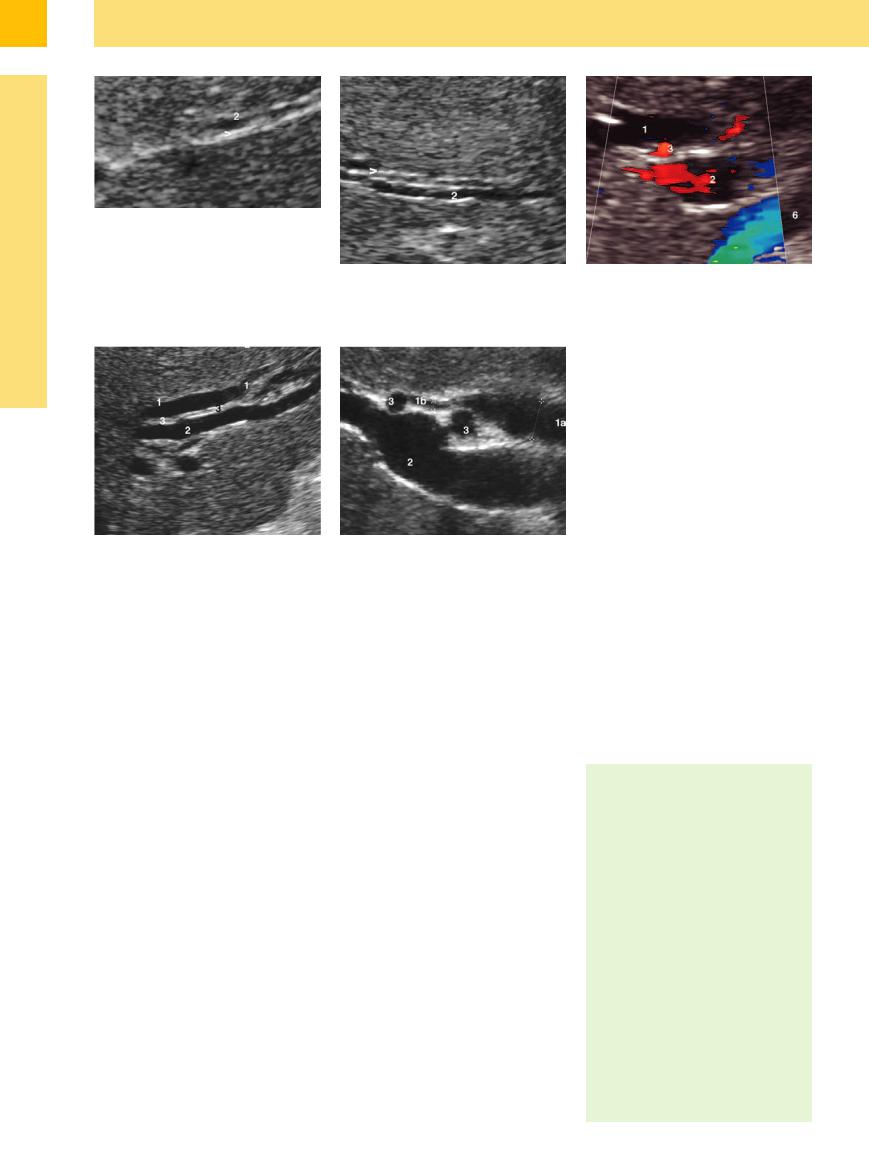
Diameter (Fig. 3.1, Fig. 3.2)
●Barely visible interlobar branches
●Right/left hepatic duct: 1–2 mm
●Hilar common hepatic duct: 1–2 mm/ detection limit
●Prepancreatic CBD: 3–7(9) mm
Shape
●Slender interlobar segment/close to the hepatic duct confluence
●Hepatic duct confluence not or barely visualized
●Slender hilar segment
●Slender/slightly ectatic prepancreatic segment
●Intrapancreatic segment not or barely visualized
Fig. 3.1 Anatomy of the biliary tree.
3
Biliary Tree
127
3
Biliary Tree and Gallbladder
Fig. 3.2 Diameter of the intrahepatic biliary tree.
a Slender intrahepatic bile duct (>) (segment II), accompanying branch of the portal vein (2).
endoscopic intervention. Thus, any statement of “standard values” for the diameter of the intrahepatic and extrahepatic bile ducts carries quite a large degree of uncertainty.
Shape. Under normal pressure conditions (<20 cmH2O), the intrahepatic and extrahepatic biliary tree is slender, particularly so upstream of where the hepatic artery crosses the com-
b Slightly dilated intrahepatic bile duct (>) (segment III), accompanying branch of the portal vein (2).
mon duct. The hepatic duct confluence is very difficult to visualize on ultrasound ( 3.1 d). Even minor increases in intraductal pressure will change the morphology of the confluence (Fig. 3.2b), i. e., it appears to become visualized more easily rather than there being any actual changes in the measurements themselves, and the differentiation between the intrahepatic and extrahepatic segments of the biliary sys-
3.1 d). Even minor increases in intraductal pressure will change the morphology of the confluence (Fig. 3.2b), i. e., it appears to become visualized more easily rather than there being any actual changes in the measurements themselves, and the differentiation between the intrahepatic and extrahepatic segments of the biliary sys-
c Hepatic duct confluence with moderate biliary obstruction. Hepatic duct confluence (1) and portal vein (2), branch of the hepatic artery (3), inferior vena cava (6).
Fig. 3.3 Dilated intrahepatic bile duct (1), accompanying branch of the portal vein (2), and hepatic artery (3) (segment III).
fFig. 3.4 Prepancreatic cholangiectasis with ampullary CBD (1a) and slender segment near the hepatic duct confluence (1b); early branching of the hepatic artery as a regular variant (3); portal vein (2).
tem increases almost excessively (Fig. 3.2c). Those segments close to the hepatic duct con-
fluence and the latter itself can be differentiated immediately and the intrahepatic bile ducts become dilated, resulting in the wellknown “double-barreled shotgun sign” (Fig. 3.2b, Fig. 3.3).2,3
Topography and Ultrasound Morphology
Ultrasound Morphology 





































Both the other vessels of the hepatic triad, the trunks and branches of the portal vein and the hepatic artery, can be considered mandatory and highly reliable sonographic landmarks accompanying the intrahepatic and extrahepatic biliary tree.
Intrahepatic biliary tree. Ultrasound visualization of the intrahepatic biliary tree (Fig. 3.2, Fig. 3.3) is facilitated by the fact that the regular vascular branching of the hepatic triad (“vascular architecture”) at all levels results in multiple, ever-smaller branches running parallel to the surface of the probe, which makes for optimum detection. The best resolution of detail, almost resembling that of a magnifying glass, is seen in the portal vein branches (up to the intralobular level), followed by the small branches of the bile ducts. Normally, only the large intrahepatic branches of the hepatic artery can be seen (with color-flow Doppler scanning even more peripheral branches may be
visualized especially in typical cirrhotic arterial hyperperfusion).
Extrahepatic biliary tree ( 3.1). The hilar/ prepancreatic course of the extrahepatic biliary tree is also well defined in terms of ultrasound anatomy by the vascular triads originating here. The portal vein always runs posterior to the more slender common duct (see Fig. 3.1,
3.1). The hilar/ prepancreatic course of the extrahepatic biliary tree is also well defined in terms of ultrasound anatomy by the vascular triads originating here. The portal vein always runs posterior to the more slender common duct (see Fig. 3.1,
Fig. 3.2c, Fig. 3.4, Fig. 3.5a,b). The relationship of the portal vein with the hepatic artery and its variant extrahepatic hilar branches is somewhat more complex (Fig. 3.5c,d). The hepatic artery always enters the porta hepatis from the left4 ( 3.1e–g) and therefore initially lies to the left of the common duct; it (or its main right branch) then crosses behind the common duct. Thus, it courses anterior to the portal vein and posterior to the common duct (
3.1e–g) and therefore initially lies to the left of the common duct; it (or its main right branch) then crosses behind the common duct. Thus, it courses anterior to the portal vein and posterior to the common duct ( 3.1a–c, Fig. 3.2c), and in scans of the porta hepatis (
3.1a–c, Fig. 3.2c), and in scans of the porta hepatis ( 3.1e–g) it appears as a round tubular crosssection. Infrequently—only in about 5%—this
3.1e–g) it appears as a round tubular crosssection. Infrequently—only in about 5%—this
Topography
●Hepatic triads:
Branches of the bile ducts, hepatic artery, and portal vein running in parallel
●Intrahepatic:
Interlobular sheaths of connective tissue
●Extrahepatic:
Between segments I (caudate lobe) and IVb, then posterior to the duodenum and head of the pancreas/intrapancreatic caudad to the gastroduodenal artery
Sonographic landmarks
●Intrahepatic:
Typical topography of the branching structures accompanying the portal vein (segments II + III)
●Extrahepatic:
Portal vein to the posterior hepatic artery from the left running between portal vein and common duct, denting the latter
128
3
Biliary Tree
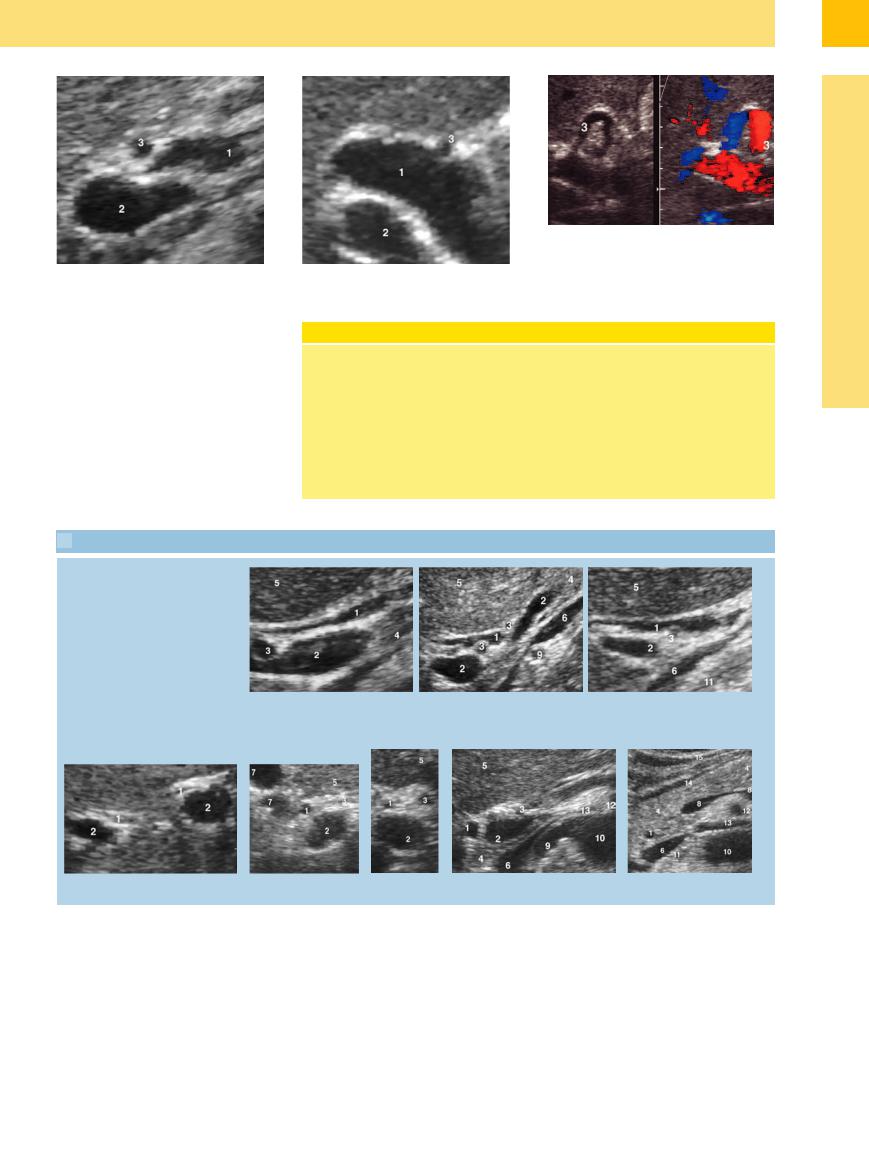
Fig. 3.5 Hepatic artery.
a and b Variants in the position of the hepatic artery (3); here, it is anterior to the dilated common duct (1); portal vein (2).
cross-section of the hepatic artery may progress into its intrahepatic course anterior to the common duct (Fig. 3.5a,b).5 Owing to the pressure of the adjacent pancreatic parenchyma, the intrapancreatic segment of the CBD is almost impossible to visualize; it is best seen in sections orthogonal to its anatomical course ( 3.1h).
3.1h).
Clinical Notes
The structures of the porta hepatis are best imaged with the patient in the left lateral decubitus position and inhaling deeply: this moves the liver caudad and to the left, thereby providing an excellent “sono-opti- cal” window. Occasionally intercostal planes are necessary in relative diaphragmatic elevation. Planes that capture the structures of the porta hepatis parallel to their longitudinal axis are preferable. As a
c and d Kinking of the hepatic artery (3).
result, in slim patients the probe must be tilted more towards the longitudinal axis, in stouter patients more to the horizontal axis.
Previous surgery in the upper abdomen often leads to significant scarring with a subsequent left shift of the intestinal organs (including the common duct being located in front of the pancreas) as the adhesions tend to shrink.
 3.1 Anatomy of the Extrahepatic Biliary Tree
3.1 Anatomy of the Extrahepatic Biliary Tree
Common duct (1), portal vein (2), hepatic artery (3), pancreas (4), liver (5), inferior vena cava (6), left and right hepatic ducts (7), splenic vein (8), right renal artery (9), abdominal aorta (10), crura of diaphragm (11), superior mesenteric artery (12), left renal vein (13), posterior wall of the gastric antrum (14), anterior wall of the gastric antrum (15)
a |
b |
c |
d |
e |
f |
g |
h |
129
