
- •Contents
- •Preface
- •Contributors
- •1 Vessels
- •1.1 Aorta, Vena Cava, and Peripheral Vessels
- •Aorta, Arteries
- •Anomalies and Variant Positions
- •Dilatation
- •Stenosis
- •Wall Thickening
- •Intraluminal Mass
- •Perivascular Mass
- •Vena Cava, Veins
- •Anomalies
- •Dilatation
- •Intraluminal Mass
- •Compression, Infiltration
- •1.2 Portal Vein and Its Tributaries
- •Enlarged Lumen Diameter
- •Portal Hypertension
- •Intraluminal Mass
- •Thrombosis
- •Tumor
- •2 Liver
- •Enlarged Liver
- •Small Liver
- •Homogeneous Hypoechoic Texture
- •Homogeneous Hyperechoic Texture
- •Regionally Inhomogeneous Texture
- •Diffuse Inhomogeneous Texture
- •Anechoic Masses
- •Hypoechoic Masses
- •Isoechoic Masses
- •Hyperechoic Masses
- •Echogenic Masses
- •Irregular Masses
- •Differential Diagnosis of Focal Lesions
- •Diagnostic Methods
- •Suspected Diagnosis
- •3 Biliary Tree and Gallbladder
- •3.1 Biliary Tree
- •Thickening of the Bile Duct Wall
- •Localized and Diffuse
- •Bile Duct Rarefaction
- •Localized and Diffuse
- •Bile Duct Dilatation and Intraductal Pressure
- •Intrahepatic
- •Hilar and Prepancreatic
- •Intrapancreatic
- •Papillary
- •Abnormal Intraluminal Bile Duct Findings
- •Foreign Body
- •The Seven Most Important Questions
- •3.2 Gallbladder
- •Changes in Size
- •Large Gallbladder
- •Small/Missing Gallbladder
- •Wall Changes
- •General Hypoechogenicity
- •General Hyperechogenicity
- •General Tumor
- •Focal Tumor
- •Intraluminal Changes
- •Hyperechoic
- •Hypoechoic
- •Nonvisualized Gallbladder
- •Missing Gallbladder
- •Obscured Gallbladder
- •4 Pancreas
- •Diffuse Pancreatic Change
- •Large Pancreas
- •Small Pancreas
- •Hypoechoic Texture
- •Hyperechoic Texture
- •Focal Changes
- •Anechoic Lesion
- •Hypoechoic Lesion
- •Isoechoic Lesion
- •Hyperechoic Lesion
- •Irregular (Complex Structured) Lesion
- •Dilatation of the Pancreatic Duct
- •Marginal/Mild Dilatation
- •Marked Dilatation
- •5 Spleen
- •Nonfocal Changes of the Spleen
- •Diffuse Parenchymal Changes
- •Large Spleen
- •Small Spleen
- •Focal Changes of the Spleen
- •Anechoic Mass
- •Hypoechoic Mass
- •Hyperechoic Mass
- •Splenic Calcification
- •6 Lymph Nodes
- •Peripheral Lymph Nodes
- •Head/Neck
- •Extremities (Axilla, Groin)
- •Abdominal Lymph Nodes
- •Porta Hepatis
- •Splenic Hilum
- •Mesentery (Celiac, Upper and Lower Mesenteric Station)
- •Stomach
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •Small/Large Intestine
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •8 Peritoneal Cavity
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Wall Structures
- •Smooth Margin
- •Irregular Margin
- •Intragastric Processes
- •Intraintestinal Processes
- •9 Kidneys
- •Anomalies, Malformations
- •Aplasia, Hypoplasia
- •Cystic Malformation
- •Anomalies of Number, Position, or Rotation
- •Fusion Anomaly
- •Anomalies of the Renal Calices
- •Vascular Anomaly
- •Diffuse Changes
- •Large Kidneys
- •Small Kidneys
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Irregular Structure
- •Circumscribed Changes
- •Anechoic Structure
- •Hypoechoic or Isoechoic Structure
- •Complex Structure
- •Hyperechoic Structure
- •10 Adrenal Glands
- •Enlargement
- •Anechoic Structure
- •Hypoechoic Structure
- •Complex Echo Structure
- •Hyperechoic Structure
- •11 Urinary Tract
- •Malformations
- •Duplication Anomalies
- •Dilatations and Stenoses
- •Dilated Renal Pelvis and Ureter
- •Anechoic
- •Hypoechoic
- •Hypoechoic
- •Hyperechoic
- •Large Bladder
- •Small Bladder
- •Altered Bladder Shape
- •Intracavitary Mass
- •Hypoechoic
- •Hyperechoic
- •Echogenic
- •Wall Changes
- •Diffuse Wall Thickening
- •Circumscribed Wall Thickening
- •Concavities and Convexities
- •12.1 The Prostate
- •Enlarged Prostate
- •Regular
- •Irregular
- •Small Prostate
- •Regular
- •Echogenic
- •Circumscribed Lesion
- •Anechoic
- •Hypoechoic
- •Echogenic
- •12.2 Seminal Vesicles
- •Diffuse Change
- •Hypoechoic
- •Circumscribed Change
- •Anechoic
- •Echogenic
- •Irregular
- •12.3 Testis, Epididymis
- •Diffuse Change
- •Enlargement
- •Decreased Size
- •Circumscribed Lesion
- •Anechoic or Hypoechoic
- •Irregular/Echogenic
- •Epididymal Lesion
- •Anechoic
- •Hypoechoic
- •Intrascrotal Mass
- •Anechoic or Hypoechoic
- •Echogenic
- •13 Female Genital Tract
- •Masses
- •Abnormalities of Size or Shape
- •Uterus
- •Abnormalities of Size or Shape
- •Myometrial Changes
- •Intracavitary Changes
- •Endometrial Changes
- •Fallopian Tubes
- •Hypoechoic Mass
- •Anechoic Cystic Mass
- •Solid Echogenic or Nonhomogeneous Mass
- •14 Thyroid Gland
- •Diffuse Changes
- •Enlarged Thyroid Gland
- •Small Thyroid Gland
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Circumscribed Changes
- •Anechoic
- •Hypoechoic
- •Isoechoic
- •Hyperechoic
- •Irregular
- •Differential Diagnosis of Hyperthyroidism
- •Types of Autonomy
- •15 Pleura and Chest Wall
- •Chest Wall
- •Masses
- •Parietal Pleura
- •Nodular Masses
- •Diffuse Pleural Thickening
- •Pleural Effusion
- •Anechoic Effusion
- •Echogenic Effusion
- •Complex Effusion
- •16 Lung
- •Masses
- •Anechoic Masses
- •Hypoechoic Masses
- •Complex Masses
- •Index

8
Peritoneal Cavity
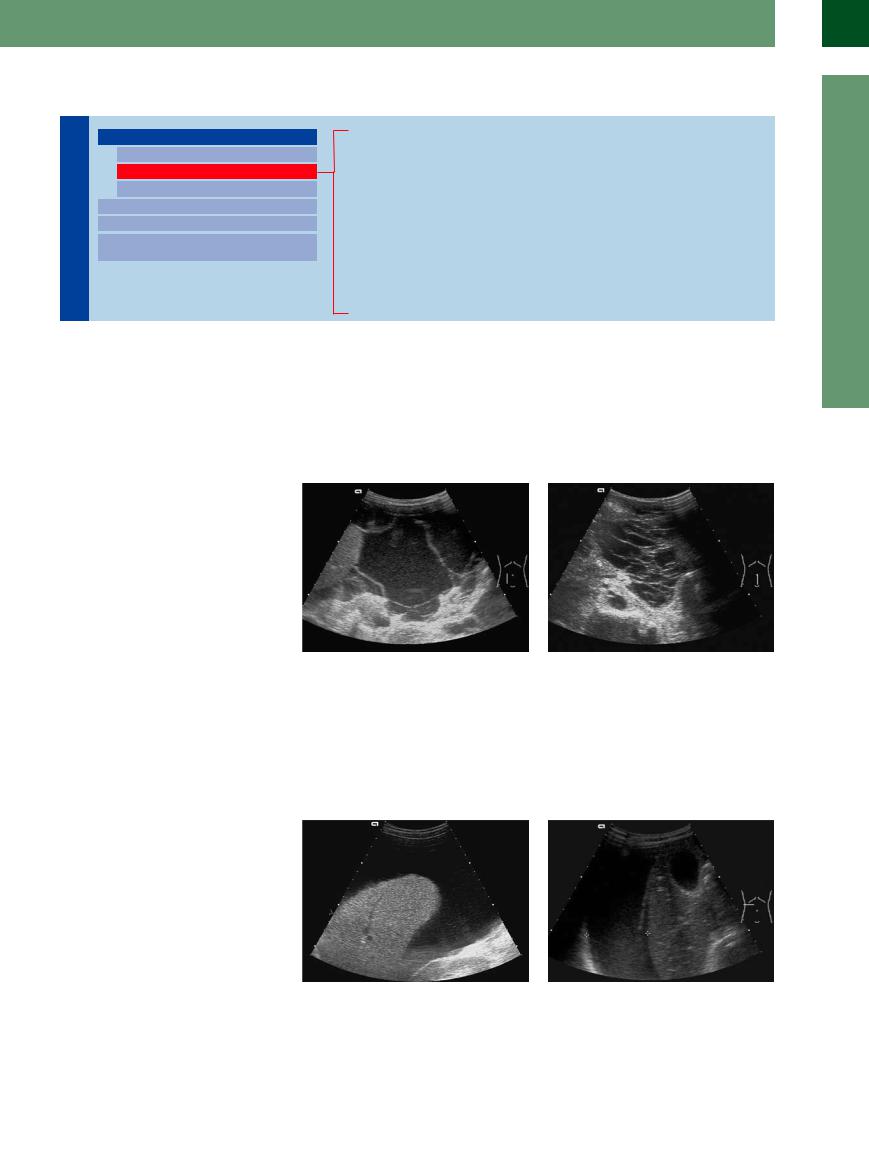
Table 8.4 Differential diagnosis of intraperitoneal fluid12 |
|
|
|
Transudate (anechoic) |
Exudate |
Hemorrhage |
Postoperative, posttraumatic |
|
(anechoic or echogenic) |
|
(echogenic) |
Cirrhosis of the liver |
Peritoneal carcinomatosis |
Trauma |
Hematoma |
Budd–Chiari syndrome |
Peritonitis |
Iatrogenic |
Seroma |
Right-sided heart failure |
Pancreatitis |
Ectopic pregnancy |
Biloma |
Inferior vena cava syndrome |
Tuberculosis |
Coagulation disorder |
Urinoma |
Nephrotic syndrome |
Peritoneal dialysis |
Ruptured abdominal aortic aneurysm |
Chyme |
Mesenteric venous thrombosis |
Mesothelioma |
|
Contents of a cyst |
Hypoalbuminemia |
|
|
Lymphocele (chyliform ascites) |
Anechoic Structure
Peritoneal Cavity

Diffuse Changes
Anechoic Structure
Hypoechoic Structure
Hyperechoic Structure
Localized Changes
Wall Structures
Differentiating Intraand Extraluminal
GI Tract Fluid
Cirrhosis of the Liver
Heart Failure
Peritonitis
Hypoalbuminemia
Peritoneal Carcinomatosis
Hemoperitoneum
Ruptured Cyst
Urinoma (Intraperitoneal)
Transudate. Most anechoic intra-abdominal |
peritoneal carcinomatosis. Note that acute |
masses are transudates. There are no fine par- |
hemorrhage after blunt abdominal trauma |
ticles floating in the fluid, no strands of fibrin, |
may also appear as anechoic fluid during its |
and no irregularities in the wall, examples |
early phase. |
being cirrhosis of the liver, heart failure, and |
|
Cirrhosis of the Liver
of the Liver 
















































In most cases ascites in cirrhosis with hepatic failure is anechoic (Fig. 8.14). When the patient is being repositioned it will shift location and may be demonstrated in all compartments. The underlying disease can be diagnosed quite easily based on the organ changes in the liver: altered shape, outline, size, intrahepatic vascular pattern, and the extrahepatic signs of portal hypertension, splenomegaly, and portovenous shunts (collaterals) (see  2.2, p. 65, and
2.2, p. 65, and  2.7, p. 83). The irregular surface of the liver and the splenomegaly are the easiest and most reliable signs to detect.
2.7, p. 83). The irregular surface of the liver and the splenomegaly are the easiest and most reliable signs to detect.
Fig. 8.14 Diffuse collection of anechoic fluid in alcoholic |
b Coarsely structured hepatic parenchyma, changes in |
cirrhosis of the liver. |
the vascular pattern, rounded margin. |
a Transverse view high up in the upper right quadrant: |
|
ascites (A) and pleural effusion (E); the abdominal and |
|
thoracic cavity are separated by the echogenic dia- |
|
phragm (ZW). L = liver. |
|
300
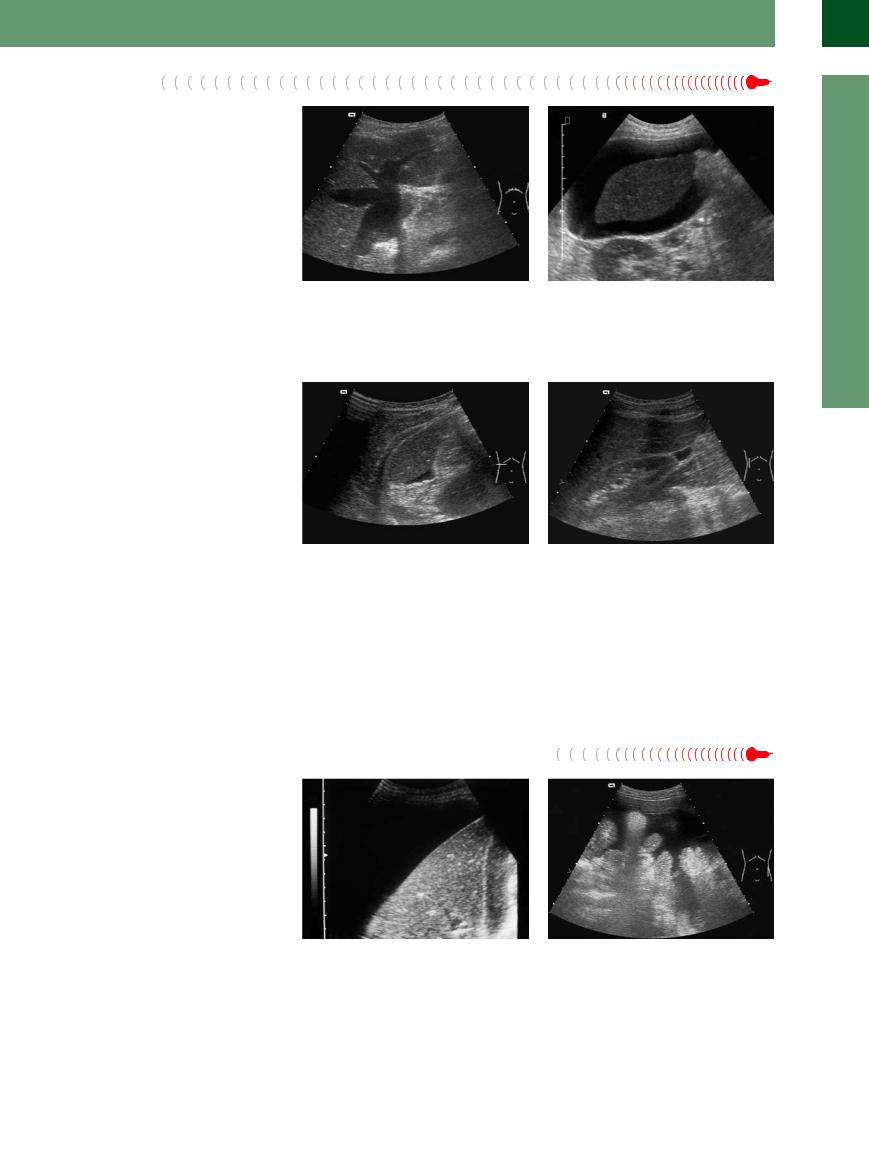
Heart Failure
Transudate in decompensated right-sided heart failure is a late symptom and appears after or concomitant with pleural effusion (right > left). Apart from the general clinical signs, ultrasound will demonstrate a markedly wide and rigid inferior vena cava and wide hepatic veins (with pronounced star-like junction) as definite signs firming up the suspected diagnosis (Fig. 8.15).
Fig. 8.15 Right-sided heart failure. |
b Right hepatic lobe bathed in anechoic ascites (transu- |
a The wide and rigid inferior vena cava and the wide |
date) in decompensated right-sided heart failure. |
hepatic veins are characteristic for right ventricular failure. |
|
Peritonitis 






















































Inflammation and infection in the peritoneal cavity mostly result in exudates, and thus in echogenic ascites with strands of fibrin and septation. If there is only a small amount of hypersecretion, e. g., in viral infection with polyserositis, the ascites may also be anechoic (Fig. 8.16). Markedly purulent peritonitis is characterized by echogenic contents, adhesions, and bowel loops that no longer glide unencumbered. In “spontaneous bacterial peritonitis” (SBP) complicating decompensated cirrhosis of the liver, there will often be fine echoes within the fluid.
Fig. 8.16
a Small amount of subhepatic ascites in viral polyserositis (accompanied by pleural and pericardial effusion = multicavity effusion).
Hypoalbuminemia


















































Irrespective of its origin, protein deficiency |
bladder is thicker than normal (>3 mm). Apart |
with a markedly low level of plasma albumin |
from this observation, the liver appears un- |
may result in the production of a hypoechoic |
changed and there are no wide veins. Labora- |
transudate. In these cases the wall of the gall- |
tory studies will yield further diagnostic clues. |
b Small “angle of ascites” between the right hepatic lobe and the inferior pole of the right kidney in concomitant viral peritonitis.
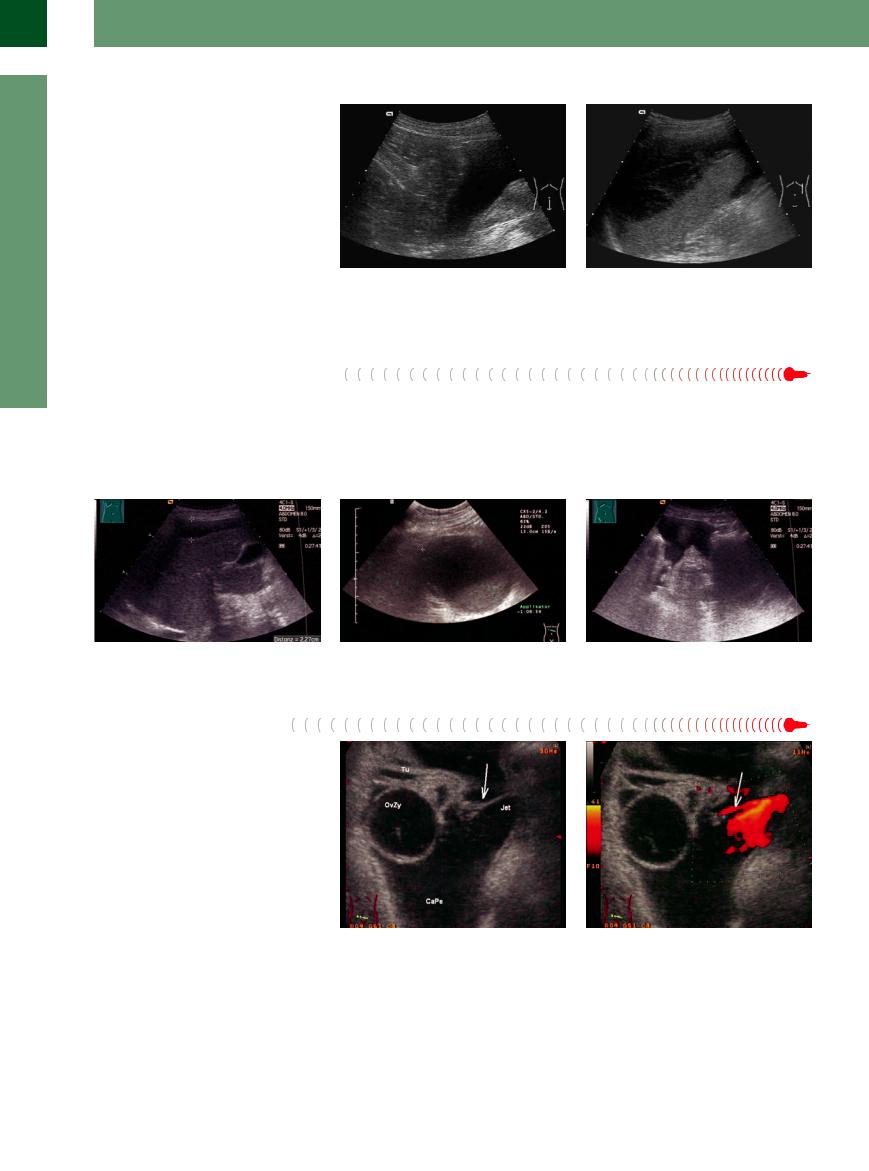
Peritoneal Carcinomatosis 






















The malignant ascites in peritoneal carcinomatosis may also be anechoic (Fig. 8.17, Fig. 8.18), but internal echoes within the fluid are much more common. In anechoic ascites, the lack of any signs for cirrhosis of the liver or portal hypertension on the one hand and the demonstration of a possible primary tumor or metastases on the other will lead one to suspect the malignant origin. A detailed description of the ultrasound criteria differentiating between benign and malignant ascites is found in the section on “Wall Structures” (pp. 315–316).
Fig. 8.17 Anechoic ascites enveloping the liver in peritoneal carcinomatosis of metastatic gastric cancer. Most often peritoneal carcinomatosis will display echoes within the fluid, but it may also be anechoic.
Fig. 8.18 Anechoic malignant ascites in advanced gastric cancer. The retracted mesentery quite clearly pulls the bowel loops together.
8
Diffuse Changes
301
8
Peritoneal Cavity
Hemoperitoneum


















































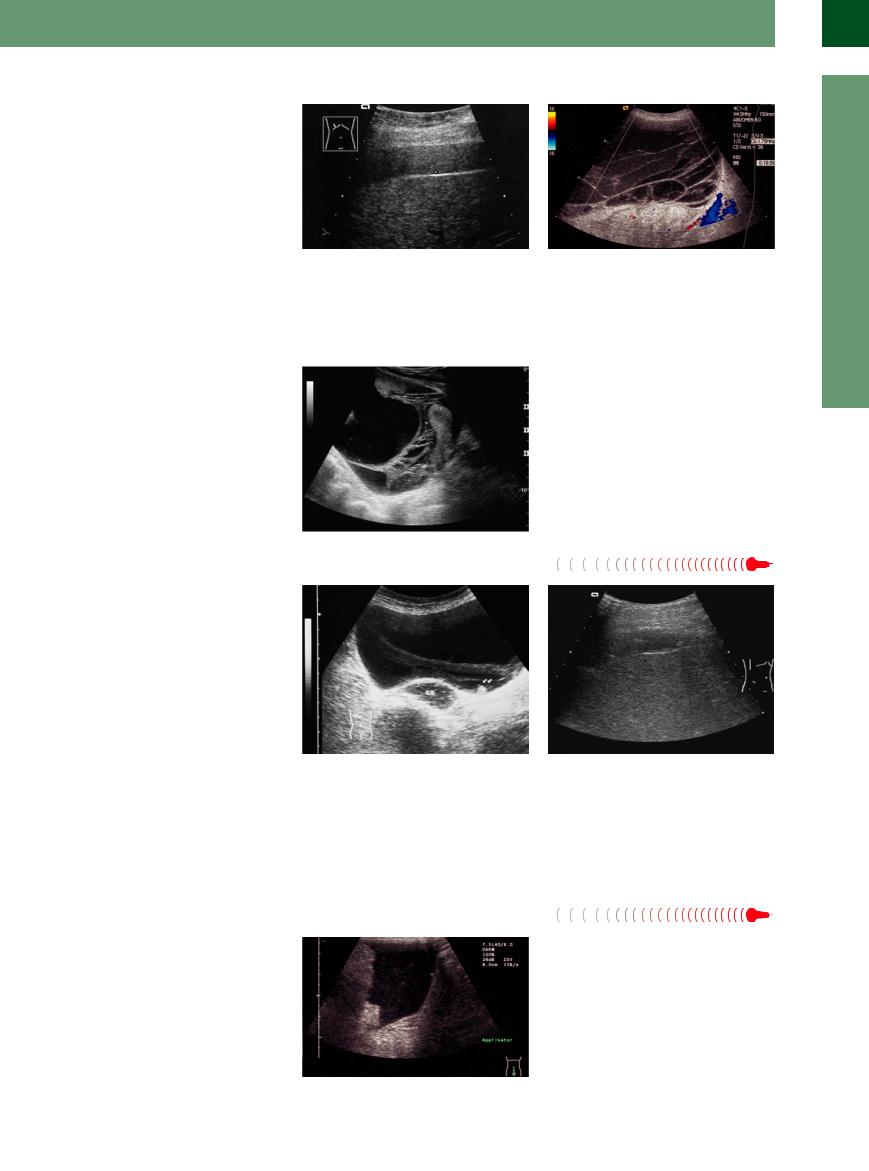
During its early phase, acute bleeding into the peritoneal cavity after blunt abdominal trauma, iatrogenic injury, in ectopic pregnancy, or drug-induced pathology (e. g., anticoagulation therapy) will also demonstrate an anechoic fluid collection (Fig. 8.19). However, as time passes (hours) there will be echogenic internal echoes due to strands of fibrin that are formed while coagulation sets in. History, clinical signs, and the changing ultrasound image will firm up the diagnosis in 95–98% of cases.
Fig. 8.19 |
b This massive hemoperitoneum was caused by a |
a Anechoic hemoperitoneum with blood in the lesser |
marked splenic lesion. The hematoma encompasses |
pelvis after blunt abdominal trauma. With the passage |
more than 50% of the organ, while at the inferior pole |
of time there will be echoes and strands of fibrin, indicat- |
of the spleen there is free blood, indicating open rupture. |
ing the beginning of organization. |
|
Ruptured Cyst
Cyst










Liver cysts, kidney cysts, and pancreatic |
If previous scans of the cyst exist, the diag- |
(pseudo-) cysts can rupture and spill their con- |
nosis is easily made if the cyst is now missing. |
tents into the peritoneal cavity creating the |
Pancreatic pseudocysts in particular can mimic |
picture of ascites of unknown origin. This may |
the symptoms and signs of an acute abdomen |
occur without clinical symptoms or may cause |
(Fig. 8.20a–c). |
extensive pain. |
|
Fig. 8.20 |
b Pancreatic cyst showed signs of an acute abdomen a |
c Demonstration of free liquid in the lower abdominal |
a Perihepatic accumulation of liquid after pancreas pseu- |
few days before the painful rupture, but conservative |
cavity after a ruptured pancreatic pseudocyst. |
docyst rupture. |
treatment was possible. |
|
Urinoma  (Intraperitoneal)
(Intraperitoneal)
A collection of urine in the abdominal cavity is mainly caused by iatrogenic, traumatic, or malignant leakage of the urinary tract system. Intra-abdominal liquid in this case is mainly anechoic or slightly echogenic. Acute leakage of urine is typically painful, but chronic urine leakage, on the other hand, can be tolerated for a long time (Fig. 8.21a,b).
Fig. 8.21 |
b With color Doppler (power mode) a leaking ureter can |
a Unidentified ascites in the left lower abdomen with |
be detected. Ureter leak (arrow) after iatrogenic injury to |
demonstration of a small ovarian cyst (OvZy) of the left |
the left ureter. |
adnexa. TU = fallopian tube; CaPe = peritoneal cavity. |
(Images courtesy of Dr. Albrecht Holle, University of Ro- |
|
stock, Germany.) |
302
Hypoechoic Structure
Cavity |
|
Diffuse Changes |
|||
|
|
|
|
||
|
|
|
|
|
Anechoic Structure |
Peritoneal |
|
|
Hypoechoic Structure |
||
|
|
||||
|
|
Hyperechoic Structure |
|||
|
|
|
|
|
|
|
|
|
|
Localized Changes |
|
|
|
|
|
||
|
|
|
|
Wall Structures |
|
|
|
|
|
||
|
|
|
|
Differentiating Intraand Extraluminal |
|
|
|
|
|
||
|
|
|
|
GI Tract Fluid |
|
Pancreatitis
Cirrhosis of the Liver with Spontaneous Bacterial Peritonitis (SBP) Peritoneal Carcinomatosis
Purulent Peritonitis Tuberculosis Choleperitoneum Hemoperitoneum GI Tract Perforation Chyloperitoneum
Pseudomyxoma Peritonei
Exudate. In most cases, the hypoechoic intra- |
brin will demonstrate a classic swinging or |
complication of decompensated cirrhosis of the |
abdominal liquid structure displaying fine in- |
undulating motion with the shifting intra-ab- |
liver. However, echogenic internal echoes |
ternal echoes or septation will be an exudate. |
dominal fluid. Examples of echogenic ascites |
within the fluid have been demonstrated in |
Strand-like structures adhering to the lateral |
are pancreatogenous ascites and the ascites in |
peritoneal carcinomatosis as well. |
abdominal wall or the visceral peritoneum are |
purulent peritonitis. Ascites permeated by fine |
|
also rather characteristic. These strands of fi- |
floating echoes may be present in SBP, a classic |
|
Pancreatitis 





















































In many cases of acute or recurrent pancreatitis exudation into the free peritoneal cavity will be seen. This is more true for necrotizing pancreatitis than for the hemorrhagic type. In severe cases, all compartments are involved, presenting the full-blown picture of pancreatogenous ascites. The latter may be anechoic, although internal echoes and septation as well as irregularities in the walls are much more common (Fig. 8.22, Fig. 8.23). The ultrasound image is characterized by floating strands of fibrin. The inflammatory changes in the pancreas itself (necrosis and other signs of pancreatitis as well as vascular changes) are also important for the diagnosis. If the clinical signs and ultrasound study do not result in a firm diagnosis, ultrasound-guided fine-needle paracentesis, with high levels of amylase and lipase in the ascites will prove the pancreatic origin.
Fig. 8.22 Echogenic ascites with numerous strands of fibrin (“waving flag”) resulting in septation; pancreatogenous ascites in acute necrotizing pancreatitis.
Fig. 8.23 Complete septation in the lower abdomen, classic honeycomb pattern in pancreatogenous ascites (necrotizing pancreatitis). Similar images are also seen in tuberculous ascites.
Cirrhosis  of the Liver with Spontaneous
of the Liver with Spontaneous Bacterial
Bacterial Peritonitis (SBP)
Peritonitis (SBP) 























Decompensated cirrhosis of the liver is usually characterized by anechoic ascites, although fine echoes floating in the fluid can be demonstrated in up to 20% of patients (Fig. 8.24a,b). In some marked cases there will be septation, mural strands of fibrin, and partially septated ascites. Ultrasound-guided fine-needle paracentesis and the subsequent laboratory workup (granulocyte count and bacterial culture) will firm up the diagnosis. Intractable echogenic ascites in cirrhosis of the liver implies SBP and warrants further study.
Fig. 8.24 |
b Echogenic ascites lateral to the right hepatic lobe with |
a Characteristic image of micronodular cirrhosis of the |
a single strand of fibrin in SBP. |
liver with marked ascites. The diffusely distributed fine |
|
echoes could be due to spontaneous bacterial peritonitis |
|
(SBP). |
|
8
Diffuse Changes
303
8
Peritoneal Cavity
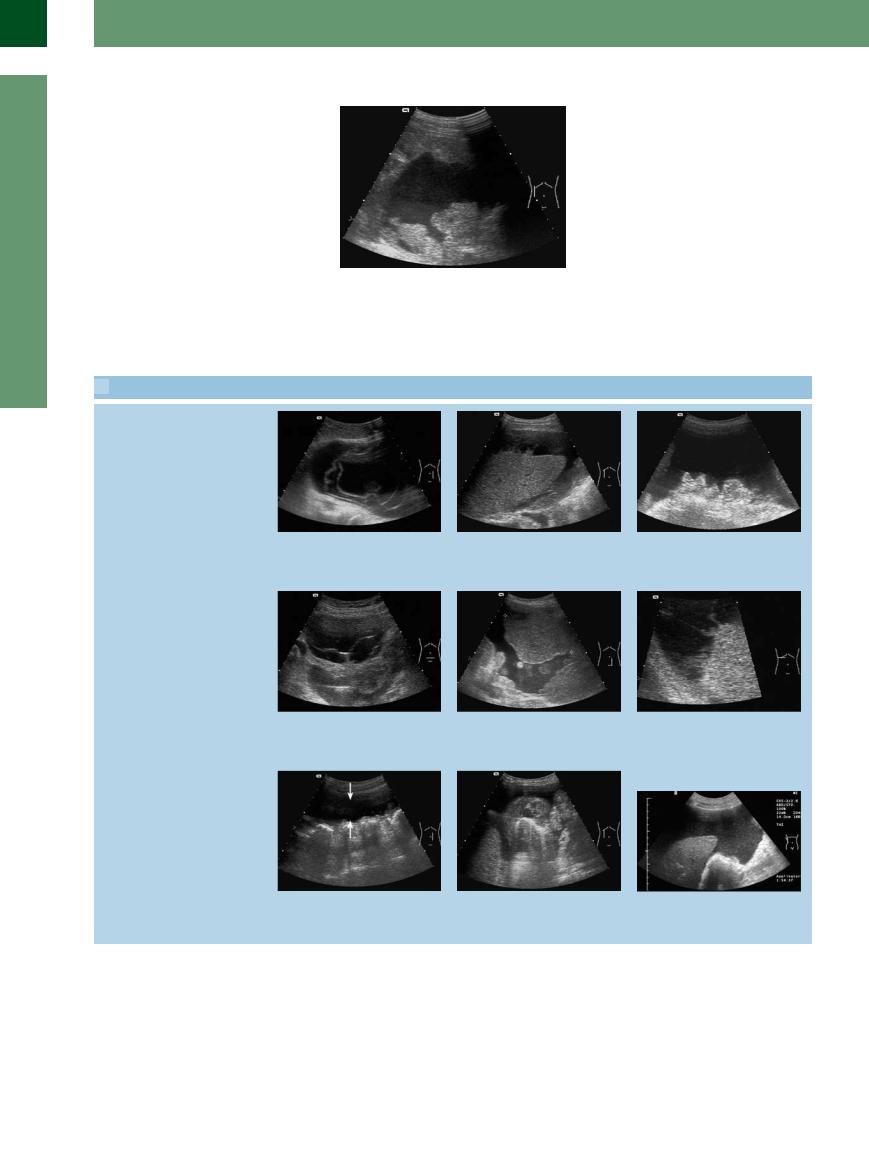
Peritoneal Carcinomatosis 













































Peritoneal carcinomatosis is characterized by echogenic ascites with fine echoes, irregular margin, septation, retraction of the mesentery, and solid structures on the peritoneum itself (Fig. 8.25,  8.3). Differentiating between benign and malignant ascites resembles putting together a puzzle and will be explained further on (see Table 8.6, Table 8.7,
8.3). Differentiating between benign and malignant ascites resembles putting together a puzzle and will be explained further on (see Table 8.6, Table 8.7,  8.6). The sensitivity of a single ultrasound-guided fine-needle puncture is unacceptably low (50–60%). If there is a definite case for suspected malignancy, repeat cytology is called for (at least three times, or until a sufficient amount of centrifugate is obtained). Peritoneal carcinomatosis can be chameleon-like in its variability; it is detailed further in
8.6). The sensitivity of a single ultrasound-guided fine-needle puncture is unacceptably low (50–60%). If there is a definite case for suspected malignancy, repeat cytology is called for (at least three times, or until a sufficient amount of centrifugate is obtained). Peritoneal carcinomatosis can be chameleon-like in its variability; it is detailed further in  8.3.
8.3.
Fig. 8.25 Echogenic ascites and markedly thickened as well as irregularly delineated peritoneum in peritoneal carcinomatosis due to advanced cancer of the colon.
 8.3 Echogenic Ascites in Peritoneal Carcinomatosis
8.3 Echogenic Ascites in Peritoneal Carcinomatosis
a Strand-like structures originating from the peritoneum in ovarian malignancy with peritoneal carcinomatosis.
d Ascites with honeycomb septation in cystic ovarian malignancy. This aspect without acute symptoms is characteristic of a gynecological process.
g Markedly pushed-back mesentery and air-filled bowel. Increased distance between omentum/bowel and abdominal wall, indicating peritoneal carcinomatosis.
b ”Turbid” echogenic ascites and fibrin apposition in peritoneal carcinomatosis of metastasizing gastric cancer. Normal hepatic texture; smooth margins.
e Marked thickening of the abdominal wall with tumor masses adhering to the peritoneum: peritoneal carcinomatosis in colon cancer.
h Thickened visceral peritoneum in peritoneal carcinomatosis (gastric cancer) mimicking a pathological gut signature.
c Malignant ascites with fine internal echoes and a markedly retracted mesentery: peritoneal carcinomatosis in cancer of the colon.
f Echogenic ascites and fine appositions on the parietal peritoneum in peritoneal carcinomatosis (gastric cancer).
i Typical “snowstorm” (echogenic ascites) surrounding the liver and a retracted mesentery in malignant ascites in a patient with advanced gastric cancer.
304
Purulent  Peritonitis
Peritonitis

















































The ultrasound image of purulent peritonitis is characterized by inhomogeneous hypoechoic structures displaying a varied echo texture and lacking a definite interconnection (Fig. 8.26). During repositioning of the patient, the septation and adhesions will not permit free shifting of the putrid ascites. The clinical symptoms take puncture over any other modality. Ultrasound studies are of limited value in the primary diagnosis and are much more useful in identifying walled-off abscesses. Most often treatment is by surgery.
Fig. 8.26
a Purulent peritonitis. Structured fluid (calipers) enveloping the liver. Clinically: perforated duodenal ulcer.
b Diffuse purulent peritonitis with locular (structured) ascites after a surgical revision of the bile duct.
Tuberculosis





















































The sonographic morphology of tuberculous |
Fig. 8.27 Extensive peritoneal tuberculosis in a young |
ascites resembles that in necrotizing pancrea- |
woman. Pronounced structure with septa between the |
titis. As well as echoes within the fluid there is |
abdominal fluid. |
|
|
also septation and the wall is irregular in out- |
|
line. If the paracentetic specimen is hemorrha- |
|
gic, this is also indicative in terms of diagnosis |
|
(Fig. 8.27). |
|
Choleperitoneum 



























Bile leakage may be due to a perforated hydropic or empyemic gallbladder as a rare complication of cholecystolithiasis. Localized perforation is much more common than free bile leakage into the abdominal cavity (choleperitoneum). Other causes may be intraoperative lesions to the biliary tree or iatrogenic endoscopic injury. Another quite common complication after external percutaneous transhepatic bile duct drainage (PTCD) for palliation of a stenosing malignancy is dislocation of the drain with subsequent bile leakage.
Initially the leaking bile is anechoic, but after a few hours the characteristic streaks and septa will appear that induce layering and which are pathognomonic (Fig. 8.28). In those few cases with uncertain diagnosis, ultrasound-guided fine-needle puncture will confirm the free in- tra-abdominal bile (gross assessment and bilirubin panel).
Fig. 8.28
a Anechoic intra-abdominal formation with streaks of internal structures in choleperitoneum due to a perforated gallbladder (GB).
b Thin hypoechoic film around the right hepatic lobe due to intra-abdominal collection of bile in biliary leakage after a dislocated PTCD.
Hemoperitoneum



























Within a few hours after hemorrhage, the organizing hemoperitoneum will become more and more echogenic, comprising internal echoes, strands of fibrin, and septation. The effusion will become more hyperechoic and inhomogeneous (Fig. 8.29, Fig. 8.30). If there is no increase in volume (bleeding staunched), ultrasonography lends itself quite easily to morphological follow-up. The advancing orga-
Fig. 8.29 Echogenic ascites in the lower abdomen in a female patient with an overdose of phenprocoumon and extensive free bleeding into the peritoneal cavity (hemoperitoneum).
8
Diffuse Changes
305

8
Peritoneal Cavity
nization will be accompanied by absorption, and sometimes some regions will undergo reliquefaction.
Fig. 8.30 |
b Organizing hemoperitoneum in the lesser pelvis after |
a Hypoechoic seam below the right liver lobe after liver |
blunt force trauma with ruptured spleen. Blood collects in |
puncture. Iatrogenic hemoperitoneum after Menghini |
the deepest spot, in the early phase hypoechoic, later |
puncture (rare complication). |
echogenic and then increasingly septated and honey- |
|
combed. |
GI Tract Perforation


























The cardinal symptom of GI tract perforation is the demonstration of free gas within the peritoneal cavity. However, there may also be fluid leaking from the stomach or bowel. This fluid is permeated by echoes and displays gas inclusion (Fig. 8.31). Demonstration of the actual site leaking gas and liquid is a rare feat. The preferred localization of fluid collections in a perforated upper GI tract is around the stomach and duodenum as well as around both hepatic lobes. In perforation of the more downstream intestinal regions, the free gas tends to accumulate more in the lower abdomen (e. g., diverticulitis).
It should be kept in mind that the combination of free gas and free fluid may be indicative of GI tract perforation.
Fig. 8.31 Demonstration of echogenic fluid and some free gas after upper GI tract perforation (duodenal ulcer).
Chyloperitoneum 


















































Chyle leaking into the abdominal cavity is a rare event; possible causes include trauma or a postoperative complication. Chyloperitoneum has also been demonstrated in malignant lymphoma (cf. chylothorax in Chapter 15). Ultrasound will depict homogeneous ascites permeated by fine echoes, resulting in a “milky” image. In examinations with color Doppler ultrasound the color flow sign can be seen during movements. Ultrasound-guided fine-needle puncture permits diagnosis of chyloperitoneum at a glance: there is milky white, turbid lymph (Fig. 8.32a,b).
Fig. 8.32
a Transversal scan, ventral of the right kidney. Demonstration of a chyloperitoneum in a high-grade non-Hodg- kin lymphoma. Fibrin at the peritoneum.
b Drainage of a chyloperitoneum in a patient with nonHodgkin lymphoma; the bag contains yellow turbid lymphogenic drainage fluid.
306
