
- •Contents
- •Preface
- •Contributors
- •1 Vessels
- •1.1 Aorta, Vena Cava, and Peripheral Vessels
- •Aorta, Arteries
- •Anomalies and Variant Positions
- •Dilatation
- •Stenosis
- •Wall Thickening
- •Intraluminal Mass
- •Perivascular Mass
- •Vena Cava, Veins
- •Anomalies
- •Dilatation
- •Intraluminal Mass
- •Compression, Infiltration
- •1.2 Portal Vein and Its Tributaries
- •Enlarged Lumen Diameter
- •Portal Hypertension
- •Intraluminal Mass
- •Thrombosis
- •Tumor
- •2 Liver
- •Enlarged Liver
- •Small Liver
- •Homogeneous Hypoechoic Texture
- •Homogeneous Hyperechoic Texture
- •Regionally Inhomogeneous Texture
- •Diffuse Inhomogeneous Texture
- •Anechoic Masses
- •Hypoechoic Masses
- •Isoechoic Masses
- •Hyperechoic Masses
- •Echogenic Masses
- •Irregular Masses
- •Differential Diagnosis of Focal Lesions
- •Diagnostic Methods
- •Suspected Diagnosis
- •3 Biliary Tree and Gallbladder
- •3.1 Biliary Tree
- •Thickening of the Bile Duct Wall
- •Localized and Diffuse
- •Bile Duct Rarefaction
- •Localized and Diffuse
- •Bile Duct Dilatation and Intraductal Pressure
- •Intrahepatic
- •Hilar and Prepancreatic
- •Intrapancreatic
- •Papillary
- •Abnormal Intraluminal Bile Duct Findings
- •Foreign Body
- •The Seven Most Important Questions
- •3.2 Gallbladder
- •Changes in Size
- •Large Gallbladder
- •Small/Missing Gallbladder
- •Wall Changes
- •General Hypoechogenicity
- •General Hyperechogenicity
- •General Tumor
- •Focal Tumor
- •Intraluminal Changes
- •Hyperechoic
- •Hypoechoic
- •Nonvisualized Gallbladder
- •Missing Gallbladder
- •Obscured Gallbladder
- •4 Pancreas
- •Diffuse Pancreatic Change
- •Large Pancreas
- •Small Pancreas
- •Hypoechoic Texture
- •Hyperechoic Texture
- •Focal Changes
- •Anechoic Lesion
- •Hypoechoic Lesion
- •Isoechoic Lesion
- •Hyperechoic Lesion
- •Irregular (Complex Structured) Lesion
- •Dilatation of the Pancreatic Duct
- •Marginal/Mild Dilatation
- •Marked Dilatation
- •5 Spleen
- •Nonfocal Changes of the Spleen
- •Diffuse Parenchymal Changes
- •Large Spleen
- •Small Spleen
- •Focal Changes of the Spleen
- •Anechoic Mass
- •Hypoechoic Mass
- •Hyperechoic Mass
- •Splenic Calcification
- •6 Lymph Nodes
- •Peripheral Lymph Nodes
- •Head/Neck
- •Extremities (Axilla, Groin)
- •Abdominal Lymph Nodes
- •Porta Hepatis
- •Splenic Hilum
- •Mesentery (Celiac, Upper and Lower Mesenteric Station)
- •Stomach
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •Small/Large Intestine
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •8 Peritoneal Cavity
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Wall Structures
- •Smooth Margin
- •Irregular Margin
- •Intragastric Processes
- •Intraintestinal Processes
- •9 Kidneys
- •Anomalies, Malformations
- •Aplasia, Hypoplasia
- •Cystic Malformation
- •Anomalies of Number, Position, or Rotation
- •Fusion Anomaly
- •Anomalies of the Renal Calices
- •Vascular Anomaly
- •Diffuse Changes
- •Large Kidneys
- •Small Kidneys
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Irregular Structure
- •Circumscribed Changes
- •Anechoic Structure
- •Hypoechoic or Isoechoic Structure
- •Complex Structure
- •Hyperechoic Structure
- •10 Adrenal Glands
- •Enlargement
- •Anechoic Structure
- •Hypoechoic Structure
- •Complex Echo Structure
- •Hyperechoic Structure
- •11 Urinary Tract
- •Malformations
- •Duplication Anomalies
- •Dilatations and Stenoses
- •Dilated Renal Pelvis and Ureter
- •Anechoic
- •Hypoechoic
- •Hypoechoic
- •Hyperechoic
- •Large Bladder
- •Small Bladder
- •Altered Bladder Shape
- •Intracavitary Mass
- •Hypoechoic
- •Hyperechoic
- •Echogenic
- •Wall Changes
- •Diffuse Wall Thickening
- •Circumscribed Wall Thickening
- •Concavities and Convexities
- •12.1 The Prostate
- •Enlarged Prostate
- •Regular
- •Irregular
- •Small Prostate
- •Regular
- •Echogenic
- •Circumscribed Lesion
- •Anechoic
- •Hypoechoic
- •Echogenic
- •12.2 Seminal Vesicles
- •Diffuse Change
- •Hypoechoic
- •Circumscribed Change
- •Anechoic
- •Echogenic
- •Irregular
- •12.3 Testis, Epididymis
- •Diffuse Change
- •Enlargement
- •Decreased Size
- •Circumscribed Lesion
- •Anechoic or Hypoechoic
- •Irregular/Echogenic
- •Epididymal Lesion
- •Anechoic
- •Hypoechoic
- •Intrascrotal Mass
- •Anechoic or Hypoechoic
- •Echogenic
- •13 Female Genital Tract
- •Masses
- •Abnormalities of Size or Shape
- •Uterus
- •Abnormalities of Size or Shape
- •Myometrial Changes
- •Intracavitary Changes
- •Endometrial Changes
- •Fallopian Tubes
- •Hypoechoic Mass
- •Anechoic Cystic Mass
- •Solid Echogenic or Nonhomogeneous Mass
- •14 Thyroid Gland
- •Diffuse Changes
- •Enlarged Thyroid Gland
- •Small Thyroid Gland
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Circumscribed Changes
- •Anechoic
- •Hypoechoic
- •Isoechoic
- •Hyperechoic
- •Irregular
- •Differential Diagnosis of Hyperthyroidism
- •Types of Autonomy
- •15 Pleura and Chest Wall
- •Chest Wall
- •Masses
- •Parietal Pleura
- •Nodular Masses
- •Diffuse Pleural Thickening
- •Pleural Effusion
- •Anechoic Effusion
- •Echogenic Effusion
- •Complex Effusion
- •16 Lung
- •Masses
- •Anechoic Masses
- •Hypoechoic Masses
- •Complex Masses
- •Index

4
Pancreas
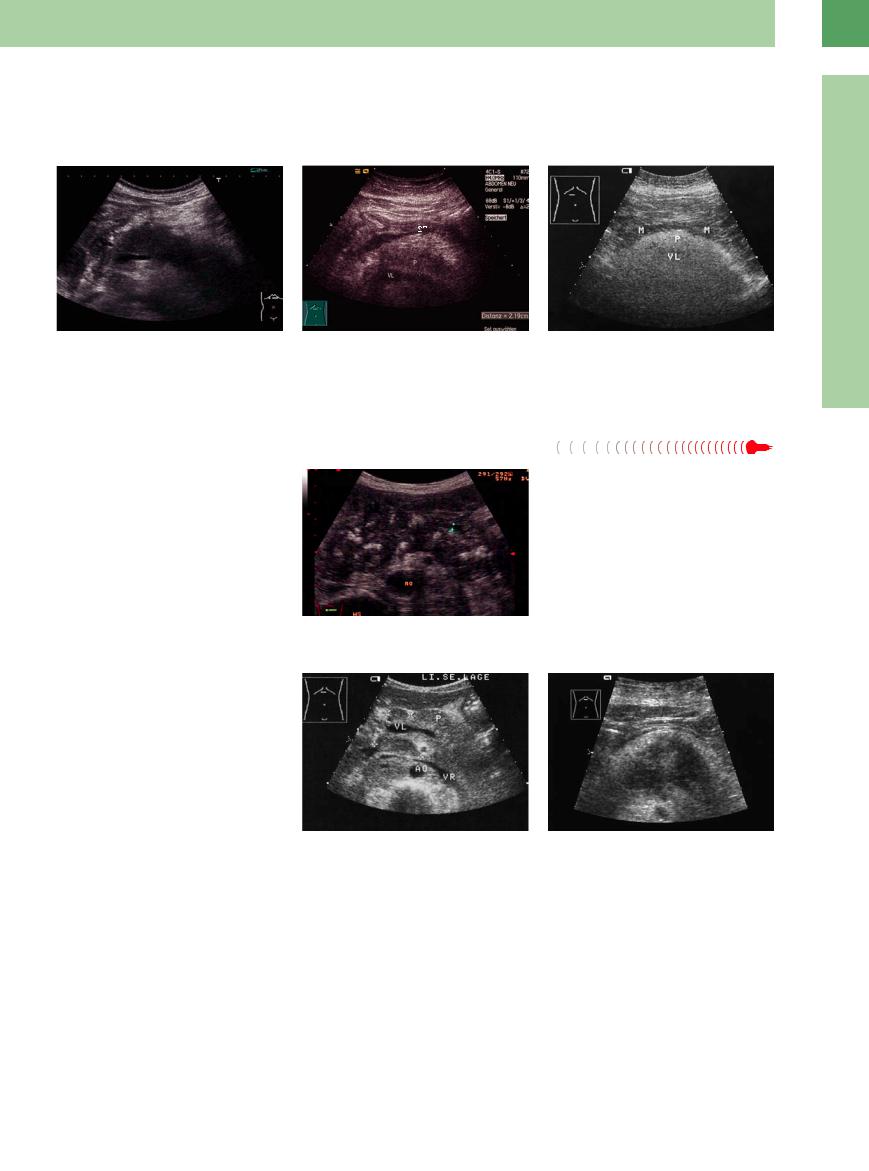
Fig. 4.2 Schematic diagram of the relationships of the pancreas.
Fig. 4.4 The tail of the pancreas (P), anterior to the splenic vein (VL), reaches the hilum of the spleen (M); high lateral view.
nancy these lymph nodes quite often harbor metastases, which are demonstrable in sonographic imaging. Regional lymph node meta-
measures, are not in themselves absolutely signs of inoperability; see below.
Fig. 4.3 Ultrasound topography of the pancreas and the relationships with its neighboring organs.
a Oblique right epigastric view: the head of the pancreas
(P) is lateral and posterior to the gallbladder (GB), posterior to the right hepatic lobe, and anterior to the vena cava (VC). AO = aorta; K = venous confluence.
b Median transverse epigastric view: the median regions of the right and left hepatic lobes are visualized from anterior to posterior; the splenic vein (VL) lies at the inferior border of the pancreas (P), followed by crosssectional views of the superior mesenteric artery, vena cava (VC), and aorta (AO). AL = splenic artery.
c Left oblique epigastric view: demonstration of the entire tail of the pancreas (P) posterior to the left hepatic lobe (L); the splenic artery (AL, Fig. 4.3b) meanders through the pancreatic tail.
■ Diffuse Pancreatic Change
In ultrasonography, diffuse pancreatic change will alter the size and echo texture of the organ.
Large Pancreas
Pancreas

Diffuse Pancreatic Change
Large Pancreas
Small Pancreas
Hypoechoic Texture
Hyperechoic Texture
Focal Changes
Dilatation of the Pancreatic Duct
Acute Pancreatitis
Chronic Pancreatitis
Tumor Invasion
Acute Pancreatitis


















































Pancreatic edema. Acute pancreatitis will usu- |
interstitial edema, which in turn decreases the |
ally lead to diffuse enlargement of the entire |
echogenicity. Increased size and hypoechoge- |
pancreas; however, in most cases of concurrent |
nicity are the most striking characteristics of |
pancreatitis the standard dimensions will not |
mild episodes of acute pancreatitis (Fig. 4.5). |
be exceeded. The increase in size is caused by |
Subsiding edema is followed by a return to |
normal size and echogenicity. However, even after months there may be residual spiculation of the organ contour.
170
Necrosis of the peripancreatic fat. In severe |
gland, thus resulting in a pseudo-enlargement |
and therefore may also mimic enlargement of |
cases of acute necrotizing pancreatitis, focal |
of the organ (Fig. 4.6). |
the gland (Fig. 4.7). |
masses, such as intrapancreatic and peri- |
Extensive peripancreatic fatty infiltration in |
|
pancreatic fluid, fatty necrosis, hemorrhage, |
obesity and diabetes may blur the contours of |
|
and exudate, may hamper delineation of the |
the pancreas by beam scattering and reflection, |
|
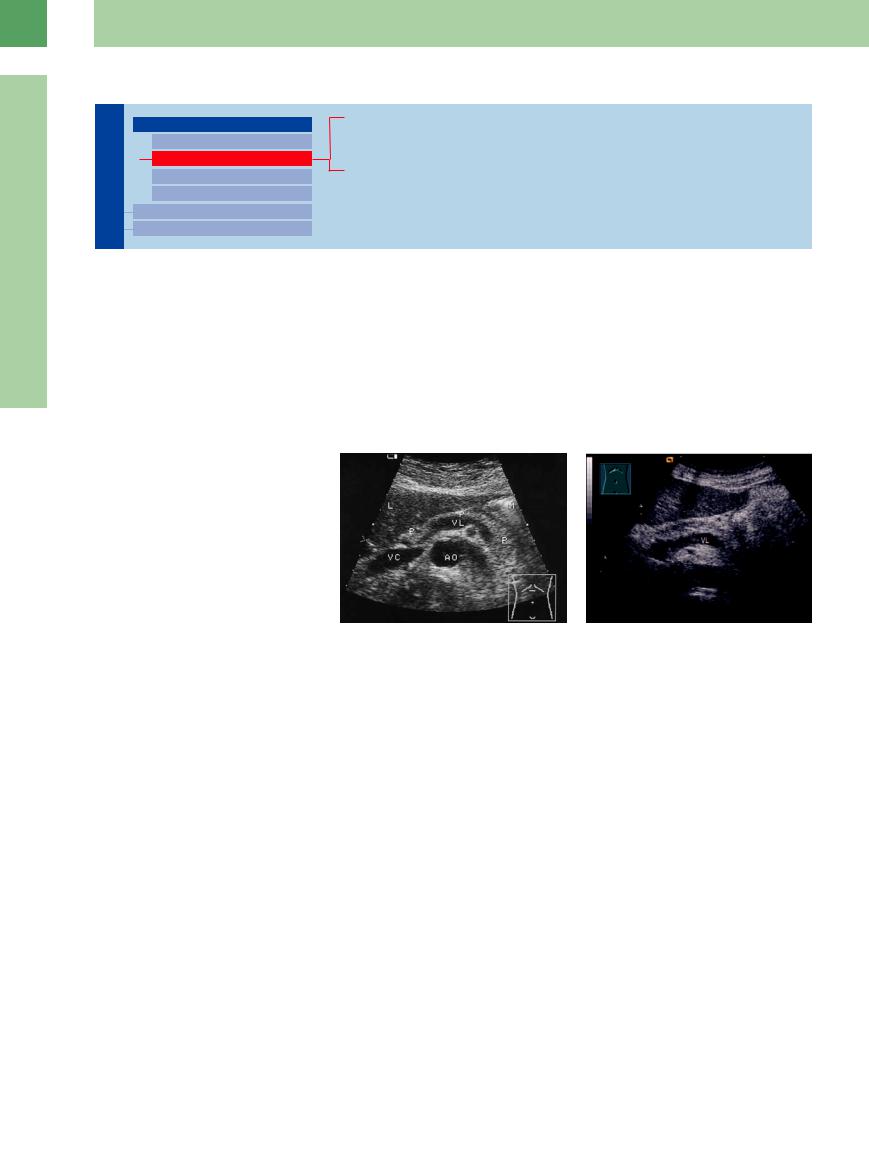
Fig. 4.5 Acute edematous pancreatitis : diffusely enlarged |
Fig. 4.6 Acute pancreatitis: apparent enlargement by |
Fig. 4.7 Apparent enlargement of the pancreas (P) be- |
pancreas; blurred hypoechoic texture. VL = splenic vein. |
echogenic peripancreatic areas (fat necrosis, hemorrha- |
cause intensive scattering (fibromatosis/lipomatosis, peri- |
|
gic areas), which indent the posterior stomach (ST). The |
pancreatic fat) makes delineation by ultrasound impossi- |
|
pancreas (P) is slightly enlarged up to 2.1 cm and has a |
ble; splenic vein (VL) just barely visualized. M = stomach. |
|
hazy, hypoechoic structure. VL = splenic vein. |
|
Chronic Pancreatitis


























Particularly in the early stages, an acute inflammatory episode of chronic pancreatitis will result in an enlarged pancreas. But in this case texture and contour will tend to undergo mottled, ill-defined, or irregular hyperechoic transformation (Fig. 4.8).
Fig. 4.8 Chronic alcohol-associated pancreatitis: distinctive enlargement, calcification with shadowing. Cursors: slightly dilated pancreatic duct. AO = aorta, WS = vertebral column.
Tumor Invasion 



















































In the rather rare case of diffuse carcinoma or in malignant tumor invasion, enlargement of the gland and misdiagnosis may also be encountered (Fig. 4.9). The echo pattern may be isoechoic or hypoechoic (see Fig. 4.36).
Fig. 4.9 |
b Diffusely growing ductal pancreatic carcinoma, en- |
a Confluent intrapancreatic and peripancreatic lympho- |
larged organ, supposed infiltration of the splenic vein. |
mas (calipers), resulting in enlargement of the pancreas |
|
(P) anterior and posterior to the splenic vein (VL). AO = |
|
aorta; VR = renal vein. |
|
4
Diffuse Pancreatic Change
171
4
Pancreas
Pancreas

Diffuse Pancreatic Change
Large Pancreas
Small Pancreas
Hypoechoic Texture
Hyperechoic Texture
Focal Changes
Dilatation of the Pancreatic Duct
The Aging Pancreas
Pancreatic Atrophy
Post-pancreatic Necrosis/Pancreatectomy
sion. Nevertheless, a thickness of less than 10 mm in the pancreatic head, body, or tail would suggest a smaller than normal size. If the reduced thickness is segmental, it may be simply a physiological variant (see Fig. 4.1).
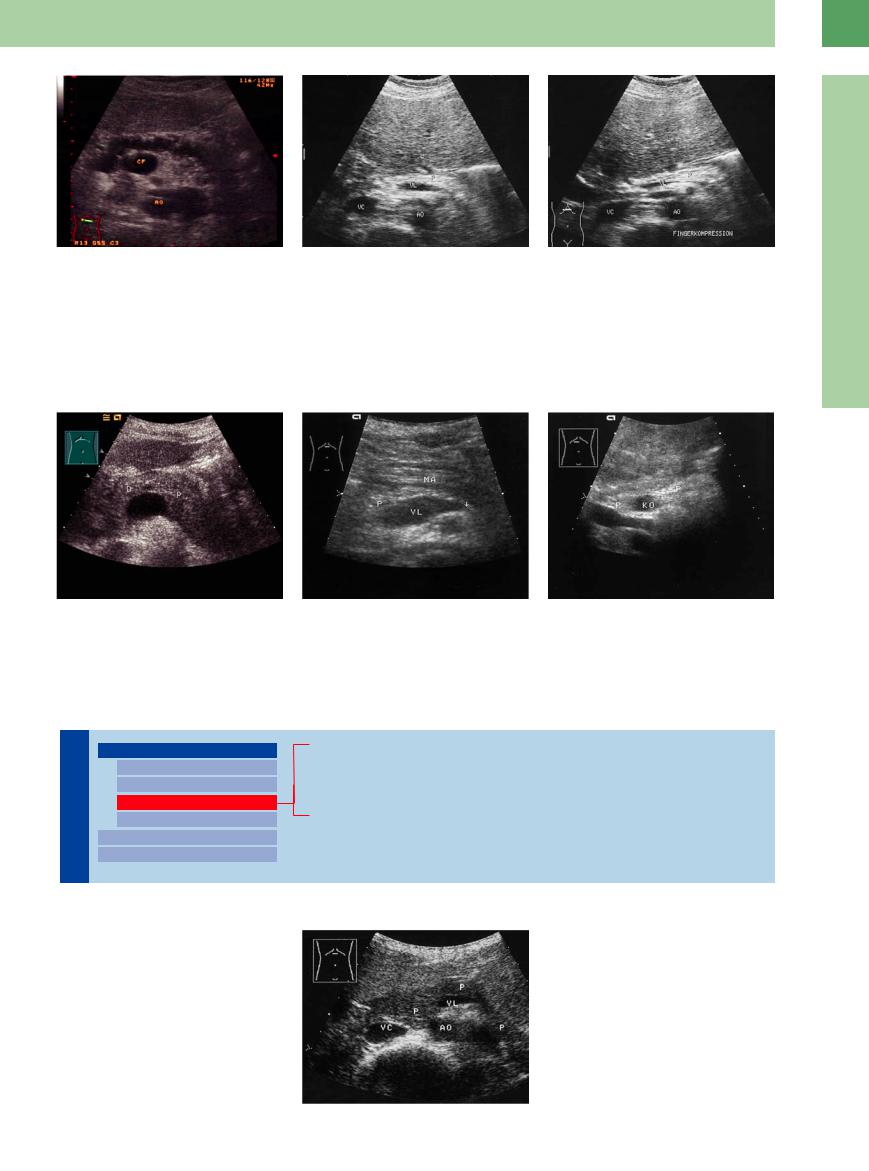
The Aging Pancreas

















































The most common cause of a smaller than normal pancreas is age-dependent atrophy, which is quite common in slim, elderly patients. It affects all parts of the organ evenly. Echogenicity may be normal or increased. Any hypergenicity is due to parenchyma being replaced by fatty and connective tissue (fibrolipomatosis). In cachectic patients problems in differential diagnosis arise if tubular structures are very closely related, making orientation rather difficult (splenic artery and vein; dilated pancreatic duct/common hepatic artery/renal vein; CBD/portal vein/proper hepatic artery). In this case, color-flow Doppler scanning (CDS) will differentiate the various vessels and facilitate visualization of the narrow pancreatic parenchyma (Fig. 4.10).
Fig. 4.10
a Pancreas in old age: narrowed pancreas (P), normal texture. VL = splenic vein; AO = aorta; VC = vena cava; L = liver; M = gastric body.
b Pancreatic atrophy in autoimmune pancreatitis.
Pancreatic  Atrophy
Atrophy 

















































Differentiation of atrophy in chronic pancreatitis from aging pancreas is possible only if there are changes in the texture or in case of ductal dilatation. Pancreatic atrophy is the terminal stage of chronic pancreatitis and may still exhibit the ultrasound criteria of this disease, i. e., calcification and fibrosis. Scarring will often warp the duct and dilate it irregularly, and it may be the only vestige of the gland.
Pancreatic atrophy as a sequel to chronic pancreatitis or chronic autoimmune pancreatitis (Fig. 4.10b) implies diabetes and maldigestion. Also pancreatic head cancer with atrophy of the pancreatic body and tail will lead to diabetes mellitus and maldigestion. Newly diagnosed diabetes mellitus or unexplained weight loss may be the only clinical symptoms. Early signs in ultrasound morphology might be
localized or diffuse hypoechogenicity without the other signs of chronic pancreatitis (Fig. 4.11, Fig. 4.66a,b, Fig. 4.67a–c).1,2
Hemochromatosis. In atrophy concomitant with advanced hemochromatosis, the fibrosis may lead to diffuse or focal hyperechogenicity of the pancreas (Fig. 4.12).
172
4
Fig. 4.11 Atrophy resulting from “burnt-out” chronic pancreatitis: only a narrow band of hyperechoic parenchyma and irregularly defined dilated pancreatic duct with small echoic contents. CF = venous confluence; AO = aorta.
Fig. 4.12 Fibrosis of the pancreas (P) with diabetes mellitus in hemochromatosis. VL = splenic vein; AO = aorta; VC = vena cava; L = liver.
a Narrow hyperechoic organ.
Diffuse Pancreatic Change
b In contrast to lipomatosis, here the pancreas cannot be compressed by the palpating fingers. Fingerkompression = finger compression.
Post-pancreatitic Necrosis/Pancreatectomy 




































After necrosis and partial resection of the pancreas, as well as after total pancreatectomy, it is almost impossible to differentiate sonographi-
cally between the peripancreatic fat/connective tissue and the residual pancreatic tissue because they hardly differ in impedance
(Fig. 4.13). In these cases, differential diagnosis has to fall back on patient history and clinical symptoms.
Fig. 4.13
a Resection of the pancreatic head following chronic pancreatitis: lack of parts of the pancreatic head (arrows). The small bowel loop (D) fixed to the pancreatic body (arrow) simulates a normal pancreas.
b Resection of the pancreatic tail, relapsing pancreatitis, lacking pancreatic tail and in parts (arrow, VL) splenic vein. P = pancreatic head, MA = stomach.
c Subtotal pancreatic necrosis after acute, severe pancreatitis: while the pancreatic head (P) is still preserved, the body and tail are almost completely missing. KO = venous confluence.
Hypoechoic Texture
|
|
|
Diffuse Pancreatic Change |
|||
Pancreas |
||||||
|
|
Hypoechoic Texture |
||||
|
|
|
|
|
Large Pancreas |
|
|
|
|
|
|
||
|
|
|
|
|
Small Pancreas |
|
|
|
|
|
|
||
|
|
|
|
|
Hyperechoic Texture |
|
|
|
|
|
|
||
|
|
|
|
|
||
|
|
|
|
|
||
|
|
|
Focal Changes |
|||
|
|
|
||||
|
|
|
|
|
||
|
|
|
Dilatation of the Pancreatic Duct |
|||
|
|
|
||||
Juvenile Pancreas
Acute Pancreatitis
Early/Recurrent Chronic Pancreatitis
Autoimmune Pancreatitis
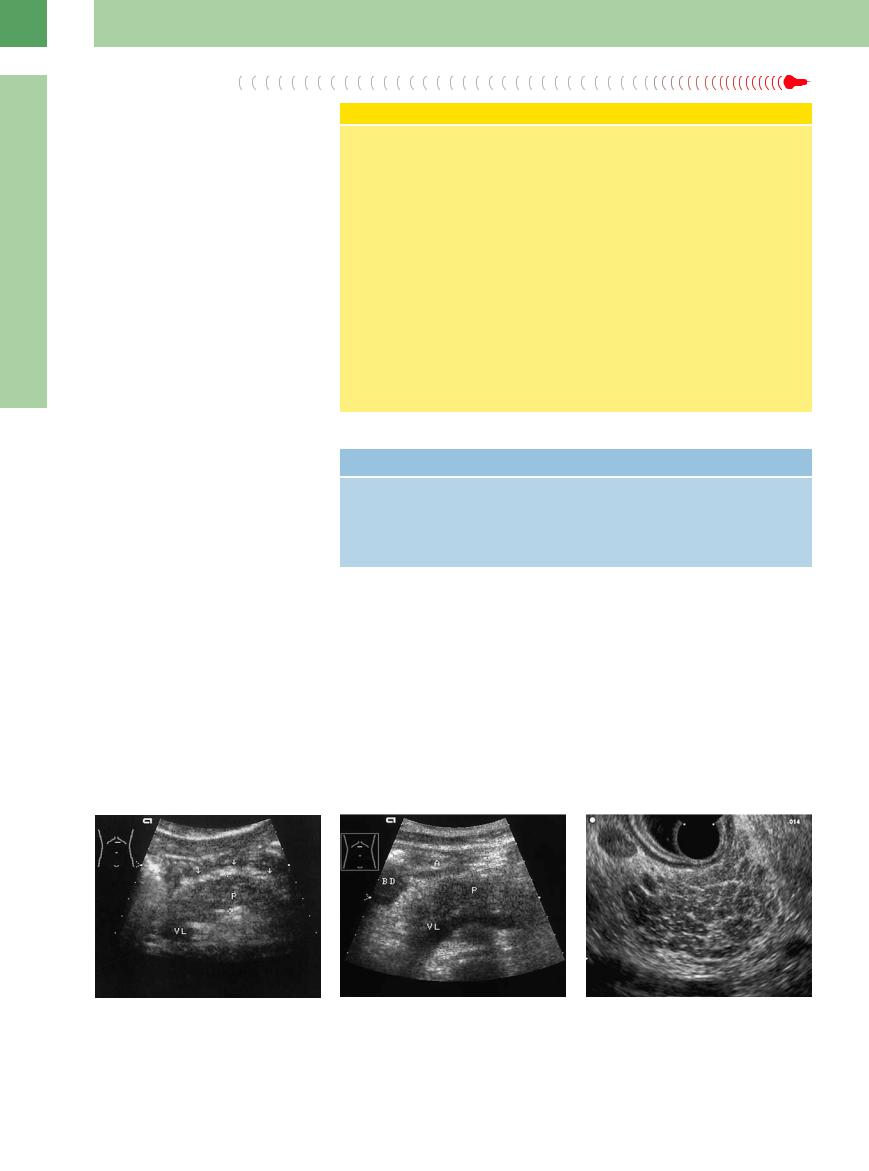
Juvenile Pancreas 


















































Quite often, the juvenile pancreas will be exceptionally hypoechoic and might be mistaken for edematous pancreas in acute pancreatitis, although the “juvenile organ” will demonstrate normal size (Fig. 4.14).
Fig. 4.14 Juvenile pancreas in a slender female: compared with acute pancreatitis the pancreas (P) is markedly hypoechoic but with unchanged dimensions in all segments. AO = aorta; VC = vena cava; VL = splenic vein.
173
4
Pancreas
enlargement of the organ, which is characterized by intensive homogeneous hypoechoic transformation of its texture. These changes correspond to the histological finding of pancreatic edema.
Necrosis of the peripancreatic fat may result in the common ultrasonographic finding of band-shaped hyperechoic peripancreatic masses (Figs. 4.5, 4.6, 4.15).
In addition there also may be fluid collections around the pancreas, liver, and kidney/ spleen, while a large exudate tends to be present in the more severe form (Table 4.1). Compression-induced dilatation of the pancreatic duct is uncommon and would indicate pancreas divisum or periampullary ductal obstruction (prepapillary gallstone).
On the basis of the ultrasound findings, the differential diagnosis should consider the early stage of chronic or recurrent chronic pancreatitis (Fig. 4.15, Fig. 4.16) or even the rarer case of a hypoechoic juvenile pancreas (Fig. 4.14).
International Classification of Acute Pancreatitis (2012)3
The new international classification is |
● Mild acute pancreatitis is characterized |
|
based on the actual local and systemic |
by the absence of both (peri)pancreatic |
|
determinants of severity. The local deter- |
necrosis and organ failure. |
|
minant relates to whether there is (peri)- |
● Moderate acute pancreatitis is character- |
|
pancreatic necrosis or not and, if present, |
ized by the presence of sterile (peri)- |
|
whether it is sterile or infected. |
pancreatic necrosis and/or transient or- |
|
● Sterile (peri)pancreatic necrosis is the ab- |
gan failure. |
|
sence of proven infection in necrosis. |
● Severe acute pancreatitis is characterized |
|
● Infected (peri)pancreatic necrosis is de- |
by the presence of either infected (peri)- |
|
fined when at least one of the following |
pancreatic necrosis or persistent organ |
|
is present: |
failure. |
|
– |
Gas bubbles within (peri)pancreatic |
● Critical acute pancreatitis is characterized |
|
necrosis |
by the presence of infected (peri)- |
– |
A positive culture of (peri)pancreatic |
pancreatic necrosis and persistent organ |
|
necrosis obtained by image-guided |
failure. |
|
fine-needle aspiration |
|
–A positive culture of (peri)pancreatic necrosis obtained during the first drainage and/or necrosectomy
Table 4.1 Diagnostic ultrasound criteria in acute pancreatitis
Mild pancreatitis |
Severe pancreatitis |
● Enlarged organ (leading sign) |
In addition to the mild form: |
● Blurred hypoechoic texture |
● Focal hypo-/hyperechoic intraand extra- |
● Regular size and texture in “concurrent” |
pancreatic mass (hemorrhage/necrosis/ |
pancreatitis |
fatty necrosis) |
● Heterogeneous texture possible |
● Ascites, pleural e usion |
Early/Recurrent Chronic Pancreatitis
Pancreatitis








































Chronic pancreatitis is characterized by hyper- |
chronic pancreatitis from malignancy or other |
i. e., irregular contour, undulating duct, or in- |
echoic fibrosis and calcification as well as an- |
forms of fibrosis, or even acute pancreatitis, |
terspersed fibrotic regions. Early chronic pan- |
echoic/hypoechoic microcysts and macrocysts |
becomes difficult. Particularly in alcohol-asso- |
creatitis frequently shows a “pitted” texture in |
and ductal dilatation. If all signs are present, |
ciated pancreatitis, the texture may become |
endoscopic ultrasound (EUS) (Figs. 4.15, |
the diagnosis is confirmed. In the presence of |
hypoechoic; however, on detailed study it dis- |
Fig. 4.16). |
just one or two criteria, differentiation of |
plays the characteristics of chronic pancreatitis, |
|
Fig. 4.15 |
b Acute pancreatitis in regression, still hypoechoic organ |
c Early stage of chronic pancreatitis, EUS, pitted tex- |
a Late stage of acute pancreatitis: hypoechoic pancreas |
(P) with undulating limitation. VL = splenic vein; A = |
ture.10 |
(P), peripancreatic hyperechoic mass (arrows). VL = |
antrum; BD = duodenal bulb. |
|
splenic vein. |
|
|
174
