
- •Contents
- •Preface
- •Contributors
- •1 Vessels
- •1.1 Aorta, Vena Cava, and Peripheral Vessels
- •Aorta, Arteries
- •Anomalies and Variant Positions
- •Dilatation
- •Stenosis
- •Wall Thickening
- •Intraluminal Mass
- •Perivascular Mass
- •Vena Cava, Veins
- •Anomalies
- •Dilatation
- •Intraluminal Mass
- •Compression, Infiltration
- •1.2 Portal Vein and Its Tributaries
- •Enlarged Lumen Diameter
- •Portal Hypertension
- •Intraluminal Mass
- •Thrombosis
- •Tumor
- •2 Liver
- •Enlarged Liver
- •Small Liver
- •Homogeneous Hypoechoic Texture
- •Homogeneous Hyperechoic Texture
- •Regionally Inhomogeneous Texture
- •Diffuse Inhomogeneous Texture
- •Anechoic Masses
- •Hypoechoic Masses
- •Isoechoic Masses
- •Hyperechoic Masses
- •Echogenic Masses
- •Irregular Masses
- •Differential Diagnosis of Focal Lesions
- •Diagnostic Methods
- •Suspected Diagnosis
- •3 Biliary Tree and Gallbladder
- •3.1 Biliary Tree
- •Thickening of the Bile Duct Wall
- •Localized and Diffuse
- •Bile Duct Rarefaction
- •Localized and Diffuse
- •Bile Duct Dilatation and Intraductal Pressure
- •Intrahepatic
- •Hilar and Prepancreatic
- •Intrapancreatic
- •Papillary
- •Abnormal Intraluminal Bile Duct Findings
- •Foreign Body
- •The Seven Most Important Questions
- •3.2 Gallbladder
- •Changes in Size
- •Large Gallbladder
- •Small/Missing Gallbladder
- •Wall Changes
- •General Hypoechogenicity
- •General Hyperechogenicity
- •General Tumor
- •Focal Tumor
- •Intraluminal Changes
- •Hyperechoic
- •Hypoechoic
- •Nonvisualized Gallbladder
- •Missing Gallbladder
- •Obscured Gallbladder
- •4 Pancreas
- •Diffuse Pancreatic Change
- •Large Pancreas
- •Small Pancreas
- •Hypoechoic Texture
- •Hyperechoic Texture
- •Focal Changes
- •Anechoic Lesion
- •Hypoechoic Lesion
- •Isoechoic Lesion
- •Hyperechoic Lesion
- •Irregular (Complex Structured) Lesion
- •Dilatation of the Pancreatic Duct
- •Marginal/Mild Dilatation
- •Marked Dilatation
- •5 Spleen
- •Nonfocal Changes of the Spleen
- •Diffuse Parenchymal Changes
- •Large Spleen
- •Small Spleen
- •Focal Changes of the Spleen
- •Anechoic Mass
- •Hypoechoic Mass
- •Hyperechoic Mass
- •Splenic Calcification
- •6 Lymph Nodes
- •Peripheral Lymph Nodes
- •Head/Neck
- •Extremities (Axilla, Groin)
- •Abdominal Lymph Nodes
- •Porta Hepatis
- •Splenic Hilum
- •Mesentery (Celiac, Upper and Lower Mesenteric Station)
- •Stomach
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •Small/Large Intestine
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •8 Peritoneal Cavity
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Wall Structures
- •Smooth Margin
- •Irregular Margin
- •Intragastric Processes
- •Intraintestinal Processes
- •9 Kidneys
- •Anomalies, Malformations
- •Aplasia, Hypoplasia
- •Cystic Malformation
- •Anomalies of Number, Position, or Rotation
- •Fusion Anomaly
- •Anomalies of the Renal Calices
- •Vascular Anomaly
- •Diffuse Changes
- •Large Kidneys
- •Small Kidneys
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Irregular Structure
- •Circumscribed Changes
- •Anechoic Structure
- •Hypoechoic or Isoechoic Structure
- •Complex Structure
- •Hyperechoic Structure
- •10 Adrenal Glands
- •Enlargement
- •Anechoic Structure
- •Hypoechoic Structure
- •Complex Echo Structure
- •Hyperechoic Structure
- •11 Urinary Tract
- •Malformations
- •Duplication Anomalies
- •Dilatations and Stenoses
- •Dilated Renal Pelvis and Ureter
- •Anechoic
- •Hypoechoic
- •Hypoechoic
- •Hyperechoic
- •Large Bladder
- •Small Bladder
- •Altered Bladder Shape
- •Intracavitary Mass
- •Hypoechoic
- •Hyperechoic
- •Echogenic
- •Wall Changes
- •Diffuse Wall Thickening
- •Circumscribed Wall Thickening
- •Concavities and Convexities
- •12.1 The Prostate
- •Enlarged Prostate
- •Regular
- •Irregular
- •Small Prostate
- •Regular
- •Echogenic
- •Circumscribed Lesion
- •Anechoic
- •Hypoechoic
- •Echogenic
- •12.2 Seminal Vesicles
- •Diffuse Change
- •Hypoechoic
- •Circumscribed Change
- •Anechoic
- •Echogenic
- •Irregular
- •12.3 Testis, Epididymis
- •Diffuse Change
- •Enlargement
- •Decreased Size
- •Circumscribed Lesion
- •Anechoic or Hypoechoic
- •Irregular/Echogenic
- •Epididymal Lesion
- •Anechoic
- •Hypoechoic
- •Intrascrotal Mass
- •Anechoic or Hypoechoic
- •Echogenic
- •13 Female Genital Tract
- •Masses
- •Abnormalities of Size or Shape
- •Uterus
- •Abnormalities of Size or Shape
- •Myometrial Changes
- •Intracavitary Changes
- •Endometrial Changes
- •Fallopian Tubes
- •Hypoechoic Mass
- •Anechoic Cystic Mass
- •Solid Echogenic or Nonhomogeneous Mass
- •14 Thyroid Gland
- •Diffuse Changes
- •Enlarged Thyroid Gland
- •Small Thyroid Gland
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Circumscribed Changes
- •Anechoic
- •Hypoechoic
- •Isoechoic
- •Hyperechoic
- •Irregular
- •Differential Diagnosis of Hyperthyroidism
- •Types of Autonomy
- •15 Pleura and Chest Wall
- •Chest Wall
- •Masses
- •Parietal Pleura
- •Nodular Masses
- •Diffuse Pleural Thickening
- •Pleural Effusion
- •Anechoic Effusion
- •Echogenic Effusion
- •Complex Effusion
- •16 Lung
- •Masses
- •Anechoic Masses
- •Hypoechoic Masses
- •Complex Masses
- •Index
12Prostate, Seminal Vesicles, Testis, Epididymis
G. Schmidt
Prostatic changes. Diseases of the prostate consist of inflammatory changes (prostatitis), hyperplasias, and neoplasias. Inflammatory changes are most common in young men, while hyperplasia and carcinoma are typical diseases of aging. The incidence of prostatic carcinoma rises with aging. Its peak age incidence is the highest of all malignancies, between the seventh and eighth decades. As a result, prostate cancer has become the leading cause of death in men over age 55. Benign prostatic hyperplasia (BPH), which involves a nodular transformation of the gland, is based on a hormonal disorder.
Hyperplasia predominantly affects the upper central portion of the gland, whereas carcinoma tends to arise in the lower periph-
eral zone.1 This is important sonographically because focal lesions located in the median lobe of the prostate generally represent hyperplasia, while cancers are typically located in the periphery of the gland. When it comes to differentiating between benign and malignant prostatic lesions, transabdominal ultrasound is less rewarding than transurethral and transrectal scanning (which are not described here but may be found in the specialized urological literature). Transabdominal scanning is of unquestioned value in assessing the size of the enlarged prostate and in the general detection of pathomorphological changes. Besides enlargement and structural abnormalities, ultrasound can demonstrate fibrotic areas, calcifications, and cysts.
Seminal vesicle changes. The seminal vesicles are paired glands that secret fluid necessary for the transport and nutrition of the sperm. The seminal vesicles can be filled (normal status, as in Fig.12.3b, or empty after ejaculation). Primary diseases of the seminal vesicle are extremely rare, but the gland is commonly involved by diseases spreading from adjacent organs (e. g., invasion by prostatic tumor). Cystic dilatations and calcifications are occasionally noted on ultrasound examination.
Testicular changes. The location of the testes makes them easily accessible to ultrasound scanning. As a result, sonography is the modality of choice for investigating inflammatory changes and masses.
12.1 The Prostate
Anatomy and Topography
and Topography 













































Structure
●Gross anatomy: right lobe, left lobe, median lobe (posterior, superior)
●Zonal anatomy: periurethral zone, inner zone, outer zone with capsule
Relations
●Superior: bladder trigone and ureteral orifices
●Posterosuperior: seminal vesicles
●Inferior: corpora cavernosa
●Posterior: rectum
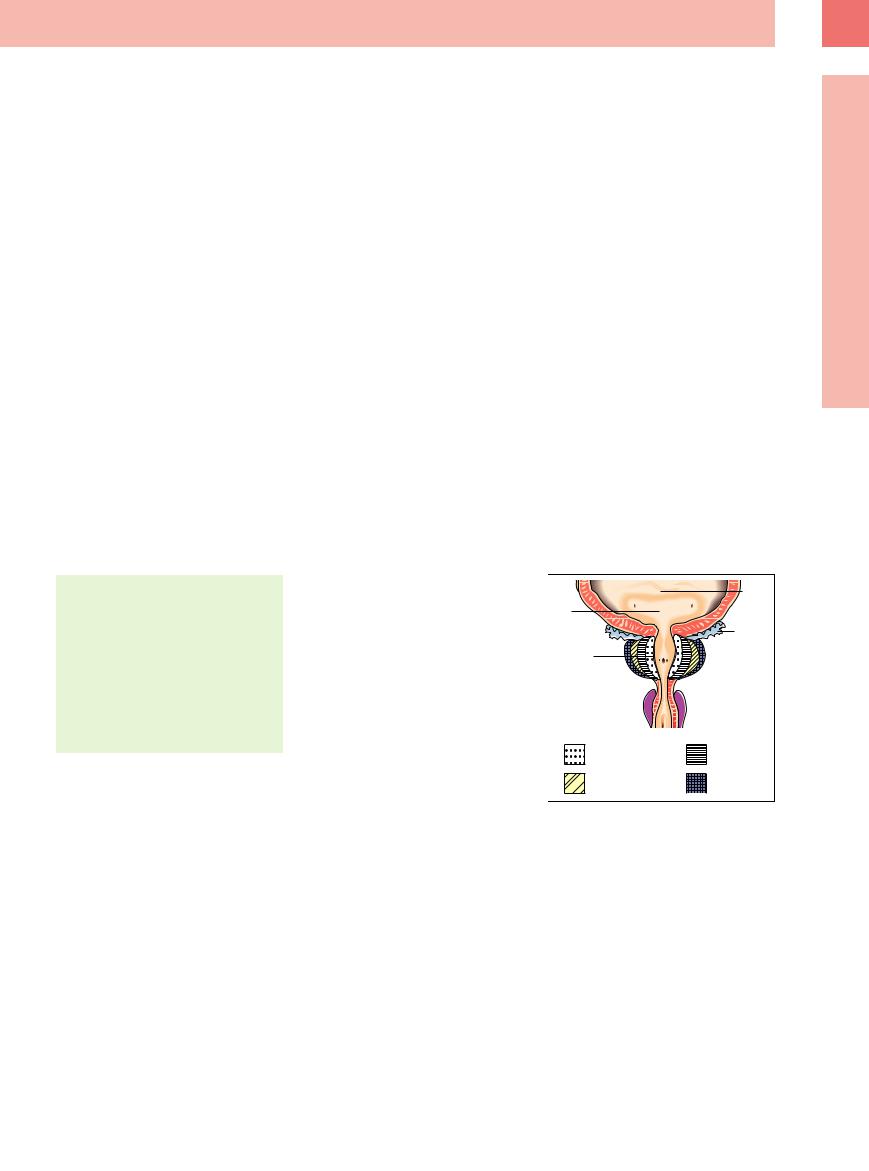
The prostate lies against the posterior bladder floor and can be clearly visualized by placing the transducer over the distended bladder and angling the scan plane caudally (Fig.12.2). The paired seminal vesicles are found posteriorly between the bladder floor and prostate (see below). The urethra runs from the funnelshaped urethral orifice through the center of the prostate, defining a periurethral zone that can be distinguished from the inner and outer zones (Fig.12.1).
This is of key importance in sonography, because it is primarily the stroma (smooth muscle) and glandular tissue in the periurethral and inner zones (transitional zone) of the posterosuperior median lobe that are susceptible to hyperplasia. The remaining portions of the gland are compressed by the hyperplas- tic tissue, forming an apparent capsule called the “surgical capsule.” Carcinomas, on the other hand, generally arise in the predominantly glandular outer zone. These zones of predilection in the prostate aid the examiner in differentiating between carcinoma and hyperplasia. Special attention is given to the prostatic capsule surrounding the outer zone in the evaluation of transcapsular tumor spread.
Fig. 12.1 Coronal section through the prostate, demon- strating the zones of the prostate, the bladder trigone with the ureteral orifices, and the seminal vesicles posterior to the prostate.
12
Prostate, Seminal Vesicles, Testis, Epididymis
417
