
- •Contents
- •Preface
- •Contributors
- •1 Vessels
- •1.1 Aorta, Vena Cava, and Peripheral Vessels
- •Aorta, Arteries
- •Anomalies and Variant Positions
- •Dilatation
- •Stenosis
- •Wall Thickening
- •Intraluminal Mass
- •Perivascular Mass
- •Vena Cava, Veins
- •Anomalies
- •Dilatation
- •Intraluminal Mass
- •Compression, Infiltration
- •1.2 Portal Vein and Its Tributaries
- •Enlarged Lumen Diameter
- •Portal Hypertension
- •Intraluminal Mass
- •Thrombosis
- •Tumor
- •2 Liver
- •Enlarged Liver
- •Small Liver
- •Homogeneous Hypoechoic Texture
- •Homogeneous Hyperechoic Texture
- •Regionally Inhomogeneous Texture
- •Diffuse Inhomogeneous Texture
- •Anechoic Masses
- •Hypoechoic Masses
- •Isoechoic Masses
- •Hyperechoic Masses
- •Echogenic Masses
- •Irregular Masses
- •Differential Diagnosis of Focal Lesions
- •Diagnostic Methods
- •Suspected Diagnosis
- •3 Biliary Tree and Gallbladder
- •3.1 Biliary Tree
- •Thickening of the Bile Duct Wall
- •Localized and Diffuse
- •Bile Duct Rarefaction
- •Localized and Diffuse
- •Bile Duct Dilatation and Intraductal Pressure
- •Intrahepatic
- •Hilar and Prepancreatic
- •Intrapancreatic
- •Papillary
- •Abnormal Intraluminal Bile Duct Findings
- •Foreign Body
- •The Seven Most Important Questions
- •3.2 Gallbladder
- •Changes in Size
- •Large Gallbladder
- •Small/Missing Gallbladder
- •Wall Changes
- •General Hypoechogenicity
- •General Hyperechogenicity
- •General Tumor
- •Focal Tumor
- •Intraluminal Changes
- •Hyperechoic
- •Hypoechoic
- •Nonvisualized Gallbladder
- •Missing Gallbladder
- •Obscured Gallbladder
- •4 Pancreas
- •Diffuse Pancreatic Change
- •Large Pancreas
- •Small Pancreas
- •Hypoechoic Texture
- •Hyperechoic Texture
- •Focal Changes
- •Anechoic Lesion
- •Hypoechoic Lesion
- •Isoechoic Lesion
- •Hyperechoic Lesion
- •Irregular (Complex Structured) Lesion
- •Dilatation of the Pancreatic Duct
- •Marginal/Mild Dilatation
- •Marked Dilatation
- •5 Spleen
- •Nonfocal Changes of the Spleen
- •Diffuse Parenchymal Changes
- •Large Spleen
- •Small Spleen
- •Focal Changes of the Spleen
- •Anechoic Mass
- •Hypoechoic Mass
- •Hyperechoic Mass
- •Splenic Calcification
- •6 Lymph Nodes
- •Peripheral Lymph Nodes
- •Head/Neck
- •Extremities (Axilla, Groin)
- •Abdominal Lymph Nodes
- •Porta Hepatis
- •Splenic Hilum
- •Mesentery (Celiac, Upper and Lower Mesenteric Station)
- •Stomach
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •Small/Large Intestine
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •8 Peritoneal Cavity
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Wall Structures
- •Smooth Margin
- •Irregular Margin
- •Intragastric Processes
- •Intraintestinal Processes
- •9 Kidneys
- •Anomalies, Malformations
- •Aplasia, Hypoplasia
- •Cystic Malformation
- •Anomalies of Number, Position, or Rotation
- •Fusion Anomaly
- •Anomalies of the Renal Calices
- •Vascular Anomaly
- •Diffuse Changes
- •Large Kidneys
- •Small Kidneys
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Irregular Structure
- •Circumscribed Changes
- •Anechoic Structure
- •Hypoechoic or Isoechoic Structure
- •Complex Structure
- •Hyperechoic Structure
- •10 Adrenal Glands
- •Enlargement
- •Anechoic Structure
- •Hypoechoic Structure
- •Complex Echo Structure
- •Hyperechoic Structure
- •11 Urinary Tract
- •Malformations
- •Duplication Anomalies
- •Dilatations and Stenoses
- •Dilated Renal Pelvis and Ureter
- •Anechoic
- •Hypoechoic
- •Hypoechoic
- •Hyperechoic
- •Large Bladder
- •Small Bladder
- •Altered Bladder Shape
- •Intracavitary Mass
- •Hypoechoic
- •Hyperechoic
- •Echogenic
- •Wall Changes
- •Diffuse Wall Thickening
- •Circumscribed Wall Thickening
- •Concavities and Convexities
- •12.1 The Prostate
- •Enlarged Prostate
- •Regular
- •Irregular
- •Small Prostate
- •Regular
- •Echogenic
- •Circumscribed Lesion
- •Anechoic
- •Hypoechoic
- •Echogenic
- •12.2 Seminal Vesicles
- •Diffuse Change
- •Hypoechoic
- •Circumscribed Change
- •Anechoic
- •Echogenic
- •Irregular
- •12.3 Testis, Epididymis
- •Diffuse Change
- •Enlargement
- •Decreased Size
- •Circumscribed Lesion
- •Anechoic or Hypoechoic
- •Irregular/Echogenic
- •Epididymal Lesion
- •Anechoic
- •Hypoechoic
- •Intrascrotal Mass
- •Anechoic or Hypoechoic
- •Echogenic
- •13 Female Genital Tract
- •Masses
- •Abnormalities of Size or Shape
- •Uterus
- •Abnormalities of Size or Shape
- •Myometrial Changes
- •Intracavitary Changes
- •Endometrial Changes
- •Fallopian Tubes
- •Hypoechoic Mass
- •Anechoic Cystic Mass
- •Solid Echogenic or Nonhomogeneous Mass
- •14 Thyroid Gland
- •Diffuse Changes
- •Enlarged Thyroid Gland
- •Small Thyroid Gland
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Circumscribed Changes
- •Anechoic
- •Hypoechoic
- •Isoechoic
- •Hyperechoic
- •Irregular
- •Differential Diagnosis of Hyperthyroidism
- •Types of Autonomy
- •15 Pleura and Chest Wall
- •Chest Wall
- •Masses
- •Parietal Pleura
- •Nodular Masses
- •Diffuse Pleural Thickening
- •Pleural Effusion
- •Anechoic Effusion
- •Echogenic Effusion
- •Complex Effusion
- •16 Lung
- •Masses
- •Anechoic Masses
- •Hypoechoic Masses
- •Complex Masses
- •Index
1
Vessels
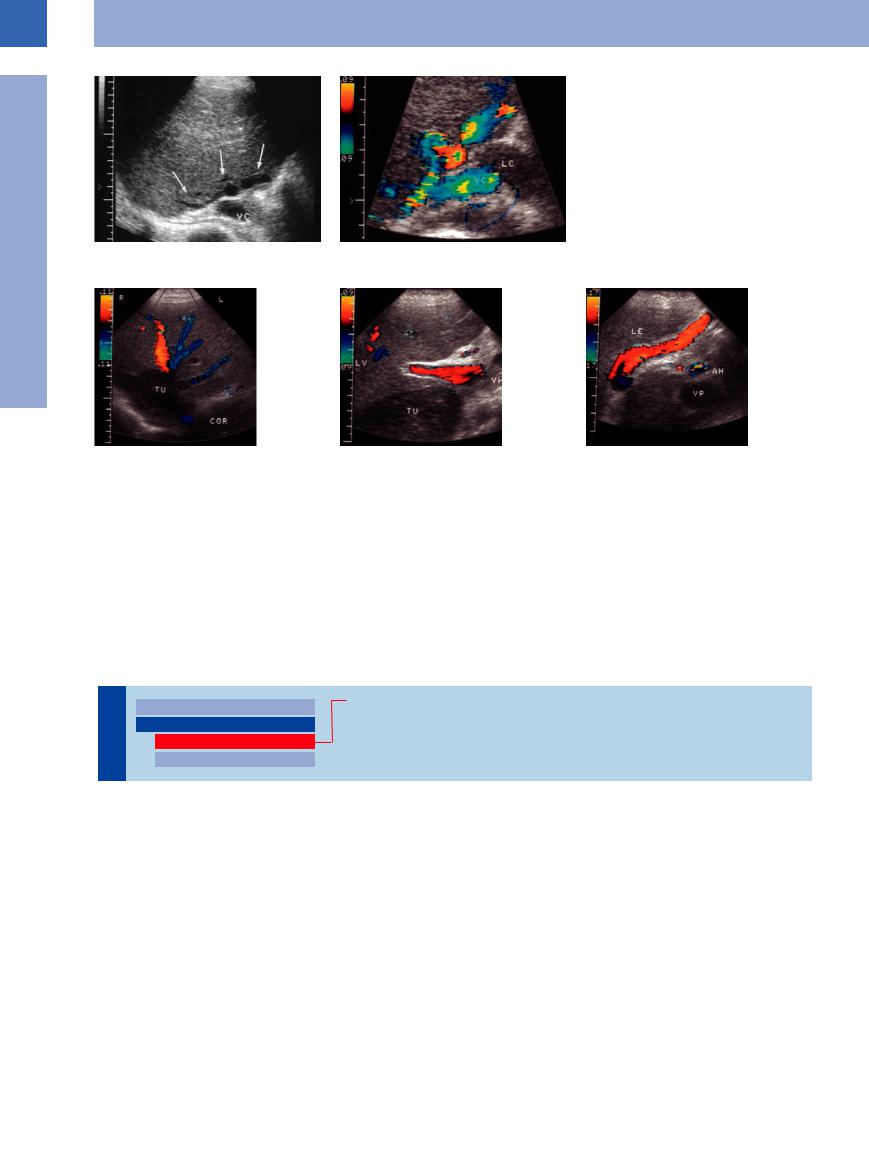
Fig. 1.96 A 24-year-old man with multiple drug dependence: old hepatic veno-occlusive disease (Budd–Chiari syndrome) with esophageal varices. Normal hepatic veins cannot be demonstrated (a); singular varicosities around the junction of the hepatic veins. VC = vena cava; LC = caudate lobe (b).
Fig. 1.97 Patient presenting with primary leiomyoma of |
b Demonstration of the tumor and portal vein (VP) with |
c Marked recanalization of the umbilical vein in post- |
the vena cava. |
normal direction of flow. |
hepatic block. LE = liver; AH = hepatic artery. |
a Intracaval tumor mass (TU); flow reversal in the right |
|
|
hepatic vein. COR = heart. |
|
|
Patients with posthepatic block usually ex- |
ragmatic veins draining in a cephalad direction. |
duced blood flow with a pulsatile profile, |
hibit thickening of the gallbladder wall, and |
Flow reversal in the portal vein may also be |
which in some cases turns into full-fledged |
sometimes it is possible to demonstrate intra- |
seen.17 Quite often in patients with cardiac de- |
pulse-synchronous flow reversal. |
hepatic venovenous collaterals or transdiaph- |
compensation, the portal vein will exhibit re- |
|
■ Intraluminal Mass
Thrombosis
|
|
|
|
Enlarged Lumen Diameter |
|
Portal Vein Thrombosis |
|
|
|
|
|
||||
|
|
|
|
Intraluminal Mass |
|
Splenic Vein Thrombosis |
|
Vessels |
|
||||||
|
|
Thrombosis |
|
Thrombosis of the Superior Mesenteric Vein |
|||
|
|
|
|||||
|
|
Tumor |
|
||||
|
|
|
|
|
|
|
|
Portal Vein Thrombosis















































The etiology of portal vein thrombosis is rather varied (Table 1.4). Cirrhosis of the liver is by far the most common cause, although in fresh thrombosis hepatocellular carcinoma must be ruled out.18 Portal vein thrombosis may be subdivided into partial intrahepatic thrombosis, complete or partial thrombosis of the portal trunk, and additional thrombosis of the tributaries (splenic and mesenteric veins).
In acute thrombosis the lumen of the portal vein most often is enlarged and displays a rel-
atively homogeneous anechogenicity ( 1.9 d,g). If color-flow Doppler scanning demonstrates no flow, the diagnosis is confirmed.19 This venous occlusion will open up collaterals, some of which will drain in hepatopetal fashion. Over the course of time the former portal tree will exhibit an atypical vascular architecture; the underlying process is described as cavernous transformation (
1.9 d,g). If color-flow Doppler scanning demonstrates no flow, the diagnosis is confirmed.19 This venous occlusion will open up collaterals, some of which will drain in hepatopetal fashion. Over the course of time the former portal tree will exhibit an atypical vascular architecture; the underlying process is described as cavernous transformation ( 1.9e,f,i). In ultrasonography, marked varices can mimic a tumor (cavernoma). The extent and duration of this
1.9e,f,i). In ultrasonography, marked varices can mimic a tumor (cavernoma). The extent and duration of this
cavernous transformation may be quite varied ( 1.9i,l,m).
1.9i,l,m).
Other less frequent collaterals may be seen alongside these cavernous transformations:
●Atypical paraportal collaterals (Fig.1.98)
●Varices around the peribiliary vascular plexus (Fig.1.99)
In addition, there may be hepatofugal collaterals via the right gastric vein or collaterals draining in a caudad direction.20
48
 1.9 Typical Findings in Portal Vein Thrombosis
1.9 Typical Findings in Portal Vein Thrombosis
Portal vein with partial thrombosis
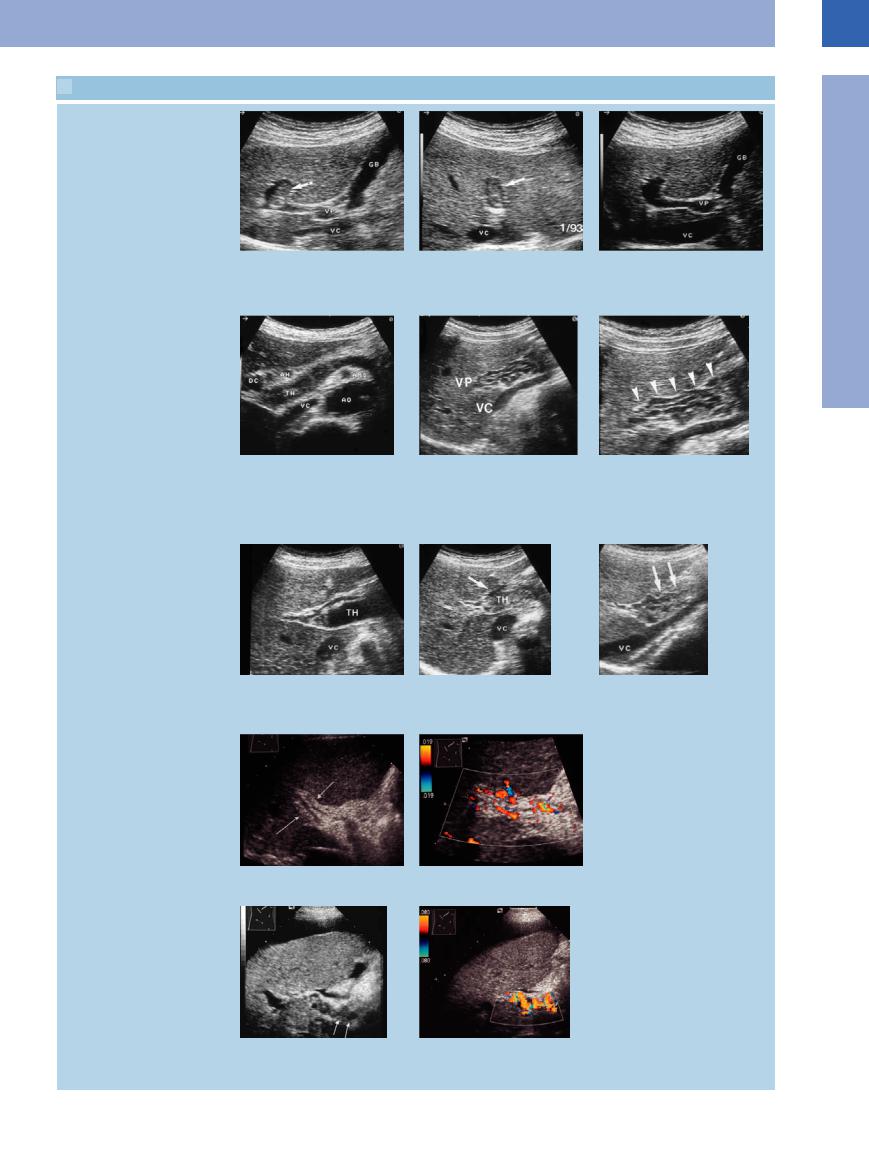
a–c A 71-year-old patient with cancer of the colon. GB = gallbladder; VC = vena cava; VP = portal vein.
a and b Upper abdomen longitudinal and transverse section. Incidental finding of partial thrombosis of the intrahepatic portal vein.
c Spontaneous lysis after 2 months.
Portal vein thrombosis and cavernous transformation of portal vein
d Echogenic image of the portal vein in |
e and f A 24-year-old woman with esoph- f Section magnification. |
thrombosis. DC = bile duct; AH = hepatic |
ageal varices secondary to portal vein |
artery; TH = thrombus; VC = vena cava; AO |
thrombosis. |
= aorta. |
e Varicosities along the portal vein as a |
|
result of cavernous transformation of the |
|
portal vein. VC = vena cava; VP = portal |
|
vein. |
g–i Sonographic course of a fresh portal |
h Increasingly echogenic transformation of i Beginning recanalization after 4 months. |
vein thrombosis (TH). VC = vena cava. |
the thrombosis. |
g Hypoechoic image of the thrombotic |
|
material. |
|
Portal vein thrombosis and partial recanalization
j and k Portal vein thrombosis, 6 years old. |
k CDS: no significant recanalization de- |
j Fibrotic occlusion of the portal vein. |
monstrable. |
l and m Thrombosis of the portal vein with |
m Color-flow duplex scan of the cavernous |
cavernous recanalization. |
recanalization. |
l Cavernous recanalization cephalad of the |
|
portal vein. |
|
1
Intraluminal Mass
49
1
Vessels
Table 1.4 Etiology of portal vein thrombosis22
● Idiopathic
● Liver cirrhosis
● Malignant tumors ● Pancreatic diseases ● Para-infective
● Posttraumatic
● Collagenosis
● Thrombophilia
● Myeloproliferative diseases
Fig. 1.98 A 3-year-old thrombosis of the portal vein with paraportal “recanalization” (collaterals). The portal blood drains toward the gallbladder (GB) and from there into the liver. VP = portal vein.
Fig. 1.99
a Patient with Klatskin tumor, stent palliation, and occlusion of the portal vein (VP).
b Originating from the portal vein there are marked cephalad collaterals around the peribiliary venous plexus. GB = gallbladder.
Splenic Vein Thrombosis 























Complete or partial thrombosis of the splenic vein is a common complication of acute pancreatitis and cancer of the pancreas. It may also originate from portal vein thrombosis and grow by apposition.
The ultrasound image depicts a hypoechoic vascular lumen without any flow on color-flow Doppler scanning. Partial thrombosis of the
splenic vein is sometimes observed. One of the sequelae of this vascular obstruction is “segmental” portal hypertension. Collateralization primarily opens the peripancreatic and perigastric veins draining cephalad via esophageal varices as well as veins running in a caudad direction (omental veins draining into the mesenteric veins) (Figs. 1.100, 1.101, 1.102).
A finding of hepatosplenomegaly is not mandatory, and neither is the build-up of ascites. Over time, the splenic vein may become recanalized or undergo cavernous transformation, although quite often the collaterals will persist. In thrombosis of the splenic vein, one rare complication is splenic infarction or even rupture.
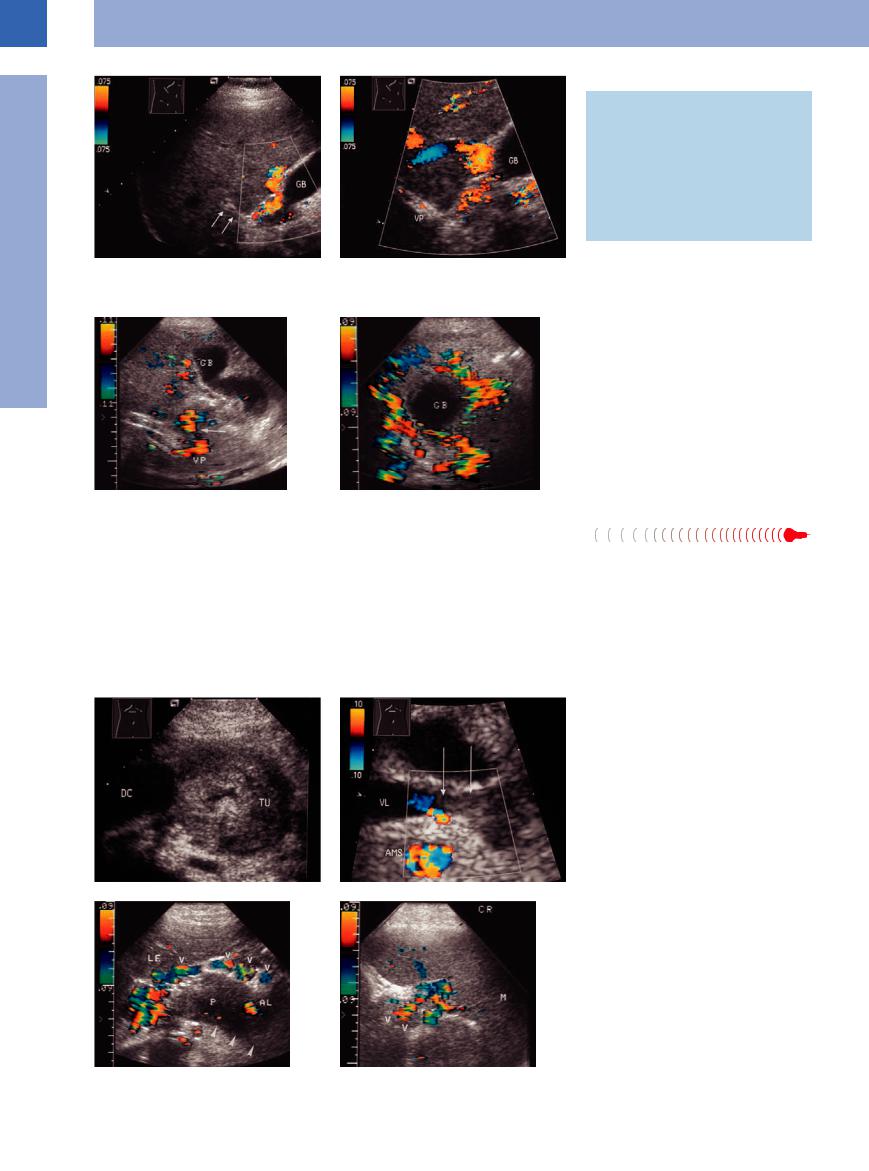
Fig. 1.100 Splenic vein thrombosis.
a Cancer (TU) of the pancreatic head. DC = bile duct.
b Demonstration of echogenic material in the splenic vein (VL). AMS = superior mesenteric vein.
Fig. 1.101 Acute pancreatitis.
a The splenic vein cannot be imaged. Marked varices anterior to the pancreas.
b Demonstration of varicosities (V). M = spleen; LE = liver; P = pancreas; AL = splenic artery.
50
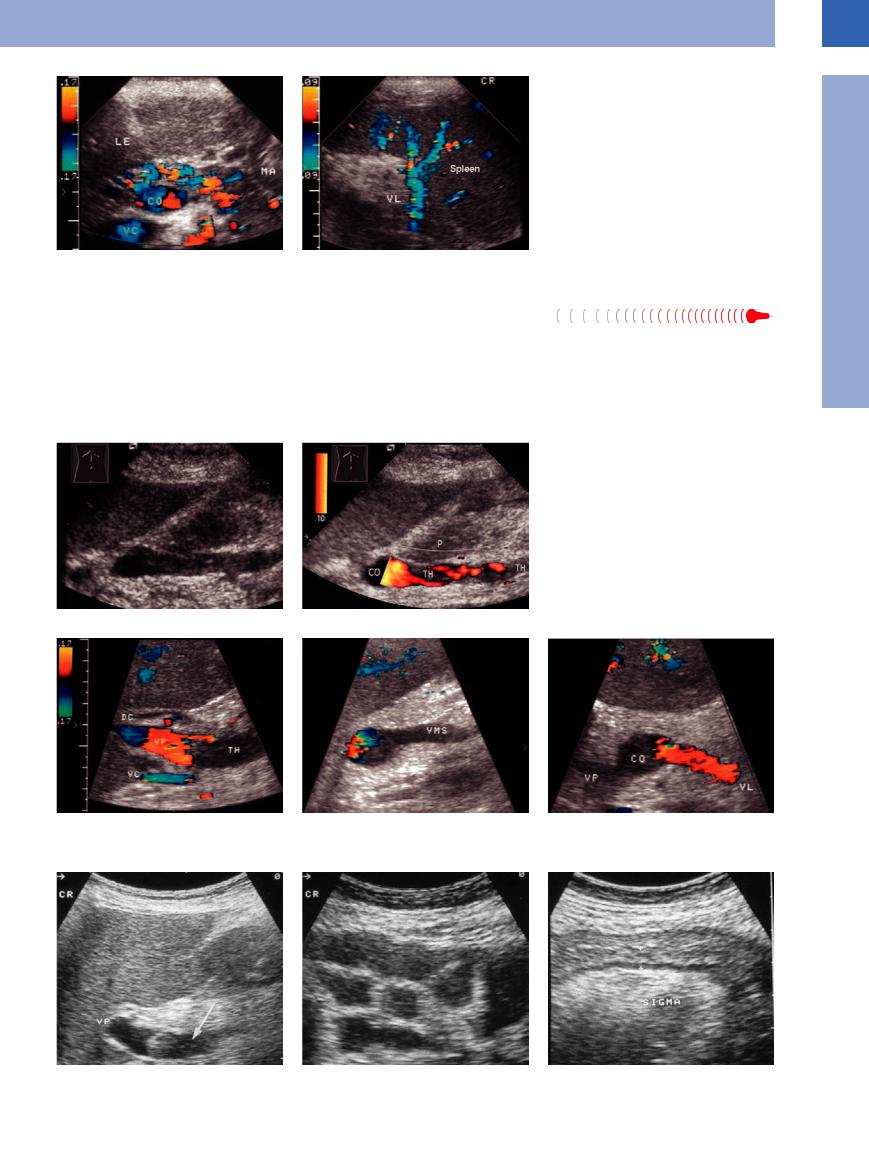
Fig. 1.102 Thrombosis of the splenic vein after mesenteric irradiation of a malignant lymphoma. LE = liver; MA = stomach; CO = venous confluence; VC = vena cava; VL = splenic vein; Milz = spleen.
a The splenic vein cannot be imaged and there is marked peripancreatic collateralization.
b Regular appearance of the splenic vein at the splenic portal.
Thrombosis of the
the Superior Mesenteric Vein
Superior Mesenteric Vein 












Truly isolated thrombosis of the superior mesenteric vein does not result in portal hypertension. However, it may be associated with splenic and/or portal vein thrombosis. The etiology is primarily inflammatory, in particular acute pancreatitis (Fig.1.103). During the acute
phase, the clinical symptoms with severe abdominal pain are impressive (Fig.1.104). On ultrasound the mesenteric vessels appear dilated and lined with echogenic structures. Color-flow Doppler scanning will not elicit any flow signals. Partial thrombosis is possible.
In rare cases there may be segmental infarction of the intestines. Usually this disorder does not require surgery, and quite often there will be spontaneous recanalization.
Fig. 1.103 Patient with acute pancreatitis.
a The tip of the thrombus within the superior mesenteric vein extends into the confluence of the mesenteric and splenic veins. Color-flow duplex scanning demonstrates echogenic thrombotic material.
b Color-flow duplex scanning depicts partial recanalization. P = tail of pancreas; CO = venous confluence; TH = thrombosis.
Fig. 1.104 A 50-year-old patient with acute abdomen.
a–c Color-flow duplex scanning demonstrates complete thrombosis of the superior mesenteric vein (VMS). DC = common bile duct; TH = thrombosis; VP = portal vein; VC = vena cava; CO = venous confluence; VL = splenic vein.
d–f B-mode imaging also depicts the thrombosis. Massive dilatation of the small intestine. There is thickening of the colonic wall at the level of the sigmoid and a lack of peristalsis (nonsurgical treatment proved successful).
1
Intraluminal Mass
51
