
- •Contents
- •Preface
- •Contributors
- •1 Vessels
- •1.1 Aorta, Vena Cava, and Peripheral Vessels
- •Aorta, Arteries
- •Anomalies and Variant Positions
- •Dilatation
- •Stenosis
- •Wall Thickening
- •Intraluminal Mass
- •Perivascular Mass
- •Vena Cava, Veins
- •Anomalies
- •Dilatation
- •Intraluminal Mass
- •Compression, Infiltration
- •1.2 Portal Vein and Its Tributaries
- •Enlarged Lumen Diameter
- •Portal Hypertension
- •Intraluminal Mass
- •Thrombosis
- •Tumor
- •2 Liver
- •Enlarged Liver
- •Small Liver
- •Homogeneous Hypoechoic Texture
- •Homogeneous Hyperechoic Texture
- •Regionally Inhomogeneous Texture
- •Diffuse Inhomogeneous Texture
- •Anechoic Masses
- •Hypoechoic Masses
- •Isoechoic Masses
- •Hyperechoic Masses
- •Echogenic Masses
- •Irregular Masses
- •Differential Diagnosis of Focal Lesions
- •Diagnostic Methods
- •Suspected Diagnosis
- •3 Biliary Tree and Gallbladder
- •3.1 Biliary Tree
- •Thickening of the Bile Duct Wall
- •Localized and Diffuse
- •Bile Duct Rarefaction
- •Localized and Diffuse
- •Bile Duct Dilatation and Intraductal Pressure
- •Intrahepatic
- •Hilar and Prepancreatic
- •Intrapancreatic
- •Papillary
- •Abnormal Intraluminal Bile Duct Findings
- •Foreign Body
- •The Seven Most Important Questions
- •3.2 Gallbladder
- •Changes in Size
- •Large Gallbladder
- •Small/Missing Gallbladder
- •Wall Changes
- •General Hypoechogenicity
- •General Hyperechogenicity
- •General Tumor
- •Focal Tumor
- •Intraluminal Changes
- •Hyperechoic
- •Hypoechoic
- •Nonvisualized Gallbladder
- •Missing Gallbladder
- •Obscured Gallbladder
- •4 Pancreas
- •Diffuse Pancreatic Change
- •Large Pancreas
- •Small Pancreas
- •Hypoechoic Texture
- •Hyperechoic Texture
- •Focal Changes
- •Anechoic Lesion
- •Hypoechoic Lesion
- •Isoechoic Lesion
- •Hyperechoic Lesion
- •Irregular (Complex Structured) Lesion
- •Dilatation of the Pancreatic Duct
- •Marginal/Mild Dilatation
- •Marked Dilatation
- •5 Spleen
- •Nonfocal Changes of the Spleen
- •Diffuse Parenchymal Changes
- •Large Spleen
- •Small Spleen
- •Focal Changes of the Spleen
- •Anechoic Mass
- •Hypoechoic Mass
- •Hyperechoic Mass
- •Splenic Calcification
- •6 Lymph Nodes
- •Peripheral Lymph Nodes
- •Head/Neck
- •Extremities (Axilla, Groin)
- •Abdominal Lymph Nodes
- •Porta Hepatis
- •Splenic Hilum
- •Mesentery (Celiac, Upper and Lower Mesenteric Station)
- •Stomach
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •Small/Large Intestine
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •8 Peritoneal Cavity
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Wall Structures
- •Smooth Margin
- •Irregular Margin
- •Intragastric Processes
- •Intraintestinal Processes
- •9 Kidneys
- •Anomalies, Malformations
- •Aplasia, Hypoplasia
- •Cystic Malformation
- •Anomalies of Number, Position, or Rotation
- •Fusion Anomaly
- •Anomalies of the Renal Calices
- •Vascular Anomaly
- •Diffuse Changes
- •Large Kidneys
- •Small Kidneys
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Irregular Structure
- •Circumscribed Changes
- •Anechoic Structure
- •Hypoechoic or Isoechoic Structure
- •Complex Structure
- •Hyperechoic Structure
- •10 Adrenal Glands
- •Enlargement
- •Anechoic Structure
- •Hypoechoic Structure
- •Complex Echo Structure
- •Hyperechoic Structure
- •11 Urinary Tract
- •Malformations
- •Duplication Anomalies
- •Dilatations and Stenoses
- •Dilated Renal Pelvis and Ureter
- •Anechoic
- •Hypoechoic
- •Hypoechoic
- •Hyperechoic
- •Large Bladder
- •Small Bladder
- •Altered Bladder Shape
- •Intracavitary Mass
- •Hypoechoic
- •Hyperechoic
- •Echogenic
- •Wall Changes
- •Diffuse Wall Thickening
- •Circumscribed Wall Thickening
- •Concavities and Convexities
- •12.1 The Prostate
- •Enlarged Prostate
- •Regular
- •Irregular
- •Small Prostate
- •Regular
- •Echogenic
- •Circumscribed Lesion
- •Anechoic
- •Hypoechoic
- •Echogenic
- •12.2 Seminal Vesicles
- •Diffuse Change
- •Hypoechoic
- •Circumscribed Change
- •Anechoic
- •Echogenic
- •Irregular
- •12.3 Testis, Epididymis
- •Diffuse Change
- •Enlargement
- •Decreased Size
- •Circumscribed Lesion
- •Anechoic or Hypoechoic
- •Irregular/Echogenic
- •Epididymal Lesion
- •Anechoic
- •Hypoechoic
- •Intrascrotal Mass
- •Anechoic or Hypoechoic
- •Echogenic
- •13 Female Genital Tract
- •Masses
- •Abnormalities of Size or Shape
- •Uterus
- •Abnormalities of Size or Shape
- •Myometrial Changes
- •Intracavitary Changes
- •Endometrial Changes
- •Fallopian Tubes
- •Hypoechoic Mass
- •Anechoic Cystic Mass
- •Solid Echogenic or Nonhomogeneous Mass
- •14 Thyroid Gland
- •Diffuse Changes
- •Enlarged Thyroid Gland
- •Small Thyroid Gland
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Circumscribed Changes
- •Anechoic
- •Hypoechoic
- •Isoechoic
- •Hyperechoic
- •Irregular
- •Differential Diagnosis of Hyperthyroidism
- •Types of Autonomy
- •15 Pleura and Chest Wall
- •Chest Wall
- •Masses
- •Parietal Pleura
- •Nodular Masses
- •Diffuse Pleural Thickening
- •Pleural Effusion
- •Anechoic Effusion
- •Echogenic Effusion
- •Complex Effusion
- •16 Lung
- •Masses
- •Anechoic Masses
- •Hypoechoic Masses
- •Complex Masses
- •Index
■ Enlarged Lumen Diameter
Precise diagnosis of any enlargement of the portal vein diameter is one of the strong points of ultrasonography.
Portal Hypertension
Vessels |
|
|
Posthepatic Block |
||
|
|
|
Enlarged Lumen Diameter |
|
Prehepatic Block |
|
|
|
Portal Hypertension |
|
Intrahepatic Block |
|
|
|
Intraluminal Mass |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Portal hypertension is defined as a pressure of more than 10 mmHg in the portal vein. The pressure depends on the resistance of the runoff bed within the liver, the blood volume in the splanchnic vessels, and the pressure in the inferior vena cava. The etiology of its various types and causes is classified according to the location of the flow impediment. Accordingly, portal hypertension may be subdivided into prehepatic, intrahepatic, and posthepatic types, with the intrahepatic type being subdivided into postsinusoidal, sinusoidal, and presinusoidal forms (Table 1.2).
Table 1.2 Formation of possible collaterals in portal hypertension (after Seitz et al24)
Cephalad-draining collaterals
●Right gastric vein
●Short gastric veins
●Periumbilical veins
●Portogastric collaterals
●Portorenal collaterals
●Hepatic, phrenic, and splenic capsule veins
Caudad-draining veins
●Paraumbilical veins
●Gastrosplenic shunts
●Splenorenal shunts
●Splenolumbar shunts
●Hemorrhoidal plexus via the mesenteric veins
The pathophysiology of portal hypertension is characterized by a drop in flow velocity, enlarged vein diameter, sclerosis, opening up of collaterals, and flow reversal in the portal vein or its tributaries. The collaterals are differentiated by the direction of their drainage, i. e., they are subdivided into cephaladand caudaddraining shunts (Table 1.3).
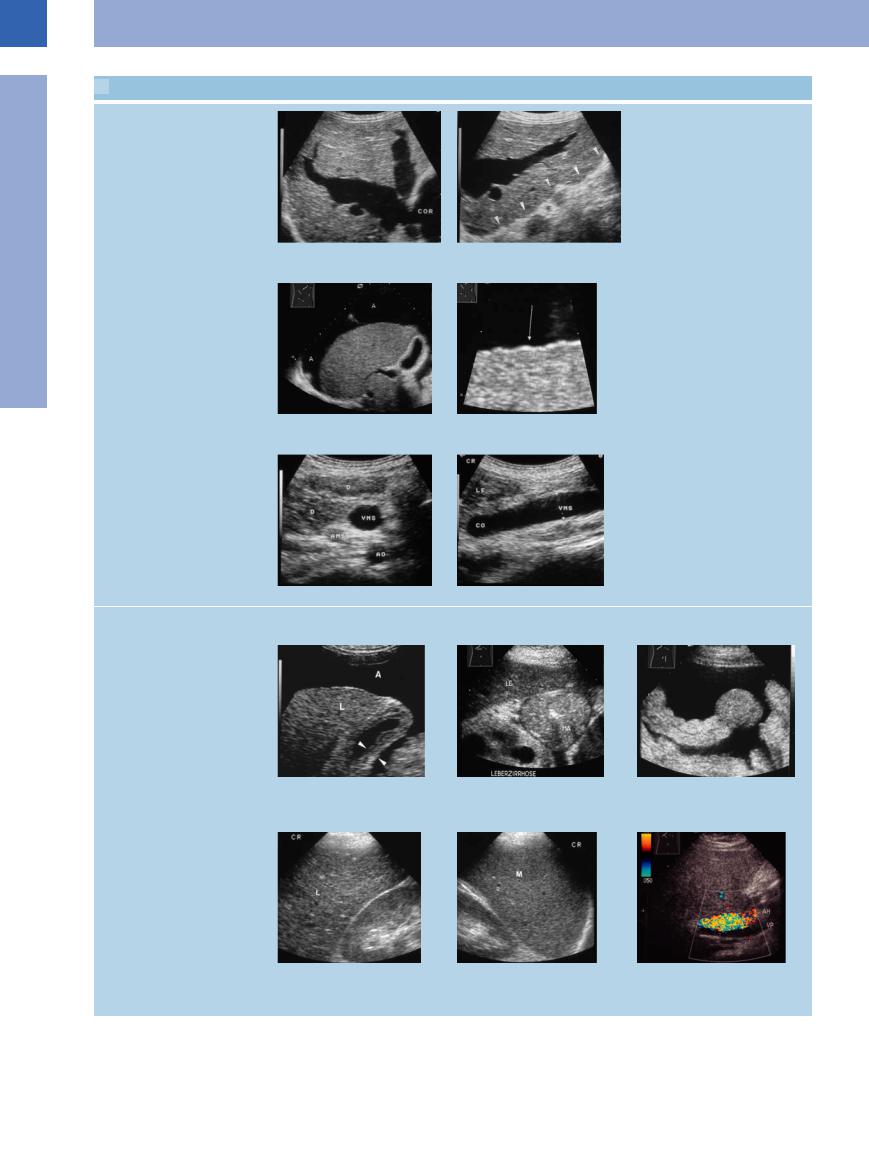
Sonographic studies in portal hypertension will yield presumed and rather firm findings. Images similar to  1.7 should raise the suspicion of portal hypertension:
1.7 should raise the suspicion of portal hypertension:
Table 1.3 Etiology of portal vein thrombosis (after Seitz et al24)
●Idiopathic
●Cirrhosis of the liver
●Malignancies
●Diseases of the pancreas
●Parainfectious
●Posttraumatic
●Collagen disorders
●Thrombophilia
●Myeloproliferative disorders
●Enlarged vena cava and hepatic veins (
1.7a,b)
●Demonstration of ascites ( 1.7c,d)
1.7c,d)
●Demonstration of liver cirrhosis ( 1.7a–d)
1.7a–d)
●No respiratory variation in the diameter of the portal vessels ( 1.7e,f)
1.7e,f)
●Thickening of the gallbladder wall, thickening of the gastric/intestinal wall ( 1.7 g–i)
1.7 g–i)
●Fibrosis of the liver, splenomegaly, flow alterations in portal vein and hepatic artery ( 1.7j–l)
1.7j–l)
1
Enlarged Lumen Diameter
41
1
Vessels
 1.7 Portal Hypertension: Suspect Findings
1.7 Portal Hypertension: Suspect Findings
Hepatic cirrhosis
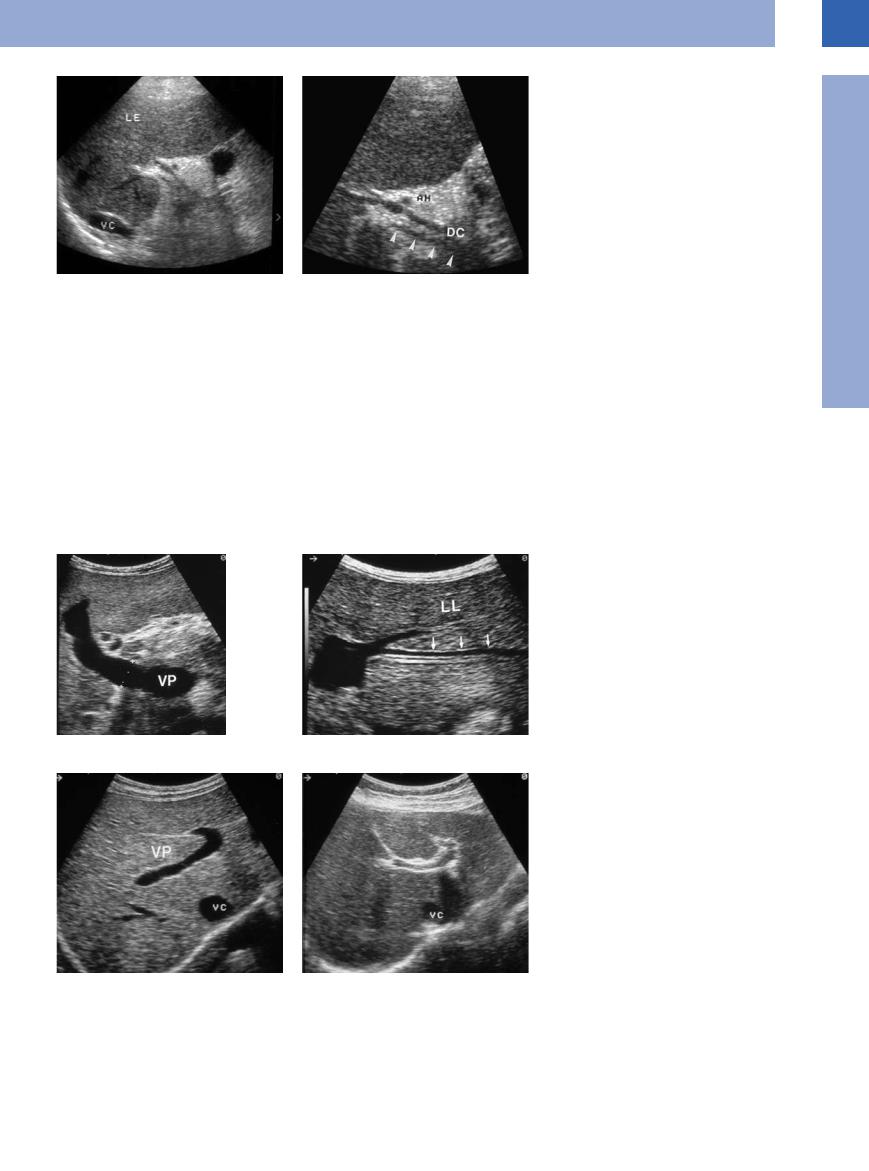
a and b Cardiac cirrhosis in tricuspid insu ciency. Massively dilated hepatic veins; the posteroinferior aspect of the liver has a corrugated appearance (arrows). COR = heart.
Contour signs
c and d Completely cirrhotic liver with ascites (A) and corrugated appearance (arrow) in a chronic alcoholic.
Ascites, thickening of the gallbladder, vascular change
e and f Markedly enlarged lumen of the mesenteric vein (VMS) and its confluence in portal hypertension without respiratory variation. LE = liver; CO = venous confluence. e Upper abdomen transverse scan.
f Longitudinal scan.
Thickening of the gallbladder wall, stomach, and bowel walls
Fibrosis of the liver, splenomegaly, altered flow in the portal vein and hepatic artery
g–i Congested walls in portal hypertension.
g Thickening of the gallbladder wall (arrows) in liver cirrhosis (L) with ascites (A).
j Completely cirrhotic liver (L) with markedly coarse hepatic parenchyma.
h Stomach, with marked thickening of the gastric wall in cirrhosis of the liver and portal hypertension. A = ascites, MA = gastric wall; LE = liver.
k Portal hypertension with pronounced splenomegaly (M).
i Pronounced intestinal wall in portal hypertension.
l Posthepatic cirrhosis of the liver with decreased portal blood flow and increased flow in the hepatic artery (AH). VP = portal vein.
42
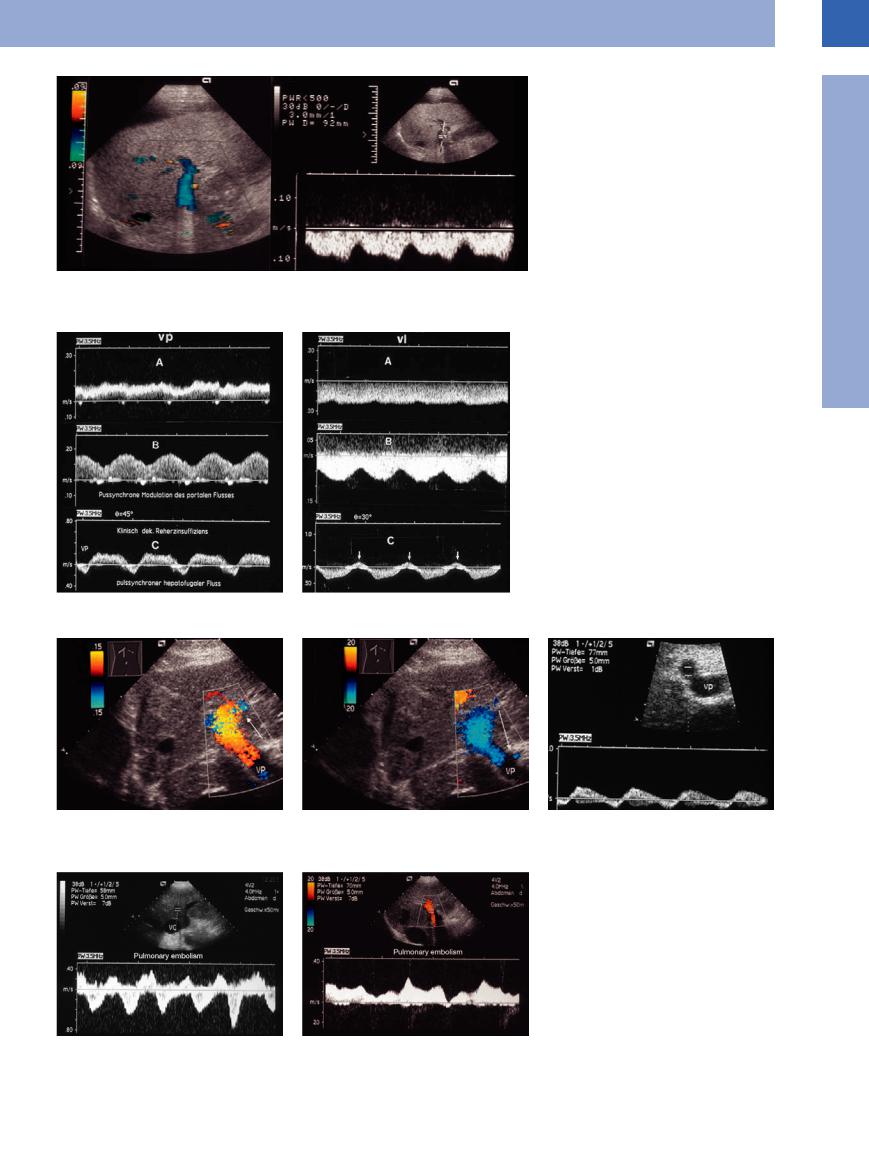
Fig. 1.84 Continuous flow reversal in the portal vein (hepatofugal flow) in a patient with liver cirrhosis.
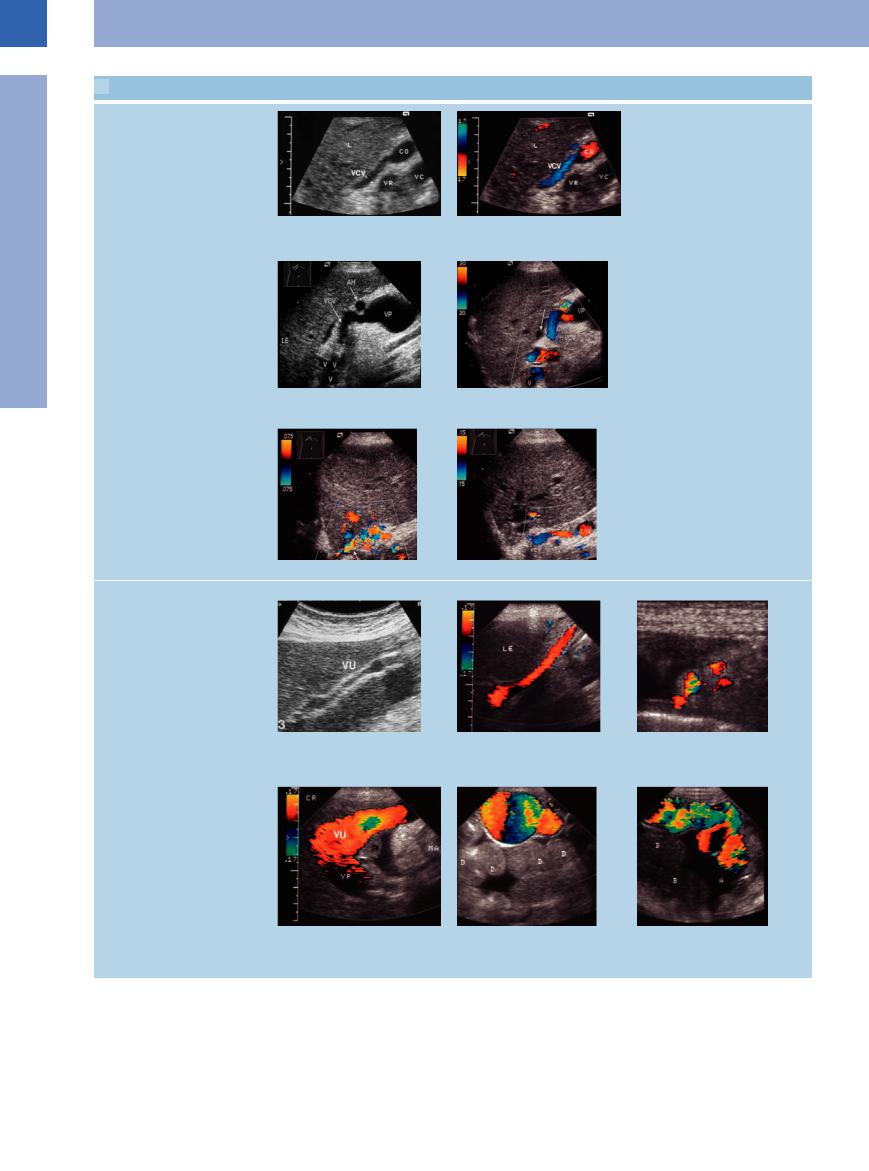
Since the introduction of color-flow Doppler imaging, the following are considered rather firm signs of portal hypertension:
●Flow reversal in the portal vein or some of its tributaries (Fig.1.84)
●Oscillating flow in the portal vein or some of its tributaries (Figs. 1.85, 1.86, 1.87)
●No flow (Fig.1.88b)
●Demonstration of portosystemic collaterals
Fig. 1.85 Images of different flow profiles: A, continuous hepatopetal flow; B, pulsatile hepatopetal flow; C, pulsatile flow with brief pulse-synchronous flow reversal (arrows).
a In the portal vein.
b In the splenic vein.
1
Enlarged Lumen Diameter
Fig. 1.86 Pulsatile portal flow with brief pulse-synchronous flow reversal in a patient with cardiac cirrhosis. VP = portal vein.
Fig. 1.87 Patient with clinically evident symptomatic pulmonary embolism.
a Flow profile of the hepatic veins with severe pulsesynchronous reflux.
b Flow profile in the portal vein with predominantly hepatopetal flow but also brief hepatofugal flow.
43
1
Vessels
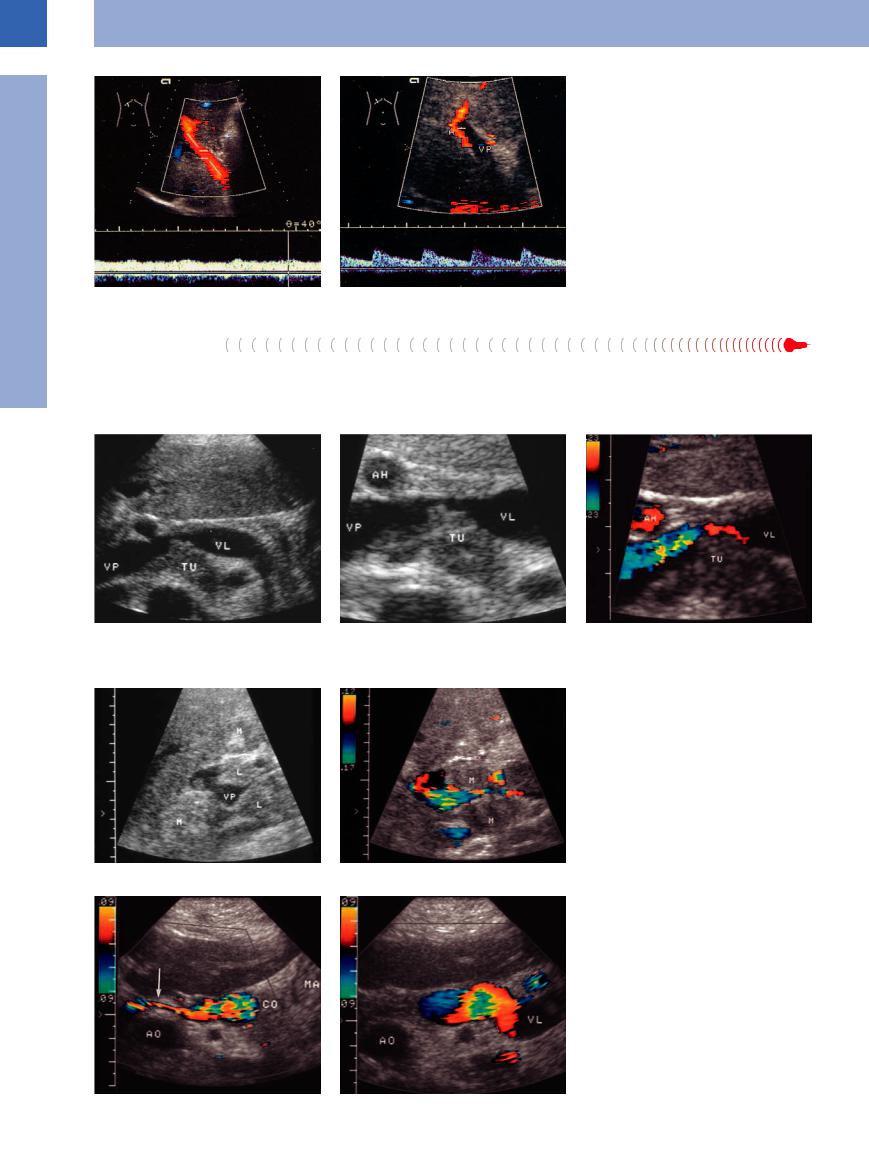
Prehepatic Block
Block
In less than 20% of patients portal hypertension will be due to a prehepatic block. Important causes of prehepatic block are total or partial
thrombosis of the portal, splenic, and mesenteric veins (Fig.1.89). Extrinsic portal vein compression (Fig.1.90), agenesis, or hypoplastic
Fig. 1.88 Portal hypertension, CDS. a Drop in flow velocity to 9 cm/s.
b No flow in the portal vein (VP); increased diameter of the hepatic artery (A) (source: Schmidt23).
malformation also may result in portal hypertension (Fig.1.91, Fig.1.92).
Fig. 1.89 Patient with pancreatic cancer. |
c Color-flow Doppler scanning demonstrates turbulence, |
a and b Tumor (TU) infiltrating the splenic vein (VL). VP = portal vein; AH = hepatic artery. |
signifying a stenosis. |
Fig. 1.90 Hepatic hilar lymph nodes in a patient with stomach cancer.
a Portal vein (VP) compression. M = spleen; L = liver.
b Color-flow Doppler scanning demonstrates turbulence, signifying a stenosis.
Fig. 1.91 Portal vein hypoplasia of unknown etiology, with severe compression of the vessel (a), prestenotic dilatation, and turbulence phenomena in color-flow Doppler scanning (b).
44
Intrahepatic  Block
Block


















































With ~80% of cases, intrahepatic block is by far the most common cause of portal hypertension. The most important factors are hepatic disorders, in particular cirrhosis of the liver.
Cirrhotic vascular changes. The sonographic criteria for transformation of the hepatic parenchyma should be noted since the cirrhotic vascular changes will point the way toward the diagnosis of portal hypertension:
●Enlarged diameter of the portal vein and sudden diameter changes in the branches
of the portal vein (Fig.1.93)
● Pronounced periportal encasement (Fig.1.94)
● Rarified peripheral vascular tree in the liver
Collaterals. Demonstration of any collaterals is of particular interest, the following collateral systems being of primary importance:
●Enlarged left gastric vein with flow reversal ( 1.8a,b)
1.8a,b)
Fig. 1.92 Aplastic portal vein with collateralization, possibly due to old thrombotic and now fibrotic occlusion of the vein, in a 25-year-old woman.
a Survey image in an oblique upper abdominal scan: no detectable portal vein.
b Detail view: Posterior to the CBD barely visible part of the portal vein (arrows).
AH = hepatic artery; DC = common bile duct; LE = liver; VC = vena cava.
●Demonstration of esophageal varices (
1.8c–f)
●Recanalization of the umbilical veins (inner
and outer caput medusae) ( 1.8 g–l)
1.8 g–l)
● Demonstration of varicosities in the splenic hilum (short gastric veins) ( 1.8 m–o)
1.8 m–o)
●Demonstration of splenorenal shunting (
1.8 p–r)
Shunts. In rare cases, intrahepatic portocaval or intrasplenic cephalad-draining varicosities may be demonstrated ( 1.8 s–u).
1.8 s–u).
Fig. 1.93 Portal hypertension. a Enlarged portal vein (VP).
b Sudden caliber change in the portal branches of the left hepatic lobe (LL).
Fig. 1.94 Pronounced periportal echogenicity. VC = vena cava.
a Normal branching of the portal vein (VP).
b Pronounced echogenic boundary of the portal vein (although this finding is also seen as a normal variant).
1
Enlarged Lumen Diameter
45
1
Vessels
 1.8 Collaterals in Intrahepatic Block
1.8 Collaterals in Intrahepatic Block
Enlargement and reversal of flow in the left gastric vein
a and b Enlarged left gastric vein (VCV) with normal flow into the portal vein. CO = confluence of superior mesenteric and splenic vein, VR = renal vein, VC = vena cava, L = liver.
c and d Flow reversal in the right gastric vein (VCV) in portal hypertension. V = paraesophageal varices; AH = hepatic artery; VP = portal vein; LE = liver.
Paraesophageal varices
e Marked paraesophageal varices (arrow).
Recanalized umbilical vein (inner and outer caput medusae)
f The paraesophageal varices are supplied by the left gastric vein.
g–i Distinct recanalization of the umbilical |
h and i CDS. |
i Transverse section. |
vein (VU). |
h Longitudinal section. |
|
g B-mode. |
|
|
j Massively dilated umbilical vein.
k and l These images (cephalocaudal view) demonstrate the varicosities of an inner caput medusae. They could be mistaken for localized intra-abdominal fluid (caution: aspiration). Color-flow duplex scans of the varicosities. VP = portal vein; VU = umbilical vein; MA = stomach; A = ascites; D = small intestine.
46
 1.8 Collaterals in Intrahepatic Block (Continued)
1.8 Collaterals in Intrahepatic Block (Continued)
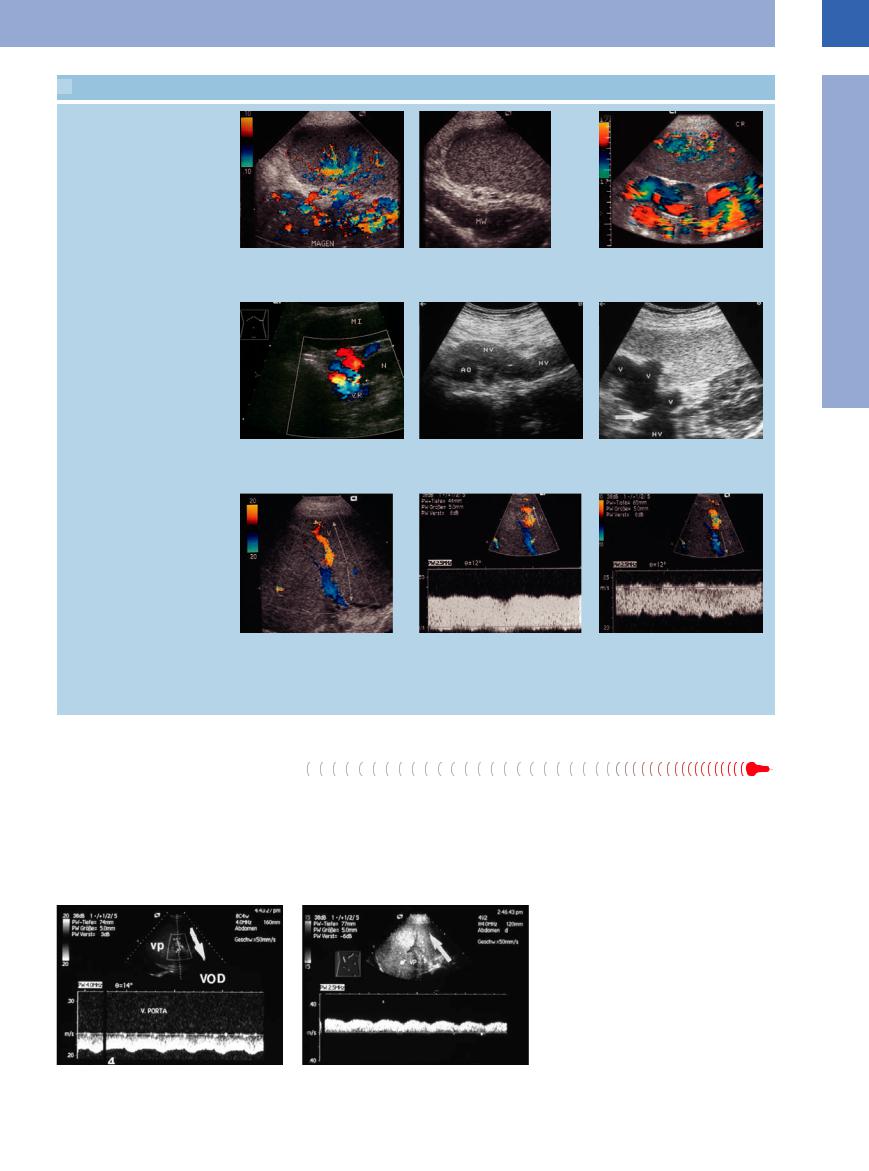
Splenic hilum varices and collaterals (short gastric vessels)
m Numerous collateral veins running from the splenic hilum to the gastric wall (Magen) in cirrhosis of the liver.
Splenorenal shunts
p Splenorenal collaterals. Inflow from splenic hilum varices into the renal vein. N = kidney, Mi = spleen.22
Shunts: Intrahepatic portocaval shunts or intrasplenic varices, draining cranially
s–u Intrasplenic venous “watershed”. The hilar splenic veins exhibit normal drainage into the hilum, whereas the cortical splenic veins drain toward the surface of the spleen (flow reversal).
s CDS The color-coded (red/blue) vessel with arrows showing the flow direction.
n and o Massive splenic varices in portal hypertension.
n B-mode.
q Suspiciously dilated renal vein (NV). AO = aorta.
t CDS with spectral analysis of the cortical splenic veins draining toward the surface of the spleen (flow reversal).
o CDS.
r Hilar splenic varices (V) draining into the renal vein (NV), resulting in a splenorenal shunt.
u CDS with spectral analysis of the hilar splenic veins with normal drainage into the hilum.
Posthepatic Block








Posthepatic block is quite rare and occurs in around 1% of all patients with portal hypertension. Budd–Chiari syndrome is really a thrombosis with occlusion of the major hepatic veins. The most important etiological factors are systemic hematological disease, disorders
in hemostasis, and hepatic metastasis. In venous occlusive disease the major hepatic veins are patent while the small veins at the microscopic level are thrombosed. The primary etiological factor is graft rejection after allogeneic bone marrow transplant. Chronic constrictive
pericarditis (armored heart) is a rare cause of posthepatic block, and another rare causative entity is primary tumor of the vena cava (Figs. 1.95, 1.96, 1.97).
Fig. 1.95 A 23-year-old patient with acute lymphocytic leukemia (ALL) after allogeneic bone marrow transplantation.
a Clinical diagnosis of hepatic veno-occlusive disease (VOD) with flow reversal in the portal vein (VP).
b Post-therapy demonstration of normal direction of flow in the portal vein.
1
Enlarged Lumen Diameter
47
