
- •Contents
- •Preface
- •Contributors
- •1 Vessels
- •1.1 Aorta, Vena Cava, and Peripheral Vessels
- •Aorta, Arteries
- •Anomalies and Variant Positions
- •Dilatation
- •Stenosis
- •Wall Thickening
- •Intraluminal Mass
- •Perivascular Mass
- •Vena Cava, Veins
- •Anomalies
- •Dilatation
- •Intraluminal Mass
- •Compression, Infiltration
- •1.2 Portal Vein and Its Tributaries
- •Enlarged Lumen Diameter
- •Portal Hypertension
- •Intraluminal Mass
- •Thrombosis
- •Tumor
- •2 Liver
- •Enlarged Liver
- •Small Liver
- •Homogeneous Hypoechoic Texture
- •Homogeneous Hyperechoic Texture
- •Regionally Inhomogeneous Texture
- •Diffuse Inhomogeneous Texture
- •Anechoic Masses
- •Hypoechoic Masses
- •Isoechoic Masses
- •Hyperechoic Masses
- •Echogenic Masses
- •Irregular Masses
- •Differential Diagnosis of Focal Lesions
- •Diagnostic Methods
- •Suspected Diagnosis
- •3 Biliary Tree and Gallbladder
- •3.1 Biliary Tree
- •Thickening of the Bile Duct Wall
- •Localized and Diffuse
- •Bile Duct Rarefaction
- •Localized and Diffuse
- •Bile Duct Dilatation and Intraductal Pressure
- •Intrahepatic
- •Hilar and Prepancreatic
- •Intrapancreatic
- •Papillary
- •Abnormal Intraluminal Bile Duct Findings
- •Foreign Body
- •The Seven Most Important Questions
- •3.2 Gallbladder
- •Changes in Size
- •Large Gallbladder
- •Small/Missing Gallbladder
- •Wall Changes
- •General Hypoechogenicity
- •General Hyperechogenicity
- •General Tumor
- •Focal Tumor
- •Intraluminal Changes
- •Hyperechoic
- •Hypoechoic
- •Nonvisualized Gallbladder
- •Missing Gallbladder
- •Obscured Gallbladder
- •4 Pancreas
- •Diffuse Pancreatic Change
- •Large Pancreas
- •Small Pancreas
- •Hypoechoic Texture
- •Hyperechoic Texture
- •Focal Changes
- •Anechoic Lesion
- •Hypoechoic Lesion
- •Isoechoic Lesion
- •Hyperechoic Lesion
- •Irregular (Complex Structured) Lesion
- •Dilatation of the Pancreatic Duct
- •Marginal/Mild Dilatation
- •Marked Dilatation
- •5 Spleen
- •Nonfocal Changes of the Spleen
- •Diffuse Parenchymal Changes
- •Large Spleen
- •Small Spleen
- •Focal Changes of the Spleen
- •Anechoic Mass
- •Hypoechoic Mass
- •Hyperechoic Mass
- •Splenic Calcification
- •6 Lymph Nodes
- •Peripheral Lymph Nodes
- •Head/Neck
- •Extremities (Axilla, Groin)
- •Abdominal Lymph Nodes
- •Porta Hepatis
- •Splenic Hilum
- •Mesentery (Celiac, Upper and Lower Mesenteric Station)
- •Stomach
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •Small/Large Intestine
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •8 Peritoneal Cavity
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Wall Structures
- •Smooth Margin
- •Irregular Margin
- •Intragastric Processes
- •Intraintestinal Processes
- •9 Kidneys
- •Anomalies, Malformations
- •Aplasia, Hypoplasia
- •Cystic Malformation
- •Anomalies of Number, Position, or Rotation
- •Fusion Anomaly
- •Anomalies of the Renal Calices
- •Vascular Anomaly
- •Diffuse Changes
- •Large Kidneys
- •Small Kidneys
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Irregular Structure
- •Circumscribed Changes
- •Anechoic Structure
- •Hypoechoic or Isoechoic Structure
- •Complex Structure
- •Hyperechoic Structure
- •10 Adrenal Glands
- •Enlargement
- •Anechoic Structure
- •Hypoechoic Structure
- •Complex Echo Structure
- •Hyperechoic Structure
- •11 Urinary Tract
- •Malformations
- •Duplication Anomalies
- •Dilatations and Stenoses
- •Dilated Renal Pelvis and Ureter
- •Anechoic
- •Hypoechoic
- •Hypoechoic
- •Hyperechoic
- •Large Bladder
- •Small Bladder
- •Altered Bladder Shape
- •Intracavitary Mass
- •Hypoechoic
- •Hyperechoic
- •Echogenic
- •Wall Changes
- •Diffuse Wall Thickening
- •Circumscribed Wall Thickening
- •Concavities and Convexities
- •12.1 The Prostate
- •Enlarged Prostate
- •Regular
- •Irregular
- •Small Prostate
- •Regular
- •Echogenic
- •Circumscribed Lesion
- •Anechoic
- •Hypoechoic
- •Echogenic
- •12.2 Seminal Vesicles
- •Diffuse Change
- •Hypoechoic
- •Circumscribed Change
- •Anechoic
- •Echogenic
- •Irregular
- •12.3 Testis, Epididymis
- •Diffuse Change
- •Enlargement
- •Decreased Size
- •Circumscribed Lesion
- •Anechoic or Hypoechoic
- •Irregular/Echogenic
- •Epididymal Lesion
- •Anechoic
- •Hypoechoic
- •Intrascrotal Mass
- •Anechoic or Hypoechoic
- •Echogenic
- •13 Female Genital Tract
- •Masses
- •Abnormalities of Size or Shape
- •Uterus
- •Abnormalities of Size or Shape
- •Myometrial Changes
- •Intracavitary Changes
- •Endometrial Changes
- •Fallopian Tubes
- •Hypoechoic Mass
- •Anechoic Cystic Mass
- •Solid Echogenic or Nonhomogeneous Mass
- •14 Thyroid Gland
- •Diffuse Changes
- •Enlarged Thyroid Gland
- •Small Thyroid Gland
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Circumscribed Changes
- •Anechoic
- •Hypoechoic
- •Isoechoic
- •Hyperechoic
- •Irregular
- •Differential Diagnosis of Hyperthyroidism
- •Types of Autonomy
- •15 Pleura and Chest Wall
- •Chest Wall
- •Masses
- •Parietal Pleura
- •Nodular Masses
- •Diffuse Pleural Thickening
- •Pleural Effusion
- •Anechoic Effusion
- •Echogenic Effusion
- •Complex Effusion
- •16 Lung
- •Masses
- •Anechoic Masses
- •Hypoechoic Masses
- •Complex Masses
- •Index
14 Thyroid Gland
Thyroid Gland |
477 |
|||
|
Diffuse Changes |
479 |
||
|
||||
|
|
|
Enlarged Thyroid Gland |
479 |
|
|
|
||
Diffuse Parenchymatous Goiter Diffuse Colloid Goiter
Hypertrophic Hashimoto Thyroiditis Hyperthyroidism due to Graves Disease Subacute de Quervain Thyroiditis Invasive Sclerosing Thyroiditis
(Riedel Goiter) Goiter in Acromegaly Amyloidosis
Small Thyroid Gland |
483 |
Acquired Autoimmune Thyroiditis (AIT): Atrophic Lymphocytic Thyroiditis (Juvenile) Acquired Autoimmune Thyroiditis
(AIT) in Polyglandular Autoimmune Syndrome (PAS)
Lithiumor Amiodarone-Induced Thyroiditis
Neonatal Hypothyroidism Postoperative Thyroid/Unilateral Aplasia Radioiodine-Treated Thyroid Radiation-Induced Hypothyroidism
Hypoechoic Structure |
487 |
Chronic Thyroiditis with Transient
Hyperthyroidism,
Postpartum Thyroiditis
Pregnany-Induced
Thyroid Dysfunction
Silent (Sporadic) Thyroiditis
Lithiumor Amiodarone-Induced
Thyroiditis
Interferon-Induced Thyroiditis
|
|
Hyperechoic Structure |
489 |
||||
|
|
|
|
|
|
Radiation-Induced Hypothyroidism |
|
Circumscribed Changes |
489 |
||||||
|
|
Anechoic |
489 |
||||
|
|
||||||
|
|
|
|
|
|
Cysts |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Vessels |
|
|
|
|
|
|
|
||
|
|
|
|
|
|
Abscess |
|
|
|
|
Hypoechoic |
491 |
|||
|
|
|
|||||
Microfollicular (Papillary)
Adenoma
Oncocytic Adenoma
Parathyroid Adenoma
Abscess
Focal de Quervain Thyroiditis
Malignant Lymphoma
Carcinoma
Tumor Infiltration or Metastasis
Isoechoic |
499 |
Normofollicular Adenoma Hemorrhagic or Colloid Cyst Regressive Changes in an Adenoma or Adenomatous Nodule Parathyroid Adenoma/Hyperplasia Lipoma
|
Hyperechoic |
501 |
|
Macrofollicular Adenoma or Nodule
Hemorrhagic Cyst, Colloid Cyst
Nodule with Regressive Changes
Hemangioma, Myolipoma, Thyroid
Regressive Changes
Calcifications
Irregular |
502 |
Nodular Goiter
Regressive Nodular Goiter
Tumor

|
|
|
|
Differential Diagnosis of |
|
|||
|
|
|
|
|
||||
|
|
|
Hyperthyroidism |
504 |
||||
|
|
|
|
|
Types of Autonomy |
504 |
||
|
|
|
|
|
|
|
Unifocal Autonomy |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Bifocal Autonomy |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Multifocal Autonomy |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Disseminated Autonomy |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|

14Thyroid Gland
G. Schmidt
The thyroid gland is an endocrine gland whose function is to secrete three hormones: tetraiodothyronine (thyroxine, T4), trace amounts of triiodothyronine (T3; most T3 is produced peripherally by the deiodination of T4), and calcitonin. Thyroxine and triiodothyronine are synthesized in the thyrocytes while calcitonin is produced in the C cells of the colloid-contain- ing follicular epithelium.
Thyroid calcitonin plays a key role in bone metabolism along with serum calcium, serum phosphate, and parathormone and is subject to a feedback control mechanism.
An intrathyroid iodine deficiency leads to a numerical increase in the thyrocyte population (follicular hyperplasia), while an increase in thyroid-stimulating hormone (TSH) leads to thyroid enlargement (follicular hypertrophy).
Both processes, then, are responsible in different ways for the development of a goiter.
Ultrasonography is the method of first choice for imaging the thyroid and for evaluating the lymph nodes in the neck and thyroid region. MRI and CT are useful only in selected investigations. Radionuclide scanning (scintigraphy) is best for evaluating focal thyroid lesions and investigating hyperthyroidism.
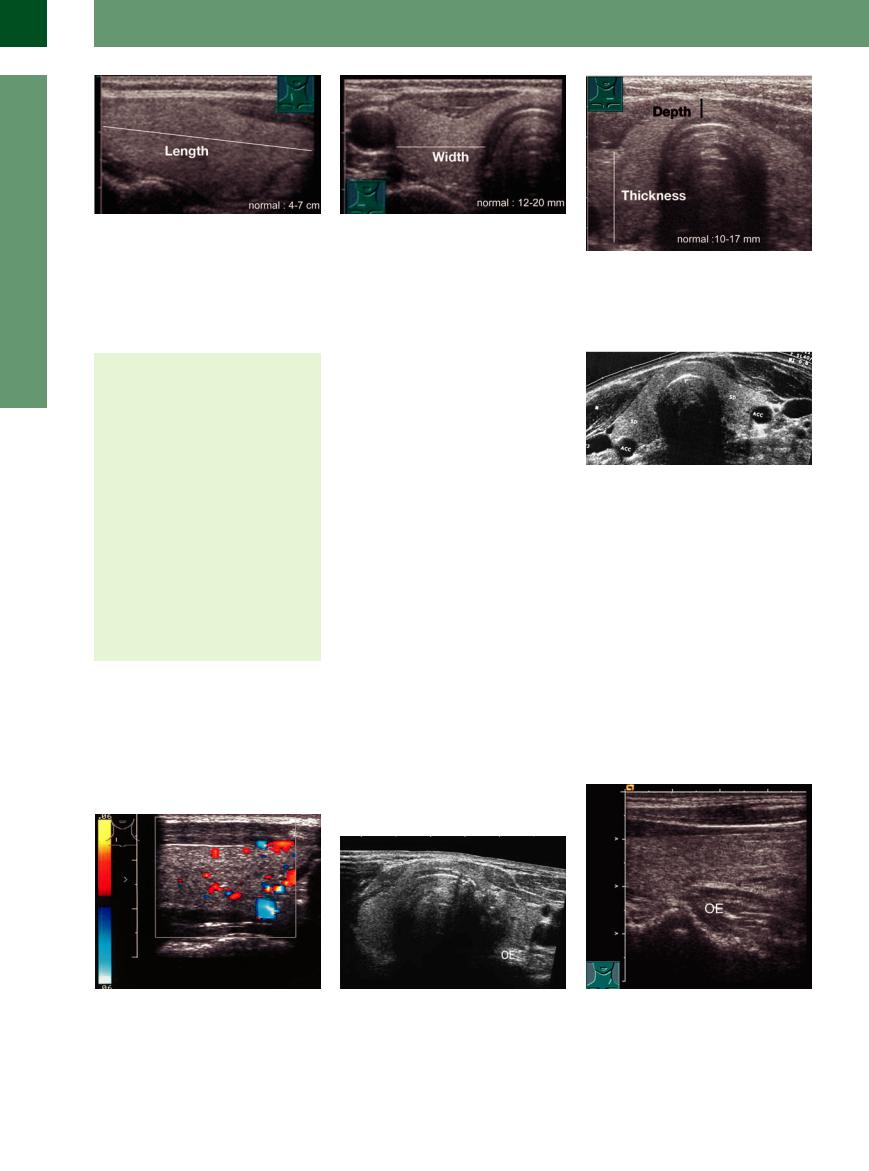
Anatomy























































Shape
●Anterior aspect: butterfly-shaped
●In cross-section: horseshoe-shaped
Size
●AP diameter: 10–17 mm
●Transverse diameter: 12–20 mm
●Length of a thyroid lobe: 40–70 mm
Microanatomy
●Colloid-filled microfollicles, macrofollicles, and normal-sized follicles
●Follicular epithelium composed of thyrocytes and calcitonin cells
Blood supply
●Superior and inferior thyroid arteries (both paired)
When viewed from the front, the thyroid gland has a butterfly shape, with the head represented by the often rudimentary pyramidal lobe and the two wings by the thyroid lobes. The pyramidal lobe is a remnant of the thyroglossal duct present during embryonic development of the thyroid gland from the tongue base. Incomplete obliteration of the thyroglossal duct occasionally results in medial neck cysts.
The thyroid gland is surrounded by muscles. The sternohyoid and sternothyroid muscles are anterior to the thyroid, the sternocleidomas-
Table 14.1 Upper normal limits for sonographic measurements of thyroid volume
Age/sex |
Volume (corresponds to |
|
weight in grams) |
Newborn |
1.5–2 mL |
Up to 2 years |
2–3 mL |
3–4 years |
3 mL |
Up to 6 years |
4 mL |
Up to 10 years |
6 mL |
Up to 12 years |
7 mL |
Up to 14 years |
8–10 mL |
15–18 years |
15 mL |
Adult women |
up to 18 mL |
Adult men |
up to 25 mL |
toid muscles are lateral, and the longus colli muscle is posterior. The blood vessels of the thyroid run through the gland in pairs: the superior thyroid artery above and the inferior thyroid artery below. Lateral to the gland are the common carotid artery and internal jugular vein (Fig.14.1).
Horseshoe shape. While the thyroid gland has a butterfly shape when viewed from the front and by radionuclide scanning, it exhibits a horseshoe shape in the transverse ultrasound scan (Fig.14.2a). The curved arms of the horse-
shoe are formed by the lobes, which are united by the thyroid isthmus. The borders of the thyroid are smooth owing to the presence of the thyroid capsule.
Size. The size of the thyroid gland is determined sonographically by measuring each lobe separately in a transverse scan on the right and left sides (Fig.14.2). This method yields the following approximate dimensions:1 AP depth 10–17 mm, transverse diameter 12–20 mm, longitudinal dimension of each lobe 40–70 mm.
Volume. The volume of the thyroid gland is calculated using the volume formula for a rotational ellipsoid: length of one lobe × width of the lobe × depth × 0.5.
Each thyroid lobe is measured separately and the results are added together to obtain the total volume (the volume of the isthmus is ignored). The normal values for age are shown in Table 14.1. The volume calculation is only an approximation, as it overestimates smaller volumes and underestimates larger volumes. It is difficult to make a reasonably accurate volume measurement in a nodular goiter with poorly defined margins.
Unilateral aplasia is occasionally detected incidentally in adults (previous surgery should be excluded).
Microanatomy of the Thyroid Gland
The microanatomy of the thyroid gland is determined by the follicles. The microfollicles, macrofollicles, and normal-sized follicles range from 50 to 200 μm in size and contain colloid, which consists mainly of thyroglobulin and deposits of monoiodotyrosine and diiodothyrosine. The iodination of thyroglobulin by inorganic iodide to monoiodothyrosine and diiodothyrosine, and probably their coupling to tetra- iodo-thyronine (thyroxine) and triiodothyronine, are catalyzed by the enzyme thyroid peroxidase (TPO).
The single row of epithelial cells in the follicles consists of thyrocytes and calcitonin cells. Even the normal thyroid gland contains thyrocytes, isolated or in aggregates, that are primarily autonomous cells, i. e., not subject to the feedback control system. These cells can proliferate, especially in an iodine-deficient state, and grow into autonomous nodules (adenomas).
Fig. 14.1 Cross-section through the neck at the level of the thyroid gland.
14
Thyroid Gland
477
14
Thyroid Gland
Fig. 14.2 Measuring the size of the thyroid gland (the measuring cursors are shown).
a Length (longitudinal scan on the right side).
b Width (transverse scan through the neck on the right |
c Thickness/depth (transverse scan). |
side). |
|
Topography 





















































Location of the thyroid gland
●Anterior to the first and fourth tracheal rings
●Isthmus and pyramidal lobe at the level of the cricoid cartilage
●Thyroid lobes anterior in the thyroid trigone
●Relates posteriorly to the pharynx and upper esophagus
Location of the parathyroid glands
●Outside the thyroid capsule
●Upper parathyroids at the level of the cricoid cartilage between the trachea and esophagus, on the posterior aspect of the upper third of the thyroid
●Lower parathyroids on the trunk and between the branches of the inferior thyroid artery; on the lateral or posterior aspect of the inferior thyroid pole or at a lower level
The thyroid gland has a horseshoe shape in anatomical cross-section. From anterior to posterior are the cervical fascia followed by the sternohyoid and sternothyroid muscles, the omohyoid muscles anterolaterally, and the
Fig. 14.4 Longitudinal color duplex scan of the right, structurally normal thyroid gland (TH, cursors). The less echogenic anterior neck muscles are visible anteriorly. Normal, scant color spots appear at a low pulse repetition frequency (PRF) corresponding to a flow velocity of 0.06 m/s.
powerful sternocleidomastoid muscles laterally. Posterior to these muscles are the isthmus of the thyroid gland and the left and right thyroid lobes. They are followed posteriorly by the trachea, parathyroid glands, esophagus (a little to the left), and retropharyngeal connective tissue. Behind that, placed lateral to the spinal column, are the longus colli muscles. The relations noted in this anatomical cross-section can be appreciated in the corresponding transverse ultrasound scan and longitudinal scans through each thyroid lobe (Fig.14.3, Fig.14.4). The portion of the upper esophagus behind the thyroid gland is visible posteriorly between the left thyroid lobe and the tracheal acoustic shadow (Fig.14.5).
Vessels. Ultrasound can consistently demonstrate the blood vessels that run in and around the thyroid gland. The common carotid artery and internal jugular vein run lateral to the thyroid. The superior and inferior thyroid arteries that supply the organ are consistently defined at its upper and lower poles in longitudinal scans (Figs. 14.6, 14.7, 14.8).
Parathyroid glands. The four parathyroid glands show frequent variations in their num-
Fig. 14.5 Left lobe of the thyroid gland lying anterior to the cervical part of the esophagus (OE).
a Transverse scan. See also Fig. 14.10.
Fig. 14.3 Topographic relations of the thyroid gland (TH). M = sternocleidomastoid muscle; ACC = common carotid artery; JV = jugular vein; T = trachea. Posterior to the left thyroid lobe is the esophagus (appearing here as a triangular hypoechoic structure). In the right posterolateral quadrant, the inferior thyroid vein enters the jugular vein.
ber and position; usually only two or three are present. They are located on the posterior aspect of the thyroid. Generally the upper parathyroids are extracapsular (rarely intracapsular) and are at the level of the cricoid cartilage between the trachea and esophagus. The lower parathyroids are located on the branches or trunk of the inferior thyroid artery or, in rare cases, directly on the lower poles (see
Fig.14.35, Fig.14.36).
b Longitudinal scan: the anterior wall shows the typical three-part alternation between hypoechoic, hyperechoic, and hypoechoic layers.
478
