
- •Contents
- •Preface
- •Contributors
- •1 Vessels
- •1.1 Aorta, Vena Cava, and Peripheral Vessels
- •Aorta, Arteries
- •Anomalies and Variant Positions
- •Dilatation
- •Stenosis
- •Wall Thickening
- •Intraluminal Mass
- •Perivascular Mass
- •Vena Cava, Veins
- •Anomalies
- •Dilatation
- •Intraluminal Mass
- •Compression, Infiltration
- •1.2 Portal Vein and Its Tributaries
- •Enlarged Lumen Diameter
- •Portal Hypertension
- •Intraluminal Mass
- •Thrombosis
- •Tumor
- •2 Liver
- •Enlarged Liver
- •Small Liver
- •Homogeneous Hypoechoic Texture
- •Homogeneous Hyperechoic Texture
- •Regionally Inhomogeneous Texture
- •Diffuse Inhomogeneous Texture
- •Anechoic Masses
- •Hypoechoic Masses
- •Isoechoic Masses
- •Hyperechoic Masses
- •Echogenic Masses
- •Irregular Masses
- •Differential Diagnosis of Focal Lesions
- •Diagnostic Methods
- •Suspected Diagnosis
- •3 Biliary Tree and Gallbladder
- •3.1 Biliary Tree
- •Thickening of the Bile Duct Wall
- •Localized and Diffuse
- •Bile Duct Rarefaction
- •Localized and Diffuse
- •Bile Duct Dilatation and Intraductal Pressure
- •Intrahepatic
- •Hilar and Prepancreatic
- •Intrapancreatic
- •Papillary
- •Abnormal Intraluminal Bile Duct Findings
- •Foreign Body
- •The Seven Most Important Questions
- •3.2 Gallbladder
- •Changes in Size
- •Large Gallbladder
- •Small/Missing Gallbladder
- •Wall Changes
- •General Hypoechogenicity
- •General Hyperechogenicity
- •General Tumor
- •Focal Tumor
- •Intraluminal Changes
- •Hyperechoic
- •Hypoechoic
- •Nonvisualized Gallbladder
- •Missing Gallbladder
- •Obscured Gallbladder
- •4 Pancreas
- •Diffuse Pancreatic Change
- •Large Pancreas
- •Small Pancreas
- •Hypoechoic Texture
- •Hyperechoic Texture
- •Focal Changes
- •Anechoic Lesion
- •Hypoechoic Lesion
- •Isoechoic Lesion
- •Hyperechoic Lesion
- •Irregular (Complex Structured) Lesion
- •Dilatation of the Pancreatic Duct
- •Marginal/Mild Dilatation
- •Marked Dilatation
- •5 Spleen
- •Nonfocal Changes of the Spleen
- •Diffuse Parenchymal Changes
- •Large Spleen
- •Small Spleen
- •Focal Changes of the Spleen
- •Anechoic Mass
- •Hypoechoic Mass
- •Hyperechoic Mass
- •Splenic Calcification
- •6 Lymph Nodes
- •Peripheral Lymph Nodes
- •Head/Neck
- •Extremities (Axilla, Groin)
- •Abdominal Lymph Nodes
- •Porta Hepatis
- •Splenic Hilum
- •Mesentery (Celiac, Upper and Lower Mesenteric Station)
- •Stomach
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •Small/Large Intestine
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •8 Peritoneal Cavity
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Wall Structures
- •Smooth Margin
- •Irregular Margin
- •Intragastric Processes
- •Intraintestinal Processes
- •9 Kidneys
- •Anomalies, Malformations
- •Aplasia, Hypoplasia
- •Cystic Malformation
- •Anomalies of Number, Position, or Rotation
- •Fusion Anomaly
- •Anomalies of the Renal Calices
- •Vascular Anomaly
- •Diffuse Changes
- •Large Kidneys
- •Small Kidneys
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Irregular Structure
- •Circumscribed Changes
- •Anechoic Structure
- •Hypoechoic or Isoechoic Structure
- •Complex Structure
- •Hyperechoic Structure
- •10 Adrenal Glands
- •Enlargement
- •Anechoic Structure
- •Hypoechoic Structure
- •Complex Echo Structure
- •Hyperechoic Structure
- •11 Urinary Tract
- •Malformations
- •Duplication Anomalies
- •Dilatations and Stenoses
- •Dilated Renal Pelvis and Ureter
- •Anechoic
- •Hypoechoic
- •Hypoechoic
- •Hyperechoic
- •Large Bladder
- •Small Bladder
- •Altered Bladder Shape
- •Intracavitary Mass
- •Hypoechoic
- •Hyperechoic
- •Echogenic
- •Wall Changes
- •Diffuse Wall Thickening
- •Circumscribed Wall Thickening
- •Concavities and Convexities
- •12.1 The Prostate
- •Enlarged Prostate
- •Regular
- •Irregular
- •Small Prostate
- •Regular
- •Echogenic
- •Circumscribed Lesion
- •Anechoic
- •Hypoechoic
- •Echogenic
- •12.2 Seminal Vesicles
- •Diffuse Change
- •Hypoechoic
- •Circumscribed Change
- •Anechoic
- •Echogenic
- •Irregular
- •12.3 Testis, Epididymis
- •Diffuse Change
- •Enlargement
- •Decreased Size
- •Circumscribed Lesion
- •Anechoic or Hypoechoic
- •Irregular/Echogenic
- •Epididymal Lesion
- •Anechoic
- •Hypoechoic
- •Intrascrotal Mass
- •Anechoic or Hypoechoic
- •Echogenic
- •13 Female Genital Tract
- •Masses
- •Abnormalities of Size or Shape
- •Uterus
- •Abnormalities of Size or Shape
- •Myometrial Changes
- •Intracavitary Changes
- •Endometrial Changes
- •Fallopian Tubes
- •Hypoechoic Mass
- •Anechoic Cystic Mass
- •Solid Echogenic or Nonhomogeneous Mass
- •14 Thyroid Gland
- •Diffuse Changes
- •Enlarged Thyroid Gland
- •Small Thyroid Gland
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Circumscribed Changes
- •Anechoic
- •Hypoechoic
- •Isoechoic
- •Hyperechoic
- •Irregular
- •Differential Diagnosis of Hyperthyroidism
- •Types of Autonomy
- •15 Pleura and Chest Wall
- •Chest Wall
- •Masses
- •Parietal Pleura
- •Nodular Masses
- •Diffuse Pleural Thickening
- •Pleural Effusion
- •Anechoic Effusion
- •Echogenic Effusion
- •Complex Effusion
- •16 Lung
- •Masses
- •Anechoic Masses
- •Hypoechoic Masses
- •Complex Masses
- •Index
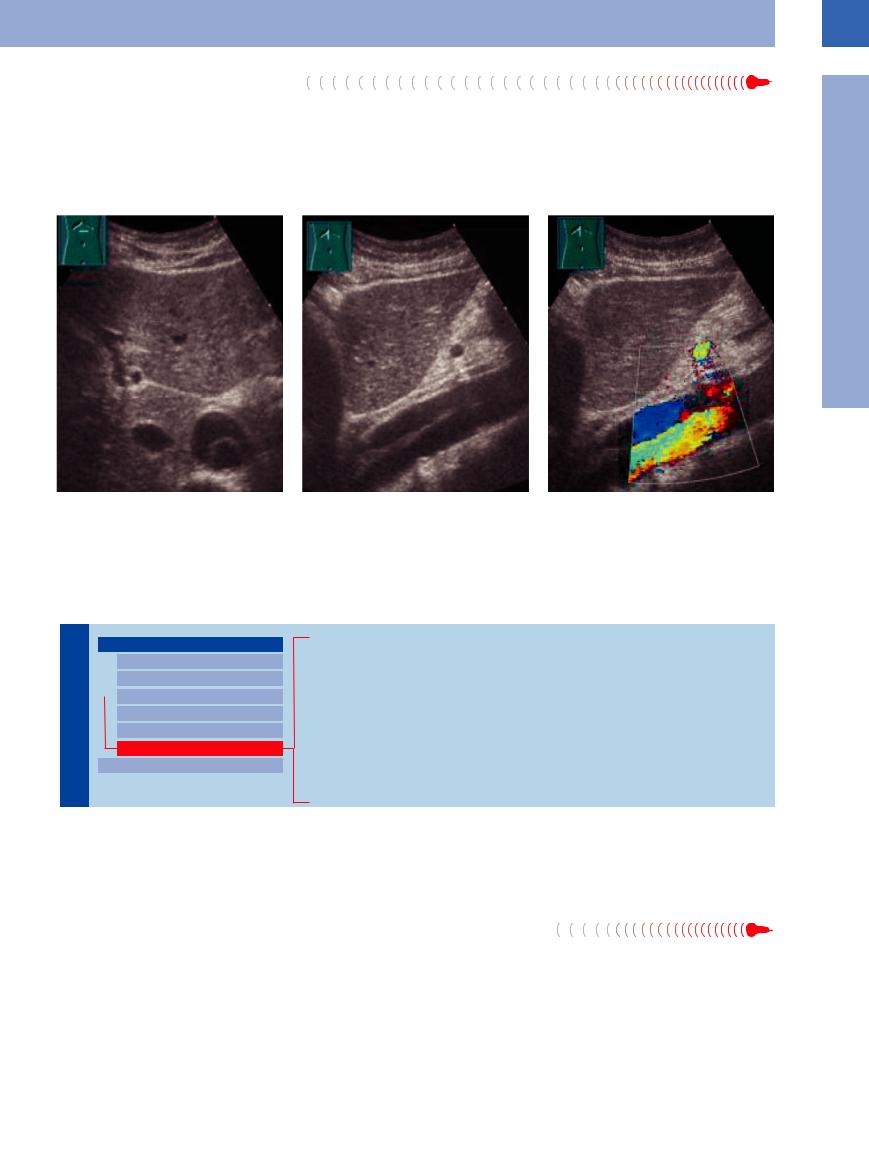
Intimal Dissection








The sonographic image of intimal dissection in the aorta or in aneurysms is similar to that of an endovascular stent; however, most often the patient’s history is known, which then facilitates the differential diagnosis. Furthermore, the intima tends to be thicker and presents as
a solitary echogenic intraluminal band. The origin of the dissection can be identified in only a few cases. An undulating membrane is a typical sign. True and false lumina can be differentiated by contrast-enhanced ultrasound (CEUS): a true lumen presents an early
contrast flow, while a false one presents late. The most important preoperative questions can be answered by CEUS: Are the renal arteries running out of the false lumen and is the kidney perfused? Are the liver and kidneys perfused (Fig.1.51).
1
Aorta, Arteries
Fig. 1.51a–c 58-year-old patient with very severe and uncharacteristic pains in the upper abdomen: dissecting aortal aneurysm. a and b Longitudinal and transverse section, B-mode.
c Longitudinal section, CDS.
Perivascular Mass
Vessels |
|
|
Aorta, Arteries |
|
|
|
|
|
|
|
Anomalies and Variant Positions |
|
|
|
|
|
|
|
Dilatation |
|
|
|
Stenosis |
|
|
|
|
|
|
|
Wall Thickening |
|
|
|
Intraluminal Mass |
|
|
|
Perivascular Mass |
|
|
|
Vena Cava, Veins |
|
|
Pseudoaneurysm
Arteriovenous Fistula/Arteriovenous Malformation
Suture-line Aneurysm
Suture-line Breakdown, Graft Infection
Hematoma, Abscess
Lymphomas, Metastases
Retroperitoneal Fibrosis
Horseshoe Kidney
Intestinal Loop
Perivascular masses may originate from the vessel itself (pseudoaneurysm, suture-line breakdown, graft infection) or arise completely independently of it. Ultrasound plays a vital
role in the differential diagnosis of these diseases. The diagnosis cannot be confirmed in all cases; quite often the clinical picture will yield important clues, and sometimes additional
imaging modalities are required or other diagnostic measures such as ultrasound-guided needle aspiration for cytology and histology.
Pseudoaneurysm 



























A pseudoaneurysm (or false aneurysm) is a |
Doppler scanning the fistula with the perfused |
perivascular mass representing the extravasa- |
aneurysm and the degree of thrombosis can be |
tion of blood after iatrogenic or traumatic in- |
seen directly, while smaller leaks are detected |
jury to the artery. This leads to a perivascular |
particularly well with CEUS. After deliberate |
hematoma with either remaining blood flow or |
compression of the fistula with the ultrasound |
complete thrombosis. Ultrasonography will |
probe for about 20 minutes the canal of the |
demonstrate a hypoechoic mass. In color-flow |
fistula and the aneurysm should become |
thrombosed, thus making open surgery a thing of the past. This does not apply to arteriovenous fistulas.14 The arterial influx can be occluded more rapidly with an ultrasoundguided injection of fibrin glue (Fig.1.52).
25
1
Vessels
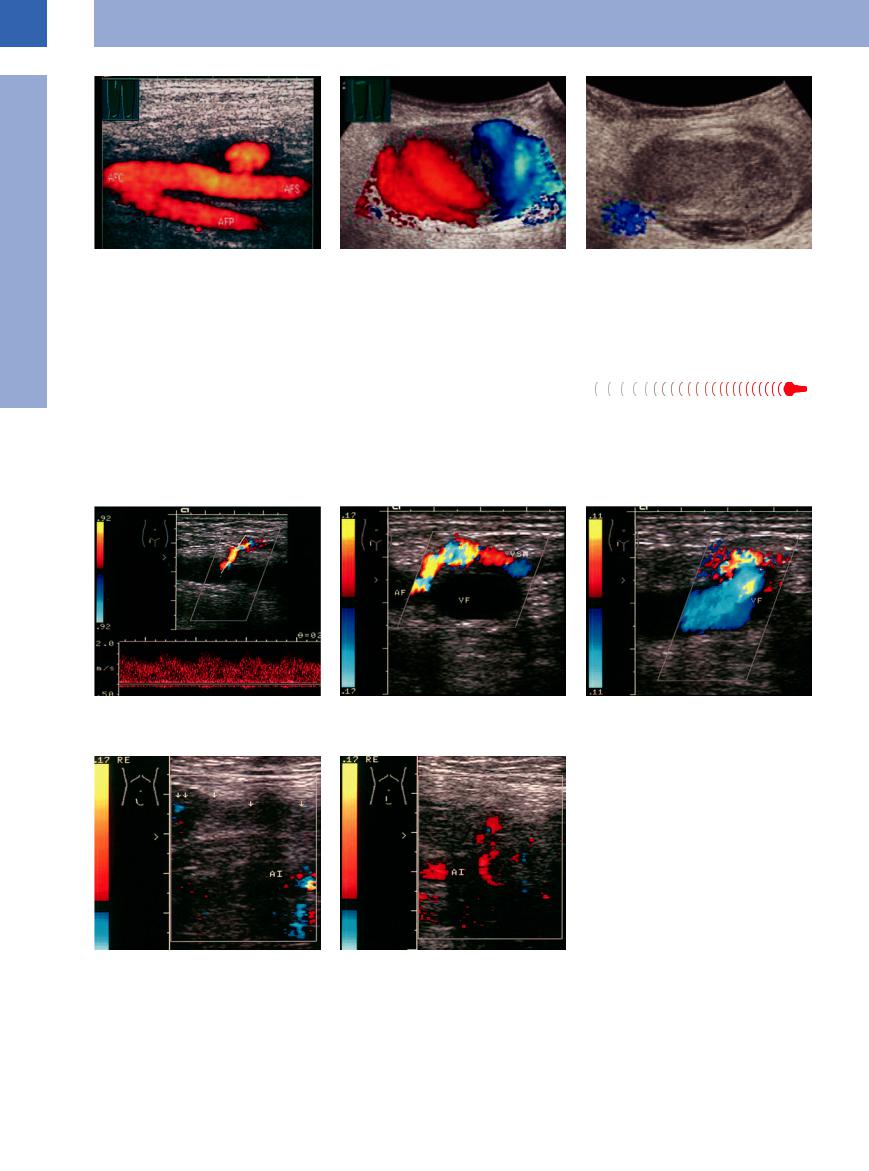
Fig. 1.52a–c Pseudoaneurysm. |
b and c Female patient after catheterization: large false |
c Almost completely thrombosed after compression. |
a False aneurysm (after catheterization): periarterial hy- |
aneurysm. |
|
poechoic mass (CDS; “power Doppler”). Therapeutic op- |
b CDS: red-blue color change caused by altered flow |
|
tions: manual compression, transducer compression, US- |
direction. |
|
guided thrombin injection. AFC, AFS, AFP = common, |
|
|
superficial, deep femoral artery. |
|
|
Arteriovenous Fistula/Arteriovenous
Fistula/Arteriovenous Malformation
Malformation









As is true for pseudoaneurysms, the most common cause of arteriovenous fistulas is iatrogenic (e. g., catheterization); shrapnel injuries have become quite rare. The sonographic diagnosis is derived from the B-mode image and
the arterial signal detected in the vein during duplex scanning.
An arteriovenous malformation is a congenital vascular anomaly in which an artery and vein are interconnected by undifferentiated
vessels without a capillary network. The tangled vessels can be made visible by color duplex and spectral analysis in the presence of a high shunt volume (Fig.1.53, Fig.1.54, see also Fig. 2.69, p. 95).
Fig. 1.53a–c Arteriovenous fistula (F) between the femoral artery (AF) and the greater saphenous vein after catheterization. a Color-flow Doppler spectrum sampled in the fistula with an arterial signal.
b and c Fistula to the greater saphenous vein (VSM/arrow). VF = femoral vein.
Fig. 1.54a and b Arteriovenous malformation.
a Hypoechoic mass (arrows) anterior to and beside the iliac vessels (AI = iliac artery).
b Undifferentiated vessels with low flow in the color duplex scan.
26
Suture-line Aneurysm
Aneurysm
















































In a few cases bypass grafting may be compli- |
ysm, the sonographic finding being the same as |
is confirmed by color-flow duplex scanning. |
cated by the formation of a true or false aneur- |
for the “normal” arterial system. The diagnosis |
|
Suture-line Breakdown,
Breakdown, Graft
Graft Infection
Infection 















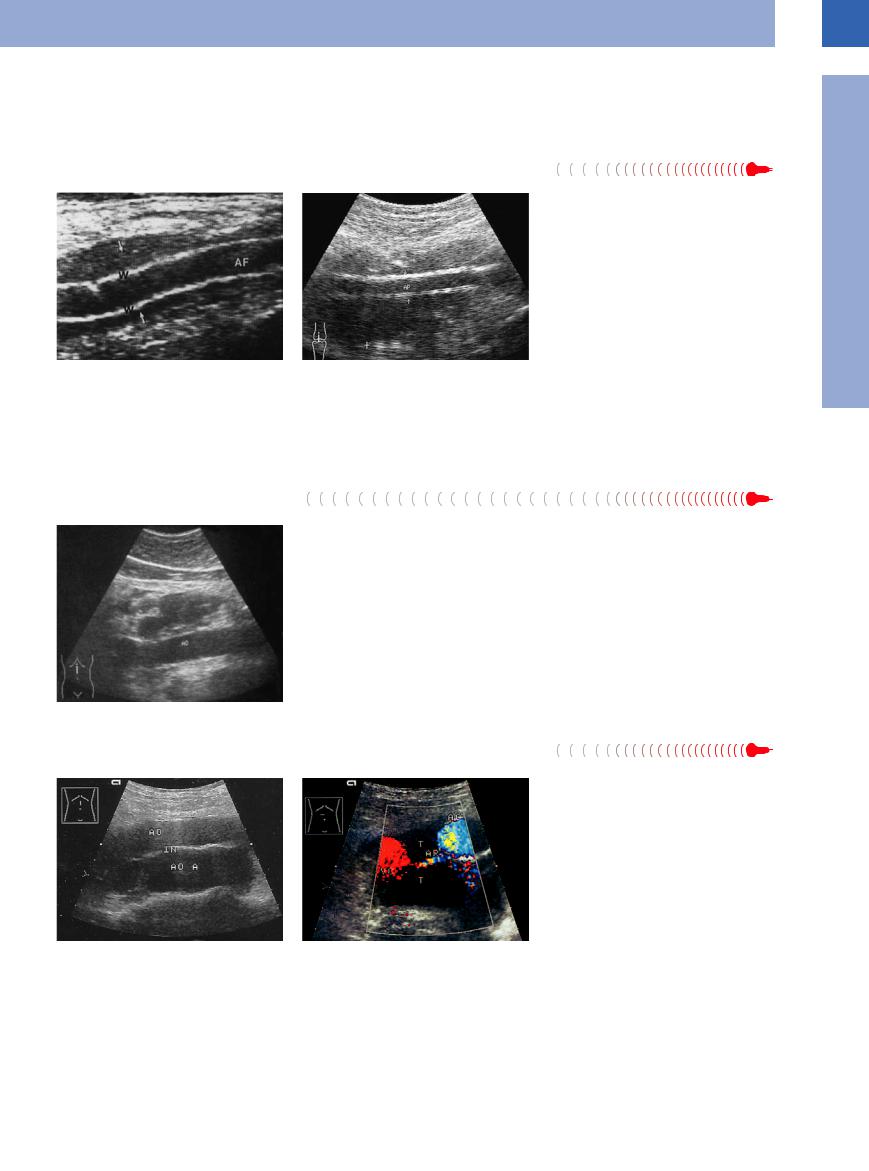
Fig. 1.55
a Leaking femoral graft and infected hematoma. The fluid surrounding the infected graft (arrows) permits excellent insonation of the graft wall (W). Longitudinal section. AF = left femoral artery.
b Infected popliteal graft (arrows; AP) with extensive suppuration (calipers). Clinical signs were fever of unknown origin and possible thrombosis of the popliteal vein.
In most cases postoperative complications after bypass grafting manifest themselves immediately. A delayed onset combined with general symptoms, such as swelling, fever, or sepsis, may be difficult to diagnose.
The typical sonographic appearance of su- ture-line breakdown or graft infection is a hypoechoic perigraft mass; a local, walled-off mass tends to be a hematoma, whereas a bandlike mass is more characteristic of purulent graft infection (Fig.1.55).
Hematoma, Abscess







Fig. 1.56 Postoperative abscess anterior to the aorta after perforated appendicitis. (Clinical picture and possible echogenic gas bubbles, barely seen here, may point the way.) AO = aorta.
There is no clear-cut sonographic distinction between hematoma and abscess presenting as perivascular (aortic) mass, and the sonographer has to rely on the patient’s history and the clinical signs. If the ultrasound findings are ambivalent, sonographically guided fine-nee- dle aspiration may settle the diagnostic issue, possibly followed by therapeutic evacuation of the hematoma or abscess (Fig.1.56).
Lymphomas, Metastases
Metastases 























Malignant lymphoma may appear as hypoechoic para-aortic mass in 50% of cases. Malignant metastases usually are found along the lymphatics draining the tumor and thus may help pinpoint the primary. Whereas metastases are round, lymphomas tend to present a “sandwich” structure (Fig.1.57).
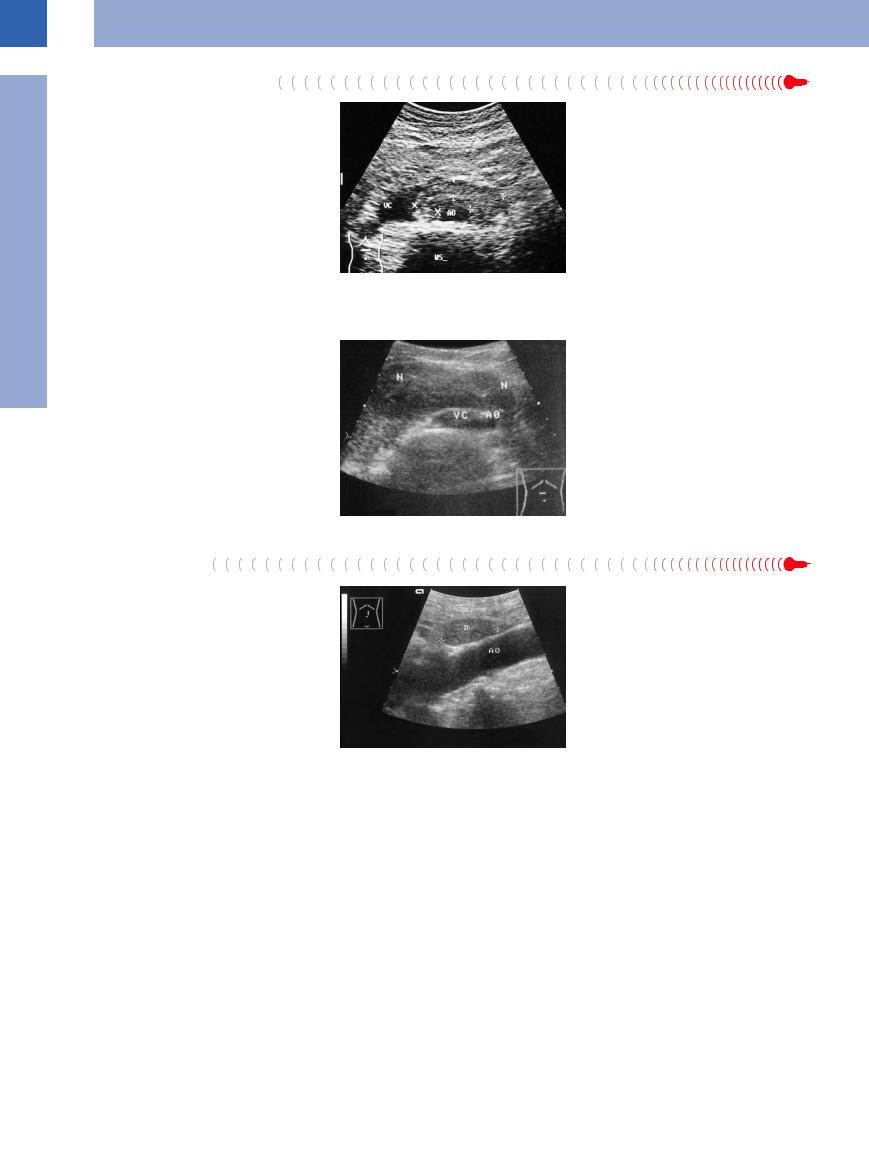
Fig. 1.57 Differential diagnosis aortic aneurysm/para- |
b Periaortic (AO) and pericaval (VC) anechoic lympho- |
aortic mass.23 |
mas (T). The renal artery is drawing throughout the |
a First sonographic diagnosis: dissecting aortic aneur- |
lymphomas. Histologic diagnosis: malignant non-Hodg- |
ysm with dissecting membrane (separated intima = IN). |
kin lymphoma. |
1
Aorta, Arteries
27
1
Vessels
Retroperitoneal Fibrosis
In rare cases a hyperechoic periaortic and pericaval “encasing” mass may be due to retroperitoneal fibrosis, a disease associated with other manifestations (Fig.1.58, also see Chapter 11 “Urinary Tract,” Fig.11.28, p. 391).
Fig. 1.58 Retroperitoneal fibrosis: hypoechoic masses (calipers) encasing the aorta (AO). WS = spine; VC = compressed vena cava.
Horseshoe Kidney
Kidney


















































A hypoechoic mass anterior to the aorta, round or oval (in the transverse diameter), will confirm the diagnosis of a horseshoe kidney, if the study is continued into the flanks and a connection with the kidney becomes evident (Fig.1.59).
Fig. 1.59 Hypoechoic mass resembling lymph nodes anterior to the large abdominal vessels: horseshoe kidney
(N). AO = aorta; VC = vena cava.
Intestinal Loop
Loop
Differential diagnosis of a para-aortic mass has to include the possibility of a hypoechoic intestinal loop distended by fluid. If the mass is observed over a period of time and shows signs of peristalsis, this will settle any doubts (Fig.1.60).
Fig. 1.60 Periaortic “mass”: fluid-filled intestinal loop, differentiation from a true intra-abdominal mass is possible only by its motion. AO = aorta; D = small bowel.
28
