
- •Contents
- •Preface
- •Contributors
- •1 Vessels
- •1.1 Aorta, Vena Cava, and Peripheral Vessels
- •Aorta, Arteries
- •Anomalies and Variant Positions
- •Dilatation
- •Stenosis
- •Wall Thickening
- •Intraluminal Mass
- •Perivascular Mass
- •Vena Cava, Veins
- •Anomalies
- •Dilatation
- •Intraluminal Mass
- •Compression, Infiltration
- •1.2 Portal Vein and Its Tributaries
- •Enlarged Lumen Diameter
- •Portal Hypertension
- •Intraluminal Mass
- •Thrombosis
- •Tumor
- •2 Liver
- •Enlarged Liver
- •Small Liver
- •Homogeneous Hypoechoic Texture
- •Homogeneous Hyperechoic Texture
- •Regionally Inhomogeneous Texture
- •Diffuse Inhomogeneous Texture
- •Anechoic Masses
- •Hypoechoic Masses
- •Isoechoic Masses
- •Hyperechoic Masses
- •Echogenic Masses
- •Irregular Masses
- •Differential Diagnosis of Focal Lesions
- •Diagnostic Methods
- •Suspected Diagnosis
- •3 Biliary Tree and Gallbladder
- •3.1 Biliary Tree
- •Thickening of the Bile Duct Wall
- •Localized and Diffuse
- •Bile Duct Rarefaction
- •Localized and Diffuse
- •Bile Duct Dilatation and Intraductal Pressure
- •Intrahepatic
- •Hilar and Prepancreatic
- •Intrapancreatic
- •Papillary
- •Abnormal Intraluminal Bile Duct Findings
- •Foreign Body
- •The Seven Most Important Questions
- •3.2 Gallbladder
- •Changes in Size
- •Large Gallbladder
- •Small/Missing Gallbladder
- •Wall Changes
- •General Hypoechogenicity
- •General Hyperechogenicity
- •General Tumor
- •Focal Tumor
- •Intraluminal Changes
- •Hyperechoic
- •Hypoechoic
- •Nonvisualized Gallbladder
- •Missing Gallbladder
- •Obscured Gallbladder
- •4 Pancreas
- •Diffuse Pancreatic Change
- •Large Pancreas
- •Small Pancreas
- •Hypoechoic Texture
- •Hyperechoic Texture
- •Focal Changes
- •Anechoic Lesion
- •Hypoechoic Lesion
- •Isoechoic Lesion
- •Hyperechoic Lesion
- •Irregular (Complex Structured) Lesion
- •Dilatation of the Pancreatic Duct
- •Marginal/Mild Dilatation
- •Marked Dilatation
- •5 Spleen
- •Nonfocal Changes of the Spleen
- •Diffuse Parenchymal Changes
- •Large Spleen
- •Small Spleen
- •Focal Changes of the Spleen
- •Anechoic Mass
- •Hypoechoic Mass
- •Hyperechoic Mass
- •Splenic Calcification
- •6 Lymph Nodes
- •Peripheral Lymph Nodes
- •Head/Neck
- •Extremities (Axilla, Groin)
- •Abdominal Lymph Nodes
- •Porta Hepatis
- •Splenic Hilum
- •Mesentery (Celiac, Upper and Lower Mesenteric Station)
- •Stomach
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •Small/Large Intestine
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •8 Peritoneal Cavity
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Wall Structures
- •Smooth Margin
- •Irregular Margin
- •Intragastric Processes
- •Intraintestinal Processes
- •9 Kidneys
- •Anomalies, Malformations
- •Aplasia, Hypoplasia
- •Cystic Malformation
- •Anomalies of Number, Position, or Rotation
- •Fusion Anomaly
- •Anomalies of the Renal Calices
- •Vascular Anomaly
- •Diffuse Changes
- •Large Kidneys
- •Small Kidneys
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Irregular Structure
- •Circumscribed Changes
- •Anechoic Structure
- •Hypoechoic or Isoechoic Structure
- •Complex Structure
- •Hyperechoic Structure
- •10 Adrenal Glands
- •Enlargement
- •Anechoic Structure
- •Hypoechoic Structure
- •Complex Echo Structure
- •Hyperechoic Structure
- •11 Urinary Tract
- •Malformations
- •Duplication Anomalies
- •Dilatations and Stenoses
- •Dilated Renal Pelvis and Ureter
- •Anechoic
- •Hypoechoic
- •Hypoechoic
- •Hyperechoic
- •Large Bladder
- •Small Bladder
- •Altered Bladder Shape
- •Intracavitary Mass
- •Hypoechoic
- •Hyperechoic
- •Echogenic
- •Wall Changes
- •Diffuse Wall Thickening
- •Circumscribed Wall Thickening
- •Concavities and Convexities
- •12.1 The Prostate
- •Enlarged Prostate
- •Regular
- •Irregular
- •Small Prostate
- •Regular
- •Echogenic
- •Circumscribed Lesion
- •Anechoic
- •Hypoechoic
- •Echogenic
- •12.2 Seminal Vesicles
- •Diffuse Change
- •Hypoechoic
- •Circumscribed Change
- •Anechoic
- •Echogenic
- •Irregular
- •12.3 Testis, Epididymis
- •Diffuse Change
- •Enlargement
- •Decreased Size
- •Circumscribed Lesion
- •Anechoic or Hypoechoic
- •Irregular/Echogenic
- •Epididymal Lesion
- •Anechoic
- •Hypoechoic
- •Intrascrotal Mass
- •Anechoic or Hypoechoic
- •Echogenic
- •13 Female Genital Tract
- •Masses
- •Abnormalities of Size or Shape
- •Uterus
- •Abnormalities of Size or Shape
- •Myometrial Changes
- •Intracavitary Changes
- •Endometrial Changes
- •Fallopian Tubes
- •Hypoechoic Mass
- •Anechoic Cystic Mass
- •Solid Echogenic or Nonhomogeneous Mass
- •14 Thyroid Gland
- •Diffuse Changes
- •Enlarged Thyroid Gland
- •Small Thyroid Gland
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Circumscribed Changes
- •Anechoic
- •Hypoechoic
- •Isoechoic
- •Hyperechoic
- •Irregular
- •Differential Diagnosis of Hyperthyroidism
- •Types of Autonomy
- •15 Pleura and Chest Wall
- •Chest Wall
- •Masses
- •Parietal Pleura
- •Nodular Masses
- •Diffuse Pleural Thickening
- •Pleural Effusion
- •Anechoic Effusion
- •Echogenic Effusion
- •Complex Effusion
- •16 Lung
- •Masses
- •Anechoic Masses
- •Hypoechoic Masses
- •Complex Masses
- •Index
■ Diffuse Changes
Diffuse thyroid changes are associated with changes in the size and/or structure of the organ. The enlarged thyroid may show a normal, hyperechoic, or hypoechoic structure, whereas the diffuse structural changes in a normal-sized thyroid are hypoechoic, with few exceptions (e. g., radiation-induced hypothyroidism). Aside from goiters composed of multiple confluent hypoechoic nodules, these
Enlarged Thyroid Gland
diffuse hypoechoic changes always have an inflammatory, immunogenic, or autoimmune etiology.
Micro-, macroand normal-sized follicles as well as blood vessels determine the normal echo structure of the thyroid gland. Changes in the dominant follicle type lead to changes in this echo structure. It is best to evaluate the thyroid structure in relation to the surrounding
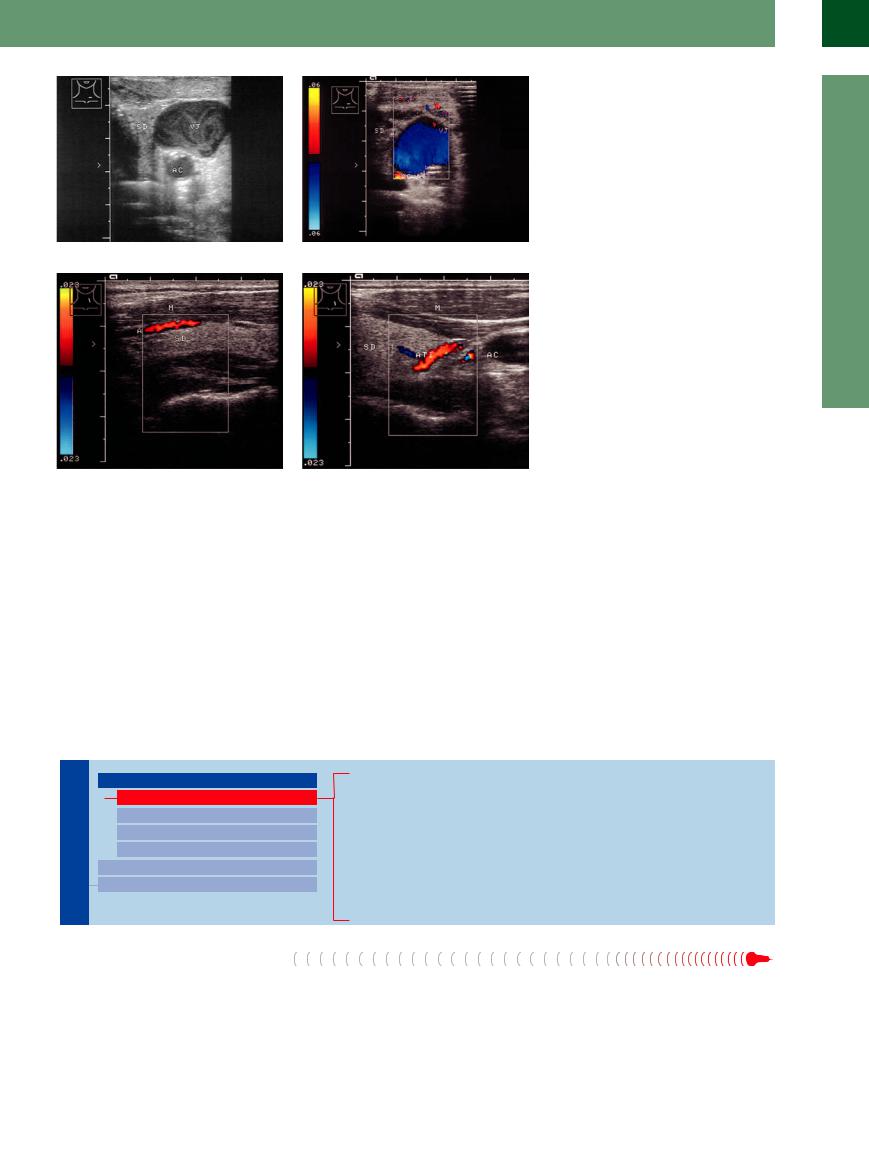
Fig. 14.6a and b Lateral to the thyroid gland (TH) are the internal jugular vein (VJ)—in this case markedly dilated with slow flow due to cardiac congestion—and, posterolaterally, the common carotid artery (AC).
Fig. 14.7 Superior thyroid artery (A) in the upper part of the thyroid gland (TH). M = musculature.
f Fig. 14.8 Inferior thyroid artery (ATI) at the lower pole of the thyroid gland (TH). AC = common carotid artery; M = anterolateral neck muscles.
musculature; otherwise the evaluation is subject to substantial errors. The normal thyroid tissues are more echogenic than the surrounding muscles (Fig.14.4). Several factors determine the echogenicity of the thyroid: the dominant follicle type (see Table 14.2, p. 492), vascularity, inflammation, and any regressive changes that have occurred.
Thyroid Gland

Diffuse Changes
Enlarged Thyroid Gland
Small Thyroid Gland
Hypoechoic Structure
Hyperechoic Structure
Circumscribed Changes
Differential Diagnosis of Hyperthyroidism
Diffuse Parenchymatous Goiter Diffuse Colloid Goiter
Hypertrophic Hashimoto Thyroiditis Hyperthyroidism due to Graves Disease Subacute de Quervain Thyroiditis
Invasive Sclerosing Thyroiditis (Riedel Goiter) Goiter in Acromegaly
Amyloidosis
Diffuse Parenchymatous Goiter
When a goiter is diagnosed clinically, adoles- |
The underlying cause of both diffuse and |
TSH-independent adaptive response consisting |
cents and adults under age 40 are most likely to |
nodular goiters in the United States, Germany, |
of hyperplasia with an increase in follicles, par- |
have a diffuse goiter, whereas older patients |
and several other European countries is a diet- |
ticularly microfollicles. |
will generally have a nodular goiter or less |
ary iodine deficiency. Under the influence of |
|
commonly a cystic or neoplastic disease. |
various growth factors, the thyroid mounts a |
|
14
Diffuse Changes
479
14
Thyroid Gland
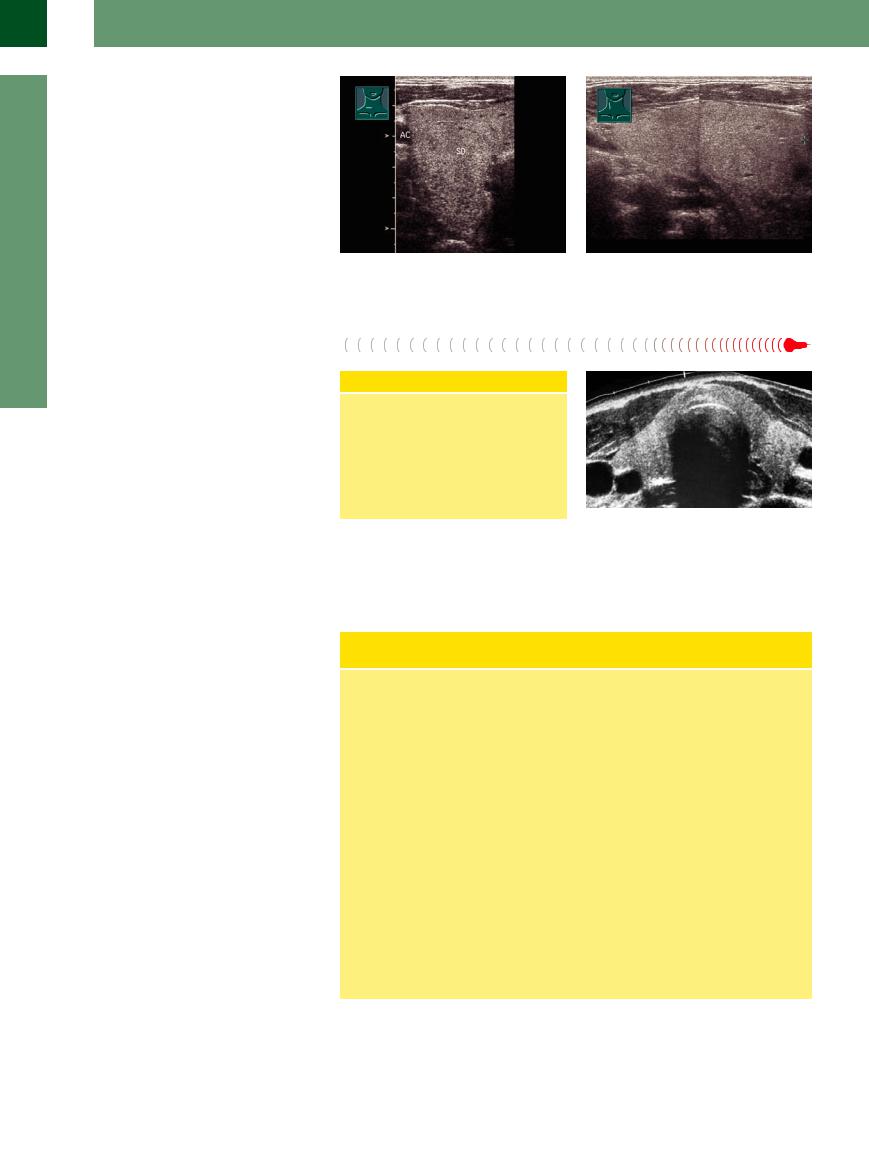
Sonographic features. The sonographic correlate of a diffuse goiter is an enlarged thyroid that retains a normal echo structure. Generally the structure is homogeneous, but circumscribed lesions such as adenomas, cysts, or calcifications may also be seen (Fig.14.9).
Fig. 14.9 Scans of a grade II goiter show greatly enlarged |
b Longitudinal scan on the right side. |
thyroid lobes (SD) with a normal echo structure relative |
|
to muscle tissue. AC= carotid artery. |
|
a Transverse scan on the right side. |
|
Diffuse Colloid Goiter
Goiter






Once hyperplasia of the thyroid has established a hormonal equilibrium, additional colloid storage occurs, causing an irregular increase in the size of the follicles. These macrofollicles and their colloid contents alter the structure of the gland, increasing its echogenicity (Fig.14.10). Sonographically, then, the diffuse colloid goiter appears as an enlarged thyroid gland with a homogeneous hyperechoic structure. This ultrasound finding, with a normal TSH level, justifies the initiation of treatment without further diagnostic tests.
Treatment of Diffuse Goiter
Iodine therapy,2 400 (to 500) g/day for 1 year, then the following maintenance
regimen: |
|
Adults and adolescents |
200 g/day |
School-age children |
140–180 g/day |
Small children |
100–120 g/day |
Pregnant or lactating women
230–260 g/day
Fig. 14.10 Diffuse colloid goiter: enlarged, hyperechoic thyroid (SieScape panoramic image).
Hypertrophic Hashimoto Thyroiditis








































Hashimoto thyroiditis is a type of autoimmune thyroid disease and the leading cause of acquired thyroid hypofunction. A rare hypertrophic form of this disease is distinguished from an atrophic form. Thyroiditis is a general term that refers to inflammation of the thyroid gland. Hashimoto thyroiditis, a chronic lymphocytic form with and without goiter is the most common cause of hypothyroidism in the United States and results in Hashimoto thyroiditis, atrophic autoimmune thyroiditis, and primary myxedema.
Sonographic features. In both the rare hypertrophic form and the atrophic form of autoimmune Hashimoto thyroiditis, ultrasound demonstrates a homogeneous, very echopenic organ that appears isoechoic to the surrounding muscles and has a bulky, often asymmetrical shape. Color duplex examination reveals an intense, speckled hypervascular pattern that is chiefly responsible for the hypoechoic structure (Figs.14.11, 14.19, 14.20).
Morphology, Clinical Aspects, and Immunology of Chronic Lymphocytic Hashimoto
Thyroiditis
Hashimoto thyroiditis is one of a number of autoimmune thyroid diseases. Histologically, the thyroid gland shows diffuse lymphocytic and plasma cell infiltration. Consistent with the immune pathogenesis, antibodies against microsomes are found—specifically against thyroid peroxidase (anti-TPO), always present in high titers. Thyroglobulin antibodies and low titers of TSH receptor-blocking antibodies are also present.
Hyperplastic form. The hyperplastic form of the disease is associated with thyroid enlargement (usually an asymmetrical goiter) and the atrophic form with a decrease in organ size. High anti-TPO titers are always combined histologically with lymphocytic infiltrates, eliminating the need for fine-needle aspiration.
Low titers of anti-TSH receptor antibodies are responsible for a transient hyperthyroid
phase. They also stimulate thyroid growth and cause thyroid enlargement, which presents clinically as an asymmetrical goiter.
Atrophic form. The atrophic form is responsible for nearly 80% of all hypothyroidism in adults. Besides lymphocytic and plasma cell infiltrates, scarring of the thyroid parenchyma is present. Hypothyroid symptoms are mild and progress slowly. Women are affected much more frequently than men.
Myxedema. Myxedema is a rare condition that represents the end stage of Hashimoto thyroiditis. Even with intensive therapy, the prognosis is poor owing to cardiovascular complications; the mortality rate is 70%.
480
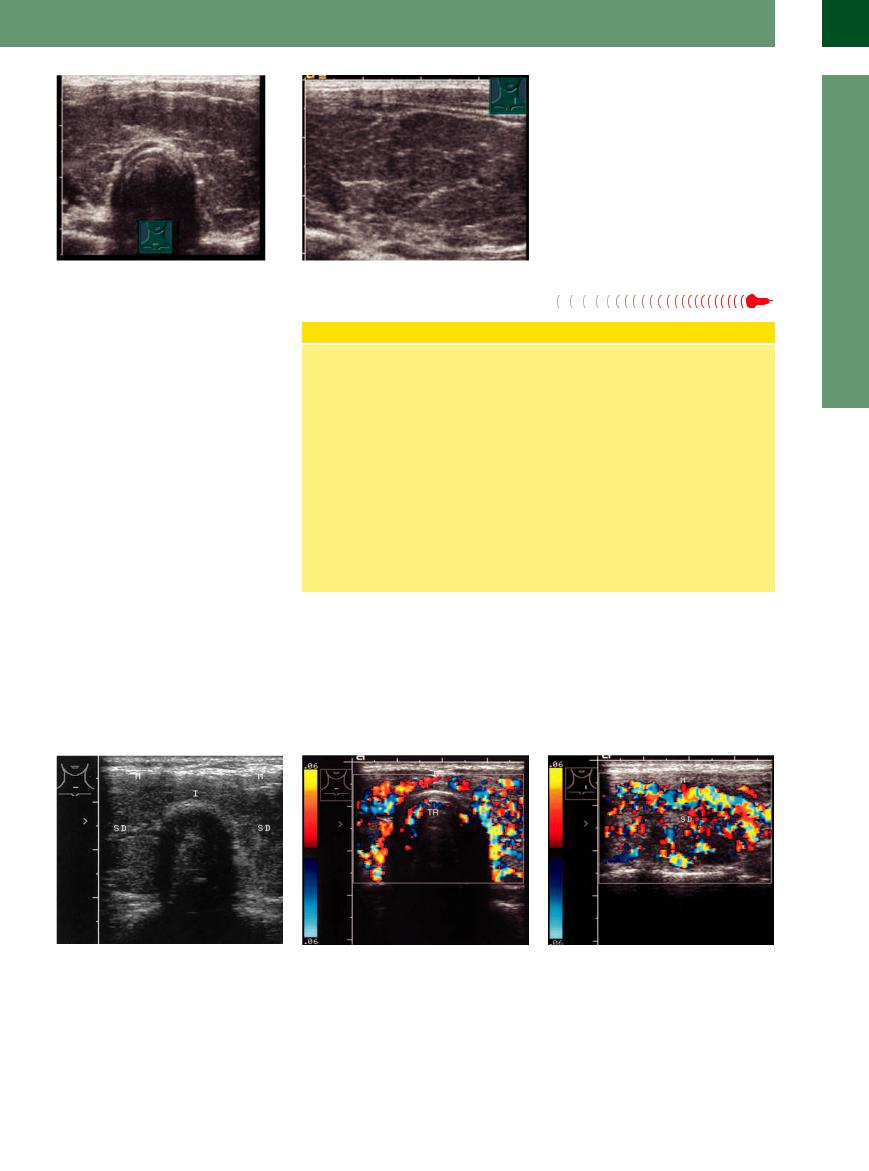
Fig. 14.11a and b Hashimoto goiter, hypertrophic form. TSH elevated, anti-TPO positive. The goiter is hypoechoic to the muscle tissue, and the thyroid gland (TH) is enlarged in both its longitudinal and AP dimensions.
Hyperthyroidism due  to Graves Disease
to Graves Disease















This condition is also commonly known as Graves disease. The term “immunogenic hyperthyroidism” expresses both the autoimmune etiology of the disease and the hyperthyroid state. The hyperthyroidism is frequently associated with extrathyroid manifestations such as endocrine ophthalmopathy and pretibial myxedema. Younger women are predominantly affected. Graves disease is the most frequent cause of hyperthyroidism in adolescents. Diagnosis is generally based on the clinical presentation and laboratory findings (autoantibody detection).
Sonographic features. Ultrasound shows a marked volume increase (up to 90 mL) and symmetrical enlargement of the thyroid. The enlargement includes the isthmus, and this is considered a significant criterion for the disease. The thyroid acquires a rounded, balloonlike appearance (Fig.14.12). The volume dwindles during remissions and increases during recurrences. Because of the rich blood supply, the thyroid shows a diffuse decrease in echogenicity with densely packed hypoechoic areas, resulting in a hypoechoic internal structure.3
Diagnosis of Graves Hyperthyroidism
Clinical features. The typical clinical symptoms present as the classic triad of goiter, exophthalmos, and tachycardia, described by Karl von Basedow in 1840 and Robert Graves in 1835.
Laboratory findings. The hyperthyroidism is confirmed by in-vitro suppression tests showing low TSH and elevated free T4 and T3. Since isolated T3 hyperthyroidism can occur, a T4 determination is insufficient in itself.
TRAbs. Autoantibodies against the TSH receptor (TRAbs) exert a TSH-like effect that directly stimulates the thyrocytes and pro-
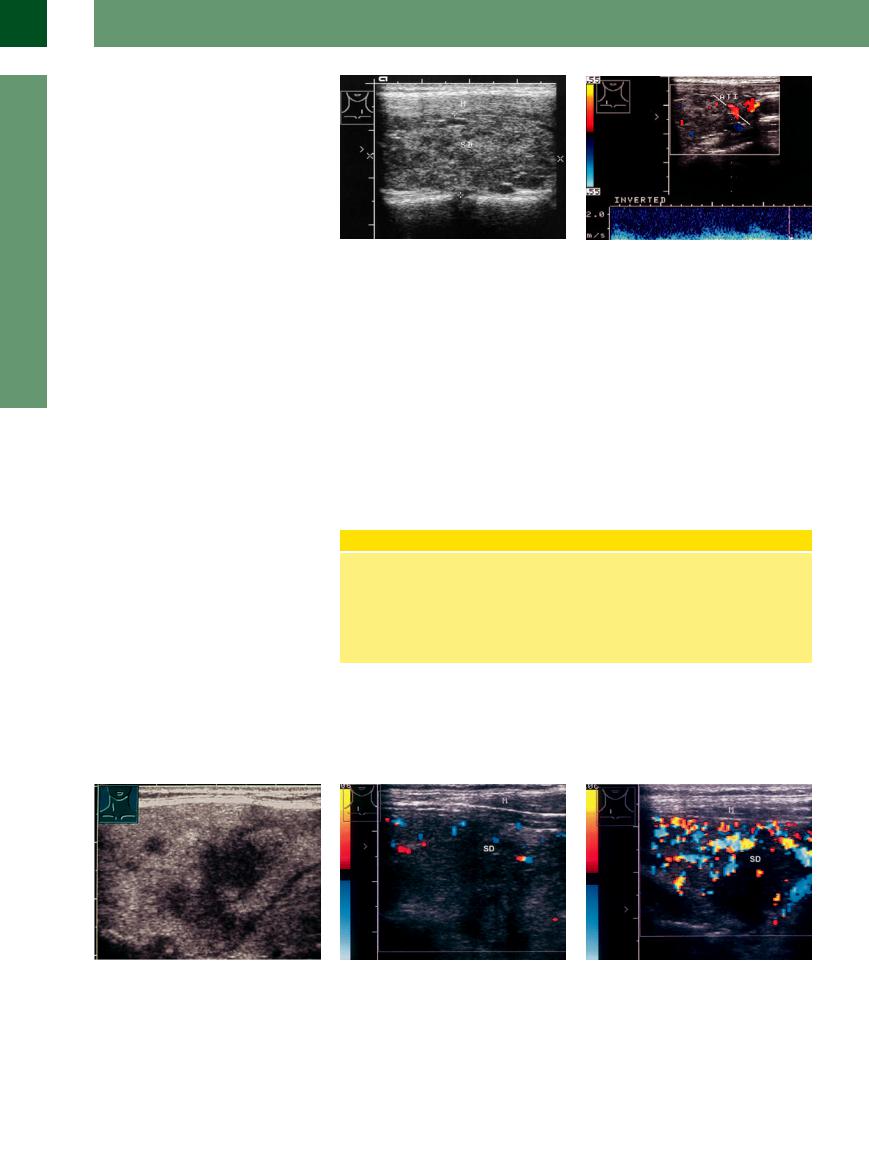
Color Doppler examination. Given the hypervascularity that underlies the characteristic echo structure, color Doppler reveals intense color-flow signals throughout the organ, creating a pattern described as a “thyroid inferno”3 or “vascular inferno” (Fig.14.13, Fig.14.14).
duces a diffuse hyperplasia and hypertrophy of the thyroid follicular epithelium. TRAbs are positive in 90% of patients with Graves disease. They are still positive in 46% of cases following radioiodine therapy and in 2% following excision of a goiter.4
Anti-TPO. Besides TRAbs, low titers of antithyroid peroxidase antibodies (anti-TPO, formerly microsomal antibodies) are found in 76% of cases.
The diagnosis is definite when signs of endocrine ophthalmopathy are seen. Other than thyroid ultrasound, there is no need for further testing.
The internal hypervascularity does not correlate with functional status, however;5 it is due chiefly to inflammation. But the density of the color pixels does correlate strongly with the need for thyrostatic treatment. Another indication for color duplex examination is follow-up, because thyroid blood flow is
14
Diffuse Changes
Fig. 14.12 Graves goiter: balloon-like enlargement of the thyroid gland (TH) with a patchy echopenic structure that is isoechoic to the muscle (M). The markedly enlarged isthmus (I), which crosses over the trachea, is a characteristic feature of Graves disease.
Fig. 14.13 Color Doppler view of a Graves goiter, showing intense hypervascularity (“vascular inferno” pattern). In our experience, the low PRF setting (corresponding to a color Doppler velocity of 0.06 m/s) is optimal for thyroid examinations (it should be lowered to 0.025 m/s only with scant vascularity to detect very slow flows). The Doppler window should encompass the entire thyroid lobe.
a Transverse scan on the midline. TR = trachea.
b Longitudinal scan of the right thyroid lobe (TH). M = muscle.
481
14
Thyroid Gland
significantly higher in patients with a recurrence, and therefore vascularity becomes an important prognostic indicator. The peak flow velocity is also markedly increased to more than 100 cm/s (normal flow velocity 20–40 cm/s) (Fig.14.15). This is best demonstrated by Doppler sampling of the inferior thyroid artery.
Differentiation from autoimmune thyroiditis.
Autoimmune thyroiditis has a similar hypoechoic structure, but Graves goiter is distinguished by a coarser hypoechoic pattern, a more rounded shape due to concomitant isthmic enlargement, and more intense vascularity with a high arterial flow velocity. Autoimmune thyroiditis also shows marked hypoechoicity, but the vascularity on color duplex examination is less pronounced and has a finer texture.
Autonomous nodules. Autonomous nodules in a hyperthyroid Graves goiter, or Graves disease developing on the basis of a nodular goiter (Marine–Lenhart syndrome ( 14.4 p–r), may occur. Autonomous nodules and adenomas do not participate in the autoimmune changes in the Graves thyroid; this confirms their auton-
14.4 p–r), may occur. Autonomous nodules and adenomas do not participate in the autoimmune changes in the Graves thyroid; this confirms their auton-
Fig. 14.14 Graves disease: patchy hypoechoic thyroid gland (TH), isoechoic to the muscle (M) (B-mode image corresponding to Fig. 14.13b).
omous growth and identifies them as true neoplasms in Graves goiters. At the same time, areas of regressive fibrosis may appear as focal lesions.
Diagnosis. The balloon-like shape, grainy hypoechoic texture, and intense vascularity are such typical sonographic features that, when hyperthyroidism is detected, ultrasound can
Fig. 14.15 Color Doppler with spectral analysis in Graves disease. The peak systolic flow velocity in the inferior thyroid artery (ATI) is greatly increased, measuring 1.55 m/s.
establish the diagnosis of Graves goiter even without serology.
Ultrasound yields a correct diagnosis in 74% of patients with Graves disease,6,7 radionuclide scanning in 96%. Given this high sensitivity of ultrasound and the reliability of serological testing, radionuclide scanning is indicated in Graves disease only in cases where ultrasound has additionally detected focal changes.
Subacute de
de Quervain Thyroiditis
Quervain Thyroiditis 









































De Quervain thyroiditis is an acute or subacute viral thyroiditis. Histologically, this form of thyroiditis is distinguished by giant-cell–like granulomas and by scarring in the healing stage. This can also be demonstrated by ultrasoundguided fine-needle aspiration cytology.
Sonographic features. Sonographically, the thyroid enlargement is based mainly on an increase in AP diameter. The isthmus does not appear as prominent as in Graves disease. With regard to echo texture, this type of goiter is distinguished by its intensely hypoechoic structure with a coarse patchy, focal, or diffuse texture (Fig.14.16, Fig.14.17).
Symptoms of de Quervain Thyroiditis
Patients manifest the clinical signs of a viral infection (adenovirus, myxovirus, paramyxovirus) with general malaise, fever, an enlarged thyroid with local tenderness, and laboratory tests positive for inflammation. Patients often describe pain radiation to the neck region. Brief cortisone therapy
Color Doppler sonography. In color Doppler, de Quervain thyroiditis shows inside the hypoechoic parts little or no vascularity, which positively distinguishes it from Graves disease.
can bring dramatic improvement, but most cases resolve spontaneously over a period of weeks or months.
Hyperthyroidism (up to 50%) is often the dominant initial finding.
Contrast-enhanced ultrasound (CEUS) likewise demonstrates reduced vascularity. Unilateral focal lesions may occur (Fig.14.17b; see also
Fig.14.38, Fig.14.39).
Fig. 14.16 De Quervain thyroiditis, female with fever and painful thyroid: patchy hypoechoic thyroid lobes.
Fig. 14.17 De Quervain thyroiditis, right lobe (SD), color duplex. M = muscle; TH = thyroid lobe.
a Patchy low echogenicity with flow voids.
b Four weeks later: regression of swelling, clear delineation of the hypoechoic area, marked increase in vascularity in the rest of the thyroid gland.
482
