
- •Contents
- •Preface
- •Contributors
- •1 Vessels
- •1.1 Aorta, Vena Cava, and Peripheral Vessels
- •Aorta, Arteries
- •Anomalies and Variant Positions
- •Dilatation
- •Stenosis
- •Wall Thickening
- •Intraluminal Mass
- •Perivascular Mass
- •Vena Cava, Veins
- •Anomalies
- •Dilatation
- •Intraluminal Mass
- •Compression, Infiltration
- •1.2 Portal Vein and Its Tributaries
- •Enlarged Lumen Diameter
- •Portal Hypertension
- •Intraluminal Mass
- •Thrombosis
- •Tumor
- •2 Liver
- •Enlarged Liver
- •Small Liver
- •Homogeneous Hypoechoic Texture
- •Homogeneous Hyperechoic Texture
- •Regionally Inhomogeneous Texture
- •Diffuse Inhomogeneous Texture
- •Anechoic Masses
- •Hypoechoic Masses
- •Isoechoic Masses
- •Hyperechoic Masses
- •Echogenic Masses
- •Irregular Masses
- •Differential Diagnosis of Focal Lesions
- •Diagnostic Methods
- •Suspected Diagnosis
- •3 Biliary Tree and Gallbladder
- •3.1 Biliary Tree
- •Thickening of the Bile Duct Wall
- •Localized and Diffuse
- •Bile Duct Rarefaction
- •Localized and Diffuse
- •Bile Duct Dilatation and Intraductal Pressure
- •Intrahepatic
- •Hilar and Prepancreatic
- •Intrapancreatic
- •Papillary
- •Abnormal Intraluminal Bile Duct Findings
- •Foreign Body
- •The Seven Most Important Questions
- •3.2 Gallbladder
- •Changes in Size
- •Large Gallbladder
- •Small/Missing Gallbladder
- •Wall Changes
- •General Hypoechogenicity
- •General Hyperechogenicity
- •General Tumor
- •Focal Tumor
- •Intraluminal Changes
- •Hyperechoic
- •Hypoechoic
- •Nonvisualized Gallbladder
- •Missing Gallbladder
- •Obscured Gallbladder
- •4 Pancreas
- •Diffuse Pancreatic Change
- •Large Pancreas
- •Small Pancreas
- •Hypoechoic Texture
- •Hyperechoic Texture
- •Focal Changes
- •Anechoic Lesion
- •Hypoechoic Lesion
- •Isoechoic Lesion
- •Hyperechoic Lesion
- •Irregular (Complex Structured) Lesion
- •Dilatation of the Pancreatic Duct
- •Marginal/Mild Dilatation
- •Marked Dilatation
- •5 Spleen
- •Nonfocal Changes of the Spleen
- •Diffuse Parenchymal Changes
- •Large Spleen
- •Small Spleen
- •Focal Changes of the Spleen
- •Anechoic Mass
- •Hypoechoic Mass
- •Hyperechoic Mass
- •Splenic Calcification
- •6 Lymph Nodes
- •Peripheral Lymph Nodes
- •Head/Neck
- •Extremities (Axilla, Groin)
- •Abdominal Lymph Nodes
- •Porta Hepatis
- •Splenic Hilum
- •Mesentery (Celiac, Upper and Lower Mesenteric Station)
- •Stomach
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •Small/Large Intestine
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •8 Peritoneal Cavity
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Wall Structures
- •Smooth Margin
- •Irregular Margin
- •Intragastric Processes
- •Intraintestinal Processes
- •9 Kidneys
- •Anomalies, Malformations
- •Aplasia, Hypoplasia
- •Cystic Malformation
- •Anomalies of Number, Position, or Rotation
- •Fusion Anomaly
- •Anomalies of the Renal Calices
- •Vascular Anomaly
- •Diffuse Changes
- •Large Kidneys
- •Small Kidneys
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Irregular Structure
- •Circumscribed Changes
- •Anechoic Structure
- •Hypoechoic or Isoechoic Structure
- •Complex Structure
- •Hyperechoic Structure
- •10 Adrenal Glands
- •Enlargement
- •Anechoic Structure
- •Hypoechoic Structure
- •Complex Echo Structure
- •Hyperechoic Structure
- •11 Urinary Tract
- •Malformations
- •Duplication Anomalies
- •Dilatations and Stenoses
- •Dilated Renal Pelvis and Ureter
- •Anechoic
- •Hypoechoic
- •Hypoechoic
- •Hyperechoic
- •Large Bladder
- •Small Bladder
- •Altered Bladder Shape
- •Intracavitary Mass
- •Hypoechoic
- •Hyperechoic
- •Echogenic
- •Wall Changes
- •Diffuse Wall Thickening
- •Circumscribed Wall Thickening
- •Concavities and Convexities
- •12.1 The Prostate
- •Enlarged Prostate
- •Regular
- •Irregular
- •Small Prostate
- •Regular
- •Echogenic
- •Circumscribed Lesion
- •Anechoic
- •Hypoechoic
- •Echogenic
- •12.2 Seminal Vesicles
- •Diffuse Change
- •Hypoechoic
- •Circumscribed Change
- •Anechoic
- •Echogenic
- •Irregular
- •12.3 Testis, Epididymis
- •Diffuse Change
- •Enlargement
- •Decreased Size
- •Circumscribed Lesion
- •Anechoic or Hypoechoic
- •Irregular/Echogenic
- •Epididymal Lesion
- •Anechoic
- •Hypoechoic
- •Intrascrotal Mass
- •Anechoic or Hypoechoic
- •Echogenic
- •13 Female Genital Tract
- •Masses
- •Abnormalities of Size or Shape
- •Uterus
- •Abnormalities of Size or Shape
- •Myometrial Changes
- •Intracavitary Changes
- •Endometrial Changes
- •Fallopian Tubes
- •Hypoechoic Mass
- •Anechoic Cystic Mass
- •Solid Echogenic or Nonhomogeneous Mass
- •14 Thyroid Gland
- •Diffuse Changes
- •Enlarged Thyroid Gland
- •Small Thyroid Gland
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Circumscribed Changes
- •Anechoic
- •Hypoechoic
- •Isoechoic
- •Hyperechoic
- •Irregular
- •Differential Diagnosis of Hyperthyroidism
- •Types of Autonomy
- •15 Pleura and Chest Wall
- •Chest Wall
- •Masses
- •Parietal Pleura
- •Nodular Masses
- •Diffuse Pleural Thickening
- •Pleural Effusion
- •Anechoic Effusion
- •Echogenic Effusion
- •Complex Effusion
- •16 Lung
- •Masses
- •Anechoic Masses
- •Hypoechoic Masses
- •Complex Masses
- •Index
12
Prostate, Seminal Vesicles, Testis, Epididymis
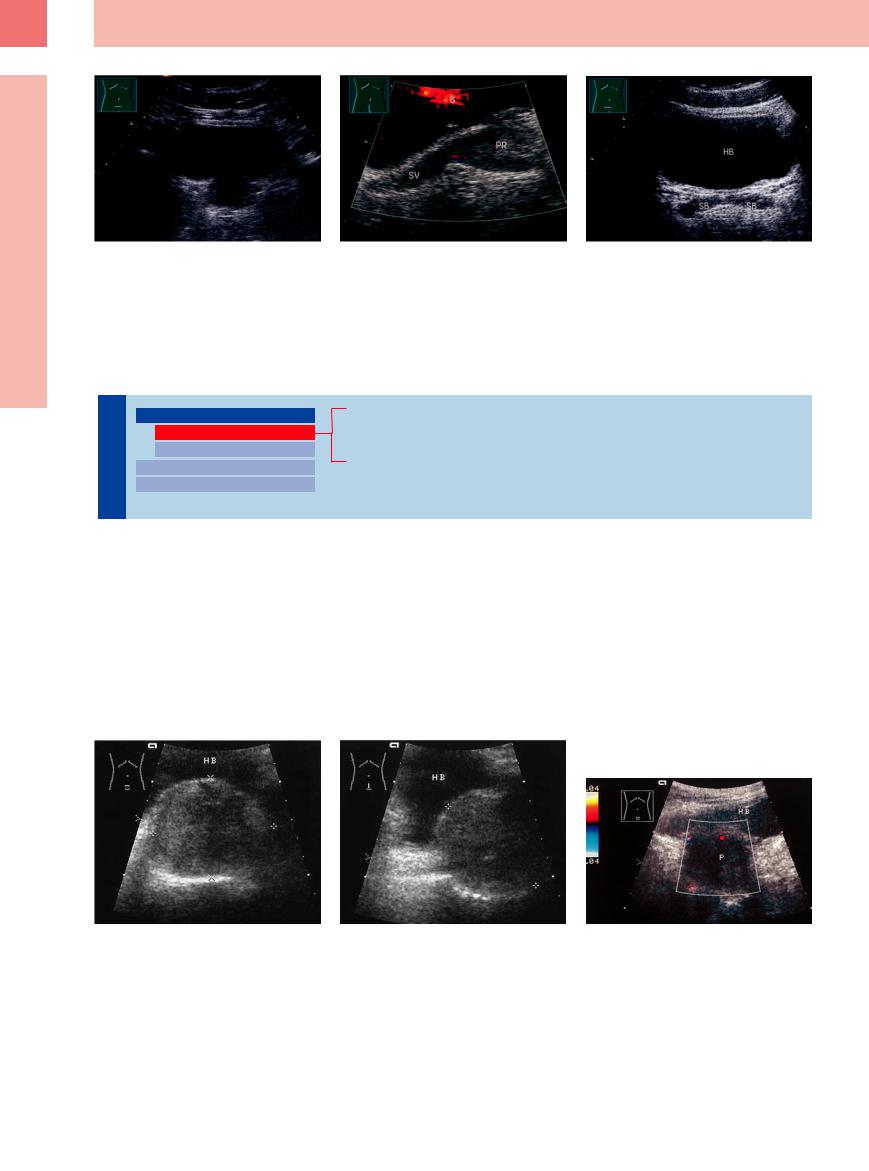
Fig. 12.2 Normal prostate inferior to the bladder. |
b Normal prostate (PR) and seminal vesicles (SV), CDS, |
c Normal (filled) seminal vesicles (SB). HB = bladder. |
a Transverse scan. |
with ureteral jet; longitudinal scan. |
|
■ Enlarged Prostate
Regular
Prostate |
|
|
Enlarged Prostate |
|
|
|
|
||
|
|
|
|
Regular |
|
|
|
|
|
|
|
|
|
Irregular |
The |
|
|
Small Prostate |
|
|
|
|||
|
|
Circumscribed Lesion |
||
|
|
|
||
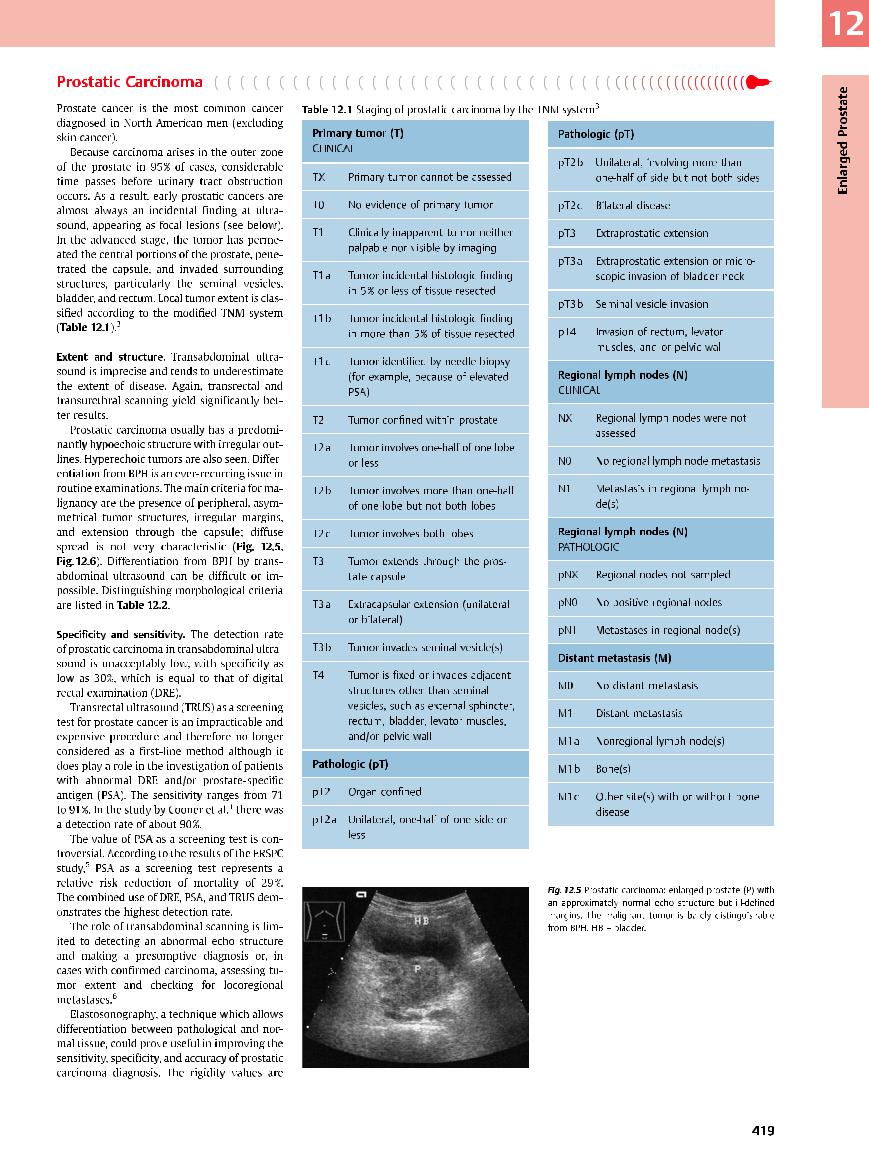
Benign Prostatic Hyperplasia
Prostatic Carcinoma
Acute Prostatitis
Benign Prostatic Hyperplasia
Hyperplasia












































BPH leads to prostatic enlargement that may be either circumscribed (see below) or diffuse. BPH is a nodular proliferation of glandular tissue and stroma (fibrovascular/fibromuscular) of the inner periurethral zone.
The volume of the prostate is determined by multiplying length (longitudinal ultrasound section) × width × depth (in transverse section) and dividing the product by the factor 0.523 (this calculation is already built into scanners
and documentation programs). This formula is fairly accurate in transabdominal ultrasound but is more accurate in transrectal scanning. Here too, however, the measured volume deviates from the actual volume or weight by up to 20%.2 Normal volume is 20 (–25) mL. Enlargement in excess of 80 mL is generally referred for transabdominal prostatectomy. However, estimated size alone is not a reliable
indicator of clinical manifestations, which depend more on the location of the hyperplasia.
A coarser echo texture is seen with diffuse enlargement, consisting of a mixed pattern of hypoechoic and hyperechoic elements. Overall, the affected tissue appears less echogenic than the normal gland; there is no real enhancement in color Doppler sonography (CDS) (Fig.12.3, Fig.12.4).
Fig. 12.3 Benign prostatic hyperplasia (BPH, cursors): ho- |
b Lower abdominal longitudinal section. |
Fig. 12.4 Benign prostatic hyperplasia (P): CDS: no detect- |
mogeneous, hypoechoic enlargement of the prostate, |
|
able vessels. |
smooth shape. Volume = 93 mL. HB = bladder. |
|
|
a Transverse section. |
|
|
418
12
Prostate, Seminal Vesicles, Testis, Epididymis
Table 12.2 Differentiation of prostatic carcinoma from benign prostatic hyperplasia
Prostatic carcinoma |
Benign prostatic hyperplasia |
●Predominantly hypoechoic or irregular structure
●Peripheral asymmetrical tumor structures
●Irregular outlines
●Capsule breached
●Invasion of seminal vesicles, less commonly of the bladder floor
●Locoregional lymphogenous spread, distant metastases
●Prostate shows low central echogenicity with rounded outlines
●Central hypoechoic tumor structure in the median lobe, indenting the bladder floor
●Smooth outlines
●Capsule intact
●Displacement, atrophy, and encapsulation of normal peripheral glandular tissue
●Possible echo-free or echogenic areas
Clinical Diagnosis of Prostatic Carcinoma6
An effective early diagnostic procedure for prostatic carcinoma consists of DRE with assessment of overall size, median sulcus, surface characteristics, and consistency (a circumscribed or diffuse “stony hard” consistency is suggestive of malignancy), combined with the determination of PSA. If induration is noted at palpation and the PSA is between 4 ng/mL (upper normal limit in men > 60 years of age; lower in younger men) and 10 ng/mL, there is a 41% chance that carcinoma is present. With a PSA in excess of 10 ng/mL, this rises to 72%. The incidence of carcinoma is 69% in cases where a hard, discrete nodule is
found in the prostate, and 91% when the corresponding PSA is higher than 10 ng/ mL. Thus, the digital findings and PSA are both critical in the detection of prostate cancer.
Transurethral sonography can support a presumptive diagnosis of carcinoma, and core biopsy can confirm the diagnosis. Even with a negative histology, however, a high PSA is still considered suspicious for carcinoma, as it is a specific tumor marker. It is extremely rare for a histological prostatic malignancy to be identified as a sarcoma or malignant lymphoma.
depicted in different colors—maximum values |
mas can be discriminated from normal pro- |
in dark blue, soft tissue ranging from green- |
static tissue (see Fig.12.10). |
yellow to red (vessels)—so that hard carcino- |
|
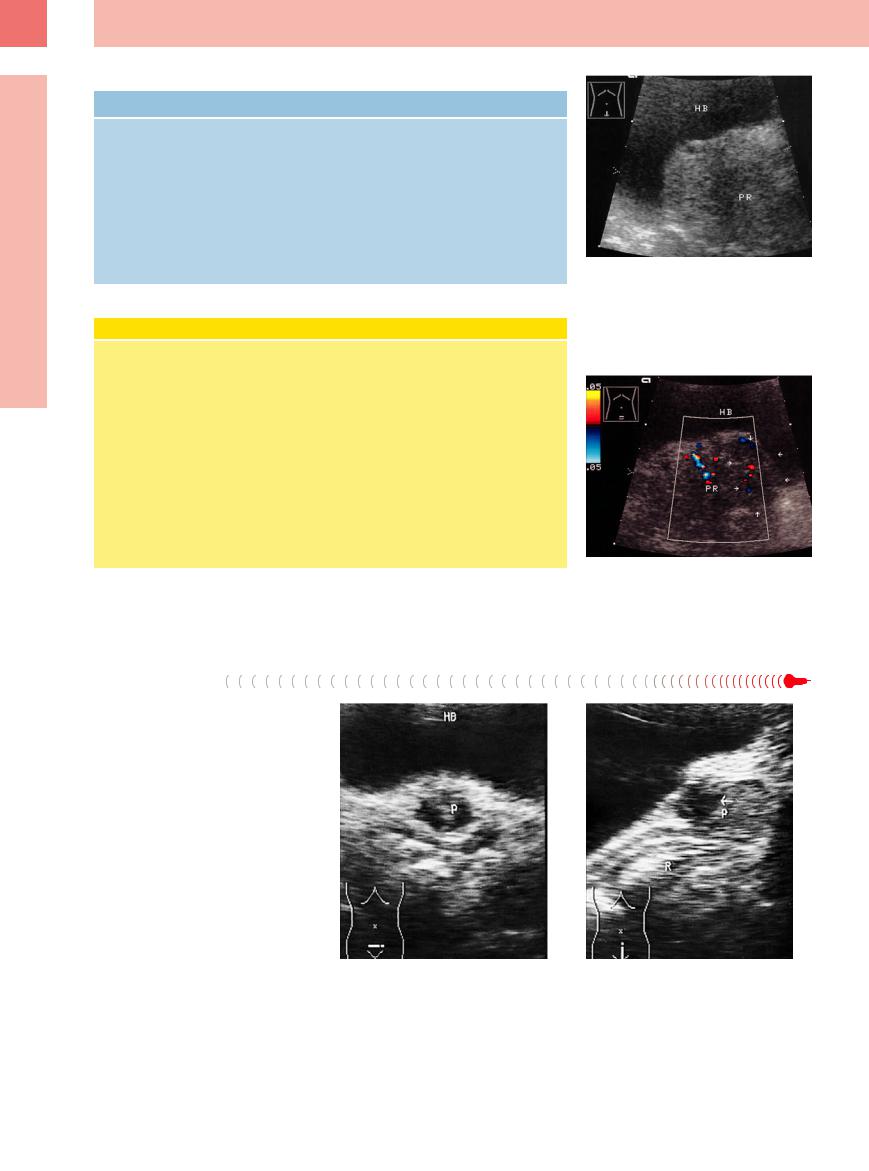
Fig. 12.6 Hypoechoic, predominantly diffuse prostatic enlargement. A circumscribed hard consistency was noted on digital rectal examination, raising strong suspicion of carcinoma. HB = bladder; PR = prostate.
a Lower abdominal longitudinal scan: enlarged prostate indenting the bladder floor, slightly less echogenic inferiorly, consistent with a tumor.
b Lower abdominal transverse scan with color Doppler: subtle echopenic area on the left side (arrows) with atypical vascularity, creating a very high index of suspicion.
Acute Prostatitis
Five different histopathologic types of prostatitis1 can underlie the rather nonspecific symptom complex of pain, aching, burning, or pressure in the anorectal or urogenital region. Chronic complaints are often referable to a functional “prostatodynia,” however.
Ultrasonography in acute prostatitis shows edematous swelling and rounding of the gland, which has a hypoechoic structure. Focal lesions (see below) may also be seen. The diagnosis is based on the clinical presentation plus corresponding sonographic findings or the detection of a causative microorganism. Swollen, hypoechoic seminal vesicles indicate concomitant inflammatory involvement of those glands (Fig.12.7).
Fig. 12.7 Prostatitis (P). |
b Lower abdominal longitudinal scan shows a small pros- |
a Lower abdominal transverse scan shows a largely an- |
tate with a mottled hypoechoic texture and an anechoic |
echoic mass. HB = bladder. |
cystic mass (arrow). The rectum (R) appears posteriorly. |
420
Histopathologic Forms of Prostatitis |
|
|
● Purulent bacterial prostatitis, which is |
● Chronic nonspecific prostatitis, in |
● Tuberculous prostatitis, which is asso- |
often associated with abscess formation. |
which the stasis of secretions with the |
ciated with foci of caseous liquefaction. |
● Gonorrheal prostatitis, once the most |
formation of amyloid bodies can lead to |
|
common form, now rare. |
secondary calcification and thus to pros- |
|
● Granulomatous prostatitis, usually |
tatolithiasis and inflammation. It is diag- |
|
with an abacterial or allergic cause, |
nosed by detecting the causative organ- |
|
marked histopathologically by destruc- |
ism in fluid sampled by “milking” the |
|
tive foci, giant cells, histiocytes, and fi- |
gland. |
|
broblasts. |
|
|
Irregular
Prostate |
|
|
|
Enlarged Prostate |
|
|
|
|
|
||
|
|
|
|
|
Regular |
|
|
|
|
|
Irregular |
|
|
|
|
|
|
The |
|
|
|
Small Prostate |
|
|
|
|
|||
|
|
|
Circumscribed Lesion |
||
|
|
|
|
||
Benign Prostatic Hyperplasia
Prostatic Carcinoma
Chronic Prostatitis
Benign Prostatic Hyperplasia
Hyperplasia












































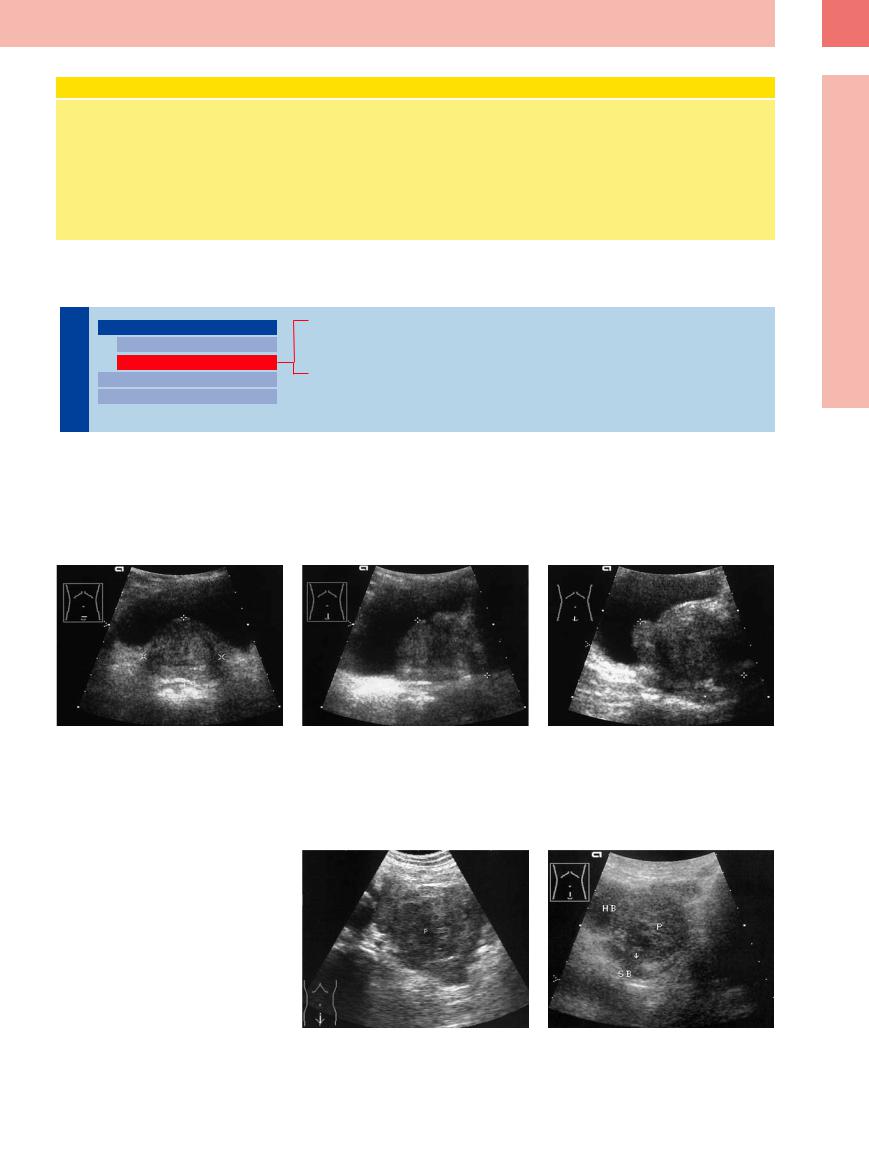
Varying proportions of stromal or glandular |
derance of glandular elements creates a more |
tions, secretory stones, and anechoic cystic |
elements affect the echo structure of BPH: a |
isoechoic or hyperechoic appearance relative |
areas are also seen (Fig.12.8). |
preponderance of stroma causes the hyperpla- |
to the normal prostate. The result is an irregu- |
|
sia to appear more hypoechoic, while a prepon- |
lar sonographic pattern. Hyperechoic calcifica- |
|
12
Enlarged Prostate
Fig. 12.8 Benign prostatic hyperplasia (cursors): opposite the displaced remaining prostatic tissue and defined by a hyperechoid line, the adenoma appears more hypoechoic.
a and b Hyperplasia of the posterosuperior median lobe; volume 50 mL, biopsy because of elevated PSA: no carcinoma.
c Prostatic adenoma (histology), indenting the bladder floor; volume 103 mL: acute urinary retention.
Prostatic Carcinoma
Carcinoma

















































BPH and prostatic carcinoma may present a predominantly homogeneous echo texture or a markedly irregular structure. The latter is particularly apt to occur when carcinoma is accompanied by adenomatous hyperplasia and/or fibrous, cystic, or calcifying prostatic elements. These different components cannot be distinguished by their transabdominal morphological features (Fig.12.9, Fig.12.10).
Fig. 12.9
a Advanced prostatic carcinoma (P), which has already metastasized. Scan shows a large, tumorous prostate with irregular borders, a coarse hypoechoic texture, and tumor extension through the prostatic capsule.
b Prostatic carcinoma (P), lower abdominal longitudinal scan: invasion of the seminal vesicle (SB), indicating a T3 tumor by ultrasound. HB = bladder.
421
