
- •Contents
- •Preface
- •Contributors
- •1 Vessels
- •1.1 Aorta, Vena Cava, and Peripheral Vessels
- •Aorta, Arteries
- •Anomalies and Variant Positions
- •Dilatation
- •Stenosis
- •Wall Thickening
- •Intraluminal Mass
- •Perivascular Mass
- •Vena Cava, Veins
- •Anomalies
- •Dilatation
- •Intraluminal Mass
- •Compression, Infiltration
- •1.2 Portal Vein and Its Tributaries
- •Enlarged Lumen Diameter
- •Portal Hypertension
- •Intraluminal Mass
- •Thrombosis
- •Tumor
- •2 Liver
- •Enlarged Liver
- •Small Liver
- •Homogeneous Hypoechoic Texture
- •Homogeneous Hyperechoic Texture
- •Regionally Inhomogeneous Texture
- •Diffuse Inhomogeneous Texture
- •Anechoic Masses
- •Hypoechoic Masses
- •Isoechoic Masses
- •Hyperechoic Masses
- •Echogenic Masses
- •Irregular Masses
- •Differential Diagnosis of Focal Lesions
- •Diagnostic Methods
- •Suspected Diagnosis
- •3 Biliary Tree and Gallbladder
- •3.1 Biliary Tree
- •Thickening of the Bile Duct Wall
- •Localized and Diffuse
- •Bile Duct Rarefaction
- •Localized and Diffuse
- •Bile Duct Dilatation and Intraductal Pressure
- •Intrahepatic
- •Hilar and Prepancreatic
- •Intrapancreatic
- •Papillary
- •Abnormal Intraluminal Bile Duct Findings
- •Foreign Body
- •The Seven Most Important Questions
- •3.2 Gallbladder
- •Changes in Size
- •Large Gallbladder
- •Small/Missing Gallbladder
- •Wall Changes
- •General Hypoechogenicity
- •General Hyperechogenicity
- •General Tumor
- •Focal Tumor
- •Intraluminal Changes
- •Hyperechoic
- •Hypoechoic
- •Nonvisualized Gallbladder
- •Missing Gallbladder
- •Obscured Gallbladder
- •4 Pancreas
- •Diffuse Pancreatic Change
- •Large Pancreas
- •Small Pancreas
- •Hypoechoic Texture
- •Hyperechoic Texture
- •Focal Changes
- •Anechoic Lesion
- •Hypoechoic Lesion
- •Isoechoic Lesion
- •Hyperechoic Lesion
- •Irregular (Complex Structured) Lesion
- •Dilatation of the Pancreatic Duct
- •Marginal/Mild Dilatation
- •Marked Dilatation
- •5 Spleen
- •Nonfocal Changes of the Spleen
- •Diffuse Parenchymal Changes
- •Large Spleen
- •Small Spleen
- •Focal Changes of the Spleen
- •Anechoic Mass
- •Hypoechoic Mass
- •Hyperechoic Mass
- •Splenic Calcification
- •6 Lymph Nodes
- •Peripheral Lymph Nodes
- •Head/Neck
- •Extremities (Axilla, Groin)
- •Abdominal Lymph Nodes
- •Porta Hepatis
- •Splenic Hilum
- •Mesentery (Celiac, Upper and Lower Mesenteric Station)
- •Stomach
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •Small/Large Intestine
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •8 Peritoneal Cavity
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Wall Structures
- •Smooth Margin
- •Irregular Margin
- •Intragastric Processes
- •Intraintestinal Processes
- •9 Kidneys
- •Anomalies, Malformations
- •Aplasia, Hypoplasia
- •Cystic Malformation
- •Anomalies of Number, Position, or Rotation
- •Fusion Anomaly
- •Anomalies of the Renal Calices
- •Vascular Anomaly
- •Diffuse Changes
- •Large Kidneys
- •Small Kidneys
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Irregular Structure
- •Circumscribed Changes
- •Anechoic Structure
- •Hypoechoic or Isoechoic Structure
- •Complex Structure
- •Hyperechoic Structure
- •10 Adrenal Glands
- •Enlargement
- •Anechoic Structure
- •Hypoechoic Structure
- •Complex Echo Structure
- •Hyperechoic Structure
- •11 Urinary Tract
- •Malformations
- •Duplication Anomalies
- •Dilatations and Stenoses
- •Dilated Renal Pelvis and Ureter
- •Anechoic
- •Hypoechoic
- •Hypoechoic
- •Hyperechoic
- •Large Bladder
- •Small Bladder
- •Altered Bladder Shape
- •Intracavitary Mass
- •Hypoechoic
- •Hyperechoic
- •Echogenic
- •Wall Changes
- •Diffuse Wall Thickening
- •Circumscribed Wall Thickening
- •Concavities and Convexities
- •12.1 The Prostate
- •Enlarged Prostate
- •Regular
- •Irregular
- •Small Prostate
- •Regular
- •Echogenic
- •Circumscribed Lesion
- •Anechoic
- •Hypoechoic
- •Echogenic
- •12.2 Seminal Vesicles
- •Diffuse Change
- •Hypoechoic
- •Circumscribed Change
- •Anechoic
- •Echogenic
- •Irregular
- •12.3 Testis, Epididymis
- •Diffuse Change
- •Enlargement
- •Decreased Size
- •Circumscribed Lesion
- •Anechoic or Hypoechoic
- •Irregular/Echogenic
- •Epididymal Lesion
- •Anechoic
- •Hypoechoic
- •Intrascrotal Mass
- •Anechoic or Hypoechoic
- •Echogenic
- •13 Female Genital Tract
- •Masses
- •Abnormalities of Size or Shape
- •Uterus
- •Abnormalities of Size or Shape
- •Myometrial Changes
- •Intracavitary Changes
- •Endometrial Changes
- •Fallopian Tubes
- •Hypoechoic Mass
- •Anechoic Cystic Mass
- •Solid Echogenic or Nonhomogeneous Mass
- •14 Thyroid Gland
- •Diffuse Changes
- •Enlarged Thyroid Gland
- •Small Thyroid Gland
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Circumscribed Changes
- •Anechoic
- •Hypoechoic
- •Isoechoic
- •Hyperechoic
- •Irregular
- •Differential Diagnosis of Hyperthyroidism
- •Types of Autonomy
- •15 Pleura and Chest Wall
- •Chest Wall
- •Masses
- •Parietal Pleura
- •Nodular Masses
- •Diffuse Pleural Thickening
- •Pleural Effusion
- •Anechoic Effusion
- •Echogenic Effusion
- •Complex Effusion
- •16 Lung
- •Masses
- •Anechoic Masses
- •Hypoechoic Masses
- •Complex Masses
- •Index
Small Spleen
Spleen |
Nonfocal Changes of the Spleen |
|||||
|
|
|
|
|
||
|
|
|
|
|
|
Diffuse Parenchymal Changes |
|
|
|
|
|
|
Large Spleen |
|
|
|
|
|
|
Small Spleen |
|
|
|
|
|
|
|
|
|
|
|
|
Focal Changes of the Spleen |
|
|
|
|
|
|
||
Variants, “Aged Spleen”
Functional Hyposplenism/Asplenia
Variants, “Aged Spleen”
“Aged Spleen” 














































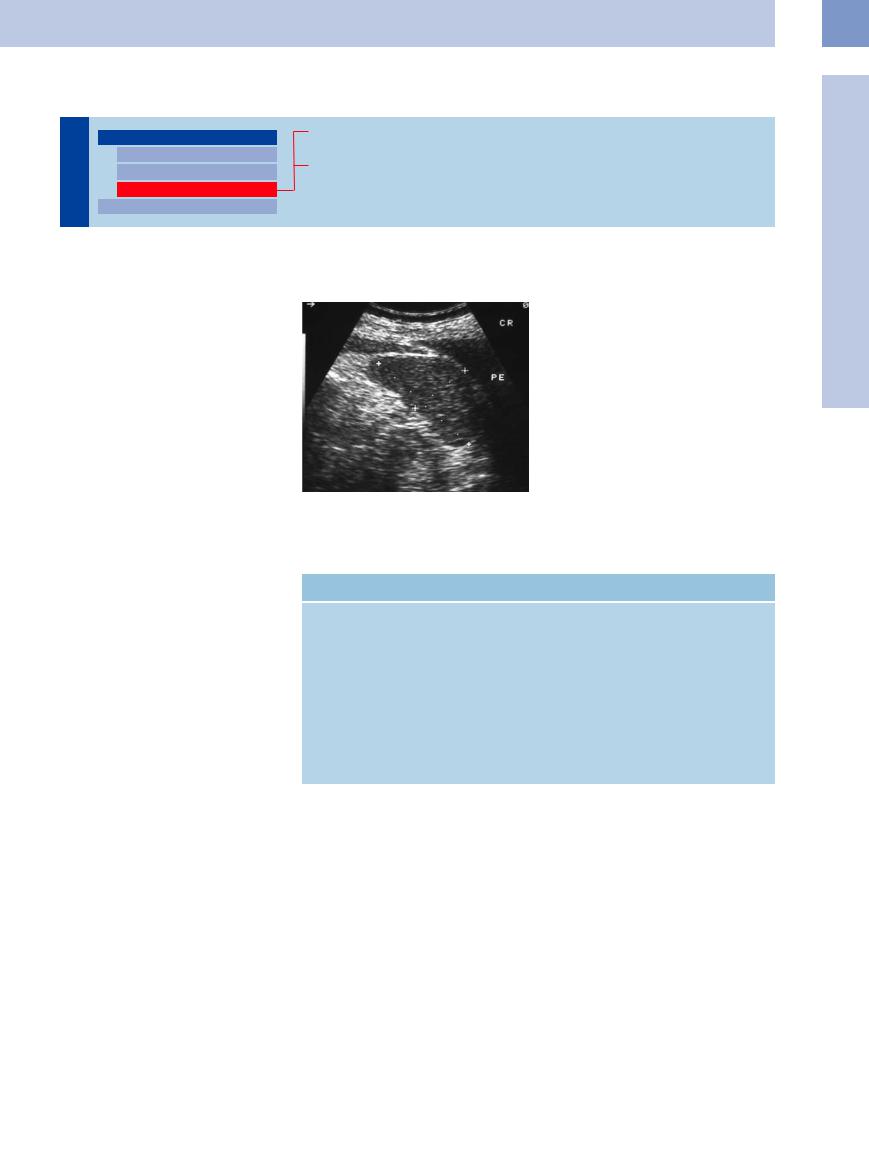
Sonographic determination of a longitudinal diameter less than 11 cm and a thickness less than 5 cm should be recorded and documented as a “small” spleen (Fig. 5.25).
To date, this finding has been regarded as a variant and certainly does not seem to be of any clinical consequence in most cases. Spleen size varies with the type of patient, and the volume of the organ also decreases with age. On colorflow Doppler scanning, these spleens will be visualized with a normal fanlike vasculature of the parenchyma. At present, it is unknown whether this age-dependent decrease in spleen size has any functional significance.
Fig. 5.25 Small spleen in a 75-year-old patient, possibly corresponding to an “aged spleen.” PE = pleural exudation.
Functional  Hyposplenism/Asplenia
Hyposplenism/Asplenia









































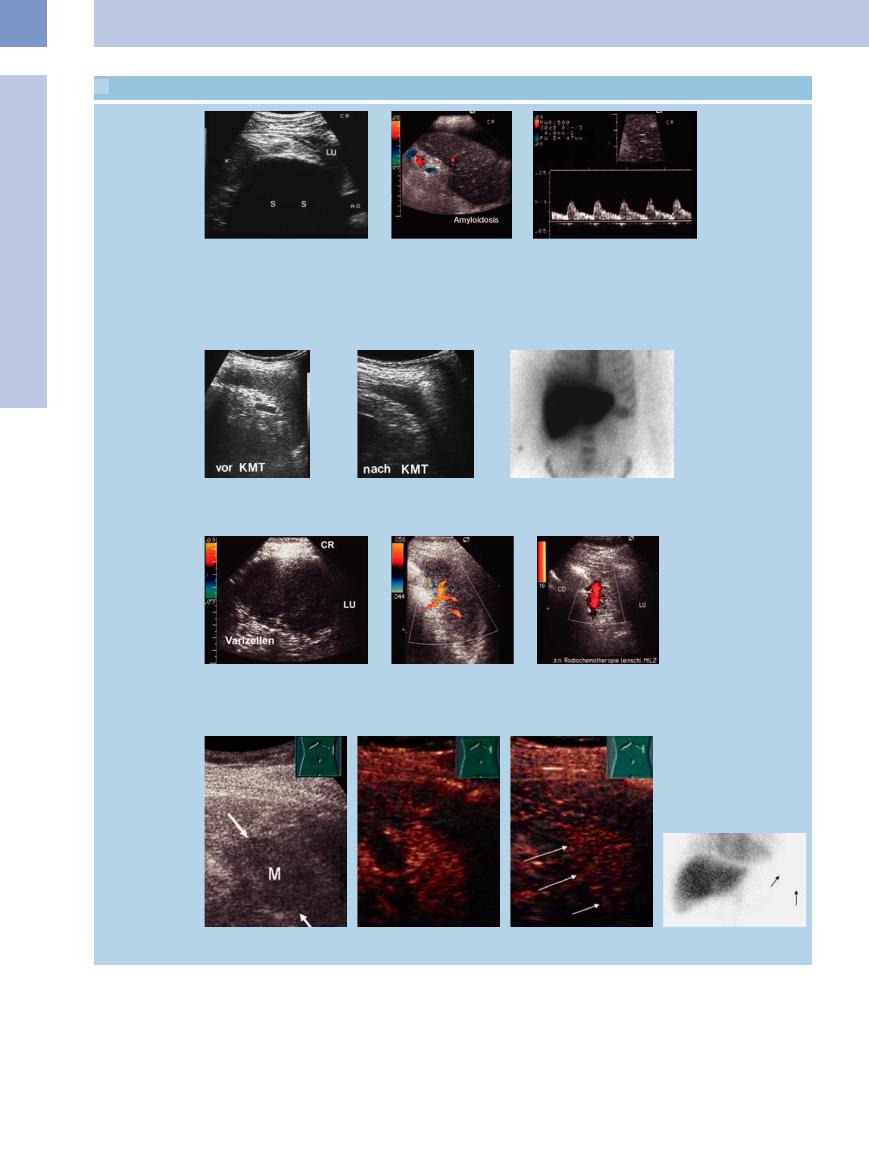
In recent years functional autosplenectomy syndromes have increasingly been reported in sickle-cell anemia ( 5.2a), after extensive splenic trauma and septic disease, in autoimmune disease (
5.2a), after extensive splenic trauma and septic disease, in autoimmune disease ( 5.2b,c), as a result of Thorotrast exposure of the spleen, and particularly following allogeneic bone marrow transplantation as a complication of chronic graft-versus- host disease (GVHD) (
5.2b,c), as a result of Thorotrast exposure of the spleen, and particularly following allogeneic bone marrow transplantation as a complication of chronic graft-versus- host disease (GVHD) ( 5.2 d–f, Table 5.2).
5.2 d–f, Table 5.2).
Apart from the clinical symptoms, the principal sonographic sign of functional splenic changes is the diminishing size of the spleen ( 5.2 g–i). The findings in color-flow Doppler scanning vary. Although in some cases there is no vascularization whatsoever, most organs will demonstrate a rarefied vascular bed. However, sonographic confirmation of splenic blood flow cannot rule out functional asplenia. This requires additional functional studies of the spleen (technetium-99 m [99 mTc] sulfur colloid labeling, platelet count, demonstration of Howell–Jolly bodies).
5.2 g–i). The findings in color-flow Doppler scanning vary. Although in some cases there is no vascularization whatsoever, most organs will demonstrate a rarefied vascular bed. However, sonographic confirmation of splenic blood flow cannot rule out functional asplenia. This requires additional functional studies of the spleen (technetium-99 m [99 mTc] sulfur colloid labeling, platelet count, demonstration of Howell–Jolly bodies).
Table 5.2 Possible causes of functional hyposplenism/asplenia
Vascular |
Parenchymal |
||
● Obstruction of the large blood vessels |
● Bone marrow transplantation |
||
– |
embolic splenic infarction |
● Amyloidosis |
|
– |
torsion of the splenic pedicle |
● Thyrotoxicosis |
|
– complete splenic vein thrombosis |
● Post radiotherapy/chemotherapy |
||
● Obstruction of the smaller blood vessels |
● Autoimmune disorders |
||
– |
sickle-cell anemia |
– |
celiac disease |
– |
vasculitis |
– |
Crohn disease |
– |
sepsis with DIC |
– |
ulcerative colitis |
– |
Thorotrast exposure |
– |
collagen disease |
|
|
● Malignant invasion |
|
In individual cases functional asplenia is characterized by reduced contrast enhancement ( Fig. 5.2j–l).
Fig. 5.2j–l).
5
Nonfocal Changes of the Spleen
211
5
Spleen
 5.2 Functional Asplenia
5.2 Functional Asplenia
Sickle-cell anemia, amyloidosis
a Small hyperechoic spleen with |
b and c Color-flow Doppler scanning of a small inhomogeneous spleen with |
hypoechoic mass and crescent- |
spurious flow signals in amyloidosis; suspected functional hyposplenism. |
shaped calcification with posterior |
|
shadowing (S) in homozygous |
|
sickle-cell anemia. Splenic scarring |
|
as sequelae of recurrent splenic |
|
infarction, suspected functional as- |
|
plenia. LU = lung; K = kidney; AO = |
|
aorta. |
|
Bone marrow transplantation (GVHD)
d–f Acute leukemia.
d Normal-sized spleen before bone marrow transplantation.
Color duplex ultrasound and CEUS
e Shrunken spleen after allogeneic bone marrow transplantation in severe GVHD.
f Colloid-labeled scintiscan: the spleen is barely visible, indicating functional hyposplenism.
g Small spleen with lack of flow signals |
h Small spleen with normal |
i Small spleen with marked hilar flow |
in sepsis and di use splenic hemorrhage |
flow signals in chronic ul- |
signals in malignant lymphoma and post |
1 year earlier; suspected functional hy- |
cerative colitis. |
radiotherapy of the spleen; suspected |
posplenism. LU = lung; Varizellen = |
|
functional hyposplenism. LU = lung; CO |
chickenpox. |
|
= venous confluence. |
j–m Missing spleen in a patient after allogenic bone marrow transplant. Subtle enhancement of contrast agent after a few seconds and reduced enhancement of contrast agent after a few seconds (j–l). Scintigraphy confirms the diagnosis of functional asplenia (m).
212
