
- •Contents
- •Preface
- •Contributors
- •1 Vessels
- •1.1 Aorta, Vena Cava, and Peripheral Vessels
- •Aorta, Arteries
- •Anomalies and Variant Positions
- •Dilatation
- •Stenosis
- •Wall Thickening
- •Intraluminal Mass
- •Perivascular Mass
- •Vena Cava, Veins
- •Anomalies
- •Dilatation
- •Intraluminal Mass
- •Compression, Infiltration
- •1.2 Portal Vein and Its Tributaries
- •Enlarged Lumen Diameter
- •Portal Hypertension
- •Intraluminal Mass
- •Thrombosis
- •Tumor
- •2 Liver
- •Enlarged Liver
- •Small Liver
- •Homogeneous Hypoechoic Texture
- •Homogeneous Hyperechoic Texture
- •Regionally Inhomogeneous Texture
- •Diffuse Inhomogeneous Texture
- •Anechoic Masses
- •Hypoechoic Masses
- •Isoechoic Masses
- •Hyperechoic Masses
- •Echogenic Masses
- •Irregular Masses
- •Differential Diagnosis of Focal Lesions
- •Diagnostic Methods
- •Suspected Diagnosis
- •3 Biliary Tree and Gallbladder
- •3.1 Biliary Tree
- •Thickening of the Bile Duct Wall
- •Localized and Diffuse
- •Bile Duct Rarefaction
- •Localized and Diffuse
- •Bile Duct Dilatation and Intraductal Pressure
- •Intrahepatic
- •Hilar and Prepancreatic
- •Intrapancreatic
- •Papillary
- •Abnormal Intraluminal Bile Duct Findings
- •Foreign Body
- •The Seven Most Important Questions
- •3.2 Gallbladder
- •Changes in Size
- •Large Gallbladder
- •Small/Missing Gallbladder
- •Wall Changes
- •General Hypoechogenicity
- •General Hyperechogenicity
- •General Tumor
- •Focal Tumor
- •Intraluminal Changes
- •Hyperechoic
- •Hypoechoic
- •Nonvisualized Gallbladder
- •Missing Gallbladder
- •Obscured Gallbladder
- •4 Pancreas
- •Diffuse Pancreatic Change
- •Large Pancreas
- •Small Pancreas
- •Hypoechoic Texture
- •Hyperechoic Texture
- •Focal Changes
- •Anechoic Lesion
- •Hypoechoic Lesion
- •Isoechoic Lesion
- •Hyperechoic Lesion
- •Irregular (Complex Structured) Lesion
- •Dilatation of the Pancreatic Duct
- •Marginal/Mild Dilatation
- •Marked Dilatation
- •5 Spleen
- •Nonfocal Changes of the Spleen
- •Diffuse Parenchymal Changes
- •Large Spleen
- •Small Spleen
- •Focal Changes of the Spleen
- •Anechoic Mass
- •Hypoechoic Mass
- •Hyperechoic Mass
- •Splenic Calcification
- •6 Lymph Nodes
- •Peripheral Lymph Nodes
- •Head/Neck
- •Extremities (Axilla, Groin)
- •Abdominal Lymph Nodes
- •Porta Hepatis
- •Splenic Hilum
- •Mesentery (Celiac, Upper and Lower Mesenteric Station)
- •Stomach
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •Small/Large Intestine
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •8 Peritoneal Cavity
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Wall Structures
- •Smooth Margin
- •Irregular Margin
- •Intragastric Processes
- •Intraintestinal Processes
- •9 Kidneys
- •Anomalies, Malformations
- •Aplasia, Hypoplasia
- •Cystic Malformation
- •Anomalies of Number, Position, or Rotation
- •Fusion Anomaly
- •Anomalies of the Renal Calices
- •Vascular Anomaly
- •Diffuse Changes
- •Large Kidneys
- •Small Kidneys
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Irregular Structure
- •Circumscribed Changes
- •Anechoic Structure
- •Hypoechoic or Isoechoic Structure
- •Complex Structure
- •Hyperechoic Structure
- •10 Adrenal Glands
- •Enlargement
- •Anechoic Structure
- •Hypoechoic Structure
- •Complex Echo Structure
- •Hyperechoic Structure
- •11 Urinary Tract
- •Malformations
- •Duplication Anomalies
- •Dilatations and Stenoses
- •Dilated Renal Pelvis and Ureter
- •Anechoic
- •Hypoechoic
- •Hypoechoic
- •Hyperechoic
- •Large Bladder
- •Small Bladder
- •Altered Bladder Shape
- •Intracavitary Mass
- •Hypoechoic
- •Hyperechoic
- •Echogenic
- •Wall Changes
- •Diffuse Wall Thickening
- •Circumscribed Wall Thickening
- •Concavities and Convexities
- •12.1 The Prostate
- •Enlarged Prostate
- •Regular
- •Irregular
- •Small Prostate
- •Regular
- •Echogenic
- •Circumscribed Lesion
- •Anechoic
- •Hypoechoic
- •Echogenic
- •12.2 Seminal Vesicles
- •Diffuse Change
- •Hypoechoic
- •Circumscribed Change
- •Anechoic
- •Echogenic
- •Irregular
- •12.3 Testis, Epididymis
- •Diffuse Change
- •Enlargement
- •Decreased Size
- •Circumscribed Lesion
- •Anechoic or Hypoechoic
- •Irregular/Echogenic
- •Epididymal Lesion
- •Anechoic
- •Hypoechoic
- •Intrascrotal Mass
- •Anechoic or Hypoechoic
- •Echogenic
- •13 Female Genital Tract
- •Masses
- •Abnormalities of Size or Shape
- •Uterus
- •Abnormalities of Size or Shape
- •Myometrial Changes
- •Intracavitary Changes
- •Endometrial Changes
- •Fallopian Tubes
- •Hypoechoic Mass
- •Anechoic Cystic Mass
- •Solid Echogenic or Nonhomogeneous Mass
- •14 Thyroid Gland
- •Diffuse Changes
- •Enlarged Thyroid Gland
- •Small Thyroid Gland
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Circumscribed Changes
- •Anechoic
- •Hypoechoic
- •Isoechoic
- •Hyperechoic
- •Irregular
- •Differential Diagnosis of Hyperthyroidism
- •Types of Autonomy
- •15 Pleura and Chest Wall
- •Chest Wall
- •Masses
- •Parietal Pleura
- •Nodular Masses
- •Diffuse Pleural Thickening
- •Pleural Effusion
- •Anechoic Effusion
- •Echogenic Effusion
- •Complex Effusion
- •16 Lung
- •Masses
- •Anechoic Masses
- •Hypoechoic Masses
- •Complex Masses
- •Index
5 Spleen
Spleen 203
|
|
|
Nonfocal Changes |
|
||||||||
|
|
|
|
|||||||||
|
|
of the Spleen |
206 |
|||||||||
|
|
|
|
|
|
Diffuse Parenchymal Changes |
206 |
|||||
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
Malignant Invasion |
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
Benign Nonhomogeneity |
|
|
|
|
|
|
Large Spleen |
208 |
||||||
|
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
Infection |
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
Congestive Splenomegaly |
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
Systemic Hematological |
|
|
|
|
|
|
|
|
|
|
|
|
Malignancy |
|
|
|
|
|
|
Small Spleen |
211 |
||||||
|
|
|
|
|
|
|
|
|
|
|
Variants, “Aged Spleen” |
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
Functional Hyposplenism/ |
|
|
|
|
|
|
|
|
|
|
|
|
Asplenia |
|
|
|
|
Focal |
|
|
Changes of the Spleen |
212 |
|||||
|
|
|||||||||||
|
|
|
|
|
Anechoic Mass |
213 |
||||||
|
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
Dysontogenetic Cysts |
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
Pseudocysts |
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
Infective Cysts |
|
|
|
|
|
|
Hypoechoic Mass |
215 |
||||||
|
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
Invasive Lymphoma |
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
Splenic Infarction |
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
Splenic Abscess |
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
Splenic Trauma |
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
Splenic Metastasis |
|
|
|
|
|
|
Hyperechoic Mass |
225 |
||||||
|
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
Hemangioma |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Hamartoma |
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
Lymphoma and |
|
|
|
|
|
|
|
|
|
|
|
|
Myeloproliferative Disorders |
|
|
|
|
|
|
Splenic Calcification |
228 |
||||||
|
|
|
|
|
|
|
|
|
|
|
Focal Calcification |
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
Diffuse Calcification |
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
Vascular Calcification |
|

5Spleen
C. Goerg
The spleen appears about the fifth week of embryonic development as a localized thickening of the coelomic epithelium of the dorsal mesogastrium near its cranial end. Its characteristic shape is evident even during initial development, and the early lobulated appearance of the fetal spleen will resolve usually at birth. The spleen fulfils numerous functions:
●Hematopoiesis: normally only during fetal life
●Immune function: antibody and lymphocyte production
●Erythrocyte storage: not nearly as marked in the human spleen as in other species
●Phagocytosis: removal of old and damaged blood cells, immune complexes, and particulate matter in the bloodstream.
The arterial hemodynamics of the spleen must be viewed within the context of the other splanchnic organs. On the venous side it is regarded as part of the portal venous system.
Anatomy























































Size
●Length along the maximum cephalocaudal diameter ≤ 11 cm
●Thickness from hilum to surface (cortex) ≤ 5 cm
Shape
●Crescent/coffee bean configuration, highly variable
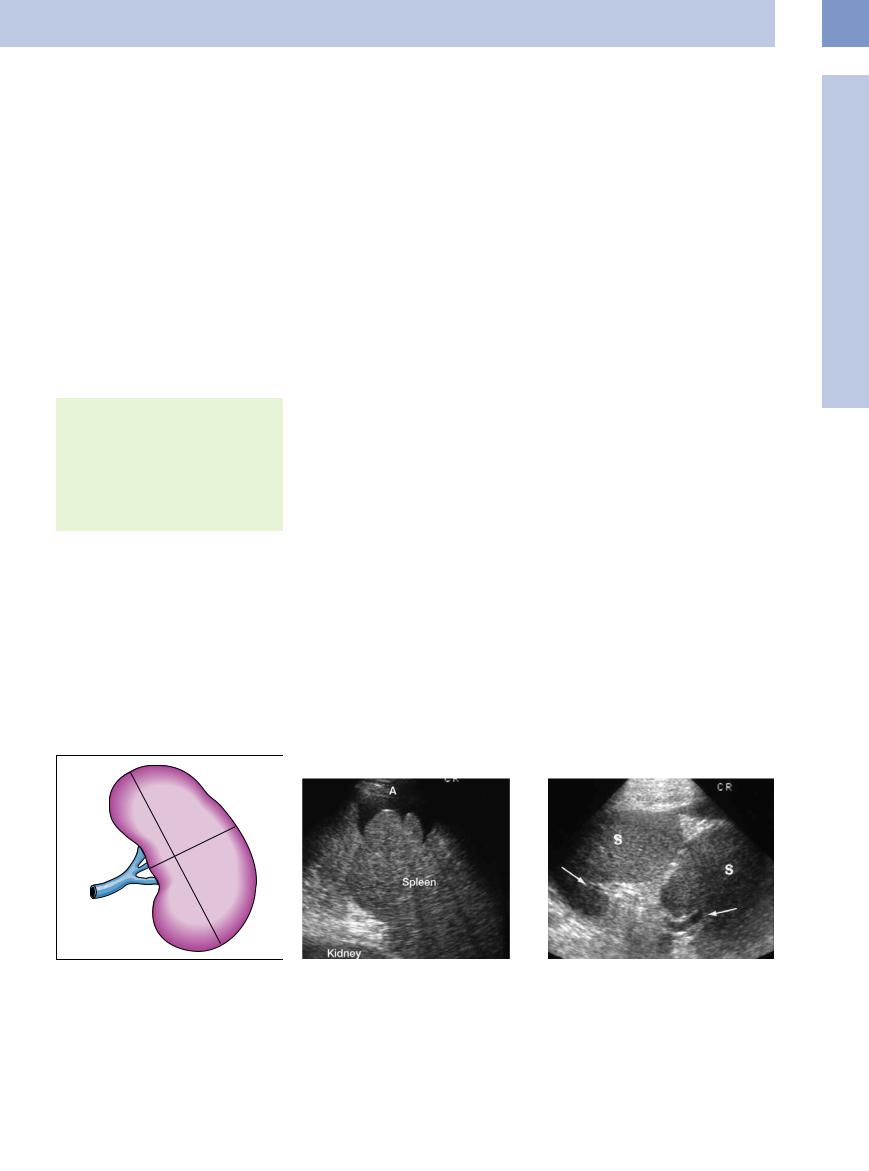
Size. Intercostal scanning provides the most reliable measurements of splenic dimensions. In this view the largest distance between the two poles should be determined (maximum length). The thickness is determined orthogonal to the maximum length by measuring from the hilum to the apex of the splenic convexity (Fig. 5.1). Additional measurement of the width for computation of the splenic volume by the ellipsoid method has not become part of routine clinical practice.
Fig. 5.1 Sonographic illustration of the splenic hilum with assessment of length (D1) and thickness (D2).
Normal dimensions of the adult spleen are a maximum length < 11 cm and a thickness < 5 cm. The severity of any splenomegaly depends on the size of the spleen:
●Mild to moderate: ≥ 5 cm, ≥ 11 cm
●Marked: ≥ 6 cm, ≥ 16 cm
●Extreme: ≥ 8 cm, ≥ 20 cm
Any splenic dimensions above these normal values have to result in the presumed diagnosis of an enlarged spleen. Depending on the patient’s age (juvenile) and physique, a slightly longer and thinner (asthenic) or shorter and plumpish (pyknic) spleen can be regarded as normal. During childhood the spleen tends to be smaller.
Shape. The shape of the spleen is that of a halfmoon or crescent/coffee bean but is highly variable and depends on the plane of the ultrasound view. The diaphragmatic surface is convex and smooth, while the concave visceral
Fig. 5.2 Splenic septa at the diaphragmatic aspect may become evident in the presence of ascites (A).
surface presents gastric, renal, pancreatic, and colic impressions.
Vestiges of the complex embryological development of the splenic anlage in the dorsal mesogastrium may also be found as notches and septa in the diaphragmatic surface (Fig. 5.2). Complete congenital cleft with separate hilar blood supply may be demonstrated in rare cases (Fig. 5.3).
Sometimes branches of the vasculature penetrate the visceral surface at various points. In a few patients, blood vessels terminating on the diaphragmatic aspect will also be seen. Usually, the splenic vein has a diameter of less than 0.5 cm and runs straight from the hilum of the spleen. Varicosities and kinking along the course of these vessels have been observed.
Ultrasound texture. Comparison of healthy organs in the same patient demonstrates that the spleen is slightly less echogenic than the liver, but significantly more echogenic than the kidney.
Fig. 5.3 Congenital cleft of the spleen (S) with demonstration of separate hilar blood supply (arrows).
5
Spleen
203
5
Spleen
Topography 











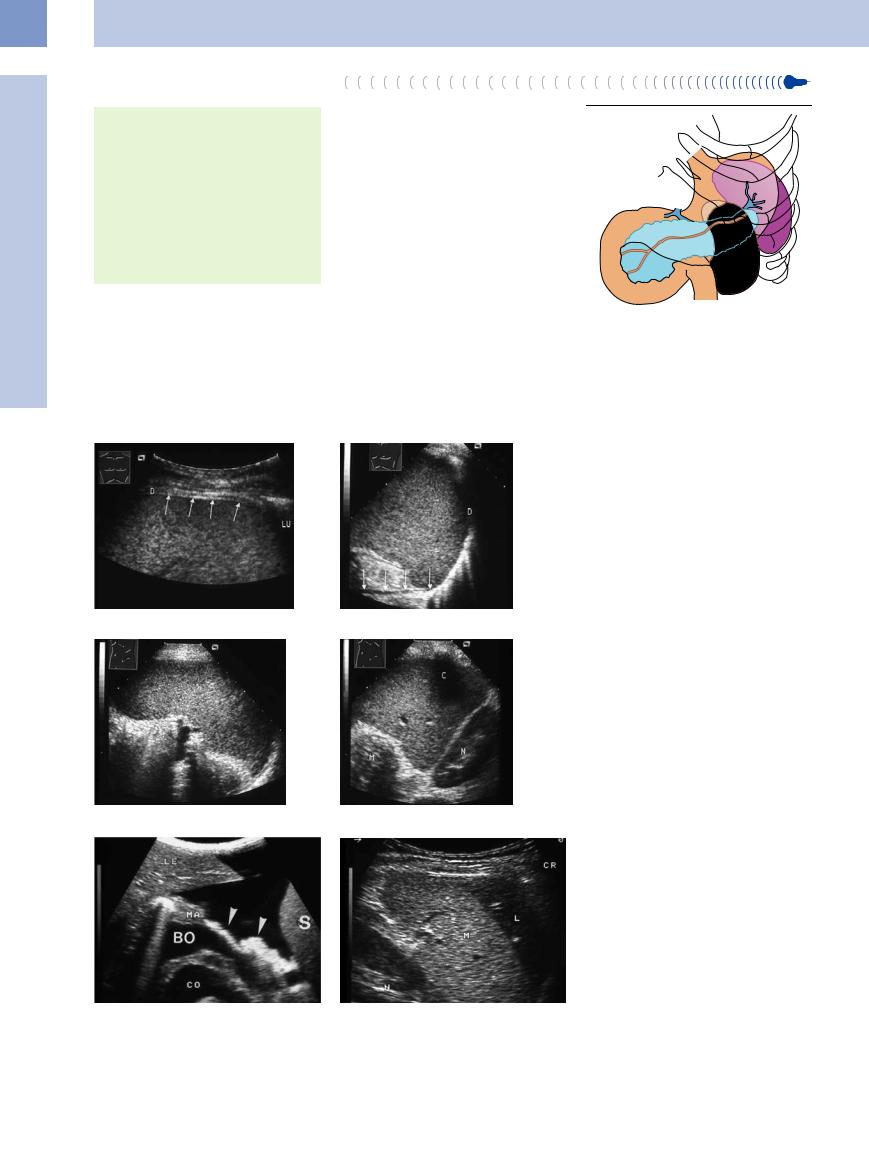
Relations (Fig. 5.4)
●Diaphragmatic surface with the left dome of the diaphragm
●Gastric surface with the posterior gastric wall
●Renal surface with the upper pole of the left kidney
●Pancreatic tail touching the hilum of the spleen
Ultrasound landmark structure
● Hilar blood vessels of the spleen
The spleen is situated principally in the left hypochondric region of the abdomen and is an almost completely intraperitoneal organ. Its convex diaphragmatic aspect is in broad relation with the abdominal surface of the diaphragm (Fig. 5.5). It is protected posteriorly and laterally by the 9th to 12th ribs, and the organ is overlapped by the costophrenic recess, which may extend down as far as the inferior
Fig. 5.7 Transverse left hypochondric view visualizing the gastrosplenic ligament (arrows) due to the presence of intraperitoneal fluid. The ligament is anterior of the lesser sac (BO). CO = venous confluence; S = spleen; LE = liver; MA = stomach.
border of the organ. The longitudinal axis of the spleen roughly parallels the course of the 10th rib. The anteromedial aspect of the concave gastric surface is in relation with the posterior wall of the gastric body, while the inferior renal surface abuts the superior pole of the left kidney (Fig. 5.6). The anteroinferior aspect of the spleen is in close relation with the left colic flexure (Fig. 5.4).
Apart from the hilum, the spleen is almost entirely surrounded by peritoneum. It remains connected to the stomach by a peritoneal fold, the so-called gastrosplenic ligament (Fig. 5.7). Visualization of the splenorenal ligament depends on the extent of fusion with the dorsal peritoneum. Sometimes the gastrosplenic ligament may become evident in patients with ascites. In the presence of an enlarged left hepatic lobe the liver may be in contact with the diaphragmatic aspect of the spleen and cover it like a cap (Fig. 5.8).
Fig. 5.4 Anatomic relations of the spleen, pancreas, stomach, and kidney.
Fig. 5.5 Left lateral intercostal view. D = diaphragm.
a Visualization of the anterior crus of the diaphragm. LU = lung.
b Dome of the diaphragm and the posterior crus of the diaphragm (arrows).
Fig. 5.6 Splenic dimensions.
a Maximum length (polar diameter).
b Transverse view visualizing the posterior renal and anterior gastric aspects. N = kidney; M = stomach; C = posterior shadowing of the rib.
Fig. 5.8 In hepatomegaly the liver (L) may cap the spleen
(M). N = kidney.
204
 5.1 Blood Supply of the Spleen
5.1 Blood Supply of the Spleen
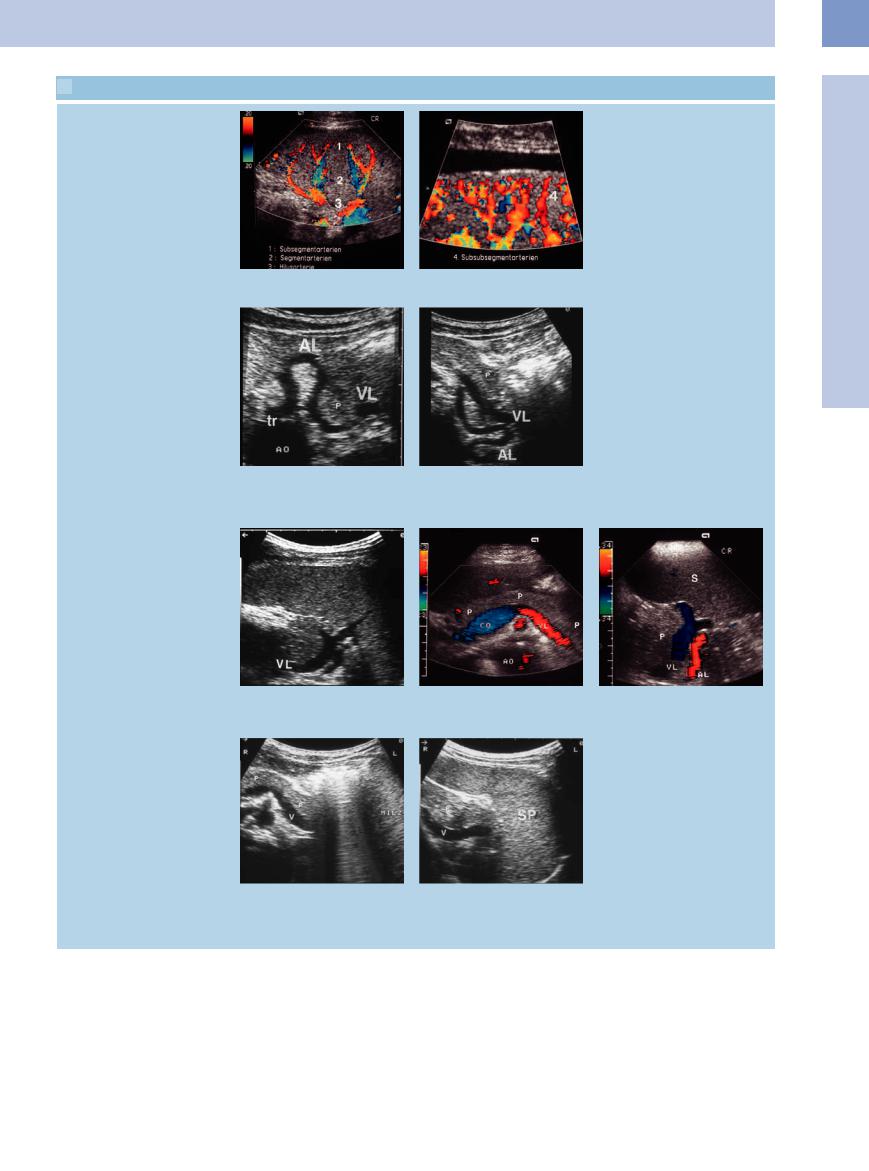
Parenchymal vessels
a and b Vessels of the splenic parenchyma on color-flow Doppler imaging.
Splenic artery
5
Spleen
c Quite often the splenic artery (AL) displays a tortuous course. VL = splenic vein; AO = aorta; tr = celiac axis; P = pancreas.
Splenic vein
e In the vicinity of the splenic hilum the splenic vein (VL) will be visualized posterior to the pancreas.
h Landmark structure: splenic vein (V). Quite often the pancreatic tail cannot be visualized because of the gastric gas. P = pancreas; Milz = spleen.
d The splenic artery (AL) courses through the pancreas.
f and g Color-flow Doppler imaging: splenic vein (VL) at the central hypochondric region and the hilum of the spleen. P = pancreas; CO = venous confluence; AO = aorta; AL = splenic artery; S = spleen.
i The region of the pancreatic tail (P) may be assessed by insonation through the spleen. P = pancreas; V = splenic vein; SP = spleen.
Blood vessels. The splenic artery originates at the celiac axis and then runs straight along the superior margin of the pancreas. On arriving near the spleen it follows a rather tortuous course and close to the hilum it divides into several branches. There are only infrequent variants of its origin at the celiac axis. The segmental branches of the splenic artery are
terminal arteries resulting in separate splenic segments. The spleen is linked into the systemic circulation via the splenic artery, and into the portal circulation via the splenic vein ( 5.1c–e). The trunk of the splenic vein (sometimes located up to 6 cm from the actual splenic hilum) commences from several tributaries issuing from the stomach and spleen,
5.1c–e). The trunk of the splenic vein (sometimes located up to 6 cm from the actual splenic hilum) commences from several tributaries issuing from the stomach and spleen,
courses posterior to the tail and body of the pancreas, and unites with the superior mesenteric vein to form the portal vein.
Vascular appearance. On color-flow Doppler scanning, the vascular appearance is dominated primarily by the spoke-like course of the segmental arteries and veins, which run
205
