
- •Preface
- •Acknowledgments
- •Contents
- •Contributors
- •1. Introduction
- •2. Evaluation of the Craniomaxillofacial Deformity Patient
- •3. Craniofacial Deformities: Review of Etiologies, Distribution, and Their Classification
- •4. Etiology of Skeletal Malocclusion
- •5. Etiology, Distribution, and Classification of Craniomaxillofacial Deformities: Traumatic Defects
- •6. Etiology, Distribution, and Classification of Craniomaxillofacial Deformities: Review of Nasal Deformities
- •7. Review of Benign Tumors of the Maxillofacial Region and Considerations for Bone Invasion
- •8. Oral Malignancies: Etiology, Distribution, and Basic Treatment Considerations
- •9. Craniomaxillofacial Bone Infections: Etiologies, Distributions, and Associated Defects
- •11. Craniomaxillofacial Bone Healing, Biomechanics, and Rigid Internal Fixation
- •12. Metal for Craniomaxillofacial Internal Fixation Implants and Its Physiological Implications
- •13. Bioresorbable Materials for Bone Fixation: Review of Biological Concepts and Mechanical Aspects
- •14. Advanced Bone Healing Concepts in Craniomaxillofacial Reconstructive and Corrective Bone Surgery
- •15. The ITI Dental Implant System
- •16. Localized Ridge Augmentation Using Guided Bone Regeneration in Deficient Implant Sites
- •17. The ITI Dental Implant System in Maxillofacial Applications
- •18. Maxillary Sinus Grafting and Osseointegration Surgery
- •19. Computerized Tomography and Its Use for Craniomaxillofacial Dental Implantology
- •20B. Atlas of Cases
- •21A. Prosthodontic Considerations in Dental Implant Restoration
- •21B. Overdenture Case Reports
- •22. AO/ASIF Mandibular Hardware
- •23. Aesthetic Considerations in Reconstructive and Corrective Craniomaxillofacial Bone Surgery
- •24. Considerations for Reconstruction of the Head and Neck Oncologic Patient
- •25. Autogenous Bone Grafts in Maxillofacial Reconstruction
- •26. Current Practice and Future Trends in Craniomaxillofacial Reconstructive and Corrective Microvascular Bone Surgery
- •27. Considerations in the Fixation of Bone Grafts for the Reconstruction of Mandibular Continuity Defects
- •28. Indications and Technical Considerations of Different Fibula Grafts
- •29. Soft Tissue Flaps for Coverage of Craniomaxillofacial Osseous Continuity Defects with or Without Bone Graft and Rigid Fixation
- •30. Mandibular Condyle Reconstruction with Free Costochondral Grafting
- •31. Microsurgical Reconstruction of Large Defects of the Maxilla, Midface, and Cranial Base
- •32. Condylar Prosthesis for the Replacement of the Mandibular Condyle
- •33. Problems Related to Mandibular Condylar Prosthesis
- •34. Reconstruction of Defects of the Mandibular Angle
- •35. Mandibular Body Reconstruction
- •36. Marginal Mandibulectomy
- •37. Reconstruction of Extensive Anterior Defects of the Mandible
- •38. Radiation Therapy and Considerations for Internal Fixation Devices
- •39. Management of Posttraumatic Osteomyelitis of the Mandible
- •40. Bilateral Maxillary Defects: THORP Plate Reconstruction with Removable Prosthesis
- •41. AO/ASIF Craniofacial Fixation System Hardware
- •43. Orbital Reconstruction
- •44. Nasal Reconstruction Using Bone Grafts and Rigid Internal Fixation
- •46. Orthognathic Examination
- •47. Considerations in Planning for Bimaxillary Surgery and the Implications of Rigid Internal Fixation
- •48. Reconstruction of Cleft Lip and Palate Osseous Defects and Deformities
- •49. Maxillary Osteotomies and Considerations for Rigid Internal Fixation
- •50. Mandibular Osteotomies and Considerations for Rigid Internal Fixation
- •51. Genioplasty Techniques and Considerations for Rigid Internal Fixation
- •52. Long-Term Stability of Maxillary and Mandibular Osteotomies with Rigid Internal Fixation
- •53. Le Fort II and Le Fort III Osteotomies for Midface Reconstruction and Considerations for Internal Fixation
- •54. Craniofacial Deformities: Introduction and Principles of Management
- •55. The Effects of Plate and Screw Fixation on the Growing Craniofacial Skeleton
- •56. Calvarial Bone Graft Harvesting Techniques: Considerations for Their Use with Rigid Fixation Techniques in the Craniomaxillofacial Region
- •57. Crouzon Syndrome: Basic Dysmorphology and Staging of Reconstruction
- •58. Hemifacial Microsomia
- •59. Orbital Hypertelorism: Surgical Management
- •60. Surgical Correction of the Apert Craniofacial Deformities
- •Index
5
Etiology, Distribution, and Classification of Craniomaxillofacial Deformities: Traumatic Defects
Richard H. Haug and Jackson P. Morgan, III
Perhaps no defect is as emotionally devastating as a deformity of the face caused by trauma.1 An individual who even minutes before led a normal life may have the focal point of their self-image permanently disfigured. This can leave enormous psychological as well as physical scars, even beyond those associated with congenital deformities whose victims have never known a different life. Yet posttraumatic defects have rarely been the focus of epidemiologic or demographic investigations. Their description has been relegated to individual case reports, anecdotal experiences, or review articles that discuss avulsion defects in general terms. Thus a description of the etiology, distribution, and classification of the traumatic deformity becomes a difficult endeavor based only upon intuitive reasoning and individual institutional experiences.
Classification
lar injury, these may also be associated with or without soft tissue loss (Figure 5.6). Additionally, considerations in the midface are the loss of such specialized structures as the nose, eyes, or ears.
The last major area in the classification of craniomaxillofacial avulsion injuries is the cranium (Figure 5.7). These include the frontal bone (and sinus), temporal bones, parietal bones, occipital bones, and base of skull. They may also be associated with or without loss of soft tissues. Consideration of neurologic injury is of paramount concern in cranial avulsion injuries (Figure 5.8).3,4
The other common system for classification of traumatic defects is by the etiology. Virtually all of the mechanisms of these types of injuries are of high energy with variations of the wounding mechanism’s parameters. Kinetic energy is described as
1
2 (Mass)(Velocity)2
No uniform or universal classification system exists for the description of traumatic defects. They are usually described in general anatomic terms or by the mechanism of the injury. Generally, craniomaxillofacial avulsion injuries are described as mandibular, midfacial, or cranial. These are then subclassified as those with or without soft tissue loss.
Virtually every type of mandibular osseous defect is possible (Figures 5.1–5.3). The classification of each anatomic area follows the classification system devised for fractures by Ivy and Curtis as condyle, coronoid, ramus, angle, body, and symphysis.2 These may or may not be associated with the loss of cutaneous or mucosal soft tissues (Figure 5.4).
The next major category of craniomaxillofacial defects is the midface. Because of the amount of energy required to avulse hard tissues, midfacial avulsion injuries are rarely isolated defects but tend to have damage involving multiple anatomic regions (Figures 5.3 and 5.5). These may involve any combination of the bones of the maxilla, palate, naso- orbital-ethmoid region, zygoma, or orbits. As with mandibu-
Handgun injuries are produced by low caliber, low velocity projectiles and are usually considered to be lowto moderate-energy injuries. Yet if a handgun is held close to the victim (Figures 5.9 and 5.10), all of the energy is absorbed by the patient. Rifle injuries are produced by low or high caliber projectiles fired at high velocity and thus are high-energy injuries. Shotgun injuries are caused by multiple low velocity, low caliber projectiles. When a single pellet injures the victim, it is usually innocuous. However, hundreds of pellets act collectively to increase the total mass and thus produce high-energy injuries, particularly at close range. Explosions are considered ultra-high-energy injuries. Occupational and industrial accidents are caused by machinery or large pieces of equipment. Although traveling at low velocity, they are so large that the mass is increased to a point that the energy transferred is that of a high-energy wound (or crush). The only other types of avulsion injuries are those caused by tearing (as in animal bites) or abrasion (as in a victim dragged by a motor vehicle).
43

44 |
R.H. Haug and J.P. Morgan, III |
FIGURE 5.1 Note the loss of the entire symphysis region in this computed tomographic three-dimensional reconstruction of a close-range handgun injury.
FIGURE 5.3 This three-dimensional computed tomographic image reveals a gross avulsion injury of the patient’s mandibular body, ramus, left maxilla, orbital floor, and nose.
FIGURE 5.2 Note in this two-dimensional computed tomographic image that the patient’s mandibular symphysis and body regions have been avulsed. They are found external to the patient (arrows).
FIGURE 5.4 The soft tissues overlying the mandible (patient seen in Figure 5.1) have been avulsed along with the bone. Note that the skin and mucosa of the lower lip, upper lip, and portions of the nose were lost by this suicide attempt with a handgun at close range. (This case courtesy of Drs. Roderick Jordan and Anthony Smith of the MetroHealth Medical Center of Cleveland, Ohio)
5. Traumatic Defects |
45 |
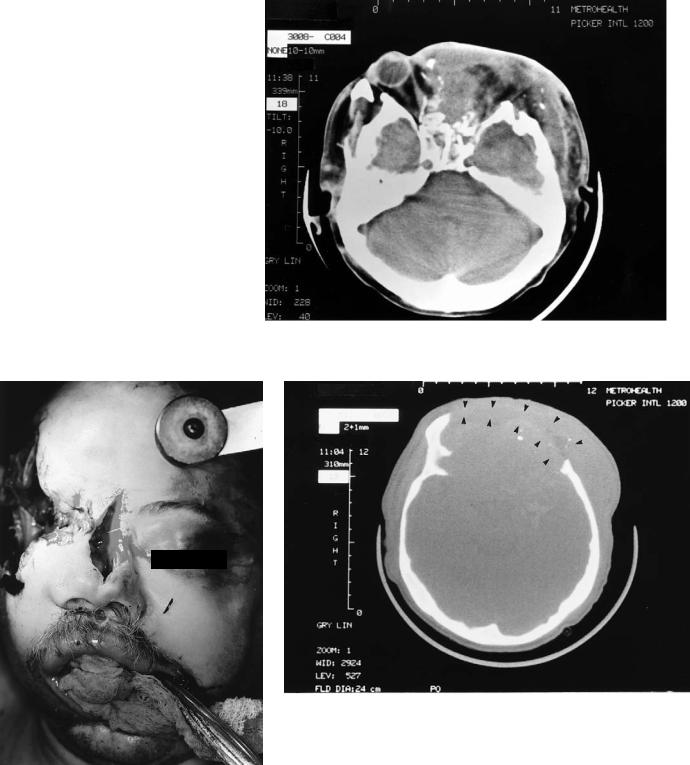
FIGURE 5.5 This computed tomographic image of a self-inflicted gunshot wound demonstrates that the amount of energy produced will damage or avulse multiple midfacial structures. Note that the left globe along with the nasal bones, nasoethmoid region, orbit, and zygoma are absent.
FIGURE 5.6 Note the soft tissue loss about the right midfacial region along with a total avulsion of the orbit (patient seen in Figure 5.5).
FIGURE 5.7 Note the large avulsed region of the frontal bone (arrows). The anterio frontal sinus table, posterior frontal sinus table, anterior cranial fossa, and portion of the left temporal bone are missing.

46 |
R.H. Haug and J.P. Morgan, III |
FIGURE 5.8 Note the gross neurologic damage that has been produced by this self-inflicted gunshot wound. A portion of the frontal bone has been avulsed. Numerous bullet fragments are noted within the brain and craniomaxillofacial soft tissues. Intracranial hemorrhage and pneumocephalus are also present.
FIGURE 5.9 Handguns at close range yield high-energy injuries, which tend to avulse both hard and soft tissues. When held in the mouth, as is common in suicides, the midface and cranium are invariably affected.
FIGURE 5.10 When the handgun is held at close range underneath the chin, the mandible is invariably affected.
5. Traumatic Defects
Distribution
The actual loss of tissue associated with craniomaxillofacial wounds is fairly rare.5 Although at first the facial tissues may appear absent, they tend to retract or roll under the wound margins. While statistics regarding the incidence of avulsion injuries are virtually nonexistent in the surgical literature, Osborn suggests in a survey of 9430 patients with maxillofacial injuries in the Vietnam conflict, that 9.4% exhibited avulsion of a significant portion of the mandible.6 The trauma registry of the MetroHealth Medical Center (Cleveland, Ohio) for 1993 indicated that approximately 150 patients were admitted for the treatment of facial fractures. Of these, 66% were mandibular fractures and 33% midfacial. In this group, 1 patient sustained an avulsion injury of the mandible (1%), and 2 patients sustained avulsion injuries of the midface (4%). All were white males between 15 and 30 years of age, injured by firearms. It seems rational to assume that the patient profile of traumatic avulsion injuries would be similar to that of the general facial fracture population. Thus we can assume that this group would be mostly male (greater than 70%) and between the ages of 18 and 35 (mean age 30 years).7,8
Etiology
Handgun Injuries
Handguns propel low caliber projectiles at low velocities. Within 1 to 2 milliseconds after impact, a pressure wave from air in front of the missile distends the soft tissues up to four times the diameter of the projectile. Along with the temporary cavity is a permanent one that contains skin, clothing, necrotic tissue, and secondary projectiles. The projectile itself and the pressure wave of the temporary cavity cause damage to the muscle, bone, blood vessels, and nerves.9 The muscles become contused, necrotic, and colonized with bacteria.9 The blood vessels are crushed, ripped, displaced, or stretched.9 This can result in arterial spasm, pseudoaneurysm, exudate production, thrombosis, and hemorrhage.9 Nerves tend to become twisted with separation of nerve fibers9 and become edematous. Gross comminution of the mandibular bone and drill-hole defects in the maxilla are common.9 When a handgun is held beneath the chin or within the mouth, as is the case with many suicide attempts (Figures 5.9 and 5.10), all of the energy from the handgun is transferred to the patient. In this situation, the wound profile resembles that of a rifle injury with the associated avulsion of the soft and hard tissues. Those soft tissues which remain behind are compromised by edema, congestion, and contamination.
47
stellate, with torn and irregular margins.10 Exit wounds with rifles tend to be avulsive with defects that are more than two or three times larger than the entrance and which are stellate, saw tooth, or triangular in shape.11 The temporary cavity in rifle wounds may be as high as eight times the diameter of the projectile.11,12 Large amounts of muscle may be avulsed.
Large-diameter nerves are found to become grossly distended with rifle injuries. The myelin sheaths become protruded and deformed with axonal degeneration. Blood vessels damaged with rifles possess all of the characteristics outlined for handgun injuries but are also found to be more congested and thrombosed.11 Veins reveal diapedesis of red blood cells as well as margination and pavementing of neutrophils.11,12 Gross fragmentation and avulsion of the craniomaxillofacial bones are the rule with rifle injuries rather than the exception.13 The remaining soft tissues are compromised by contusion, edema, congestion, and contamination with secondary projectiles and microorganisms.
Shotgun Injuries
Shotguns propel multiple low caliber spherical projectiles at low velocities. These hundreds of projectiles act collectively to injure the victim. Each individual pellet creates an entrance, temporary cavity, and permanent cavity characteristic of a handgun injury. A single pellet is relatively innocuous, multiple pellets more serious, but hundreds of pellets increase the mass of energy to create a devastating injury.10,14 Because shotguns propel at low velocity, the energy dissipates greatly as the distance of the victim from the firearm increases.14 Type III shotgun injuries (those within 3 yards or those with less than 10 cm of scatter) produce lethal avulsive injuries of both the soft and hard tissues.15,16
Explosions
Blast injuries are infrequently encountered. When they are, the victims are injured by multiple modalities. These patients initially sustain first degree burns from ignited explosives.10 A blast wave of compressed air will then throw the patient through the air, which will create secondary injuries due to the fall.10 Finally, the patient will be injured by the direct contact of exploded fragments.10 These projectiles tend to be propelled at high or ultra-high velocities and injure with high or ultra-high energy. Victims close to the source of the explosion seldom survive. Those who do must be treated for burns, blunt, and penetrating injury.17–19 The wounding profile will include both soft and hard tissue avulsion, compromised by the remaining soft tissues that are burned, contused, congested, and contaminated.
Rifle Injuries
Rifles project either low or high caliber projectiles at high velocity and are capable of causing injuries with a high amount of energy. The entrance wounds of these injuries tend to be
Occupational and Farm Injuries
Occupational and farm accidents have the potential for producing gross avulsive wounds or severe crush injuries.
48
Whether moving at low or high velocity, because of the magnitude of the mass of industrial machinery, the wheels or blades of tractors or combines, or the weight of steel I-beams and concrete walls, the injuries produced are either that of a high-en- ergy impact or of a devastating crush. If the injury is that of a high-energy impact, large portions of soft and hard tissue will be avulsed.20 If that of a crush injury, the vascular supply of the soft and hard tissues will be so compressed that large areas of bone and soft tissue will be rendered necrotic.20
Tearing Injuries
Bite injuries inflicted by the teeth of animals, tearing injuries caused by the blades of industrial machines, and ragged shearing wounds induced by machinery blades or saws can cause both avulsive injuries and contaminated crush injuries.20–23 Animals such as dogs can bite with a force of 450 lbs/in2. Their mouths are contaminated with a plethora of microorganisms.21 Thus, grossly contaminated crush injuries can cause regions of soft tissue necrosis compromised with infection. In addition, the fangs of the teeth can avulse large areas of lip, cheek, scalp, the ears, or nose. Similarly, the blades of machinery or saws contaminated with airborne or earthen microorganisms can produce contaminated crush or soft tissue avulsive injuries just as the bites of animals can. On occasion, the underlying osseous structures may be penetrated, fractured, fragmented, or avulsed.
Abrasion Injuries
The last mechanism in the production of avulsion injuries is that caused by abrasion. It is extremely rare that a victim will be dragged by a moving object. Even if a victim falls off a moving motorcycle and slides, frequently the maxillofacial region is protected by a helmet or face mask. Under these circumstances the characteristic “road rash” explains the damage to the overlying soft tissues. Infrequently, the osseous tissues will also be avulsed.
Summary
From the limited resources available, it appears that the traumatic defect patient population is composed mostly of young males. These individuals routinely have been injured by highenergy wounding mechanisms. While the amount of energy should be a guide to the patient’s evaluation and assessment, it should be understood that the clinician must treat the wound and not the etiology.24
References
1.Nordlicht S. Facial disfigurements and psychiatric sequelae. NYS J Med. 1979;79(9):1382–1384.
R.H. Haug and J.P. Morgan, III
2.Ivy RH, Curtis L. Fractures of the mandible: an analysis of 100 cases. Dent Cosmos 1926;68:439–446.
3.Graham TW, Williams PC, Harrington T, et al. Civilian gunshot wounds to the head: A prospective study. Neurosurgery 1990;27:696–700.
4.Suddaby L, Weir B, Forsyth C. The management of 22 calibre gunshot wounds of the brain: a review of 49 cases. Can J Neurol Sci. 1987;14:268–272.
5.Powers MP, Bertz J, Fonseca RJ. Management of soft tissue injuries. In: Fonseca RJ, Walker RV, eds. Oral and Maxillofacial Trauma. Philadelphia: W.B. Saunders; 1991: ch 23.
6.Osborn D. Reconstructive surgery for maxillofacial injuries. In: Fonseca RJ, Davis WH, eds. Reconstructive Preprosthetic Oral and Maxillofacial Surgery. Philadelphia: W.B. Saunders; 1986: ch 10.
7.Haug RH, Prather J, Indresano AT. An epidemiologic survey of facial fractures and concomitant injury. J Oral Maxillofac Surg. 1990;48:926–932.
8.Vetter JD, Topazian RG, Goldberg MH, et al. Facial fractures occurring in a medium sized metropolitan area: recent trends.
Int J Oral Maxillofac Surg. 1991;20:214–216.
9.Haug RH. Management of low-caliber, low-velocity gunshot wounds of the maxillofacial region. J Oral Maxillofac Surg. 1989;47:1192–1196.
10.Haug RH. Gunshot wounds to the head and neck. Topic 10. In: Kelly JP, ed. OMS Knowledge Update, Part II. Chicago: AAOMS Publishing; 1995:TRA 65–82.
11.Wang ZG, Fang SX, Liu YQ. Pathomorphological observations of gunshot wounds. Acta Clin Scand Suppl. 1986;508:185–195.
12.Wang Z, Tang C, Chen X, et al. Early pathomorphologic characteristics of the wound tract caused by fragments. J Trauma. 1988;28:S89–S95.
13.Suneson A, Hansson HA, Seeman T. Central and peripheral nervous damage following high energy missile wounds in the thigh. J Trauma. 1988;28:S197–S203.
14.Ordog GJ, Wasserberg J, Balasubramanian S. Shotgun wound ballistics. J Trauma. 1988;28:624–631.
15.Walker MC, Poindexter JM. Principles of management of shotgun wounds. Surg Gynecol Obstet. 1990;170:97–105.
16.Glezer JA, Minard G, Croce MA, et al. Shotgun wound of the abdomen. Am Surgeon. 1993;59:129–131.
17.Fackler ML, Bellamy RF, Malinowski JA. A reconsideration of the wounding mechanism of very high velocity projectiles—im- portance of projectile shape. J Trauma. 1988;28:S63–S67.
18.Ellis S. Maxillofacial surgery and the trouble in Northern Ireland. Br Dent J. 1990;168:411–412.
19.Phillips YY. Primary blast injuries. Ann Emerg Med. 1986; 15:1446–1450.
20.Cameron D, Bishop C, Sibert JR. Farm accidents in children. Br Med J. 1992;305:23–25.
21.Morgan JP, Haug RH, Murphy MT. Management of facial dog bite injuries. J Oral Maxillofac Surg. 1995;53:435–441.
22.Fukuta K, Jackson IT, Topf JS. Facial lawn mower injury treated by a vascular costochondral graft. J Oral Maxillofac Surg. 1992;40:194–198.
23.Marks RB, Fort F. Chain saw injury of the maxillofacial region.
J Oral Maxillofac Surg. 1986;44:240–243.
24.Fackler ML. Wound ballistics: a review of common misconceptions. JAMA 1988;259:2730–2736.
