
- •Preface
- •Acknowledgments
- •Contents
- •Contributors
- •1. Introduction
- •2. Evaluation of the Craniomaxillofacial Deformity Patient
- •3. Craniofacial Deformities: Review of Etiologies, Distribution, and Their Classification
- •4. Etiology of Skeletal Malocclusion
- •5. Etiology, Distribution, and Classification of Craniomaxillofacial Deformities: Traumatic Defects
- •6. Etiology, Distribution, and Classification of Craniomaxillofacial Deformities: Review of Nasal Deformities
- •7. Review of Benign Tumors of the Maxillofacial Region and Considerations for Bone Invasion
- •8. Oral Malignancies: Etiology, Distribution, and Basic Treatment Considerations
- •9. Craniomaxillofacial Bone Infections: Etiologies, Distributions, and Associated Defects
- •11. Craniomaxillofacial Bone Healing, Biomechanics, and Rigid Internal Fixation
- •12. Metal for Craniomaxillofacial Internal Fixation Implants and Its Physiological Implications
- •13. Bioresorbable Materials for Bone Fixation: Review of Biological Concepts and Mechanical Aspects
- •14. Advanced Bone Healing Concepts in Craniomaxillofacial Reconstructive and Corrective Bone Surgery
- •15. The ITI Dental Implant System
- •16. Localized Ridge Augmentation Using Guided Bone Regeneration in Deficient Implant Sites
- •17. The ITI Dental Implant System in Maxillofacial Applications
- •18. Maxillary Sinus Grafting and Osseointegration Surgery
- •19. Computerized Tomography and Its Use for Craniomaxillofacial Dental Implantology
- •20B. Atlas of Cases
- •21A. Prosthodontic Considerations in Dental Implant Restoration
- •21B. Overdenture Case Reports
- •22. AO/ASIF Mandibular Hardware
- •23. Aesthetic Considerations in Reconstructive and Corrective Craniomaxillofacial Bone Surgery
- •24. Considerations for Reconstruction of the Head and Neck Oncologic Patient
- •25. Autogenous Bone Grafts in Maxillofacial Reconstruction
- •26. Current Practice and Future Trends in Craniomaxillofacial Reconstructive and Corrective Microvascular Bone Surgery
- •27. Considerations in the Fixation of Bone Grafts for the Reconstruction of Mandibular Continuity Defects
- •28. Indications and Technical Considerations of Different Fibula Grafts
- •29. Soft Tissue Flaps for Coverage of Craniomaxillofacial Osseous Continuity Defects with or Without Bone Graft and Rigid Fixation
- •30. Mandibular Condyle Reconstruction with Free Costochondral Grafting
- •31. Microsurgical Reconstruction of Large Defects of the Maxilla, Midface, and Cranial Base
- •32. Condylar Prosthesis for the Replacement of the Mandibular Condyle
- •33. Problems Related to Mandibular Condylar Prosthesis
- •34. Reconstruction of Defects of the Mandibular Angle
- •35. Mandibular Body Reconstruction
- •36. Marginal Mandibulectomy
- •37. Reconstruction of Extensive Anterior Defects of the Mandible
- •38. Radiation Therapy and Considerations for Internal Fixation Devices
- •39. Management of Posttraumatic Osteomyelitis of the Mandible
- •40. Bilateral Maxillary Defects: THORP Plate Reconstruction with Removable Prosthesis
- •41. AO/ASIF Craniofacial Fixation System Hardware
- •43. Orbital Reconstruction
- •44. Nasal Reconstruction Using Bone Grafts and Rigid Internal Fixation
- •46. Orthognathic Examination
- •47. Considerations in Planning for Bimaxillary Surgery and the Implications of Rigid Internal Fixation
- •48. Reconstruction of Cleft Lip and Palate Osseous Defects and Deformities
- •49. Maxillary Osteotomies and Considerations for Rigid Internal Fixation
- •50. Mandibular Osteotomies and Considerations for Rigid Internal Fixation
- •51. Genioplasty Techniques and Considerations for Rigid Internal Fixation
- •52. Long-Term Stability of Maxillary and Mandibular Osteotomies with Rigid Internal Fixation
- •53. Le Fort II and Le Fort III Osteotomies for Midface Reconstruction and Considerations for Internal Fixation
- •54. Craniofacial Deformities: Introduction and Principles of Management
- •55. The Effects of Plate and Screw Fixation on the Growing Craniofacial Skeleton
- •56. Calvarial Bone Graft Harvesting Techniques: Considerations for Their Use with Rigid Fixation Techniques in the Craniomaxillofacial Region
- •57. Crouzon Syndrome: Basic Dysmorphology and Staging of Reconstruction
- •58. Hemifacial Microsomia
- •59. Orbital Hypertelorism: Surgical Management
- •60. Surgical Correction of the Apert Craniofacial Deformities
- •Index
4
Etiology of Skeletal Malocclusion
Bruce L. Greenberg
Malocclusion is a developmental deformity which may vary from minor to major deformities of dental or skeletal origin, including systemic syndromic anomalies. It may be limited to the maxillofacial bones or encompass the entire craniomaxillofacial region. Because this book is devoted to surgical reconstruction of the craniomaxillofacial skeleton with the goals of achieving normality of health, function, and facial aesthetics, it is important to review how these skeletal malocclusions arise and are classified. Skeletal malocclusion is a set of human craniofacial morphologic characteristics that either exceed or exhibit deficiency of volume and proportion. It results in an improper relationship of the jaws—a relationship that distorts the normal balance of the face, because of difficulties with dental occlusion and the temporomandibular joints. Conceptually this book focuses on the aggregate effect of abnormal growth and development of the distinct skeletal units of the craniofacial anatomy as they relate to function and physical appearance. When considering this problem theoretically, however, the problems of growth and development break down into the interrelationship between human genetics and the response of the genome to the environmental factors that influence its phenotypic expression.
Genetic and functional factors are responsible for skeletal malocclusions and underlie the problems of vertical, sagittal, and transverse interrelationships. The human genome specifies the blueprint for the biochemical components that make up cells, and indeed the aggregate formation of cells as tissues with specialized functions. Genetic expression is the basis for human craniofacial development and represents the responsible mechanisms for how this developmental process may go awry.1 During the process of craniofacial development, neural crest cells play an important role. They migrate into the mesodermal cell layer, becoming the neurovascular bundles, and the head mesenchyme, from which the craniofacial skeleton will form. Fundamentally, the quality and quantity of neural crest cell migration and the distribution of vascular networks during embryogenesis may directly impact favorably or unfavorably on the facial skeletal endowment.2,3 At this early stage of human growth and development, ge-
netic factors signal tissue differentiation. These genetic factors play the most direct role in setting the stage for the skeleton’s formation. The differentiation of tissues into functional units relates to how the genetic qualities of the major functional cranial components interact physiologically with the functional environment to cause developmental changes and balance of the skeletal units.4
This type of genetic and environmental analysis can result in a greater appreciation of the skeletal malocclusions encountered in clinical practice. Physicians can also provide patients with a better prospective understanding of their condition. This has many benefits during diagnosis, treatment planning, treatment, and the posttreatment phases. A patient and or parent who grasps the etiologic causality of the problem will have a more accurate understanding of the condition and hopefully a more realistic set of expectations when assessing treatment outcome. Therefore, each type of skeletal malocclusion will be considered, with a discussion of the genetic and functional aspects of its development.
Most basically, all malocclusions may be categorized as Class I, Class II, or Class III, based upon Angle’s classification (Figure 4.1). However, skeletal malocclusion must be considered in terms of the three dimensions of craniofacial anatomy—defined as the vertical, sagittal, and transverse planes of space. These parameters serve as the basis for the assessment of skeletal malocclusions and allow clinicians to understand that from a genetic and functional perspective, these three dimensions are clearly interrelated. An isolated distortion in one of these dimensions will impact upon the others to result in a clinical abnormality.5
Sagittal Interrelationships
Sagittal problems will exhibit either a skeletal open bite or a skeletal deep bite, with retrognathic or prognathic jaw relationships. Transverse problems may result in asymmetry, open bite, deep bite, retrognathia, or prognathism. The dimensions of skeletal anatomy are, as well, intimately interrelated.
38
4. Etiology of Skeletal Malocclusion |
39 |
a |
b |
c |
d |
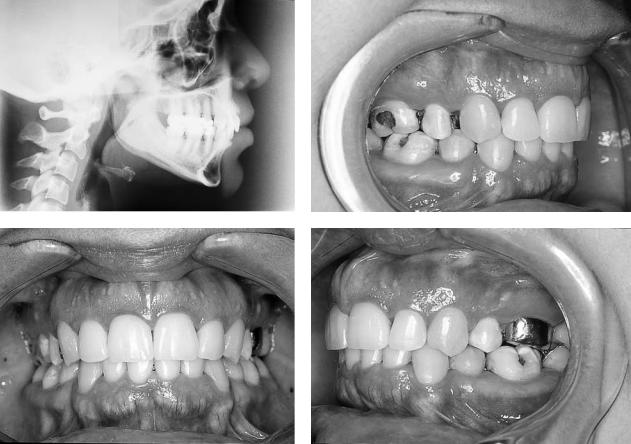
FIGURE 4.1 (a) Lateral cephalometric radiograph demonstrating Class I occlusion. (b) Intraoral view of right lateral aspect of Class I occlusion. (c) Intraoral view of frontal aspect of Class I occlusion. (d) Intraoral view of left lateral aspect of Class I occlusion.
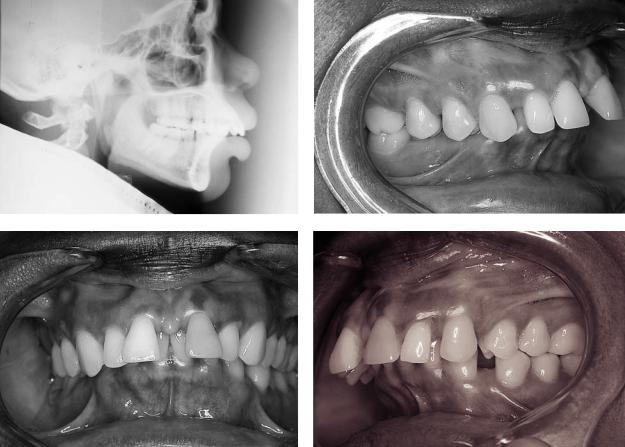
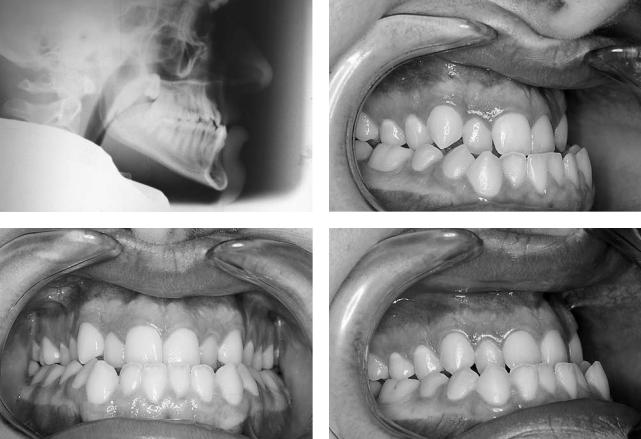
Because of the interrelationships among the skeletal dimensions, a severe mandibular retrognathia can imply a transverse problem. The narrow part of the mandibular arch may occlude with the wider aspect of the maxillary arch (Figure 4.2). Similarly a prognathic mandible relates the wider part of the mandibular arch to the narrower part of the maxillary arch (Figure 4.3). Both of these situations imply a transverse occlusal problem resulting from either a Class II or Class III skeletal relationship. The Class II maxillomandibular relationship may also result in a vertical deficiency because of the geometric overclosure of the jaws that accompanies a severe overjet. The Class III will tend toward a vertical excess because of the underclosure that accompanies underjet and its inherent lengthening of the lower third of the face.
Vertical Interrelationships
Vertical and sagittal dimensions are closely interrelated. As the vertical dimension increases, the mandible will rotate distally, accentuating a retrognathia. On the other hand, a decreased vertical dimension will result in a mesial
mandibular rotation accentuating a prognathia. Pure vertical problems usually do not impact on the transverse dimension greatly.
Transverse Interrelationships
The transverse dimension impacts on both the vertical and the sagittal dimensions because of the role of dental anatomy on skeletal jaw positions, which is also related to direct skeletal incompatibilities. A jaw width mixmatch, with its associated containment of the maxillary dental arch within the mandibular dental arch, will cause distal mandibular rotation and a resultant retrognathia with anterior open bite. In contradistinction, containment of the mandibular dental arch within the maxillary dental arch, a much more infrequent condition, will lead to mesial mandibular rotation and mandibular prognathism as well as deep bite. Asymmetric relationships of the jaws tend to result in unilateral crossbites, chin point deviation, and midfacial asymmetry, and will vary in their sagittal and vertical effects depending on such factors as dental compensations and condylar positioning.6
40 |
B.L. Greenberg |
a |
b |
c |
d |
FIGURE 4.2 (a) Lateral cephalometric radiograph demonstrating Class II occlusion. (b) Intraoral view of right lateral aspect of Class II occlusion. (c) Intraoral view of frontal aspect of Class II occlusion. (d) Intraoral view of left lateral aspect of Class II occlusion.
Specific examples of how these genetic and environmental factors affect the craniofacial skeleton can be appreciated in ways that permit interpretation of skeletal malocclusion. Consider facial asymmetries such as the hemifacial microsomias. This is a good example of how early vascular imbalance may fail to adequately support the neural crest derived head mesenchyme leading to a quantitative tissue deficit. The reduced tissue endowment ultimately means a reduced volume of connective tissue mass and musculoskeletal formation. For bone as with adipose tissue, it is the cell count that is most important. The osteogenic potential that is derived from these early developmental processes ultimately contributes to cell numbers. Although the genetic factors seem to override the embryonic events of neural crest migration as a primitive influence, the later phenotypic expression of cell morphologic type and number plays a significant role in understanding the functional cranial components. Functions of the craniofacial skeleton include vision, olfaction, respiration, deglutition, speech, and hearing. Clearly there is tremendous sensory input and motor output occurring throughout the craniofacial complex. To the extent that, for example, the lining tissues composing these functional cranial components exhibit their genetic phenotype in a normal way, skeletal units will tend to follow suit.
If the genetics are unfavorable in terms of the quality and quantity of secretions following an immunohistochemical mechanism, the functional cranial component may be disturbed. The result may be abnormal, although obligatory and compensatory, skeletal morphologic changes that may have an unfavorable impact on skeletal development.7 Perhaps the clearest application of this phenomenon is in the adenoid faces in which tonsillar and adenoid tissue masses along with the lining respiratory epithelium contribute to an altered pattern of breathing, jaw posture, tongue posture, and muscle tone. This leads to excessive vertical skeletal growth, distal mandibular rotation, mandibular retrognathia, and apertognathia.
The timing of craniofacial sutural closure and fusion will also be a result of the genomic expression and may significantly affect the symmetry of the entire upper, middle, and lower facial thirds, quite often demonstrating a significant torsion of the facial skeleton. This may often be seen as a significant deviation of the nasal septum toward the longer side of the face and of the chin to the shorter side of the face. For example, if the right side of the face grows for a longer period of time than the left side, the right eye will be observed to be higher than the left, the nasal septum will deviate to the right side with a bowing of the nasal complex around a cen-
4. Etiology of Skeletal Malocclusion |
41 |
a |
b |
c |
d |
FIGURE 4.3 (a) Lateral cephalometric radiograph demonstrating Class III occlusion. (b) Intraoral view of right lateral aspect of Class III occlusion. (c) Intraoral view of frontal aspect of Class III occlusion. (d) Intraoral view of left lateral aspect of Class III occlusion.
ter of rotation being to the left of the midline, and the right mandible will be longer with the chin deviated to the left side.8 All too often, deviation of the chin point with a resultant mandibular asymmetry is attributed to condylar dysgenesis, which is often incorrectly diagnosed. Bone scans later reveal normal metabolism. However, this does not mean to exclude the cases of actual condylar hyperplasia. The condyle may be considered one of the multifocal mandibular growth centers, which are characterized by epiphyseal bone formation. Genetic regulation of endochondral ossification in these structures may be unilaterally flawed to result in an asymmetric Class III malocclusion. Head and neck osteogenesis is also influenced by intramembranous ossification, which in the case of disruption of the growth potential of the orbital contents will lead to a consequent maxillary deformity. This may also be associated with potential overgrowth of the maxillary sinus without the balancing functional limitation of the orbit, resulting in maxillary hypertrophy and consequent changes in the dental occlusion. So we can see that there is an underlying interrelationship between what the genome programs and the environment may influence, which aids in our understanding the phenomenon of craniofacial growth and development.9 For example, analysis of the cranial base angle pro-
vides another determinant of the jaw relationship and may be a contributing factor to skeletal malocclusion. A highly deflected cranial base will tend to position the craniomandibular articulation more anteriorly and inferiorly. This would contribute to the Class III as well as the brachyfacial pattern. The minimally deflected cranial base will tend to position the articulation more posterosuperiorly, favoring the Class II as well as dolichofacial pattern.10 Clearly abnormal jaw growth and development may be rooted in fundamental genetic and longterm environmental influences, which more often than not are refractory to modification with functional orthopedic appliances and dentofacial orthopedics. Ultimately, the combined approaches of orthodontics and orthognathic surgery are the only means of correcting the skeletal malocclusion upon completion of growth.
Reconstructive craniomaxillofacial surgery requires the operating surgeon and other members of the team to restore the patient to the correct functional and cosmetic skeletal jaw, occlusal, and facial relationships and dimensions. Whatever the patient’s preexisting occlusal relationship, it should be restored inthemostoptimalway.Correctivecraniomaxillofacialsurgery differs in its approach—selective surgical, orthodontic, and restorative dental procedures alter the skeletal jaw relationship
42
to the cranial base, ultimately achieving the goals of a Class I occlusion with optimal facial esthetics and temporomandibular joint function. Utilizing diagnostic tests and skills to establish objective criteria based on a thorough grasp of the etiology of skeletal malocclusion allows for proper treatment planning for reconstructive and corrective craniomaxillofacial surgery.
References
1.Enlow DH, Hans MG. Essentials of Facial Growth. Philadelphia: W.B. Saunders; 1996.
2.Monroy A, Moscona AA. Introductory Concepts in Developmental Biology. Chicago: University of Chicago Press; 1979.
B.L. Greenberg
3.Moss ML. Neurotropic processes in orofacial growth. J Dent Res. 1971;50:1492.
4.Moss ML. Genetics, epigenetics, and causation. Am J Orthod. 1950;36:481.
5.Arnett GW, Bergman RT. Facial keys to orthodontic diagnosis and treatment planning, Part I. Am J Orthod. 1993;103:299.
6.Arnett GW, Bergman RT. Facial keys to orthodontic diadnosis and treatment planning, Part II. Am J Orthod. 1993;103:395.
7.Moss ML. The primary role of functional matrices in facial growth. Am J Orthod. 1969;55:566.
8.Dr. Robert L. Williams. Personal communication.
9.Moss ML, Salentijn L. The capsular matrix. Am J Orthod. 1969B;56:474.
10.Jarabak JR, Fizzell JA. Technique and Treatment with LightWire Edgewise Appliances, Vol. II, 2d ed. St. Louis: C.V. Mosby; 1972.
