
- •Preface
- •Acknowledgments
- •Contents
- •Contributors
- •1. Introduction
- •2. Evaluation of the Craniomaxillofacial Deformity Patient
- •3. Craniofacial Deformities: Review of Etiologies, Distribution, and Their Classification
- •4. Etiology of Skeletal Malocclusion
- •5. Etiology, Distribution, and Classification of Craniomaxillofacial Deformities: Traumatic Defects
- •6. Etiology, Distribution, and Classification of Craniomaxillofacial Deformities: Review of Nasal Deformities
- •7. Review of Benign Tumors of the Maxillofacial Region and Considerations for Bone Invasion
- •8. Oral Malignancies: Etiology, Distribution, and Basic Treatment Considerations
- •9. Craniomaxillofacial Bone Infections: Etiologies, Distributions, and Associated Defects
- •11. Craniomaxillofacial Bone Healing, Biomechanics, and Rigid Internal Fixation
- •12. Metal for Craniomaxillofacial Internal Fixation Implants and Its Physiological Implications
- •13. Bioresorbable Materials for Bone Fixation: Review of Biological Concepts and Mechanical Aspects
- •14. Advanced Bone Healing Concepts in Craniomaxillofacial Reconstructive and Corrective Bone Surgery
- •15. The ITI Dental Implant System
- •16. Localized Ridge Augmentation Using Guided Bone Regeneration in Deficient Implant Sites
- •17. The ITI Dental Implant System in Maxillofacial Applications
- •18. Maxillary Sinus Grafting and Osseointegration Surgery
- •19. Computerized Tomography and Its Use for Craniomaxillofacial Dental Implantology
- •20B. Atlas of Cases
- •21A. Prosthodontic Considerations in Dental Implant Restoration
- •21B. Overdenture Case Reports
- •22. AO/ASIF Mandibular Hardware
- •23. Aesthetic Considerations in Reconstructive and Corrective Craniomaxillofacial Bone Surgery
- •24. Considerations for Reconstruction of the Head and Neck Oncologic Patient
- •25. Autogenous Bone Grafts in Maxillofacial Reconstruction
- •26. Current Practice and Future Trends in Craniomaxillofacial Reconstructive and Corrective Microvascular Bone Surgery
- •27. Considerations in the Fixation of Bone Grafts for the Reconstruction of Mandibular Continuity Defects
- •28. Indications and Technical Considerations of Different Fibula Grafts
- •29. Soft Tissue Flaps for Coverage of Craniomaxillofacial Osseous Continuity Defects with or Without Bone Graft and Rigid Fixation
- •30. Mandibular Condyle Reconstruction with Free Costochondral Grafting
- •31. Microsurgical Reconstruction of Large Defects of the Maxilla, Midface, and Cranial Base
- •32. Condylar Prosthesis for the Replacement of the Mandibular Condyle
- •33. Problems Related to Mandibular Condylar Prosthesis
- •34. Reconstruction of Defects of the Mandibular Angle
- •35. Mandibular Body Reconstruction
- •36. Marginal Mandibulectomy
- •37. Reconstruction of Extensive Anterior Defects of the Mandible
- •38. Radiation Therapy and Considerations for Internal Fixation Devices
- •39. Management of Posttraumatic Osteomyelitis of the Mandible
- •40. Bilateral Maxillary Defects: THORP Plate Reconstruction with Removable Prosthesis
- •41. AO/ASIF Craniofacial Fixation System Hardware
- •43. Orbital Reconstruction
- •44. Nasal Reconstruction Using Bone Grafts and Rigid Internal Fixation
- •46. Orthognathic Examination
- •47. Considerations in Planning for Bimaxillary Surgery and the Implications of Rigid Internal Fixation
- •48. Reconstruction of Cleft Lip and Palate Osseous Defects and Deformities
- •49. Maxillary Osteotomies and Considerations for Rigid Internal Fixation
- •50. Mandibular Osteotomies and Considerations for Rigid Internal Fixation
- •51. Genioplasty Techniques and Considerations for Rigid Internal Fixation
- •52. Long-Term Stability of Maxillary and Mandibular Osteotomies with Rigid Internal Fixation
- •53. Le Fort II and Le Fort III Osteotomies for Midface Reconstruction and Considerations for Internal Fixation
- •54. Craniofacial Deformities: Introduction and Principles of Management
- •55. The Effects of Plate and Screw Fixation on the Growing Craniofacial Skeleton
- •56. Calvarial Bone Graft Harvesting Techniques: Considerations for Their Use with Rigid Fixation Techniques in the Craniomaxillofacial Region
- •57. Crouzon Syndrome: Basic Dysmorphology and Staging of Reconstruction
- •58. Hemifacial Microsomia
- •59. Orbital Hypertelorism: Surgical Management
- •60. Surgical Correction of the Apert Craniofacial Deformities
- •Index
57
Crouzon Syndrome: Basic Dysmorphology and Staging of Reconstruction
Jeffrey C. Posnick
Crouzon syndrome is the most frequent form of craniofacial dysostosis.1–6 It is characterized by multiple anomalies of the craniofacial skeleton. Its manifestations are generally less severe than those of Apert syndrome, and there is no involvement of the extremities. Typically, the cranial vault presentation is a brachycephalic shape to the skull caused by premature synostosis of both coronal sutures. Cranial vault suture involvement, other than coronal, may include sagittal, metopic, or lambdoidal in isolation or in any combination. The cranial base and upper face sutures are generally involved, resulting in a variable degree of midface hypoplasia with an angle class III malocclusion. The orbits are hypoplastic, resulting in a degree of proptosis with additional orbital dysplasia that may produce a mild to moderate orbital hypertelorism and flatness to the (transverse) arc of rotation of the midface.7–13
The lack of consensus about the timing and techniques used at each stage of reconstruction reflects uncertainty about the functional consequences of the congenital dysmorphology and inconsistencies of the results achieved with any one approach to treatment.14–41 Accurate objective methods for documentation of either the presenting deformity or initial and late postoperative results are few. Too much reliance has been placed on the subjective assessment of both the presenting deformity and the postoperative results achieved.
Functional Considerations
Brain volume in the normal child almost triples in the first year,42–46 and by 2 years the cranial capacity is four times that at birth. In craniosynostosis, premature suture fusion is combined with continuing brain growth. Depending on the number, location, and rate of prematurely fused sutures, the growth of the brain may be restricted. If early surgical intervention with suture release, decompression, and reshaping to restore a more normal intracranial volume and configuration does not reverse the process, diminished central nervous system function may be the end result. Elevated intracranial pressure is the most important functional problem
associated with premature suture fusion.26,32,34,40 If intracranial hypertension goes untreated, brain function is adversely affected.
When craniosynostosis is associated with increased intracranial pressure, optic nerve compression occurs. Initially, there is papilloedema with eventual optic atrophy that results in partial or complete blindness. Fundoscopic examination of the retina should reveal papilloedema, allowing for surgical intervention to limit the late effects.
If the orbits are shallow and the eyes proptotic, corneal drying may occur, which can result in ulceration. If the orbits are extremely shallow, herniation of the globes may occur, requiring emergency reduction. Divergent or convergent nonparalytic strabismus or exotropia occurs frequently and should be looked for and treated. Hydrocephalus affects 5% to 10% of children with Crouzon syndrome.47 Although the etiology is not always clear, hydrocephalus may be secondary to a generalized cranial base stenosis with constriction of the cranial base foramina. When the clinical examination is correlated with serial computed tomographic (CT) scans or magnetic resonance imaging to document progressively enlarging ventricles, a more accurate diagnosis can be determined. When hydrocephalus is detected, prompt ventriculoperitoneal shunting should be performed.
All neonates are obligate nasal breathers. A significant percentage of children born with Crouzon syndrome have severe hypoplasia of the midface with diminished nasal and nasopharyngeal spaces. This malformation increases nasal airway resistance and forces infants to breathe primarily through their mouth. This type of breathing may result in inadequate oxygenation with a tracheostomy being required.
In Crouzon syndrome, conductive hearing deficit is frequently encountered, and atresia of the external auditory canals may also occur.48
Aesthetic Assessment
Examination of the entire craniofacial region (skeletal and soft tissues) should be systematic and complete. Specific findings
713
714
are frequent in Crouzon syndrome, but each patient is unique. Achievement of symmetry, proportionality, and balance is critical to reconstructing an attractive face in a child born with Crouzon syndrome.
The upper third of the face is generally dysmorphic in an infant born with Crouzon syndrome. The establishment of the preferred position of the forehead is essential to the overall facial balance.49 The forehead is divided into two separate components, the supraorbital ridge and the superior forehead. The supraorbital ridge includes the glabella region; the supraorbital rim and its lateral extension posteriorly along the temporoparietal bones; and inferiorly down the frontozygomatic suture region. In Crouzon syndrome with brachycephaly present, this component is retruded and wide. Ideally, the eyebrows, overlying the supraorbital ridges, should rest anterior to the cornea when viewed in profile. When the supraorbital ridge is viewed from above, the rim should arc posteriorly to achieve a gentle 90° angle at the temporal fossa with the center point of the arc located at the level of each frontozygomatic suture. The superior forehead component, about 1.5 cm up from the supraorbital rim, has a gentle posterior curve of 60°, leveling out at the coronal suture region when seen in profile. The brachycephalic skull of Crouzon syndrome lacks this preferred superior forehead morphology.
In Crouzon syndrome, presenting with bilateral coronal suture synostosis extending into the cranial base, the orbitonasozygomatic region is wide and lacks forward projection. These findings are consistent with a short and wide anterior cranial base. Overall midface projection is deficient, and the upper anterior face appears vertically short from the nasion to the maxillary central incisors.8,9,12
Quantitative Assessment
The purpose of a quantitative assessment of the craniofacial complex by CT scan analysis,9,12,50–54 anthropometric measurements,8,55 cephalometric analysis, and dental model analysis is to help predict growth patterns, confirm or refute clinical impressions, aid in treatment planning, and provide a framework for objective assessment of the immediate and long-term reconstructive results.
We developed a method of analysis based on CT scan measurements which allows for a more quantitative assessment of the cranio-orbito-zygomatic skeleton in both the horizontal and transverse planes.50,51 A normative database is established using this system which enables comparison of an individual patient’s cranio-orbito-zygomatic morphology with that of an age-matched cohort group.51
Posnick et al. developed this method of quantitative CT scan analysis and then used it to document the differences in the cranio-orbito-zygomatic region between unoperated chil-
J.C. Posnick
dren with Crouzon syndrome and age-matched controls.9,12 Posnick et al. also evaluated the morphologic results achieved in those children 1 year after undergoing a standard suture release, anterior cranial vault, and upper orbital procedure designed to decompress and reshape these regions.12
The preoperative CT scan measurements of these unoperated Crouzon children confirmed a widened anterior cranial vault at 108% of normal and a cranial length averaging only 92% of normal. In comparison with age-matched controls, orbital measurements revealed a widened anterior interorbital distance at 122% of normal, an increased intertemporal width at 121% of normal, globe protrusion at 119% of normal, and a short medial orbital wall distance at only 86% of normal. The distance between the zygomatic buttresses and the interarch distances were found to be increased at 106% and 103% of normal, respectively. The zygomatic arch lengths were substantially shortened at only 87% of age-matched control values.12 These findings confirmed clinical observations of brachycephalic anterior cranial vaults with shallow, frequently hyperteloric orbits and globe proptosis. Generally, the Crouzon midface is horizontally retrusive and transversely wide, reflected in wide and shortened zygomas.
The same quantitative CT scan assessment was carried out in the operated Crouzon children more than 1 year after undergoing anterior cranial vault and upper orbital osteotomies with reshaping, and when comparing them to the new agematched control values, we were not able to demonstrate any significant improvement in the cranio-orbito-zygomatic measurements.12
In the midchildhood years, another group of Crouzon children were again assessed using the quantitative CT scan measurements.56 They were found to have cranial vault lengths averaging only 87% of the age-matched normals. The medial orbital walls were (horizontally) short at 87% of normal while the extent of globe protrusion was excessive at 134% of agematched norms. The zygomatic arch lengths averaged only 84% of normal. These findings confirmed horizontal (anteroposterior) deficiency of the upper and middle facial thirds. After undergoing a monobloc osteotomy (orbits and midface) combined with anterior cranial vault reshaping and advancement carried out through an intracranial approach, the children’s cranio-orbito-zygomatic measurements were again taken. The mean cranial length initially achieved (after monobloc osteotomy) was 98% and at 1 year 92% of the control value. When compared with age-matched controls, the orbital measurements reflected improvement in the midorbital hypertelorism (midinterorbital distance, 97% initially after operation and 102% at 1 year), and orbital proptosis (soon after surgery, 86%, and at 1 year, 92% of age-matched normals). The medial orbital wall length initially normalized at 101% and later at 97% of normal values. The zygomatic arch length initially corrected at 106% and later to 101% of normal.
57. Crouzon Syndrome: Dysmorphology and Reconstruction
Surgical Approach: Historical Perspective
The first recorded surgical approach to craniosynostosis was performed by Lannelongue in 189057 and Lane in 1892,58 who completed strip craniectomies. Their aim was to control the problem of brain compression within a congenitally small cranial vault. The classic neurosurgical techniques were refined over the ensuing decade and geared toward resecting the synostotic suture(s) in the hope that the “released” skull would reshape itself and continue to grow in a normal and symmetric fashion. The strip craniectomy procedures were supposed to allow for a creation of new suture lines at the sites of the previous synostosis. With the realization that this goal was rarely achieved, attempts were made to fragment the cranial vault surgically with pieces of flat bone used as free grafts to refashion the cranial vault shape. Problems with these methods included uncontrolled postoperative skull molding, resulting in reossification in dysmorphic configurations.
In 1950, Gillies reported his experience with an extracranial (elective) Le Fort III osteotomy to improve the anterior projection of a patient with Crouzon syndrome.59 His early enthusiasm later turned to discouragement when the patient’s facial skeleton relapsed to its preoperative status. In 1967, Tessier described a new (intracranial-cranial base) approach to the management of Crouzon syndrome.17 His landmark presentation and publications were the beginning of modern craniofacial surgery.19,60–64 To overcome Gillies’ earlier problems, Tessier developed an innovative basic surgical approach that included new locations for the Le Fort III osteotomy, a combined intracranial-extracranial (cranial base) approach, use of a coronal (skin) incision to expose the upper facial bones, and the use of autogeneous bone graft. He also applied an external fixation device to help maintain bony stability until healing had occurred.
The concept of simultaneous suture release for craniosynostosis combined with cranial vault reshaping in infants was initially discussed by Rougerie et al.65 and later refined by Hoffman and Mohr in 1976.22 Whitaker et al.66 proposed a more formal anterior cranial vault and orbital reshaping procedure for unilateral coronal synostosis in 1977,66 and then Marchac and Renier published their experience with the “floating forehead” technique for simultaneous suture release and anterior cranial vault and orbital reshaping to manage bilateral coronal synostosis in infancy.67,68
The widespread use of autogenous cranial bone grafting has virtually eliminated rib and hip grafts when bone replacement or augmentation is required in cranio-orbito-zygo- matic procedures.69 This represents another of Tessier’s contributions to craniofacial surgery.62 Phillips and Rahn documented through animal studies the advantages of stable fixation of grafts (lag screw techniques) to encourage early healing and limit graft resorption.70 In current practice, the use of miniand micro internal plate and screw fixation
715
is the preferred form of fixation when stability and threedimensional reconstruction of multiple osteotomized bone segments and grafts are required.71–75
Surgical Approach: Author’s Current
Staging of Reconstruction
Primary Cranio-Orbital Decompression:
Reshaping in Infancy
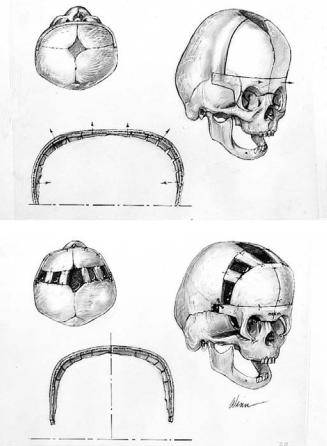
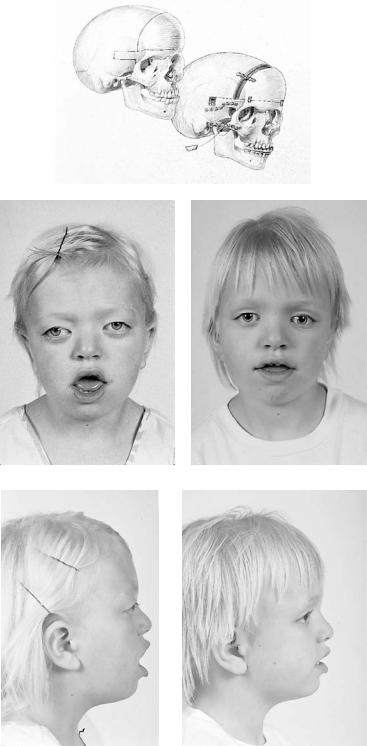
The most common cranial vault suture synostosis pattern associated with Crouzon syndrome is bilateral, premature coronal suture fusion that extends into the cranial base (Figures 57.1–57.3).4 In infancy and early childhood, it is not always possible to separate “simple” brachycephaly (bilateral coronal synostosis) from Crouzon syndrome unless either midface hypoplasia is evident or a family pedigree with an autosomal dominant inheritance pattern is known.4 The midface
FIGURE 57.1 Illustration of the craniofacial skeleton in a child with Crouzon syndrome before and after cranio-orbital reshaping. (Above) Site of osteotomies. (Below) After osteotomies, reshaping, and fixation of the cranio-orbital regions. (From Posnick10)
716 |
J.C. Posnick |
a |
|
|
|
|
|
|
|
b |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
c |
|
|
|
d |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
e |
|
|
|
|
|
f |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
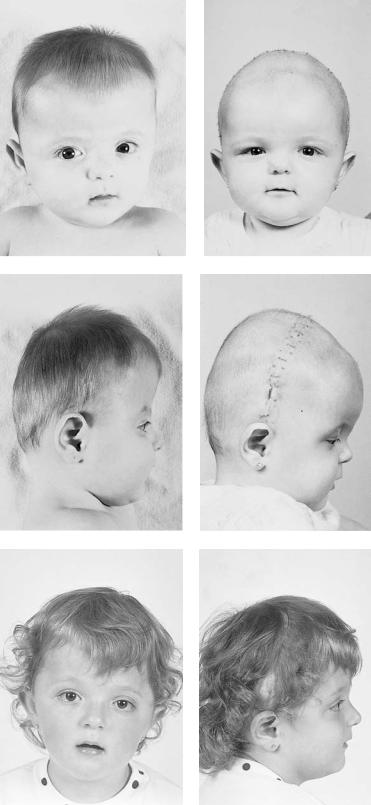
FIGURE 57.2 A 6-month-old girl with Crouzon syndrome underwent cranio-orbital reshaping. (a) Preoperative frontal view. (b) Frontal view 10 days later. (c) Preoperative profile view. (d) Profile view
10 days later. (e) Frontal view 3 years later. (f) Profile view 3 years later. (From Posnick et al.10)
57. Crouzon Syndrome: Dysmorphology and Reconstruction |
717 |
a
b |
c |
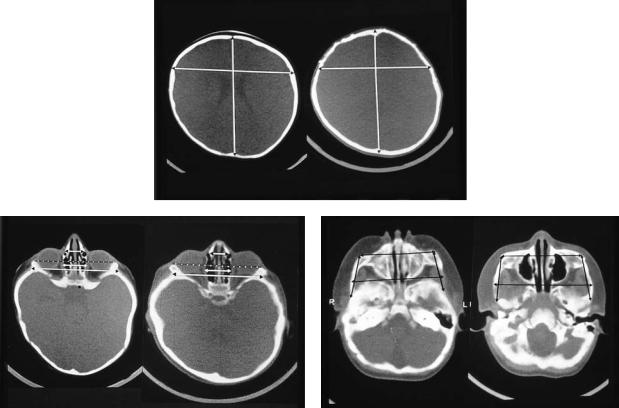
FIGURE 57.3 (a) Comparison of standard axial-sliced CT scans through the cranial vault of the 6-month-old girl with Crouzon syndrome (from Figure 57.2) before and 1 year after cranio-orbital reshaping. The cranial length has increased from 114 to 138 mm. The anterior intracranial width has increased from 100 to 108 mm and remains at 105% of the age-matched controls. (b) Comparison of standard axial-sliced CT scans through midorbit before and 1 year after reconstruction. Globe protrusion has increased from 12 to 17 mm and is now 116% of the age-matched control value. The anterior intraorbital distance has in-
deficiency associated with Crouzon syndrome is variable and not always obvious until later in childhood.4
With early bilateral coronal synostosis, the supraorbital ridge is retruded and the overlying eyebrows are posterior to the cornea of the eyes when viewed in the sagittal plane. The anterior cranial base is short in the anteroposterior (AP) dimension and wide transversely. The cranial vault is high in the superoinferior dimension, with anterior bulging of the upper forehead resulting from compensatory growth through the open metopic and the anterior sagittal sutures. The orbits are generally shallow and the eyes proptotic and with a degree of orbital hypertelorism. The sphenoid wings have a reverse curve, producing the harlequin appearance often described on an AP skull radiograph.
The initial treatment for Crouzon syndrome generally requires bicoronal suture release with decompression of the anterior cranial vault and simultaneous anterior cranial vault
creased from 23 to 26 mm and is now 146% of the control value. The lateral orbital wall distance has increased from 75 to 86 mm and is now 115% of the control value. (c) Comparison of standard axial-sliced CT scans through the zygomatic arches before and 1 year after reconstruction. The increased midface width is confirmed by the interzygomatic buttress and interzygomatic arch distances, both of which have increased to 116% of the age-matched control values. (Magnification of the individual CT scans was not controlled for in this figure.) (From Posnick et al.10)
and upper orbital osteotomies with reshaping and advance- ment.10,12,24,33,41,66–68 My preference is to carry this out when the child is 10 to 12 months old unless signs of increased intracranial pressure are identified earlier in life.10,12,41 Reshaping of the upper three-quarters of the orbital rims and supraorbital ridges is geared to decreasing the bitemporal and anterior cranial base width with simultaneous horizontal advancement to increase the AP dimension. This also increases the depth of the upper orbits with some improvement of the eye proptosis. The overlying forehead is then reconstructed according to aesthetic needs. A degree of overcorrection is preferred at the level of the supraorbital ridge when the procedure is carried out in infancy. It is my clinical impression that by allowing additional growth to occur before first-stage cranio-orbital decompression (waiting until the child is 10 to 12 months old) the improved cranial vault and upper orbital shape is better maintained with less need for repeat craniotomy procedures.

718 |
J.C. Posnick |
Repeat Craniotomy for Additional Cranial Vault Reshaping in Young Children
After the initial suture release, decompression and reshaping is carried out during infancy, the child is followed clinically at intervals by the craniofacial surgeon, pediatric neurosurgeon, pediatric neuro-ophthalmologist, and neuroradiologist along with interval CT scanning. Should signs of increased intracranial pressure develop, urgent decompression with further reshaping to expand the intracranial volume is performed.76 When increased intracranial pressure is suspected, the location of the cranial vault constriction influences the region of the skull for which further decompression and reshaping is planned (Figure 57.4).
If the brain compression is judged to be anterior, further forehead and upper orbital osteotomies with reshaping and
advancement are carried out. The technique is similar to that previously described. If the problem is posterior, decompression and expansion of the posterior cranial vault with the patient in the prone position is required.
The “repeat” craniotomy carried out for further decompression and reshaping in the Crouzon child is often complicated by brittle cortical bone, which lacks a diploic space and contains sharp spicules piercing the dura, the presence of previously placed fixation devices in the operative field (i.e., silastic sheeting with metal clips, stainless steel wires, microplates, and screws) and convoluted dura compressed against (herniated into) the inner table of the skull.75 All these problems result in a higher incidence of dural tears during the calvarectomy than would normally occur during the primary procedure. A greater amount of morbidity should be anticipated when reelevating the scalp flap, dissecting the dura free
a |
|
b |
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
c |
d |
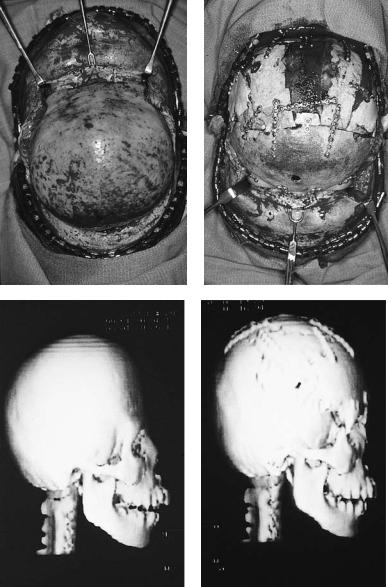
FIGURE 57.4 A 9-year-old girl with unrepaired late, bicoronal synostosis requiring suture release, total cranial vault and upper orbital osteotomies with reshaping and advancement. (a) Preoperative profile view. (b) Profile view after reconstruction. (c) Intraoperative lat-
eral view of cranial vault and upper orbits after elevation of coronal flap. (d) Same view after reconstruction. Stabilization with titanium miniplates and screws. (From Posnick13)
57. Crouzon Syndrome: Dysmorphology and Reconstruction |
719 |
e |
f |
g |
h |
FIGURE 57.4 Continued. (e) Intraoperative bird’s-eye view of cranial vault after elevation of anterior and posterior scalp flaps. (f) Same view after cranial vault and upper orbital osteotomies with reshaping. Stabilization with titanium bone plates and screws. (g) Three-
of the inner table of the skull and cranial base, and then completing the repeat craniotomy.
Management of the Total Midface
Deformity in Childhood
The type of osteotomy selected to manage the “total midface” deficiency/deformity and any residual cranial vault dysplasia should depend on the presenting deformity rather than a fixed universal approach to the midface malformation (Figures 57.5
dimensional CT scan reformation of craniofacial skeleton. Lateral view before reconstruction. (h) Lateral view after reconstruction. (From Posnick13)
and 57.6).13,37,41,56,77,78 The selection of either a monobloc (with or without additional orbital segmentalization), facial bipartition, or a Le Fort III osteotomy to manage the horizontal, transverse, and vertical midface deficiencies/deformities in a patient with Crouzon syndrome will depend on the presenting midface and anterior cranial vault morphology. The presenting dysmorphology is dependent not only on the original malformation but also on the previous procedures carried out and the effect of further skull remodeling in association with brain growth. If the supraorbital ridge with its overlying eyebrows sit in good position when viewed from the

720 |
|
|
|
|
|
|
|
J.C. Posnick |
a |
|
|
|
|
|
|
|
b FIGURE 57.5 A 16-year-old girl with a mild |
|
|
|
|
|
|
|
|
form of Crouzon syndrome is shown before |
|
|
|
|
|
|
|
|
and after undergoing an extracranial Le Fort |
|
|
|
|
|
|
|
|
III osteotomy with advancement. (a) Preop- |
|
|
|
|
|
|
|
|
erative frontal view. (b) Frontal view 1 year |
|
|
|
|
|
|
|
|
after Le Fort III. (c) Preoperative profile view. |
|
|
|
|
|
|
|
|
(d) Profile view at 1 year after Le Fort III. (e) |
|
|
|
|
|
|
|
|
Preoperative worm’s-eye view. (f) Worm’s- |
|
|
|
|
|
|
|
|
eye view at 1 year after Le Fort III. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
c |
|
|
|
d |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
e |
|
|
|
|
|
|
|
f |
|
|
|
|
|
|
|
|
|

57. Crouzon Syndrome: Dysmorphology and Reconstruction |
721 |
g |
h |
i |
j |
k |
l |
FIGURE 57.5 Continued. (g) Occlusal view before surgery. (h) Occlusal view 1 year after Le Fort III. (i), Intraoperative view of zygomatic complex after osteotomies through coronal incision. (j) Intraoperative view after stabilization with titanium bone plates and screws. (k) Intraoperative bird’s-eye view of cranial vault and orbits
through coronal incision. Stabilization of Le Fort III osteotomy with bone plates and screws. Split cranial grafts harvested from left parietal region and interposed in nasofrontal region and zygomatic arches. (l) Lateral cephalometric radiograph before and after reconstruction. (From Posnick13)
722 |
J.C. Posnick |
a
b |
|
|
|
|
|
|
|
c |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
d |
|
|
|
e |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
FIGURE 57.6 A 6-year-old girl with Cruzon syndrome who underwent anterior cranial vault and monobloc osteotomies with reshaping and advancement. (a) Illustration of craniofacial morphology before and after anterior cranial vault and monobloc osteotomies with
advancement. Osteotomy locations indicated. Stabilization with cranial bone grafts and titanium miniplates and screws. (b) Preoperative frontal view. (c) Postoperative frontal view. (d) Preoperative lateral view. (e) Postoperative lateral view 1 year after reconstruction.

57. Crouzon Syndrome: Dysmorphology and Reconstruction |
723 |
|||||||
f |
|
g |
||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
h |
i |
FIGURE 57.6 Continued. (f) Preoperative worm’s-eye view. (g) Postoperative worm’s-eye view 1 year after reconstruction. (h) Threedimensional CT scan reformations after reconstruction. (i) Addi-
sagittal plane with adequate depth of the upper orbits, there is a normal arc of rotation of the midface and forehead in the transverse plane, and the root of the nose is not too wide (orbital hypertelorism), then there is no need to reconstruct this region any further. In such patients, the basic residual upper midface deformity may be effectively managed with an extracranial Le Fort III osteotomy. If the supraorbital ridge and anterior cranial base both remain deficient in the sagittal plane along with the zygomas, nose, lower orbits, and maxilla, a monobloc osteotomy is indicated. In these patients, the forehead is generally flat and retruded, and it will also require reshaping and advancement. If orbital hypertelorism and midface flattening with loss of the normal facial curvature are present, then the monobloc unit is split vertically in the midline (facial bipartition), a wedge of intraorbital (nasal and ethmoidal) bone is removed, and the orbits are repositioned medially while the maxillary posterior arch is widened (this is rarely required in Crouzon syndrome). When a monobloc or facial bipartition osteotomy is carried out as the basic proce-
tional three-dimensional CT scan reformations initially after reconstruction including cranial base view demonstrating increased anteroposterior dimensions achieved. (From Posnick13)
dure, additional segmentalization of the upper and lateral orbits may also be required to complete a satisfactory reconstruction of the upper orbits.
For most patients, an error in judgment will occur if the surgeon attempts to simultaneously adjust the orbits and idealize the occlusion by using the Le Fort III, monobloc, or facial bipartition osteotomies in isolation without completing a separate Le Fort I osteotomy. The degrees of horizontal deficiency at the orbits and maxillary dentition are rarely uniform. This further segmentalization of the midlife complex at the Le Fort I level is required to reestablish normal proportions. If Le Fort I segmentalization of the total midface complex is not carried out and the surgeon attempts to achieve a positive overbite and overjet at the incisor teeth, enophthalmus will frequently result.
Problems specific to the Le Fort III osteotomy when its indications are less than ideal include irregular step defects in the lateral orbital rims that occur when even a moderate advancement is carried out. These step defects are often impossible to
724
effectively modify later. With the Le Fort III osteotomy, an ideal orbital depth is difficult to judge; a frequent result is either residual proptosis or enophthalmus. Simultaneous correction of orbital hypertelorism or correction of a midface arc of rotation problem is not possible with the Le Fort III procedure. Excessive lengthening of the nose, accompanied by flattening of the nasofrontal angle, will also occur if the Le Fort III osteotomy is selected when the skeletal morphology favors a monobloc or facial bipartition procedure.
Final reconstruction of the cranial vault and orbital dystopia problem in Crouzon syndrome can be managed as early as 5 to 7 years of age. By this age, the cranial vault and orbits normally attain approximately 85% to 90% of their adult size.42–46,51 When the basic midface and final cranial vault procedure is carried out at or after this age, the reconstructive objectives are to approximate adult dimensions in the cranio-orbito-zygomatic region with the expectation of a stable result once healing has occurred. Psychosocial considerations also support the time frame of 5 to 7 years of age for the elective basic (total) midface and final cranial vault procedure. When the procedure is carried out at this age, the child may enter the first grade with a real chance for satisfactory self-esteem. Routine orthognathic surgery will be necessary at the time of skeletal maturity to achieve an ideal occlusion, facial profile, and smile.
Management of the Jaw Deformity and
Malocclusion in Adolescents
While the mandible has a normal basic growth potential in Crouzon syndrome, the maxilla does not.79 An angle class III malocclusion resulting from maxillary retrusion with anterior open bite often results. A Le Fort I osteotomy to allow for horizontal advancement, transverse widening, and vertical lengthening is generally required in combination with a genioplasty (vertical reduction and horizontal advancement) to further correct the lower-face deformity. The elective orthognathic surgery is carried out in conjunction with orthodontic treatment and is planned for completion at the time of skeletal maturity (approximately 14–16 years in girls and 16 to 18 years in boys).13
Conclusion
The author’s preferred approach to the management of Crouzon syndrome is to stage the reconstruction to coincide with facial growth patterns, visceral (brain and eye) function, and psychosocial development. Recognition of the need for a staged reconstructive approach serves to clarify the objectives of each phase of treatment for the surgeon, craniofacial team, and family unit. By continuing to define our rationale for the timing and extent of surgical intervention, and then objectively evaluating both function and morphologic outcomes,
J.C. Posnick
we will further improve the quality of life for patients born with Crouzon syndrome.
References
1.Crouzon O. Dysostose cranio-faciale herediataire. Bull Mem Soc Med Hop Paris. 1912;33:545.
2.Jones K. The Crouzon syndrome revisited. J Med Genet. 1973;10:398–399.
3.Cohen MM Jr. An etiology and nosologic overview of craniosynostosis syndrome. Birth Defects Orig Artic Ser. 1975;11: 137–189.
4.Cohen MM Jr, ed. Craniosynostosis: Diagnosis, Evaluation and Management. New York: Raven Press; 1986.
5.Gorlin RJ, Cohen MM Jr, Levin LS. Syndromes of the Head and Neck. 3rd ed. New York: Oxford University Press; 1990:519– 524.
6.Kreiborg S. Birth prevalence study of the Crouzon syndrome: comparison of direct and indirect methods. Clin Genet. 1992; 41:12–15.
7.Kreiborg S, Aduss H. Apert and Crouzon syndromes contrasted. Qualitative craniofacial x-ray findings. In: Marchac D, ed. Craniofacial Surgery. Heidelberg: Springer-Verlag; 1986:92–96.
8.Kolar JC, Munro IR, Farkas LG. Patterns of dysmorphology in Crouzon syndrome: an anthropometric study. Cleft Palate J. 1988;25:235–244.
9.Carr M, Posnick J, Armstrong D, et al. Cranio-orbito-zygomatic measurements from standard CT scans in unoperated Crouzon and Apert infants: comparison with normal controls. Cleft Palate Craniofac J. 1992;29:129–136.
10.Posnick JC. Craniosynostosis: surgical management in infancy. In: Bell WH, ed. Modern Practice in Orthognathic and Reconstructive Surgery. Philadelphia: WB Saunders; 1992:1889–1931.
11.Kreiborg S, Marsh JL, Liversage M, et al. Comparative threedimensional analysis of CT scans of the calvaria and cranial base in Apert and Crouzon syndromes. J Craniomaxillofac Surg. 1993;21:181–188.
12.Posnick JC, Lin KY, Jhawar BJ, Armstrong D. Crouzon syndrome: quantitative assessment of presenting deformity and surgical results based on CT scans. Plast Reconstr Surg. 1993;92: 1027–1037.
13.Posnick JC. Craniofacial dysostosis: management of the midface deformity. In: Bell WH, ed. Modern Practice in Orthognathic and Reconstructive Surgery. Philadelphia: WB Saunders; 1992: 1839–1887.
14.Virchow R. Uber den Cretinismus, nametlich in Franken und uber pathologische Schadelforamen. Verh Phys Med Ges Wurzburg. 1851;2:230.
15.Fowler FD, Ingraham FD. A new method for applying polyeth-
ylene film to the skull in the treatment of craniosynostosis. J Neurosurg. 1957;14:584.
16.Moss ML. The pathogenesis of premature cranial synostosis in man. Acta Anat (Basel). 1959;37:351.
17.Tessier P. Osteotomies totales de la face. Syndrome de Crouzon, syndrome d’Apert: oxycephalies, scaphocephalies, turricephalies. Ann Chir Plast. 1967;12:273–286.
18.Shillito J Jr, Matson DD. Craniosynostosis: a review of 519 surgical patients. Pediatrics. 1968;41:829–853.
57.Crouzon Syndrome: Dysmorphology and Reconstruction
19.Tessier P. The definitive plastic surgical treatment of the severe facial deformities of craniofacial dysostosis. Crouzon’s and Apert’s diseases. Plast Reconstr Surg. 1971;48:419–442.
20.Pawl RP, Sugar O. Zenker’s solution in the surgical treatment of craniosynostosis. J Neurosurg. 1972;36:604–607.
21.Hogeman KE, Willmar K. On Le Fort III osteotomy for Crouzon’s disease in children: report of a four year follow-up in one patient. Scand J Plast Reconstr Surg. 1974;8:169–172.
22.Hoffman HJ, Mohr G. Lateral canthal advancement of the supraorbital margin. A new corrective technique in the treatment of coronal synostosis. J Neurosurg. 1976;45:376–381.
23.Rune B, Selvik G, Kreiborg S, et al. Motion of bones and volume changes in the neurocranium after craniectomy in Crouzon’s disease. A Roentgen stereometric study. J Neurosurg. 1979;50:494–498.
24.Persing J, Babler W, Winn HR, Jane J, Rodeheaver G. Age as a critical factor in the success of surgical correction of craniosynostosis. J Neurosurg. 1981;54:601–606.
25.Kreiborg S. Craniofacial growth in plagiocephaly and Crouzon syndrome. Scand J Plast Reconstr Surg. 1981;15:187–197.
26.Renier D, Sainte-Rose C, Marchac D, et al. Intracranial pressure in craniosynostosis. J Neurosurg. 1982;57:370–377.
27.McCarthy JG, Grayson B, Bookstein F, et al. Le Fort III advancement osteotomy in the growing child. Plast Reconstr Surg. 1984;74:343–354.
28.McCarthy JG, Epstein F, Sadove M, et al. Early surgery for craniofacial synostosis: an 8-year experience. Plast Reconstr Surg. 1984;73:521–533.
29.Kreiborg S, Aduss H. Preand postsurgical facial growth in patients with Crouzon’s and Apert’s syndromes. Cleft Palate J. 1986;23(suppl 1):78–90.
30.Kaban LB, Conover M, Mulliken J: Midface position after Le Fort III advancement: a long-term follow-up study. Cleft Palate J. 1986;23(suppl 1):75–77.
31.Whitaker LA, Bartlett SP, Schut L, Bruce D. Craniosynostosis: an analysis of the timing, treatment, and complications in 164 consecutive patients. Plast Reconstr Surg. 1987;80:195–212.
32.Renier D. Intracranial pressure in craniosynostosis: Pre and postoperative recordings—correlation with functional results. In: JA Persing, MT Edgerton, JA Jane, eds. Scientific Foundations and Surgical Treatment of Craniosynostosis. Baltimore: Williams & Wilkins; 1989;263–269.
33.McCarthy JG, Cutting CB. The timing of surgical intervention in craniofacial anomalies. Clin Plast Surg. 1990;17(1):161–182.
34.Gault DT, Renier D, Marchac D, et al. Intracranial volume in children with craniosynostosis. J Craniofac Surg. 1990;1:1–3.
35.David DJ, Sheen R. Surgical correction of Crouzon syndrome.
Plast Reconstr Surg. 1990;85:344–354.
36.Ortiz-Monasterio F, Fuente del Campo A, Carillo A. Advancements of the orbits and the midface in one piece combined with frontal repositioning for the correction of Crouzon deformities.
Plast Reconstr Surg. 1978;61:4.
37.Posnick JC. Craniofacial dysostosis: staging of reconstruction and management of the midface deformity. Neurosurg Clin North Am. 1991;2:683–702.
38.Richtsmeier JT, Grausz HM, Morris GR, et al. Growth of the cranial base in craniosynostosis. Cleft Palate Craniofac J. 1991;28:55–67.
39.Posnick JC. The role of plate and screw fixation in the treat-
725
ment of craniofacial malformations. In: Gruss JS, Manson PM, Yaremchuk MJ, eds. Rigid Fixation of the Craniomaxillofacial Skeleton. Boston: Butterworth; 1992:512.
40.Posnick JC, Bite U, Nakano P, et al. Indirect intracranial volume measurements using CT scans: clinical applications for craniosynostosis. Plast Reconstr Surg. 1992;89:34–45.
41.Posnick JC. The craniofacial dysostosis syndromes. Current reconstructive strategies. Clin Plast Surg. 1994;21(4):585–598.
42.Blinkov SM, Glezer II, Haigh B. The Human Brain in Figures and Tables: A Quantitative Handbook. New York: Basic Books; 1968.
43.Lichtenberg R. Radiographic du crane de 226 enfants normaux de la naissance a 8 ans. Impressions digitformes, capacite: angles et indices. Thesis. Paris: University of Paris; 1960.
44.Dekaban AS. Tables of cranial and orbital measurements, cranial volume and derived indexes in males and females from 7 days to 20 years of age. Ann Neurol. 1977;2:485–491.
45.Gordon IRS. Measurement of cranial capacity in children. Br J Radiol. 1966;39:377.
46.Farkas LG, Posnick JC, Hrecko T. Anthropometric growth study of the head. Cleft Palate Craniofac J. 1992;29(4):303–308.
47.Hanieh A, Sheen R, David DJ. Hydrocephalus in Crouzon’s syndrome. Child’s Nerv Syst. 1989;5(3):188–189.
48.Baldwin JL. Dysostosis craniofacialis of Crouzon. A summary of recent literature and case reports with emphasis on involvement of the ear. Laryngoscope. 1968;78(10):1660–1676.
49.Cutting C, Dean D, Bookstein FL, et al. A three-dimensional smooth surface analysis of untreated Crouzon’s syndrome in the adult. J Craniofac Surg. 1995;6(6):444–453.
50.Waitzman AA, Posnick JC, Armstrong D, et al. Craniofacial skeletal measurements based on computed tomography: part I. Accuracy and reproducibility. Cleft Palate Craniofac J. 1992; 29:112–117.
51.Waitzman AA, Posnick JC, Armstrong D, et al. Craniofacial skeletal measurements based on computed tomography. Part 2. Normal values and growth trends. Cleft Palate Craniofac J. 1992;29:118–128.
52.Posnick JC, Lin KY, Chen P, et al. Metopic synostosis: quantitative assessment of presenting deformity and surgical results based on CT scans. Plast Reconstr Surg. 1994;93:16–24.
53.Posnick JC, Lin KY, Jhawar BJ, et al. Apert syndrome: quantitative assessment by CT scan of presenting deformity and surgical results after first-stage reconstruction based on CT scan.
Plast Reconstr Surg. 1994;93:489–497.
54.Posnick JC, Lin KY, Chen P, et al. Sagittal synostosis: quantitative assessment of presenting deformity and surgical results based on CT scans. Plast Reconstr Surg. 1993;92:1015–1024.
55.Ward RE, Jamison PL. Measurement precision and reliability in craniofacial anthropometry: implications and suggestions for clinical applications. J Craniofac Genet Dev Biol. 1991;11(3): 156–164.
56.Posnick JC, Waitzman A, Armstrong D, Pron G. Monobloc and facial bipartition osteotomies: quantitative assessment of presenting deformity and surgical results based on computed tomography scans. J Oral Maxillofac Surg. 1995;53(4):358–367.
57.Lannelonque M. De la craniectomie dans la microcephalie. C R Acad Sci 1890;110:1382.
58.Lane LC. Pioneer craniectomy for reflief of mental imbecility due to premature sutural closure and microcephalus. JAMA. 1892;18:49.
726
59.Gillies H, Harrison SH. Operative correction by osteotomy of recessed malar maxillary compound in case of oxycephaly. Br J Plast Surg. 1950;3:123–127.
60.Tessier P. Dysostoses cranio-faciales (syndromes de Crouzon et d’Apert). Osteotomies totales de la face. In: Transactions of the Fourth International Congress of Plastic and Reconstructive Surgery. Amsterdam;1969:774.
61.Tessier P. Relationship of craniosynostoses to craniofacial dysostosis and to faciostenosis: a study with therapeutic implications. Plast Reconstr Surg. 1971(3):224–237.
62.Tessier P. Autogenous bone grafts taken from the calvarium or facial and cranial applications. Clin Plast Surg. 1982(4):531–538.
63.Tessier P. Total osteotomy of the middle third of the face for faciostenosis or for sequelae of Le Fort III fractures. Plast Reconstr Surg. 1971;48:533–541.
64.Tessier P. Recent improvement in the treatment of facial and cranial deformities in Crouzon’s disease and Apert’s syndrome. In: Symposium of Plastic Surgery of the Orbital Region. St. Louis: CV Mosby; 1976:271.
65.Rougerie J, Derome P, Anquez L. Craniostenoses et dysmorphies cranio-faciales: principes d’une nouvelle technique de traitment et ses resultats. Neurochirurgie. 1972;18:429–440.
66.Whitaker LA, Schut L, Kerr LP. Early surgery for isolated craniofacial dysostosis: improvement and possible prevention of increasing deformity. Plast Reconstr Surg. 1977;60:575–581.
67.Marchac D, Renier D. “Le front flottant.” Traitement precoce des facio-craniostenoses. Ann Chir Plast. 1979;24:121–126.
68.Marchac D, Renier D, Jones BM. Experience with the “floating forehead.” Br J Plast Surg. 1988;41:1–15.
69.Zins JE, Whitaker LA. Membranous versus endochondral bone: implications for craniofacial reconstruction. Plast Reconstr Surg. 1983;72:778–785.
J.C. Posnick
70.Phillips JH, Rahn BA. Fixation effects on membranous and endochondral onlay bone graft revascularization. Plast Reconstr Surg. 1988;82:872–877.
71.Luhr HG. Zur Stabilen osteosynthese bei unterkieferfrakturen.
Dtsch Zahnarztl Z. 1968;23:754.
72.Posnick JC. Pediatric cranial base surgery. In: Problems in Plastic and Reconstructive Surgery. Vol. 3. Philadelphia: JB Lippincott; 1993:107–129.
73.Posnick JC. The role of plate and screw fixation in the management of pediatric head and neck tumors. In: Gruss JS, Manson PM, Yaremchuk MJ, eds. Rigid Fixation of the Cranio maxillofacial Skeleton. Stoneham: Butterworth; 1992:956–670.
74.Posnick JC. The role of plate and screw fixation in the treatment of pediatric facial fractures. In: Gruss JS, Manson PM, Yaremchuk MJ, eds. Rigid Fixation of the Craniomaxillofacial Skeleton. Stoneham: Butterworth; 1992:396–419.
75.Posnick JC. The effects of rigid fixation on the craniofacial growth of the rhesus monkeys (Discussion). Plast Reconstr Surg. 1994;93:11–15.
76.Posnick JC, Shah N, Humphreys R, et al. The detection and management of intracranial hypertension following initial suture release and decompression for craniofacial dysostosis syndromes. Neurosurgery. 1995:703–708.
77.Wolfe SA, Morrison G, Page LK, et al. The monobloc frontofacial advancement: do the pluses outweigh the minuses? Plast Reconstr Surg. 1993;91:977–987.
78.Tessier P. The monobloc frontofacial advancement: do the pluses outweigh the minuses? (Discussion). Plast Reconstr Surg. 1993;91(6):988–999.
79.Bu BH, Kaban LB, Vargervik K. Effect of Le Fort III osteotomy on mandibular growth in patients with Crouzon and Apert syndromes. J Oral Maxillofac Surg. 1989;47(7):666–667.
