
- •Preface
- •Acknowledgments
- •Contents
- •Contributors
- •1. Introduction
- •2. Evaluation of the Craniomaxillofacial Deformity Patient
- •3. Craniofacial Deformities: Review of Etiologies, Distribution, and Their Classification
- •4. Etiology of Skeletal Malocclusion
- •5. Etiology, Distribution, and Classification of Craniomaxillofacial Deformities: Traumatic Defects
- •6. Etiology, Distribution, and Classification of Craniomaxillofacial Deformities: Review of Nasal Deformities
- •7. Review of Benign Tumors of the Maxillofacial Region and Considerations for Bone Invasion
- •8. Oral Malignancies: Etiology, Distribution, and Basic Treatment Considerations
- •9. Craniomaxillofacial Bone Infections: Etiologies, Distributions, and Associated Defects
- •11. Craniomaxillofacial Bone Healing, Biomechanics, and Rigid Internal Fixation
- •12. Metal for Craniomaxillofacial Internal Fixation Implants and Its Physiological Implications
- •13. Bioresorbable Materials for Bone Fixation: Review of Biological Concepts and Mechanical Aspects
- •14. Advanced Bone Healing Concepts in Craniomaxillofacial Reconstructive and Corrective Bone Surgery
- •15. The ITI Dental Implant System
- •16. Localized Ridge Augmentation Using Guided Bone Regeneration in Deficient Implant Sites
- •17. The ITI Dental Implant System in Maxillofacial Applications
- •18. Maxillary Sinus Grafting and Osseointegration Surgery
- •19. Computerized Tomography and Its Use for Craniomaxillofacial Dental Implantology
- •20B. Atlas of Cases
- •21A. Prosthodontic Considerations in Dental Implant Restoration
- •21B. Overdenture Case Reports
- •22. AO/ASIF Mandibular Hardware
- •23. Aesthetic Considerations in Reconstructive and Corrective Craniomaxillofacial Bone Surgery
- •24. Considerations for Reconstruction of the Head and Neck Oncologic Patient
- •25. Autogenous Bone Grafts in Maxillofacial Reconstruction
- •26. Current Practice and Future Trends in Craniomaxillofacial Reconstructive and Corrective Microvascular Bone Surgery
- •27. Considerations in the Fixation of Bone Grafts for the Reconstruction of Mandibular Continuity Defects
- •28. Indications and Technical Considerations of Different Fibula Grafts
- •29. Soft Tissue Flaps for Coverage of Craniomaxillofacial Osseous Continuity Defects with or Without Bone Graft and Rigid Fixation
- •30. Mandibular Condyle Reconstruction with Free Costochondral Grafting
- •31. Microsurgical Reconstruction of Large Defects of the Maxilla, Midface, and Cranial Base
- •32. Condylar Prosthesis for the Replacement of the Mandibular Condyle
- •33. Problems Related to Mandibular Condylar Prosthesis
- •34. Reconstruction of Defects of the Mandibular Angle
- •35. Mandibular Body Reconstruction
- •36. Marginal Mandibulectomy
- •37. Reconstruction of Extensive Anterior Defects of the Mandible
- •38. Radiation Therapy and Considerations for Internal Fixation Devices
- •39. Management of Posttraumatic Osteomyelitis of the Mandible
- •40. Bilateral Maxillary Defects: THORP Plate Reconstruction with Removable Prosthesis
- •41. AO/ASIF Craniofacial Fixation System Hardware
- •43. Orbital Reconstruction
- •44. Nasal Reconstruction Using Bone Grafts and Rigid Internal Fixation
- •46. Orthognathic Examination
- •47. Considerations in Planning for Bimaxillary Surgery and the Implications of Rigid Internal Fixation
- •48. Reconstruction of Cleft Lip and Palate Osseous Defects and Deformities
- •49. Maxillary Osteotomies and Considerations for Rigid Internal Fixation
- •50. Mandibular Osteotomies and Considerations for Rigid Internal Fixation
- •51. Genioplasty Techniques and Considerations for Rigid Internal Fixation
- •52. Long-Term Stability of Maxillary and Mandibular Osteotomies with Rigid Internal Fixation
- •53. Le Fort II and Le Fort III Osteotomies for Midface Reconstruction and Considerations for Internal Fixation
- •54. Craniofacial Deformities: Introduction and Principles of Management
- •55. The Effects of Plate and Screw Fixation on the Growing Craniofacial Skeleton
- •56. Calvarial Bone Graft Harvesting Techniques: Considerations for Their Use with Rigid Fixation Techniques in the Craniomaxillofacial Region
- •57. Crouzon Syndrome: Basic Dysmorphology and Staging of Reconstruction
- •58. Hemifacial Microsomia
- •59. Orbital Hypertelorism: Surgical Management
- •60. Surgical Correction of the Apert Craniofacial Deformities
- •Index
40
Bilateral Maxillary Defects: THORP Plate Reconstruction with Removable Prosthesis
Technique/Atlas Case Reports
Christian Lindqvist, Lars Sjövall, Anna-Lisa Söderholm, and Dorrit Hallikainen
Bilateral total maxillectomy is an uncommon surgical procedure. The indication is usually a large malignant tumor extending over the maxillary midline. Few reports can be found in the literature concerning surgical reconstructive procedures.1,2 Postsurgical prosthetic treatment is another subject that has seldom been discussed. The goal of maxillary reconstruction should always be for a prosthetic solution that makes it possible for the patient to eat, chew, swallow, and speak as normally as possible. It is also important that the aesthetic result should be satisfactory, and the appliance easy to use and clean (especially for disabled and elderly patients).
Following maxillectomy, the palate is often closed with a pedicled or free flap, when the defect is considered to be too large to be obturated only with a prosthetic device. Masticatory rehabilitation after palatal resection may be difficult when a myocutaneous flap has been used for reconstruction. In such cases, the prosthodontist often does not have an underlying stable hard tissue bed for stabilization and retention of the prosthesis. Because of the bulky, often excessive, soft tissue, the use of osseointegrated implants is also difficult. Custommade abutment extension frameworks are needed, which in turn may transmit undesirable bending forces to the implants.
The lack of retention of the prosthetic replacement is generally agreed to be a major problem. This is particularly true of the postsurgical healing phase, when sufficient adaptation of the intermediate prosthesis is hard to achieve.
The titanium hollow-screw reconstruction plate (THORP) system, originally designed for mandibular reconstruction,3,4 might in certain cases be considered for use in midfacial reconstruction. Because of the rigid locking of the screw head and the plate, the neutrally loaded device acts as both an internal and external fixator without causing unphysiologic pressure on the bone underneath.
Case 1
A 76-year-old woman had a large squamous cell carcinoma (SCC) of the edentulous maxilla (Figure 40.1). Bilateral total maxillectomy, including both hard and soft tissues, was
performed at primary surgery. The dorsal part of the soft palate was left intact. An AO-THORP reconstruction plate was anchored to both zygomatic bones by two hollow screws on each side. A split-thickness skin graft was used to cover the resected soft tissue area. The middle of the reconstruction plate was left exposed (Figure 40.2). The patient’s complete upper denture was then used as an interim prosthesis dressing plate, and was temporarily stabilized by bilateral circumzygomatic wiring.
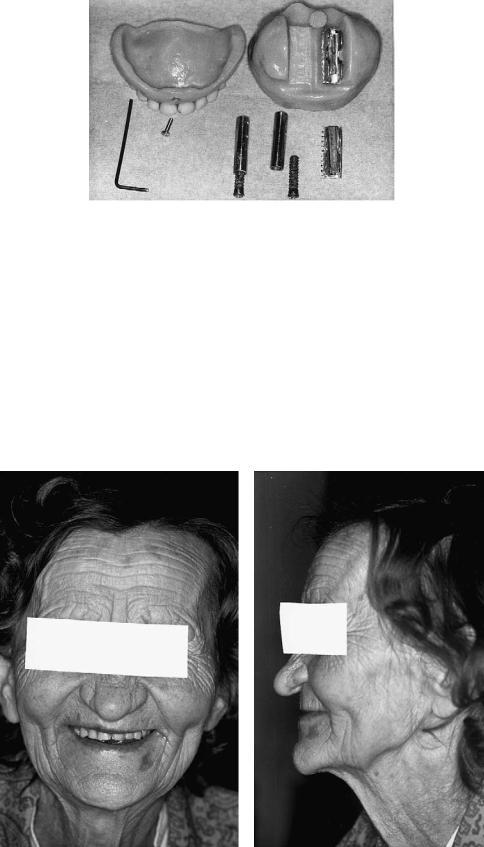
Prosthetic treatment was initiated 5 months later. Using the existing complete upper denture as a tray, an impression of the resected area was obtained. The fairly nonresilient, thin skin graft overlying the hard tissues allowed the use of a putty silicone (Coltoflax, Coltene, Switzerland) instead of a standard impression material. Thus it was possible to place a section of an actual THORP plate accurately in the impression and to have a dental cast made to reproduce the clinical situation (Figure 40.3). The plane of occlusion and the vertical dimension were registered by keeping the denture in the desired position while the impression material was setting. The existing complete lower denture was relined. Two 20mm hollow screws, similar to those attaching the THORP plate to the zygomas, were then fixed to the exposed part of the plate. Chromium-cobalt sockets were attached to the hollow screws with self-curing composite resin (Figure 40.4). The prosthesis consists of two parts: an obturator and a conventional complete upper denture. The obturator is attached to the sockets by individually cast, chromium-cobalt clips. The denture part again is fixed to the obturator by a dorsal undercut and a screw in the front (Figure 40.5). A two-part construction was chosen to facilitate handling of the prosthesis during daily insertion and removal for cleaning. Later on, the two parts were fused, owing to the patient’s improved skill in handling the prosthesis. The clips were adjusted to provide maximal retention while enabling the patient herself to remove the prosthesis (without assistance). The patient is now able to speak clearly and leads a normal social life. She did not lose any weight during the first postoperative year (Figure 40.6).
Five years postoperatively, the plate is completely stable.
439
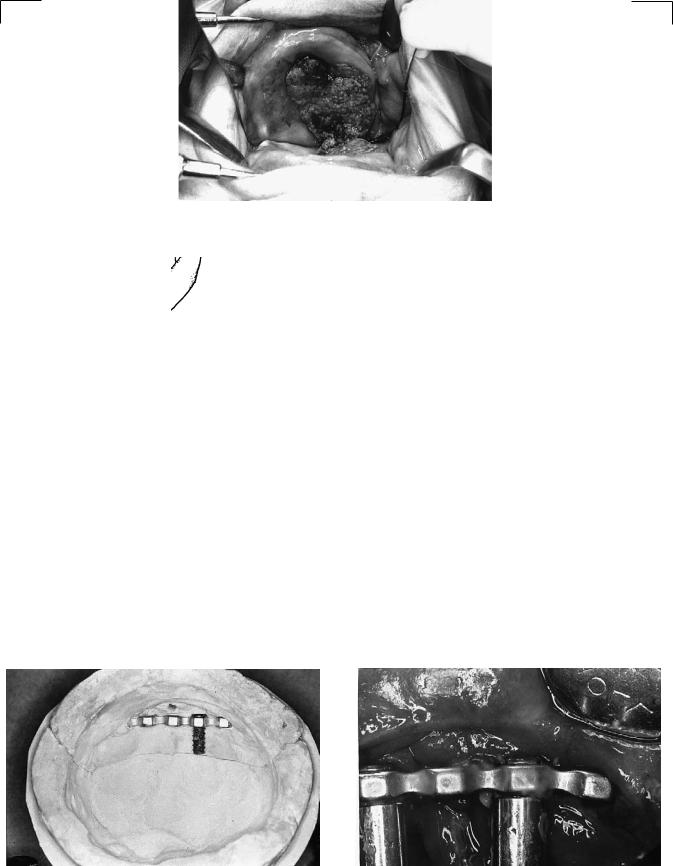
FIGURE 40.1 Case 1. Preoperative view showing extensive squamous cell carcinoma of the patient’s upper jaw.
FIGURE 40.2 Drawing of a skull with the AO-THORP plate anchored to zygomas.
FIGURE 40.3 Stone cast showing the resected undercut free maxillary area with exposed part of plate clearly visible.
FIGURE 40.4 Chromium-cobalt sockets connected by hollow screws and composite resin to exposed part of palate.
40. Bilateral Maxillary Defects: THORP Plate Reconstruction with Removable Prosthesis |
441 |
FIGURE 40.5 Prosthetic components. Clips were fixed to the obturator in the mouth by cold-curing acrylic resin.
Radiologically, no osteolysis can be found around the hollow screws (Figure 40.7). It is likely that osseointegration of the fixation screws has occurred.
Case 2
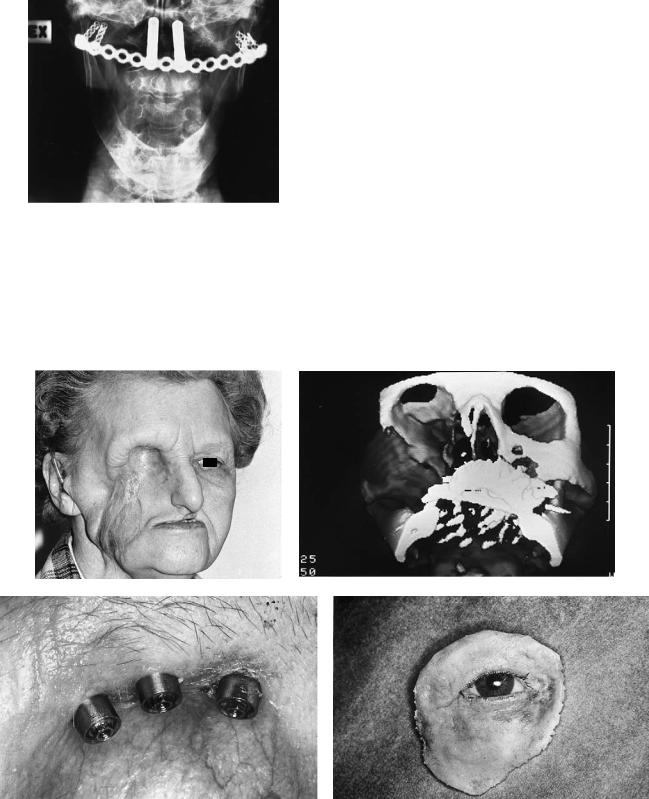
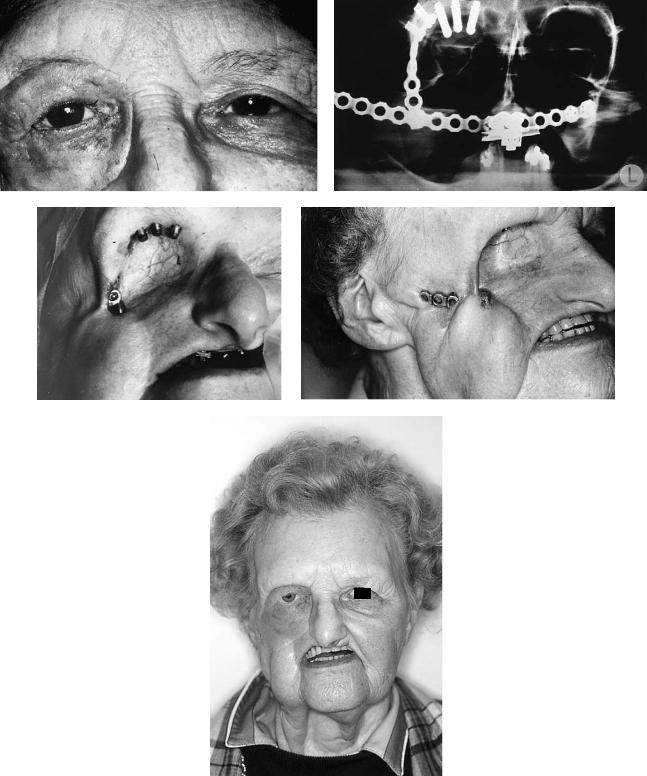
Bilateral subtotal maxillectomy and right orbital exenteration with excision of the right cheek area had been undertaken 12 months earlier in a 74-year-old woman because of an extensive SCC. The palate and skin were reconstructed with a latis-
simus dorsi flap. Postoperatively, 70-Gy radiation therapy was given. No prosthetic rehabilitation was possible, and the patient had significant problems with chewing and swallowing. The aesthetic situation was not satisfactory (Figure 40.8a). The patient was sent to us, and reconstruction was performed with a THORP plate in the same manner as in case 1. Because of a very small area for fixation of the horizontal bar to the right zygoma, a vertical one was attached to the lateral side of the orbit and was connected to the horizontal bar (Figure 40.8b). Three Brånemark implants were also placed in the supraorbital rim. The latissimus dorsi flap was partially re-
a |
b |
FIGURE 40.6 (a,b) Patient’s appearance 18 months and 36 months after tumor surgery.
442
FIGURE 40.7 Radiograph showing plate in place.
a
c
C. Lindqvist et al.
moved to create space for the prosthesis. Skin and soft tissues were reconstructed with a pectoralis major musculocutaneous flap. The prosthetic part of the treatment was accomplished by attaching a fixation device to the THORP plate for the one-part acrylic prosthesis. Eight months later, an orbital epithesis was fabricated after attaching the abutments to the three Brånemark fixtures (Figure 40.8c–f). Healing was uneventful, but 27 months postoperatively the vertical THORP bar became exposed through the skin (Figure 40.8g), and this part was removed. The horizontal part of the THORP plate had also become exposed and was covered with a temporal flap (Figure 40.8h). Forty-two months after the primary plate reconstruction, the patient still has the ability to chew and swallow well. Her speech is intelligible and the aesthetic situation is satisfactory (Figure 40.8i).
An excellent description of different methods for retention of maxillary obturators has been presented by Milton et al.5 They have used, among others, springs attached to the patient’s upper and lower dentures, and magnets. Retention can also be achieved by using undercuts created by the scar band. However, this often leads to sore spots and, in some cases,
b
d
FIGURE 40.8 (a) Case 2. Preoperative photograph before reconstruction. (b) Preoperative three-dimensional CT scan showing the extensive defect. Only the zygomatic process of the temporal bone is left of the whole zygomatic complex. (c) Three abutments in the
supraorbital margin. (d) The epithesis. (e) Epithesis in place. (f) Radiograph showing reconstruction. (g) Exposure of the orbital bar. (h) Horizontal part exposed. (i) Final result.
40. Bilateral Maxillary Defects: THORP Plate Reconstruction with Removable Prosthesis |
443 |
||||
e |
f |
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
g |
|
h |
|
|
|
i
FIGURE 40.8 Continued.
444
pressure ulcers refractory to treatment. One also needs to keep in mind that the thin split-thickness skin graft often used to cover the resection wound is highly sensitive to abrasion and mechanical loading. Coffey6 presents a technique for obturation of maxillary defects with inflatable balloons. However, there are technical problems, such as puncture of the balloon or leakage through the needle valve system.
The best functional and aesthetic result can probably be achieved with a prosthesis minimally supported by soft tissues and maximally supported by a framework attached to the facial bones by osseointegrated titanium screws. Parel et al.7 present a case in which a nasal epithesis and a maxillary prosthesis were both attached to an implant-borne framework.
The use of a reconstruction system fixed to the facial bones in the presence of radiation therapy may be considered controversial. Presurgical or postsurgical irradiation of the tumor and adjacent hard and soft tissues is usually part of the treatment of the malignancy. The osteogenetic potential of irradiated bone is markedly lower, perhaps even permanently.8,9 Still, there are reports of successful treatment with osseointegrated implants in irradiated bone.9 The success rate, however, is lower than in long-term studies concerning nonirradiated bone. On the other hand, Jacobsson9 has reported connective tissue growth around the sites of lost fixtures in radiated subjects, without signs of infection or osteoradionecrosis. Thus, there seems to be only a minor risk of severe complications when a titanium implant (or screw) is lost because of nonosseointegration. Accordingly, implantation should be considered in limited cases when the possibilities for rehabilitation are almost impossible from a prosthodontic point of view.
It is generally agreed that exposure of a mandibular reconstruction plate is a complication that often leads to infection of adjacent tissues, necrosis of the underlying bone, and loss of the plate. Although it might have been assumed that this would be the final result in these patients’ cases, other factors should be taken into account. When a mandibular reconstruction plate is exposed, the underlying bone is also usually exposed as well. Our two patients have a sufficient soft tissue collar surrounding the entrance of the plate into the tissues, simulating nonattached gingiva around a conventional endosseous titanium implant. Therefore, so long as the ex-
C. Lindqvist et al.
posed part of the plate is kept clean (i.e., free of bacterial plaque), the risk of bone infection is minimized. The survival rate of endosseous titanium implants in edentulous jaws has been shown to be high as long as certain criteria are fulfilled. After osseointegration has occurred, the peri-implant soft tissue has to be kept free of inflammation through strict hygiene, and the biomechanical loading of the implant and associated superstructure must not be excessive. These guidelines can also be applied to a reconstruction of these types of maxillary defects as described earlier. This means that the prosthetic reconstruction should be designed in such a manner that adequate oral hygiene can be maintained. Additionally, unfavorable loading conditions should be avoided by placing the THORP plate in an optimal position from the prosthodontic standpoint. This requires proper presurgical, perisurgical, and postsurgical consultation between the surgeon and prosthodontist.
References
1.Konno A, Togawa K, Iizuka K. Primary reconstruction after total extended maxillectomy for maxillary cancer. Plast Reconstr Surg. 1981;67:440–447.
2.Phillips JG, Peckitt NS. Reconstruction of the palate using bilateral temporalis muscle flaps: a case report. Br J Oral Maxillofac Surg. 1988;26:322–325.
3.Hellem S, Olofsson J. Titanium-coated hollow screw and reconstruction plate system (THORP) in mandibular reconstruction.
J Craniomaxillofac Surg. 1988;17:173–176.
4.Raveh J. Lower jaw reconstruction with the THORP system for bridging of lower jaw defects. Head Neck Cancer. 1990;2:344– 349.
5.Milton CM, Yazdanie N, Bickerton RC. Prosthetic management following bilateral total or subtotal maxillectomy. J Laryngol Otol. 1986;100:1145–1154.
6.Coffey KW. Obturation of congenital or acquired intraoral anatomic defects. J Prosthet Dent. 1984;52:559–563.
7.Parel SM, Holt RG, Brånemark P-I, et al. Osseointegration and facial prosthetics. Int J Oral Maxillofac Implants. 1986;1:12–17.
8.Jacobsson M. On bone behaviour after irradiation. Thesis. University of Gothenburg, Sweden; 1985.
9.Jacobsson M, Tjellström A, Albrektsson T, et al. Integration of titanium implants in irradiated bone. Ann Otol Rhinol Laryngol. 1988;97:337–342.
