
- •Preface
- •Acknowledgments
- •Contents
- •Contributors
- •1. Introduction
- •2. Evaluation of the Craniomaxillofacial Deformity Patient
- •3. Craniofacial Deformities: Review of Etiologies, Distribution, and Their Classification
- •4. Etiology of Skeletal Malocclusion
- •5. Etiology, Distribution, and Classification of Craniomaxillofacial Deformities: Traumatic Defects
- •6. Etiology, Distribution, and Classification of Craniomaxillofacial Deformities: Review of Nasal Deformities
- •7. Review of Benign Tumors of the Maxillofacial Region and Considerations for Bone Invasion
- •8. Oral Malignancies: Etiology, Distribution, and Basic Treatment Considerations
- •9. Craniomaxillofacial Bone Infections: Etiologies, Distributions, and Associated Defects
- •11. Craniomaxillofacial Bone Healing, Biomechanics, and Rigid Internal Fixation
- •12. Metal for Craniomaxillofacial Internal Fixation Implants and Its Physiological Implications
- •13. Bioresorbable Materials for Bone Fixation: Review of Biological Concepts and Mechanical Aspects
- •14. Advanced Bone Healing Concepts in Craniomaxillofacial Reconstructive and Corrective Bone Surgery
- •15. The ITI Dental Implant System
- •16. Localized Ridge Augmentation Using Guided Bone Regeneration in Deficient Implant Sites
- •17. The ITI Dental Implant System in Maxillofacial Applications
- •18. Maxillary Sinus Grafting and Osseointegration Surgery
- •19. Computerized Tomography and Its Use for Craniomaxillofacial Dental Implantology
- •20B. Atlas of Cases
- •21A. Prosthodontic Considerations in Dental Implant Restoration
- •21B. Overdenture Case Reports
- •22. AO/ASIF Mandibular Hardware
- •23. Aesthetic Considerations in Reconstructive and Corrective Craniomaxillofacial Bone Surgery
- •24. Considerations for Reconstruction of the Head and Neck Oncologic Patient
- •25. Autogenous Bone Grafts in Maxillofacial Reconstruction
- •26. Current Practice and Future Trends in Craniomaxillofacial Reconstructive and Corrective Microvascular Bone Surgery
- •27. Considerations in the Fixation of Bone Grafts for the Reconstruction of Mandibular Continuity Defects
- •28. Indications and Technical Considerations of Different Fibula Grafts
- •29. Soft Tissue Flaps for Coverage of Craniomaxillofacial Osseous Continuity Defects with or Without Bone Graft and Rigid Fixation
- •30. Mandibular Condyle Reconstruction with Free Costochondral Grafting
- •31. Microsurgical Reconstruction of Large Defects of the Maxilla, Midface, and Cranial Base
- •32. Condylar Prosthesis for the Replacement of the Mandibular Condyle
- •33. Problems Related to Mandibular Condylar Prosthesis
- •34. Reconstruction of Defects of the Mandibular Angle
- •35. Mandibular Body Reconstruction
- •36. Marginal Mandibulectomy
- •37. Reconstruction of Extensive Anterior Defects of the Mandible
- •38. Radiation Therapy and Considerations for Internal Fixation Devices
- •39. Management of Posttraumatic Osteomyelitis of the Mandible
- •40. Bilateral Maxillary Defects: THORP Plate Reconstruction with Removable Prosthesis
- •41. AO/ASIF Craniofacial Fixation System Hardware
- •43. Orbital Reconstruction
- •44. Nasal Reconstruction Using Bone Grafts and Rigid Internal Fixation
- •46. Orthognathic Examination
- •47. Considerations in Planning for Bimaxillary Surgery and the Implications of Rigid Internal Fixation
- •48. Reconstruction of Cleft Lip and Palate Osseous Defects and Deformities
- •49. Maxillary Osteotomies and Considerations for Rigid Internal Fixation
- •50. Mandibular Osteotomies and Considerations for Rigid Internal Fixation
- •51. Genioplasty Techniques and Considerations for Rigid Internal Fixation
- •52. Long-Term Stability of Maxillary and Mandibular Osteotomies with Rigid Internal Fixation
- •53. Le Fort II and Le Fort III Osteotomies for Midface Reconstruction and Considerations for Internal Fixation
- •54. Craniofacial Deformities: Introduction and Principles of Management
- •55. The Effects of Plate and Screw Fixation on the Growing Craniofacial Skeleton
- •56. Calvarial Bone Graft Harvesting Techniques: Considerations for Their Use with Rigid Fixation Techniques in the Craniomaxillofacial Region
- •57. Crouzon Syndrome: Basic Dysmorphology and Staging of Reconstruction
- •58. Hemifacial Microsomia
- •59. Orbital Hypertelorism: Surgical Management
- •60. Surgical Correction of the Apert Craniofacial Deformities
- •Index
31
Microsurgical Reconstruction of Large Defects of the Maxilla, Midface, and Cranial Base
Rainer Schmelzeisen
Compared to reconstructive procedures in the mandible, bone and soft tissue reconstruction of the maxilla, the midface, and the cranial base often necessitates more complex surface reconstructions. In addition to functional restrictions, extensive defects in that area also lead to changes in the appearance of the patient as the zygomatic or maxillary complex provide the characteristic sagittal and transverse projection of a face.1 The surgical strategies vary, depending on size and location of the defect. In contrast to the mandible, where significant functional loading also has to be taken into consideration, the biomechanical aspects of maxillary and midface reconstructions are of minor importance. Nevertheless, the multiform morphology of the maxilla and midface contributes to important functions such as deglutition, mastication, breathing, and speech.
Localized bony defects of the maxilla that occur in patients with cleft lip and palate or severe general atrophy of the maxilla are replaced with free corticocancellous bone grafts. Fresh autogenous bone is the material of first choice for bone replacement in these patients. It has been observed that the transfer of corticocancellous bone results in extensive resorption of the grafts if an early functional load (e.g., by the insertion of dental implants) is not applied.2
In cleft lip and palate patients, small amounts of cancellous bone usually provide a sufficient volume for later implant placement. The watertight closure of nasal and oral layers is an essential condition for undisturbed healing of these grafts and maximal bone-mass retention/survival.
In patients with severe atrophy of the maxilla, transplants of unicortical horseshoe-shaped bone grafts taken from the medial aspect of the anterior ilium can be utilized. Repositioning of the laterally pedicled cranial aspect of the iliac crest significantly reduces donor-site morbidity and aesthetic restrictions in that region. Another recognized technique is to use grafts taken from the posterior aspect of the ilium, which can provide a greater quantity of bone, although the patient’s position must be changed before the harvest.3 After reflection of the maxillary mucosa, the grafts are contoured and fixed on the residual alveolar ridge with 2.0-mm positioning screws followed by a two-layer soft tissue closure. Removal of the
positioning screws and insertion of screw-type titanium implants may be performed 4 to 6 months after bone grafting, with bone scintigraphy useful in determining the optimal time for the insertion of dental implants. In posterior aspects of the maxilla, sinus-lift procedures may be considered with regard to the needs of the prosthodontist.
Reconstruction of Extensive
Maxillary/Midface Defects
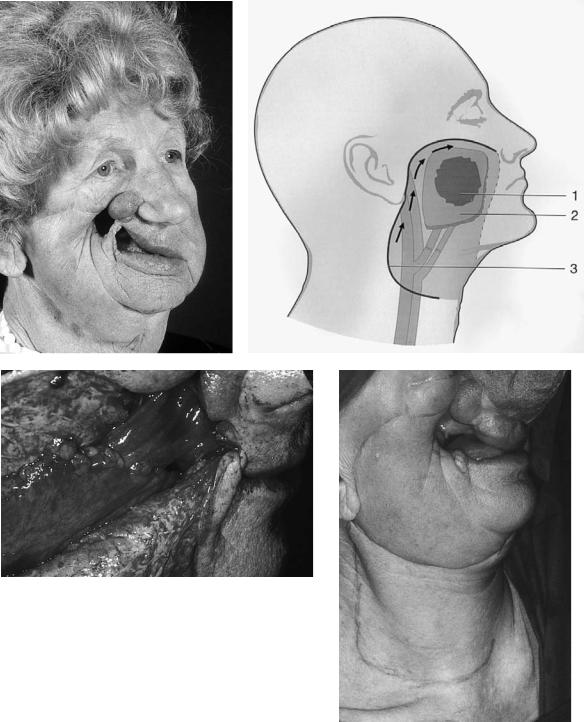
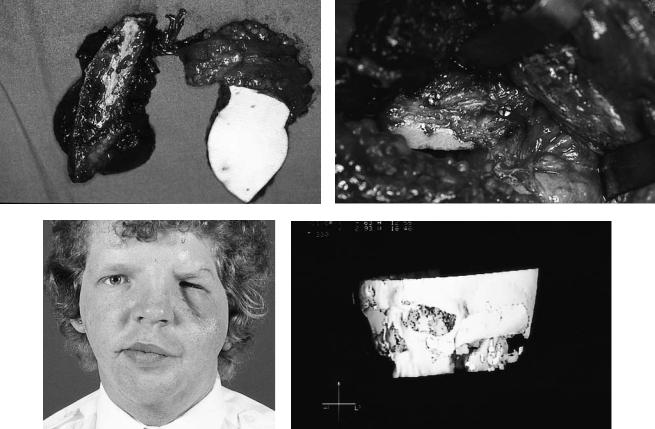
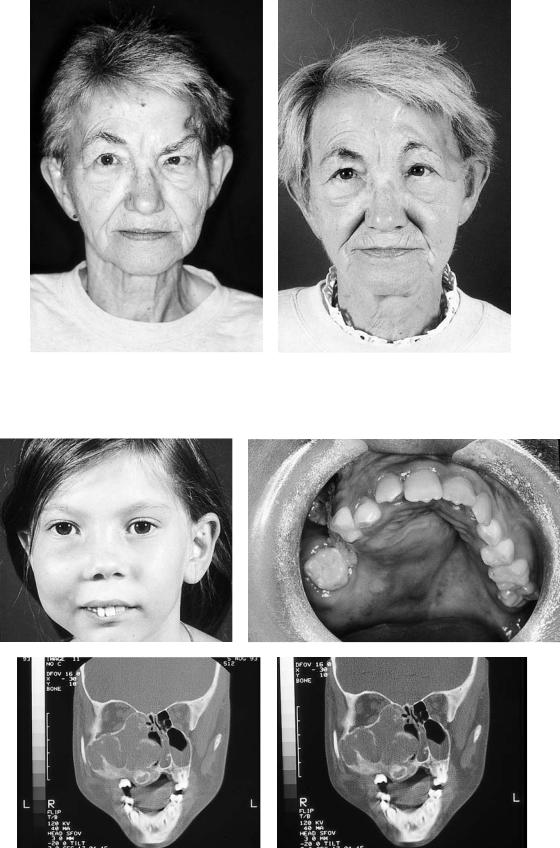
Resection of malignant tumors may cause more extensive, composite defects of the palate, cheek, and orbit, which may also include the cranial base. The possibilities for prosthodontic rehabilitation are limited and depend upon the amount of residual bone and remaining teeth. The isolated use of osseointegrated implants for solid anchoring of prosthetics also may be limited and can only be performed with regard to the residual amount and location of bone. In combined treatment protocols of malignancies, additional radiotherapy may further restrict the possibilities of conventional prosthodontic treatment (Figure 31.1).
Conventional rehabilitation usually performed with obturators may separate oral and nasal cavities effectively and permit adequate speech and deglutition. Nevertheless, the inflow of food into the nose and accumulation of debris at the surfaces of the obturator are severe disadvantages. Also, daily prosthetic care cannot be maintained by all of the patients. Large-size epithetics that also cover external surfaces may be extremely unpleasant to wear, especially in cold environments.
Up to a certain amount and in specific locations, local flaps may be used for the reconstruction of defects with a predominant soft tissue loss. Flaps from the forehead leave an extremely unfavorable donor-site scar and should be regarded as obsolete. Transposition of calvarial bone flaps, vascularized by a pedicle of the temporal muscle, allow for a combined reconstruction of soft tissue and bone defects. Nevertheless, mul- tiple-surface reconstruction or multiple-folding procedures of these local flaps are limited by the pedicle dimension and length. In these one-dimensional reconstructive procedures,
356
31. Microsurgical Reconstruction of Large Defects of the Maxilla, Midface, and Cranial Base |
357 |
||||
a |
b |
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
c |
d |
FIGURE 31.1 (a) Perforating defect of the cheek following hemimaxillectomy and a full-dose radiotherapy. (b) Schematic drawing of reconstructive principle. Intraoral reconstruction of (1) the soft tissue defect with (2) a vascularized jejunal graft. Closure of external skin defect (3) with a rotational flap from the neck. (c) Intraoral aspect of the mucosa reconstruction with a jejunal graft. Lateral view to the mesenteric surface of the graft. (d) Clinical aspect of the planned neck/cheek rotation. Continued.
the amount of bone available is limited, and it cannot be mobilized independently from the adjacent soft tissue. In addition to the possible volume deficit at the donor site, the use of these temporal flaps may be associated with injuries to the frontal branch of the facial nerve; local flaps in general increase the risk for a postoperative limited jaw opening.1,4–6
The increasing use of vascularized combined-tissue grafts has offered new possibilities for reconstruction procedures in
the maxillary/midface area. Survival of these grafts is independent of the vascularity of the surrounding tissue and generally permits multidimensional surface reconstruction of complex defects.
In addition to the possibility of a complex first-stage reconstruction, the procedures in the midface remain multiplestep rehabilitations with further minor corrections. It has to be decided, for each individual patient, the level of complexity

e
f |
|
|
|
|
|
g |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
h |
i |
FIGURE 31.1 Continued. (e) Immediate postoperative result. (f,g) Extraoral appearance of the patient 6 months following reconstruction. (h,i) Following implant insertion in the residual zygomatic complex
and the contralateral maxilla, an implant-borne obturator prosthesis was inserted.
31. Microsurgical Reconstruction of Large Defects of the Maxilla, Midface, and Cranial Base |
359 |
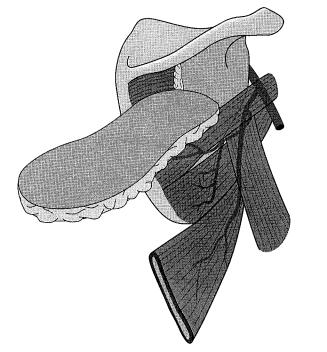
FIGURE 31.2 Schematic drawing of the scapula region. The parascapula skin flap can be raised together with the lateral border of the scapula. Pedicled to the circumflex scapular vessels, the skin flap can be mobilized relatively independent from the bone graft. Additionally, a scapula flap nourished by the transverse cutaneous branch can be harvested as a second soft tissue pedicle.
to which the primary reconstruction can be performed, especially with regard to an optimal function and safe outcome.
The thin bone of the scapula is ideal for reconstruction of the hard palate or the orbital floor.
It must be decided in the individual case whether deepithelialization of a parascapular flap is sufficient for surface contouring or whether a bipedicled scapula and parascapular flap is used for the reconstruction of surfaces or volume augmentation in separate locations (Figures 31.4, 31.5).
In maxillary reconstruction, the thicker lateral margin of the scapula, which is suitable for implant insertion, cannot always be positioned in an anatomically correct position for the alveolar process owing to the shortness of the vascular pedicle. This often requires secondary nonvascularized bone grafts as additional augmentation with screw-type implant stabilization into the vascularized scapula bone flap (Figure 31.6).
The fixation of the scapula bone generally is of minor importance. One 2.0-mm plate may be sufficient for fixation of the scapula bone to the residual maxilla or zygoma. It is of crucial importance to provide a good bony contact area between the scapula bone and the residual midfacial skeleton. Therefore, additional free-bone grafts may be inserted in bony discrepancies to provide adequate stability of the graft. Lagscrew techniques may be used if vascularized aspects of the combined scapula grafts are used for onlay grafting [e.g., in the zygomatic region; see Figure 31.4(d,e)].
For vascular anastomosis, the superficial temporal vessels are not always reliable. Therefore, a submandibular incision is chosen. The marginal branch of the facial nerve is identified and elevated. On the surface of the masseter muscle, a tunnel can be dissected toward the maxilla.
This tunnel must be of an adequate diameter not to compress the pedicle vein. No tension must be applied to the anastomosis. The preparation of the tunnel is of crucial importance for the success of the graft, as complications may be due to compression in that tunnel.
Scapula Grafts
Grafts from the scapula region are most versatile for maxillary/midface reconstructions when both soft tissue and bone defects have to be reconstructed. The grafts offer the advantage of a vascularized thin bone area, which can be combined with one or two soft tissue components, either of which individually or together may be completely or partially deepithelialized (Figure 31.2).6–9
The flap designs permit for the reconstruction of complex bony and soft tissue defects with different surfaces to be reconstructed (e.g., palatal mucosa and separation between nasal cavity and maxillary sinus).
Deepithelialized portions may be used for volume augmentation in the midface and offer acceptable volume stability over time as atrophy is unlikely to occur in contrast to muscle flaps.10 This lower tendency for resorption of the grafts makes combined scapula grafts useful in patients with hemifacial microsomia. In these patients, soft tissue augmentation may be combined with repositioning, reconstruction, or augmentation of the midfacial skeleton (Figure 31.3).
Isolated Soft Tissue Grafts
In defects with predominant soft tissue loss, reconstruction may also be performed with musculocutaneous or fasciocutaneous isolated soft tissue grafts. In general, the vascular pedicle of these flaps is longer than in combined bone and soft tissue flaps like scapula, iliac crest, or fibula grafts.
The thin radial forearm flap may be especially useful for closure of maxillary defects with a predominant soft tissue component. For these indications, it may serve as an alternative for jejunal grafts. The minimal flap thickness also makes the flap suitable for reconstruction of combined soft tissue or bone defects of the maxilla when the bone defect is of limited size, and a nonvascularized bone graft can be fixed with a circular good contact to the surrounding bone. The free-bone graft then may be covered with a radial forearm flap, and functional separation between nasal and oral cavity also can be performed by the flap. The length of the vascular pedicle of the radial forearm flap allows for reconstruction of cranially located skin areas (e.g., at the cranial base and the forehead; Figure 31.7).
a |
|
|
|
|
|
b |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
c |
|
|
|
d |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
e |
|
f |
|
|
|
|
|
|
FIGURE 31.3

31. Microsurgical Reconstruction of Large Defects of the Maxilla, Midface, and Cranial Base |
361 |
g |
h |
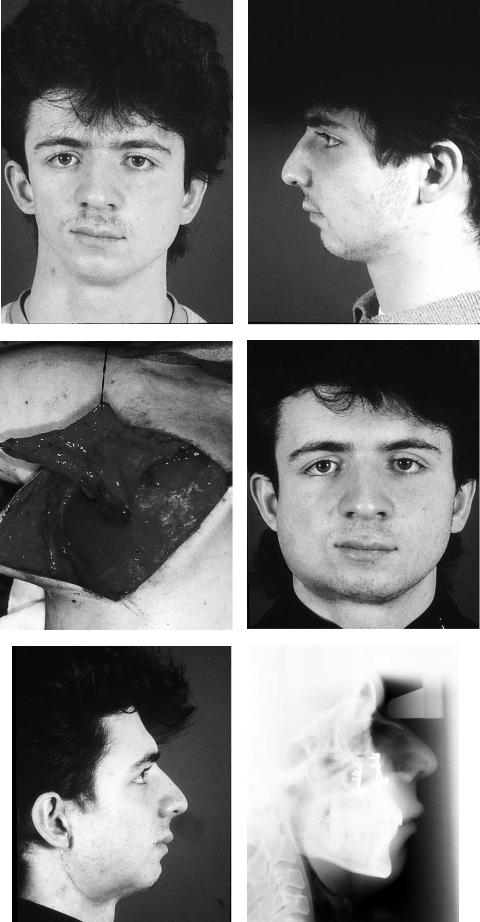
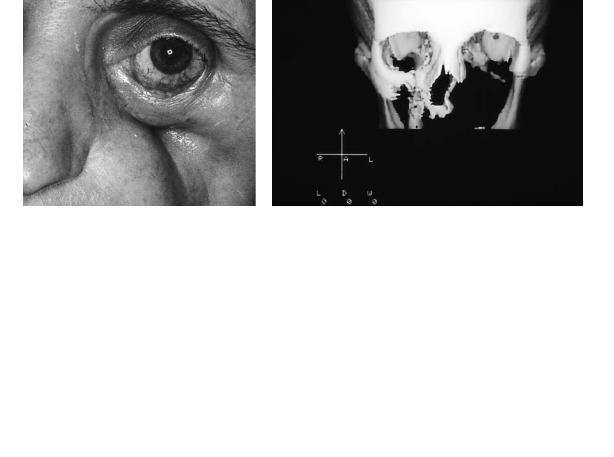
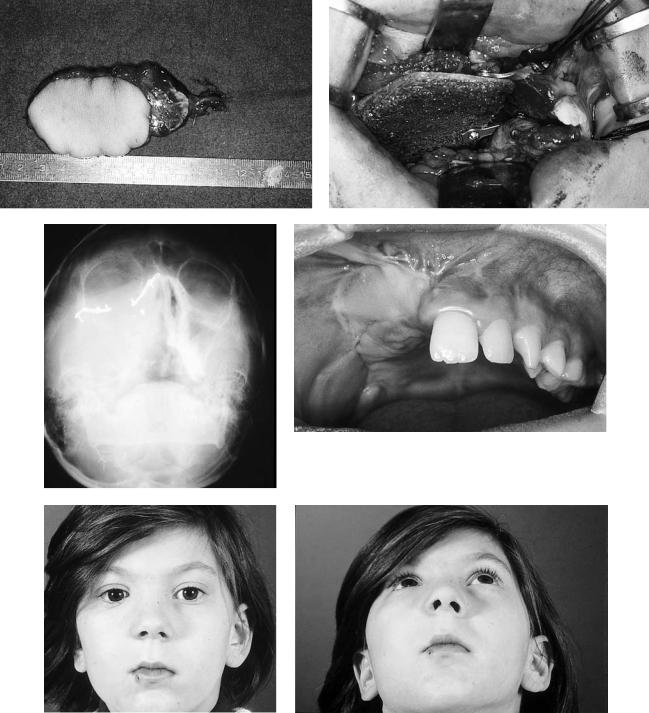
FIGURE 31.3 (a) Patient with hemifacial microsomia and asymmetry of the maxillary/mandibular complex. Additional significant soft tissue deficit in projection to the right cheek and maxillary/zygomatic region. (b) Profile analysis demonstrates an additional sagittal deficit of the mandibular projection. (c) After bimaxillary osteotomies for
If more soft tissue volume is needed, a latissimus dorsi or rectus abdominis flap may be used. The multiple skin perforators of the latissimus dorsi flap allow for the preparation of several skin paddles for reconstruction of nasal cavity, external skin, palate, or orbit. The muscle volume restores facial contour. Obliteration of the maxillary sinus may be performed with the muscle volume. The length of the vascular pedicle offers various options for the location of the vessel anastomosis.
While the rectus abdominis and latissimus dorsi musculocutaneous flaps are very similar regarding tissue volume, pedicle length, and reliability, harvesting of the rectus abdominis flap offers the advantage of an unchanged patient position.
The disadvantage of these large-volume flaps in the maxilla and midface may be an inferior dislocation of the oral flap surface, which can disturb speech and swallowing function. In general, all vascularized soft tissue flaps used for intraoral surface reconstruction of the maxilla have to be thinned out postoperatively.
Isolated soft tissue grafts may not be suitable for reconstruction of orbital floor defects as they do not provide stable support for the eye.11–13 Therefore, additional nonvascularized bone grafts (i.e., from the calvarium or iliac crest) may be used for reconstruction of the orbit and the midface.
In children, harvesting vascularized bone grafts may interfere with growth capacity at the donor site. Therefore, vascularized soft tissue reconstruction with free-bone grafting, for example, with split grafts from the ilium, may be primarily considered (Figure 31.8).
correction of the skeletal asymmetry and occlusion, a deepithelialized parascapular flap is harvested for soft tissue augmentation. (d,e) Postoperative aspect of the patient. (f) Postoperative x-ray. (g,h) Postoperative occlusion.
Reconstruction of Periorbital/Cranial
Base Defects
Whenever possible, localized combined bone and soft tissue defects in the orbital region should be surgically treated with local flaps. Although vascularized grafts offer ideal options for volume augmentation and bony support in the maxillary and midface areas, unsatisfactory aesthetic results often result when external skin areas need to be replaced with flaps from distant sites.
For smaller defects of the orbital frame, including limited external skin replacement, rotational flaps from the scalp may be used for the coverage of alloplastic materials or calvarial split grafts (Figure 31.9).
When complex soft tissue or bone defects are encountered (i.e., trauma or growth inhibition), osteotomies or orbitotomies combined with the use of autologous bone grafts should initially be considered. Tissue expanders are often useful for soft tissue reconstruction in these patients.
Large defects of the orbit and anterior skull base may necessitate again the use of microsurgically vascularized grafts, which allow for the safe coverage of the skull base and duraplasties. Musculocutaneous grafts, such as the rectus abdominis or latissimus dorsi, are used. The consistent vascular anatomy and the length of the vascular pedicle allow for vascular anastomosis with submandibular vessels.
In extensive combined periorbital defects permitting
362 |
|
|
|
R. Schmelzeisen |
a |
|
|
|
b |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
c
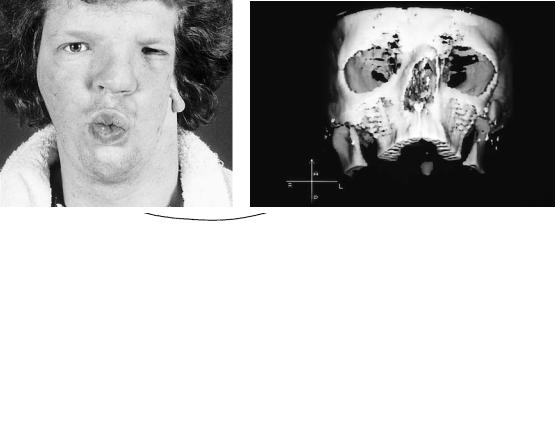
FIGURE 31.4 (a) Preoperative aspect of a 28-year-old patient with hemifacial microsomia. (b) Three-dimensional CT demonstrates hypoplasia of left maxilla, zygoma, and absence of zygomatic arch. (c) Schematic drawing of intended reconstruction.
31. Microsurgical Reconstruction of Large Defects of the Maxilla, Midface, and Cranial Base |
363 |
d |
e |
f |
|
|
|
g |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
FIGURE 31.4 Continued. (d) Harvesting of an osteocutaneous parascapular flap which was deepithelialized. (e) Lag-screw fixation of the lateral border of the scapula for reshaping the zygomatic arch and the infraorbital region by means of vascularized onlay grafting.
(f) Postoperative aspect of the patient with adequate transverse projection of the zygomatic complex. Orbital reconstruction and insertion of an orbital prosthesis still to be performed. (g) Postoperative CT scan demonstrates the amount of bony augmentation.
364 |
|
R. Schmelzeisen |
a |
|
b |
|
|
|
|
|
|
c
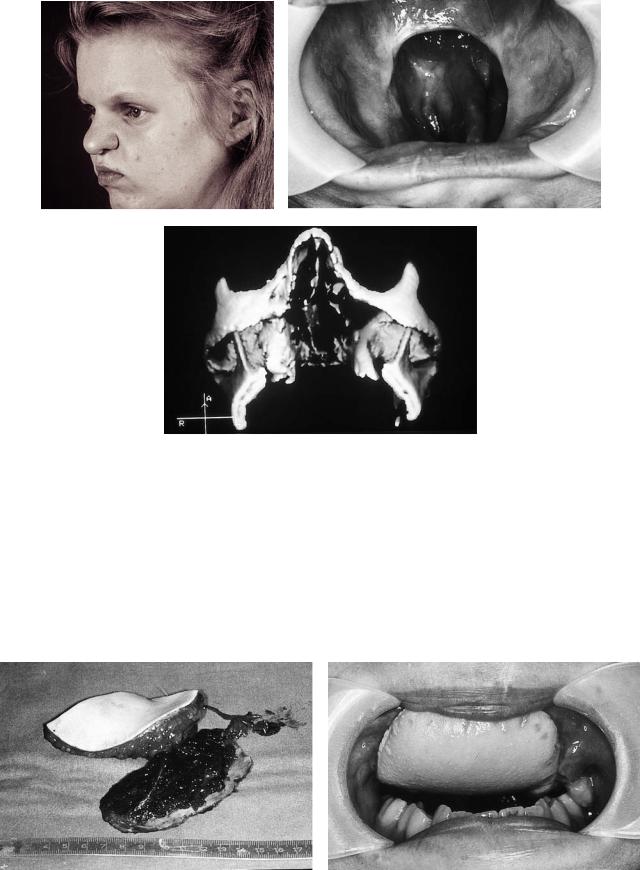
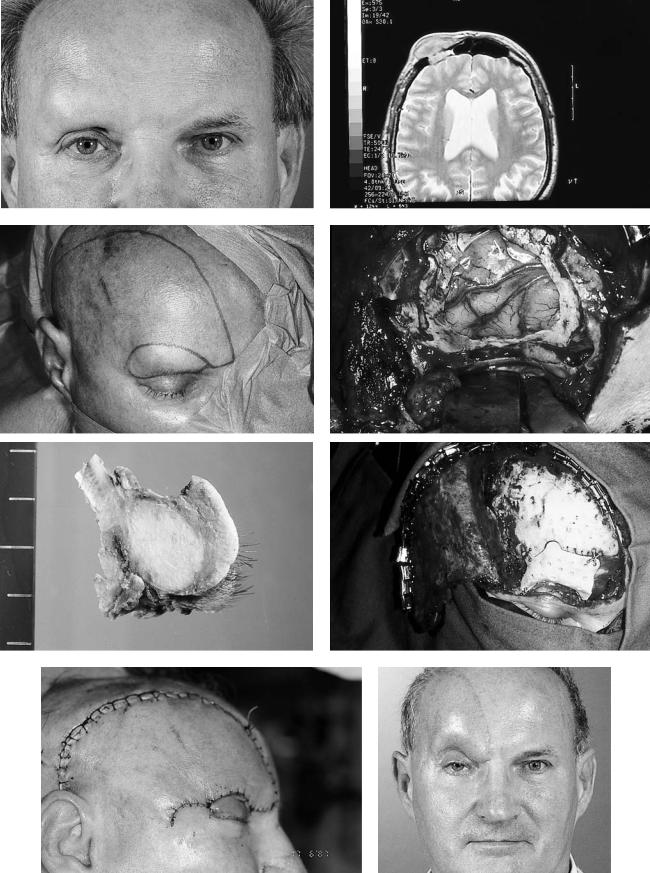
FIGURE 31.5 (a,b) Soft tissue defect following right hemimaxillectomy and resection of the orbital floor in a 50-year-old patient. (b) Postoperative 3-D CT scan demonstrating bony defect. (c) Schematic drawing of reconstructive procedure. (d) Surgical approach to the defect by reopening the preexisting Dieffenbach-Weber incision. (e) Reconstruction of the orbital floor by the thin medial aspect of a scapula graft. Bilateral fixation of the scapula bone by microplates.
(f) Partial deepithelialization of the parascapular flap. The deepithelialized part is used for cheek augmentation, and the cutaneous
preservation of the eyelids, the vascularized soft tissue graft may provide an adequate aesthetic result. Following large tumor resections, the aesthetic result is often compromised since it is necessary to primarily provide satisfactory coverage of the skull base and a clean skin surface (Figure 31.10).
Also in lateral and posterior skull defects, musculocutaneous flaps may also provide satisfactory coverage of the brain or duraplasties. For primary tumor resection, the skull bone often does not have to be reconstructed.
Radiation therapy should not be considered as a contraindication for the use of vascularized grafts for craniofacial reconstruction.14,15
aspect is inserted for oral lining of the maxillary mucosa. The vicinity of the region to be augmented and the area of missing maxillary mucosa allows for harvesting of only one parascapular flap serving both purposes. The necessity to reconstruct separate soft tissue locations would require the preparation of a scapula and a parascapular soft tissue flap. (g) Postoperative aspect of the patient 8 weeks following surgery. Quality of overlying skin often improves with time.
Summary
For complex defects in the maxilla and midface, scapula grafts have to be regarded as reconstruction methods of choice. The vascular anatomy of the scapula region allows for the reconstruction of multiple surface defects, and the thin scapula is ideally suited for reconstruction of the palate and alveolar process.
The thick bone volume of the iliac crest offers better bone volume for the insertion of dental implants. Nevertheless, adequate shaping of the iliac crest for maxillary reconstruction is more difficult, and the soft tissue pedicle cannot be mobi-

31. Microsurgical Reconstruction of Large Defects of the Maxilla, Midface, and Cranial Base |
365 |
d |
e |
f |
|
|
|
g |
|
|
|
|
|
|
|
|
|
|
FIGURE 31.5 Continued.
lized independently from the bone. The skin paddle is often extremely bulky and is not suitable for reconstruction of multiple surfaces.16
Isolated soft tissue grafts are not suitable for orbital support and may undergo gravitational ptosis. However, they may be taken into consideration if maximum safety of a procedure is necessary due to a longer vascular pedicle and a reliable vascular anatomy.
With regard to the maximum safety of reconstruction and possible growth disturbances at the donor site, vascularized soft tissue grafts with secondary bone grafts may be primarily used for reconstructive procedures in children. To our knowledge, the earliest microvascular procedure in the maxilla/midface has been performed by Posnick in a 1-year-old
child with a parameningeal head and neck rhabdomyosarcoma. In that young patient, a radial forearm flap was harvested to reconstruct the skin and the soft tissue defect of the cheek with supply for the lining of the nasal cavity. The flap was anastomosed to the superficial temporal vessels and combined with a split calvarial graft.17
The selection of reconstructive methods in the maxilla, midface, and cranial base should be highly individualized. The complexity of reconstruction should be performed with regard to the prognosis of the underlying disease and the expectations of the patient. In general, the increasing use of vascularized grafts from different donor sites has enlarged the reconstructive possibilities in the craniomaxillofacial area, and they are far superior to conventional reconstructive procedures.
a |
|
b |
||
|
|
|
|
|
|
|
|
|
|
c
d
e |
f |
FIGURE 31.6
31. Microsurgical Reconstruction of Large Defects of the Maxilla, Midface, and Cranial Base |
367 |
g |
h |
i |
j |
k
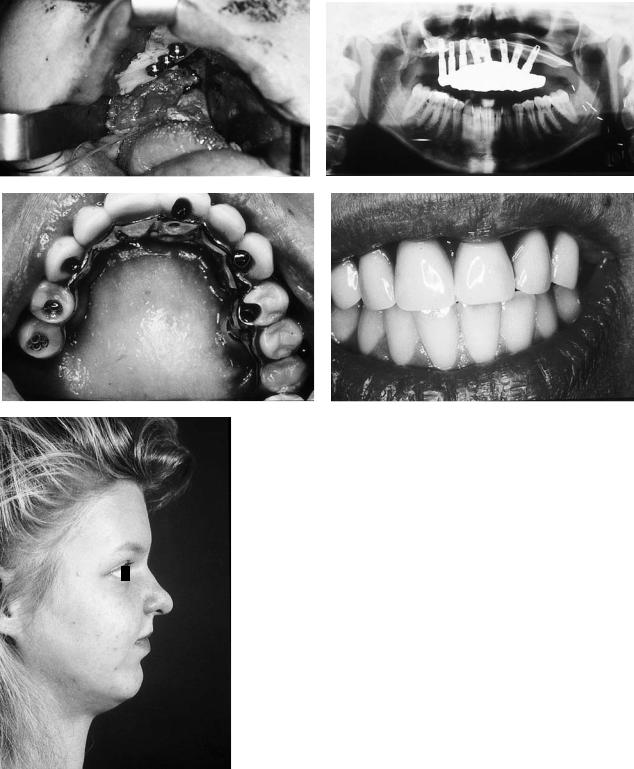
FIGURE 31.6 Continued. (a) Fifteen-year-old patient following complete maxillectomy due to a sarcoma of the maxilla at the age of 1 year. Significant soft tissue deficit with inadequate profile of the upper lip. (b) Intraoral aspect with oronasal perforation. (c) Preoperative three-dimensional CT-scan demonstrates amount of bone missing. (d) Parts 1 and 2: Schematic drawing of reconstructive strategy with primary insertion of the osteocutaneous parascapular flap. Secondarily, additional free-bone grafts were fixed to the scapula bone with dental implants acting as positioning screws. (e) Harvested osteocutaneous parascapular flap. (f) Osteocutaneous parascapular flap inserted intraorally, with immediate postoperative significant soft tissue excess. (g) Fixation of additional free bone grafts to the scapula bone with dental implants. Simultaneous volume reduction of the soft tissue flap. (h) Postoperative panoramic radiograph of prosthesis. (i,j) Intraoral views of prosthodontic rehabilitation by means of implant-borne dentures. (k) Postoperative aspect of the patient with adequate upper-lip profile.
368 |
|
|
|
|
|
|
|
R. Schmelzeisen |
a |
|
|
|
|
|
|
|
b |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
FIGURE 31.7 (a) Patient with basalioma of the left frontal skin. Biopsies proved extensions of the basalioma close to the midline of the forehead without bony invasion. (b) Excision of left forehead skin
and coverage of the defect with a radial forearm flap. The length of the pedicle allows for tensionless microvascular anastomosis to the submandibular vessels.
a |
|
|
|
b |
|
|
|
|
|
|
|
|
|
|
c |
d |
FIGURE 31.8
31. Microsurgical Reconstruction of Large Defects of the Maxilla, Midface, and Cranial Base |
369 |
e |
f |
g |
h |
i |
|
|
|
|
|
|
|
j |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
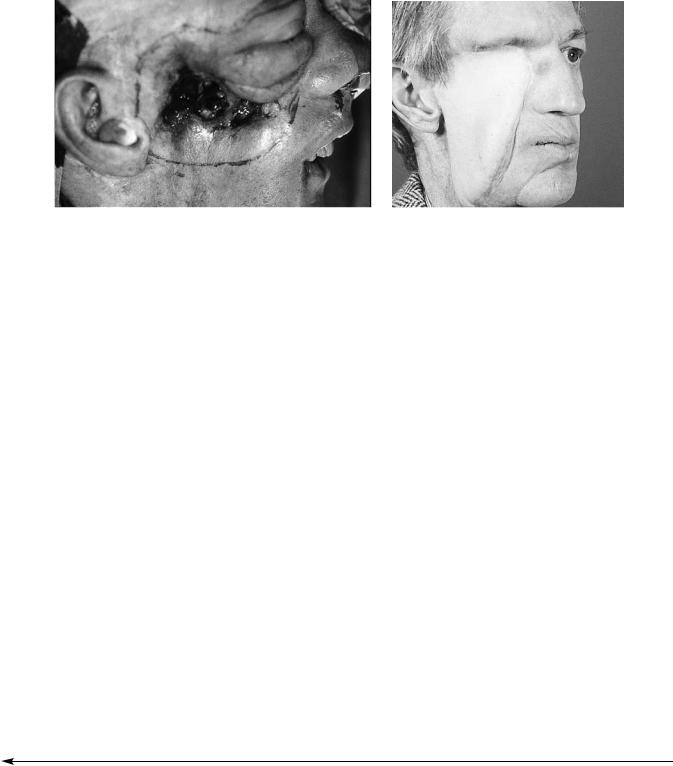
FIGURE 31.8 Continued. (a–d) Twelve-year-old girl with large ossifying fibroma of the right maxilla invading the orbit and the ethmoid cells. (e) After resection of the fibroma, a latissimus dorsi muscle flap was harvested to avoid growth disturbances at the donor site of possible combined bone and soft tissue grafts. The latissimus dorsi flap was used for coverage of the skull base, obliteration of the maxillary sinus, and lining of the nasal and oral mucosa. (f) After re-
construction of the orbital floor, the palate additionally was reconstructed using a monocortical nonvascularized bone graft from the iliac crest. Miniplate fixation of the two bone grafts. (g) Postoperative x-ray. (h) Intraoral aspect demonstrating isolated skin area of latissimus dorsi flap used for oral lining. (i,j) Postoperative aspect of the patient.
370 |
|
|
|
R. Schmelzeisen |
a |
|
|
|
b |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
c |
d |
e |
f |
g |
|
|
|
h |
|
|
|
|
|
|
|
|
|
|
FIGURE 31.9
31. Microsurgical Reconstruction of Large Defects of the Maxilla, Midface, and Cranial Base |
371 |
|
a |
|
b |
|
|
|
|
|
|
FIGURE 31.10 (a) Amount of palliative resection in a 55-year-old patient with multiple previous operations of recurrent carcinoma of the maxilla. Infiltration of the orbit and the anterior skull base. (b) Fol-
References
1.Coleman JJ. Microvascular approach to function and appearance of large orbital maxillary defects. Am J Surg. 1989;158:337–341.
2.Davis HW, Marshall MW. Effects of osseointegrated implantsupported prosthesis on bone preservation and regeneration in the edentulous mandible. In: Davis WM, Sailer H, eds. Oral and Maxillofacial Surgery Clinics of North America; 1994:765–779.
3.Marx RE. Morbidity from bone harvest in major jaw reconstruction: a randomized trial comparing the lateral anterior and posterior approaches to the ilium. J Oral Maxillofac Surg. 1988; 48:196–203.
4.Shapiro BM, Komisar A, Silver C, et al. Primary reconstruction of palatal defects. Otolaryngol Head Neck Surg. 1986;95:581– 585.
5.Colmenero C, Martorell B, Colmenero B, et al. Temporalis myofacial flap for maxillofacial reconstruction. J Oral Maxillofac Surg. 1991;49:1067–1073.
6.Kärcher H, Eskici A, Zwittnig P. Oberkieferrekonstruktion mit dem osteokutanen Skapulatransplantat nach Schußverletzung. Z Stomatol. 1988;85:371–377.
7.dos Santos LF. Le Lambeau Scapulaire et L’Artere Cutanee Scapulaire. Paris, 1980.
8.Nassif T, Vidal L, Bovet J, et al. The parascapular flap: a new cutaneous microsurgical free flap. Plast Reconstr Surg. 1982;69: 591–600.
9.Pistner H, Reuther J, Bill J. Skapularegion als potentielles Spenderareal für mikrochirurgische Transplantate. In: Schwenzer
lowing palliatively intended resection, the skull base and orbit were covered with a latissimus dorsi flap.
N, Pfeifer G, eds. Fortschritte der Kieferund Gesichtschirurgie,
Vol. 35. Stuttgart: Thieme; 1990:87–90.
10.Riediger D. Mikrochirurgische Weichgewebetransplantation in die Gesichtsregion. Munich: Hanser; 1983.
11.Hoffman HT, Jalowaysky AA, Robbins KT, et al. Oronasal reconstruction with local mucoperiosteal and free latissimus dorsi flaps. Arch Otolaryngol. 1992;118:1238–1241.
12.Peters GE, Grotting JC. Free flap reconstruction of large head and neck defects in the elderly. Microsurgery. 1989;10:325–328.
13.Meyer H, Schmidt JW, Terrahe K, et al. Modifikation des mikrovaskulär reanastomosierten Latissimus dorsi Lappens zur Rekonstruktion nach erweiterter Oberkieferresektion. HNO. 1991;39:218–223.
14.Fisher J, Jackson IT. Microvascular surgery as an adjunct to craniomaxillofacial reconstruction. Br J Plast Surg. 1989;42: 146–154.
15.Robson MC, Zachary LS, Schmidt DG, Faibisoff B, Hekmatpanah J. Reconstruction of large cranial defects in the presence of heavy radiation damage and infection utilizing tissue transferred by microvascular anastomoses. Plast Reconstr Surg. 1989;83(3):438–442.
16.Swartz WM, Banis JC, Newton ED, Ramasastry SS, Jones NF, Acland R. The osteocutaneous scapular flap for mandibular and maxillary reconstruction. Plast Reconstr Surg. 1986;77(4):530–545.
17.Posnick JC, Polley JW, Zuker RM, Chan HSL. Chemotherapy and surgical resection combined with immediate reconstruction in a 1-year-old child with rhabdomyosarcoma of the maxilla. Plast Reconstr Surg. 1992;89(2):320–325.
FIGURE 31.9 (a,b) Patient with adenocarcinoma of the right lacrimal gland with intracranial extension. (c) Planned incision for tumor resection including the overlying skin and eyebrow and closure of the defect with a scalp rotation flap. (d) Extension of the tumor necessitated additional resection of the dura. Duraplasty was performed using a fascia lata graft. (Courtesy of Prof. W Sollmann, MD, Neurosurgery, Braunschweig City Hospital) (e) Tumor specimen demon-
strates resection of frontal bone, anterior aspect of orbital roof, and overlying skin. (Courtesy of H Maschek, MD, Institute of Pathology, Medical University of Hannover, Germany) (f) After duraplasty and coverage of the frontal sinus by a galleoperiosteal flap, hard tissue reconstruction was performed with acrylic. (g) Immediate postoperative result. (h) Result 6 months postoperatively.
