
- •Preface
- •Acknowledgments
- •Contents
- •Contributors
- •1. Introduction
- •2. Evaluation of the Craniomaxillofacial Deformity Patient
- •3. Craniofacial Deformities: Review of Etiologies, Distribution, and Their Classification
- •4. Etiology of Skeletal Malocclusion
- •5. Etiology, Distribution, and Classification of Craniomaxillofacial Deformities: Traumatic Defects
- •6. Etiology, Distribution, and Classification of Craniomaxillofacial Deformities: Review of Nasal Deformities
- •7. Review of Benign Tumors of the Maxillofacial Region and Considerations for Bone Invasion
- •8. Oral Malignancies: Etiology, Distribution, and Basic Treatment Considerations
- •9. Craniomaxillofacial Bone Infections: Etiologies, Distributions, and Associated Defects
- •11. Craniomaxillofacial Bone Healing, Biomechanics, and Rigid Internal Fixation
- •12. Metal for Craniomaxillofacial Internal Fixation Implants and Its Physiological Implications
- •13. Bioresorbable Materials for Bone Fixation: Review of Biological Concepts and Mechanical Aspects
- •14. Advanced Bone Healing Concepts in Craniomaxillofacial Reconstructive and Corrective Bone Surgery
- •15. The ITI Dental Implant System
- •16. Localized Ridge Augmentation Using Guided Bone Regeneration in Deficient Implant Sites
- •17. The ITI Dental Implant System in Maxillofacial Applications
- •18. Maxillary Sinus Grafting and Osseointegration Surgery
- •19. Computerized Tomography and Its Use for Craniomaxillofacial Dental Implantology
- •20B. Atlas of Cases
- •21A. Prosthodontic Considerations in Dental Implant Restoration
- •21B. Overdenture Case Reports
- •22. AO/ASIF Mandibular Hardware
- •23. Aesthetic Considerations in Reconstructive and Corrective Craniomaxillofacial Bone Surgery
- •24. Considerations for Reconstruction of the Head and Neck Oncologic Patient
- •25. Autogenous Bone Grafts in Maxillofacial Reconstruction
- •26. Current Practice and Future Trends in Craniomaxillofacial Reconstructive and Corrective Microvascular Bone Surgery
- •27. Considerations in the Fixation of Bone Grafts for the Reconstruction of Mandibular Continuity Defects
- •28. Indications and Technical Considerations of Different Fibula Grafts
- •29. Soft Tissue Flaps for Coverage of Craniomaxillofacial Osseous Continuity Defects with or Without Bone Graft and Rigid Fixation
- •30. Mandibular Condyle Reconstruction with Free Costochondral Grafting
- •31. Microsurgical Reconstruction of Large Defects of the Maxilla, Midface, and Cranial Base
- •32. Condylar Prosthesis for the Replacement of the Mandibular Condyle
- •33. Problems Related to Mandibular Condylar Prosthesis
- •34. Reconstruction of Defects of the Mandibular Angle
- •35. Mandibular Body Reconstruction
- •36. Marginal Mandibulectomy
- •37. Reconstruction of Extensive Anterior Defects of the Mandible
- •38. Radiation Therapy and Considerations for Internal Fixation Devices
- •39. Management of Posttraumatic Osteomyelitis of the Mandible
- •40. Bilateral Maxillary Defects: THORP Plate Reconstruction with Removable Prosthesis
- •41. AO/ASIF Craniofacial Fixation System Hardware
- •43. Orbital Reconstruction
- •44. Nasal Reconstruction Using Bone Grafts and Rigid Internal Fixation
- •46. Orthognathic Examination
- •47. Considerations in Planning for Bimaxillary Surgery and the Implications of Rigid Internal Fixation
- •48. Reconstruction of Cleft Lip and Palate Osseous Defects and Deformities
- •49. Maxillary Osteotomies and Considerations for Rigid Internal Fixation
- •50. Mandibular Osteotomies and Considerations for Rigid Internal Fixation
- •51. Genioplasty Techniques and Considerations for Rigid Internal Fixation
- •52. Long-Term Stability of Maxillary and Mandibular Osteotomies with Rigid Internal Fixation
- •53. Le Fort II and Le Fort III Osteotomies for Midface Reconstruction and Considerations for Internal Fixation
- •54. Craniofacial Deformities: Introduction and Principles of Management
- •55. The Effects of Plate and Screw Fixation on the Growing Craniofacial Skeleton
- •56. Calvarial Bone Graft Harvesting Techniques: Considerations for Their Use with Rigid Fixation Techniques in the Craniomaxillofacial Region
- •57. Crouzon Syndrome: Basic Dysmorphology and Staging of Reconstruction
- •58. Hemifacial Microsomia
- •59. Orbital Hypertelorism: Surgical Management
- •60. Surgical Correction of the Apert Craniofacial Deformities
- •Index
7
Review of Benign Tumors of the Maxillofacial Region and Considerations for Bone Invasion
Joachim Prein
Tumors in the maxillofacial region are located in the soft and hard tissues. Those located in the facial skeleton are rare and can be of dental origin (odontogenic) or arise from bony tissues (osteogenic). No matter whether they are benign or malignant, clinically they often are symptomless for a long time. Only rarely do they cause pain. Even on x-ray films their appearance is very uniform. Most of them present as monoor polycystic lesions. Even the distinction of whether these lesions are well delineated or not does not help to determine whether a tumor is benign or malignant.1
Although examinations with computed tomography (CT) or magnetic resonance imaging (MRI) give much more precise information about the contents and delineation of these lesions, in most of the cases it is not possible to establish a diagnosis. This can only be done through a biopsy and a histologic examination. These biopsies should always be open biopsies to receive sufficient material in quantity and quality. This is important because many benign or malignant tumors can present with histologically similar pictures.
This is true for odontogenic tumors (e.g., for the ameloblastoma and its variants, such as ameloblastic fibroma or ameloblastic fibroodontoma). Also, it may be difficult to differentiate between fibrous dysplasia and ossifying fibroma, osteoblastoma and osteosarcoma, or desmoplastic fibroma and fibrosarcoma.
A very close cooperation between the clinician, pathologist, and radiologist is mandatory to receive an exact diagnosis. The pathologist needs all clinical and radiologic information because tumors that are histologically similar may have different diagnoses according to their different anatomic locations. A correct treatment plan can, of course, only be established with a precise preoperative diagnosis.
Odontogenic Tumors and
Tumorlike Lesions
Tumors and tumorlike lesions of dental origin are less common than those of osseous origin. Most reflect a state out of the development of a tooth. Because epithelial and mes-
enchymal tissues are involved in the formation of tooth bud, both components can be involved in the formation of an odontogenic tumor. Most odontogenic tumors are benign, and some are not even tumors, but rather tumorlike lesions or hamartomas, such as all odontomas. Therefore, most are clinically as well as radiologically and histologically well delineated and can be treated with curettage, enucleation, or sometimes fenestration. Their radiologic appearance is very uniform and often resembles a follicular cyst (Figure 7.1).
An infiltrative pattern of growth into the bony structures has histologically only been observed with ameloblastomas (Figure 7.2) and ameloblastic fibrosarcomas.
Because of size and location of some benign lesions, such as keratocysts, myxomas, or adenomatoid odontogenic tumors, it may be necessary to perform a complete resection of the involved bony area and a reconstruction thereafter. Characteristic of keratocysts is their high rate of recurrence (between 32% and 63%). In some instances, it has been reported that intraosseous carcinomas have developed out of keratocysts.
Table 7.1 mentions odontogenic lesions that necessitate a curettage or enucleation only, and according to size and location, a defect filling with cancelleous bone (Figures 7.3 and 7.4).
The ameloblastoma is a locally aggressive tumor that necessitates a complete resection with clear margins. Neither radiologic characteristics, such as monoor polycystic appearances, nor resorption of tooth roots, nor the different histologic subgroups allow a differentiation between more or less aggressive tumors. Until a few years ago, resorption of tooth roots has been interpreted as pathognomonic for ameloblastomas. Meanwhile, this phenomenon has been observed in connection with several odontogenic and nonodontogenic tumors and tumorlike lesions. It was found, however, that it does not indicate a higher aggressivness of the lesion. Table 7.2 shows a list of lesions in which radiologically resorptions of tooth roots have been observed.
Although in rare instances true malignant ameloblastomas with lymph node or skeletal metastases have been described, a neck dissection together with the resection of the tumor is
59

60 |
J. Prein |
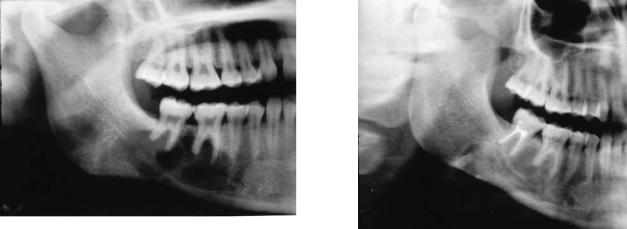
FIGURE 7.1 Cystic lesion in the left mandibular angle region with a retained molar. The x-ray appears similar to a follicular cyst. Within the cyst wall, an ameloblastoma was found.
FIGURE 7.2 Epithelial islets pathognomonic for an ameloblastoma are found to infiltrate the bony structures.
TABLE 7.1 Benign odontogenic tumors and tumorlike lesions.
Adenomatoid odontogenic tumor
Ameloblastic fibroma and myxoma
Odontogenic myxoma and fibroma
Dentinoma
Cementoma
Cementifying fibroma
Odontoma
Calcifying epithelial odontogenic tumor
Calcifying odontogenic cyst
Odontogenic keratocyst
Follicular and radicular cysts

7. Benign Tumors of the Maxillofacial Region
FIGURE 7.3 Extensive polycystic lesion in the left ramus and mandibular angle area in an 18-year-old man. The swelling was painless and the patient did not complain about loss of sensitivity in his left lower lip. Diagnosis: odontogenic keratocyst.
not indicated. As far as clinical behavior is concerned, the ameloblastoma can be compared with a basalioma. Infrequently, ameloblastic fibrosarcomas or ameloblastic odontosarcomas are observed. Regional metastasis have not been described with these.2–4
61
Histomorphologically, several types of ameloblastomas are described. The attempt to assign different grading ranks to the various types has not proven to be clinically sound. Particularly in connection with the description of malignant ameloblastomas, the acanthous type ameloblastoma has been misinterpreted as squamous cell carcinoma or adenoid cystic carcinoma or adenocarcinoma.
Ameloblastomas are predominantly located in the mandible and rarely appear before the age of 18. This is an important criterion because it helps in some instances to differentiate between ameloblastoma and lesions such as ameloblastic fibromas and myxomas.
In most instances, after complete resection of the tumor with the bone, a primary reconstruction with a reconstruction plate and a free bone graft is performed. Only rarely and depending on size and location of the defect is a primary reconstruction with a microvascular graft indicated. The most important precondition for a successful primary reconstruction is a reliable stabilization with plates and screws together with a reliable closure of the soft tissues around the grafts. The following case clearly demonstrates this.
A 41-year-old patient presented with a symptomless moderate swelling of his left mandibular angle area. On x-ray, a polycystic lesion was found and, after an open biopsy, it was diagnosed as an ameloblastoma.
After resection of the tumor through a partial mandibulectomy the defect was bridged with a 2.7 reconstruction plate. A bone graft was taken from the iliac crest and the bony defect immediately reconstructed.
Two years after the removal of the tumor the plate was removed on the patient’s request. As a rule we do not remove these plates because they are not responsible for any resorption of the bone graft through stress protection. At the occasion of the plate removal, dental implants were inserted into the bone graft (Figures 7.5–7.7).
FIGURE 7.4 Although the lesion was very extensive and reached into the area of the joint, conservative treatment with curettage and filling of the cavity with autogenous cancellous bone was performed. The patient will remain in a follow-up control for many years.
TABLE 7.2 Lesions with possible tooth root resorption on x-rays.
Ameloblastoma
Ameloblastic fibroma
Odontogenic myxoma
Adenomatoid odontogenic tumor
Cementoma
Calcifying odontogenic cyst
Odontogenic keratocyst
Ossifying fibroma
Fibrous dysplasia
Desmoplastic fibroma
Eosinophilic granuloma
Giant-cell granuloma
Hemangioma
Osteosarcoma
Plasmocytoma

62 |
J. Prein |
Nonodontogenic Tumors and Tumorlike
Lesions Within the Facial Bones
Mesenchymal tumors in the jaw bone have other characteristics compared with those of the same name in the postcranial skeleton. They are less often benign than odontogenic tumors. Some appear almost exclusively in facial bones, such as the osteoma and the ossifying fibroma, and some, such as the giant-cell tumor, are not found in the facial bones. On the other hand, the giant cell granuloma, except as a brown tumor with hyperparathyroidism, is not observed outside the fa-
FIGURE 7.5 Polycystic lesion in the left mandibular retromolar and angle area. Diagnosis: ameloblastoma.
FIGURE 7.6 Reconstruction of the mandibular defect with a reconstruction plate and an autologous bone graft taken from the iliac crest.
FIGURE 7.7 Two years after the reconstruction, the reconstruction plate was removed and dental implants inserted.
cial bones. For the pathologist, however, it may be difficult or impossible to differentiate between a giant cell tumor and a giant cell granuloma. Therefore, precise information about the clinical situation is mandatory for the pathologist. Recognizing that giant cell tumors do not appear in the facial bones is one of the most important observations made in recent years. Until the mid-1970s, many patients were overtreated with mutilating resections because giant-cell granulomas were misinterpreted as giant-cell tumors.
An important diagnostic sign is the vitality of the teeth. They often remain vital although their roots are located in the empty spaces of the cystic lesions (Figures 7.8 and 7.9).
7. Benign Tumors of the Maxillofacial Region
FIGURE 7.8 Extensive cystic lesion in the right horizontal part of the mandible surrounding the roots of the teeth 44, 45, 46, and 47. All teeth remained vital. Diagnosis: giant-cell granuloma.
The establishment of a special registry for tumors of the facial skeleton including odontogenic lesions in 1971 by the Ger- man-Austrian-Swiss Association for the Study of Tumors of the Face and Jaws (DÖSAK) and the analysis of all the giantcell lesions in the registry has led to the recognition that malignant giant cell tumors do not appear in the facial skeleton.
It was in 1974 that the DÖSAK sponsored a symposium under the chairmanship of Professors Uehlinger and Remagen during which several reclassifications had to be done.
In benign tumors, one has in general to differentiate between cartilaginous, osteofibrous, cystlike lesions, and lesions that derive from the vessels. Most of the round-cell tumors and lymphatic tumors are malignant. On x-ray examinations it is rarely possible to establish a diagnosis, because very few pathognomonic signs exist. Lesions appearing in the mandible allow more often at least approximate conclusions than those in the maxilla, whereas on regular x-ray films a very monotonous appearance of the lesions is observed.
In the mandible, most appear to be cystlike, regardless of whether they are benign or malignant. Some allow at least approximate conclusions according to the degree of metaplastic bone formation, which is dependent on age and further activities within the tumor.
The following list mentions the main benign nonodontogenic lesions in the facial skeleton:
Chondroblastic: enchondroma chondroblastoma chondromyxoid fibroma osteochondroma
Osseous origin: osteoma
osteoblastoma and osteoid-osteoma ossifying fibroma
fibrous dysplasia
63
FIGURE 7.9 After careful curettage of this lesion and defect filling with autogenous cancellous bone, only tooth 47 lost its vitality.
Histiocytosis x:
Langerhans cell granuloma
Vascular origin: hemangioma
Probably semimalignant: desmoplastic fibroma
Unknown etiology:
central giant-cell granuloma juvenile bone cyst aneurysmal bone cyst
Radical excision is necessary for all cartilaginous lesions because they have a strong tendency for recurrence. Resection or enucleation is sufficient for osteoma, osteoblastoma, ossifying fibroma, hemangioma, central giant-cell granulomas, and aneurysmal bone cysts.
A juvenile bone cyst is an empty hole without an epithelial lining. Apparently, the opening and the subsequent bleeding into the cavity initiates reossification of the area.
Surgical contouring, or in smaller lesions enucleation, is the treatment for fibrous dysplasia. Because of the tendency for recurrence or regrowth, clinical and radiologic follow-up for many years is indicated. The tendency toward malignant transformation is very low, although proven malignant transformation has been seen in connection with radiotherapy for a fibrous dysplasia.
The treatment of eosinophilic granuloma depends on its monostotic or multilocular appearance. Although desmoplastic fibroma may be considered as semimalignant and its growth pattern may be infiltrative into the cancellous areas of the bone, a first operative step can be enucleation for those well delineated on x-rays and more radical resection for those not well demarcated or in the case of recurrences.
Generally, radiotherapy is not indicated for any of the abovementioned lesions. On the contrary, radiotherapy may be harm-
64
ful since it may cause a transformation of some of these lesions into osteosarcomas. Radiotherapy may even cause secondary osteosarcomas without any lesions in this area.
References
1.Prein J, Remagen W, Spiessl B, Uehlinger E. Atlas of Tumors of the Facial Skeleton. Odontogenic and Non-odontogenic Tumors. New York: Springer Verlag; 1985.
J. Prein
2.Prein J, Remagen W, Spiessl B, Schafroth U. Ameloblastic fibroma and its sarcomatous transformation. Pathol Res Pract. 1979;11:123–130.
3.Pindborg JJ, Hjorting-Hansen E. Atlas of Diseases of the Jaws. Copenhagen: Munksgaard; 1974.
4.Takahashi K, Kitajima T, Lee M, Iwasaki N, Inoue SI, Matsue N, et al. Granular cell ameloblastoma of the mandible with metastasis to the third thoracic vertebra. Clin Orthop. 1985;197: 171–180.
