
- •1. Topographic Surface Anatomy
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •3. Superficial Face
- •Guide
- •Facts & Hints
- •4. Neck
- •Guide
- •Facts & Hints
- •5. Nasal Region
- •Guide
- •Facts & Hints
- •6. Oral Region
- •Guide
- •Facts & Hints
- •7. Pharynx
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •13. Cerebral Vasculature
- •Guide
- •Facts & Hints
- •14. Topographic Anatomy
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •16. Spinal Cord
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Thorax
- •18. Topographic Anatomy
- •Guides
- •Facts & Hints
- •19. Mammary Gland
- •Guides
- •Facts & Hints
- •20. Body Wall
- •Guides
- •Facts & Hints
- •21. Lungs
- •Guides
- •Facts & Hints
- •22. Heart
- •Guides
- •Facts & Hints
- •23. Mediastinum
- •Guides
- •Facts & Hints
- •Abdomen
- •24. Topographic Anatomy
- •Guide
- •Facts & Hints
- •25. Body Wall
- •Guide
- •Facts & Hints
- •26. Peritoneal Cavity
- •Guide
- •Facts & Hints
- •27. Viscera (Gut)
- •Guide
- •Facts & Hints
- •28. Viscera (Accessory Organs)
- •Guide
- •Facts & Hints
- •29. Visceral Vasculature
- •Guide
- •Facts & Hints
- •30. Innervation
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •32. Topographic Anatomy
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •35. Urinary Bladder
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •39. Testis, Epididymis & Ductus Deferens
- •Guide
- •Facts & Hints
- •40. Rectum
- •Guide
- •Facts & Hints
- •41. Vasculature
- •Guide
- •Facts & Hints
- •42. Innervation
- •Guide
- •Facts & Hints
- •Upper Limb
- •43. Topographic Anatomy
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •48. Neurovasculature
- •Guide
- •Facts & Hints
- •Lower Limb
- •49. Topographic Anatomy
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •51. Knee
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •54. Neurovasculature
- •Guide
- •Facts & Hints
FACTS & HINTS
High-Yield Facts
Clinical Points
Micturition
The bladder has a capacityof 400 to 500 mL
During micturition coordinated reflexive contraction of the detrusor and relaxation of the external urethral sphincter occur Controlled byautonomic and visceral innervation
Visceral afferent fibers traveling along tract of parasympathetic fibers stimulated bystretching (and pain in lower bladder)
Parasympathetic innervation via pelvic splanchnic nerves and pelvic plexus reflexivelystimulates detrusor contraction during micturition.
Sympathetic fibers via hypogastric plexus to bladder neck relaxes bladder neck (internal urethral sphincter) and prevents retrograde ejaculation during micturition in males
page 178
page 179
Clinical Points
Fractures of the Pelvis and Bladder Injury
The bladder lies immediatelyposterior to the pubic symphysis and fractures of the pubis can be complicated byrupture of the bladder. The rupture can result in the extravasation of urine intraperitoneallyif the peritoneum is torn
UrinaryTract Infections (UTIs)
As a result of a shorter urethra, women are more susceptible to UTIs Commonlyoccurs in women following sexual intercourse Pathogen is commonlyEscherichia coli
Infection maylead to urethritis, cystitis, or pyelonephritis (inflammation of urethra, bladder, and kidneys, respectively). Symptoms include: dysuria, urgency, frequency, and occasionallyhematuria
UrinaryStress Incontinence
Factors maintaining continence in the female are the external urethral sphincter (striated muscle surrounding middle third of urethra) and support of the bladder and urethra bythe levator ani muscles
Urinarystress incontinence is an involuntaryloss of urine that occurs during coughing, sneezing, laughing, lifting, or exercise, because of the inabilityof these muscles to counter the increase in intra-abdominal pressure.
Urinarystress incontinence is often seen in women who have had multiple pregnancies and vaginal childbirths and in men following prostate surgery
About 50% of all women have occasional urinaryincontinence
Mnemonics
Memory Aids
"Water under the bridge" -denotes relationship of ureter (water) to uterine artery, as it passes under the artery.
282 / 425

36 Uterus, Vagina and Supporting Structures
STUDYAIMS
At the end of your study, you should be able to:
Describe the anatomyof the uterus and its supporting ligaments
Know the anatomyof the ovaryand the uterine tubes in relation to the pelvic cavity, the peritoneum, and the uterus
Know the anatomyof the cervix
Understand the orientation of the cervixrelative to the position of the uterus and changes with childbirth
Understand the anatomyof the vagina
283 / 425

GUIDE
Pelvis and Perineum: Uterus, Vagina, and Supporting Structures
[Plate 352, Uterus, Vagina and Supporting Structures]
284 / 425
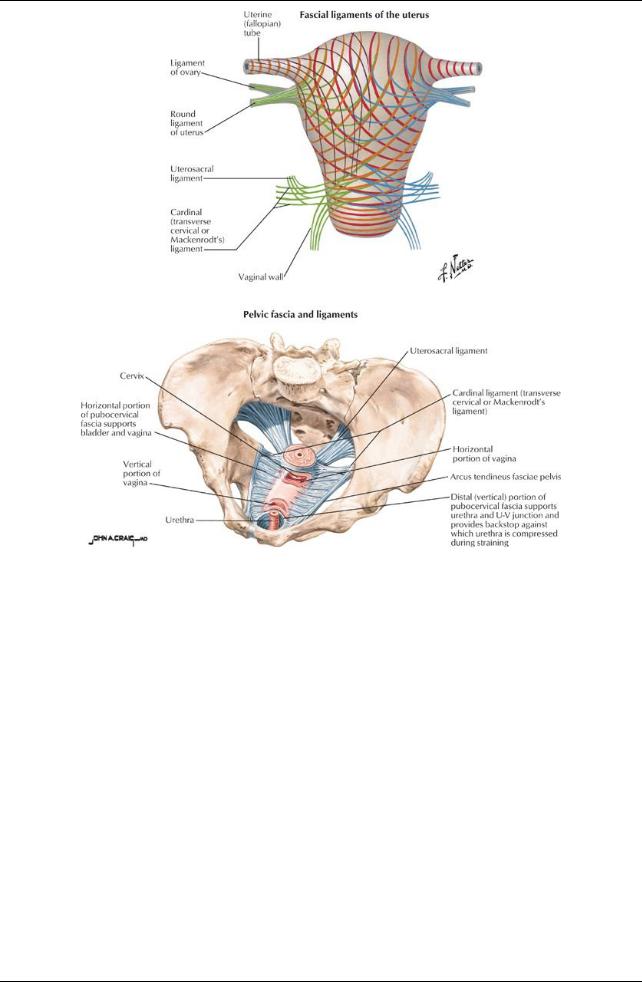
[Plate 353, Uterus: Fascial Ligaments]
285 / 425
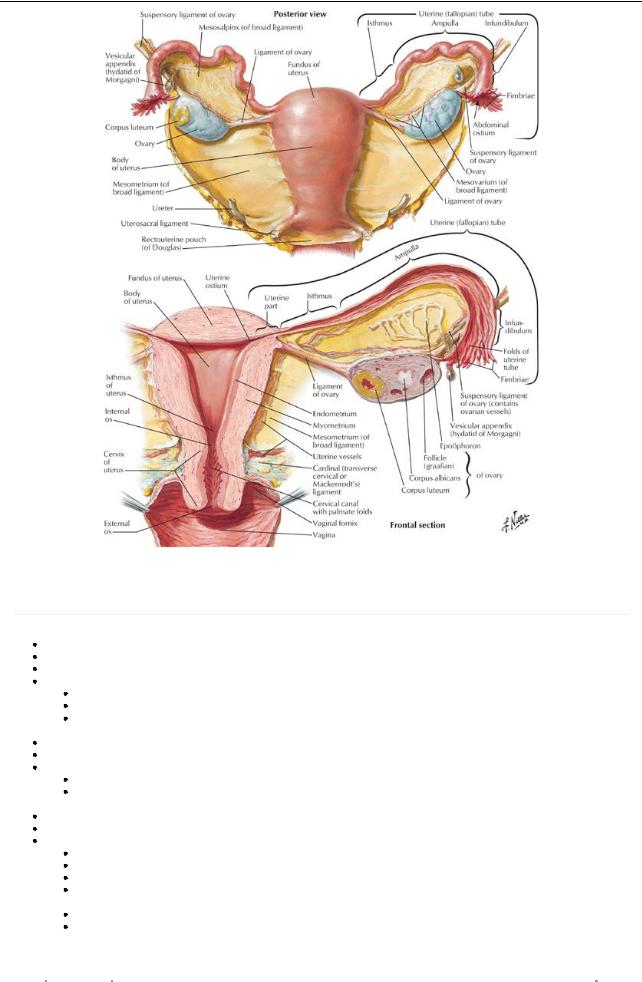
[Plate 355, Uterus and Adnexa]
Uterus
Basic structure
page 180
page 181
Pear-shaped organ
Approximately8 cm long and 5 cm wide Supported bythe pelvic diaphragm Composed of
Body(corpus) -upper two thirds
Fundus-rounded upper part superior to the entrances of the uterine tubes
Isthmus-narrower area just above the cervix
 Cervix(neck) -cylindrical inferior part that projects into the superior vagina Uterine cavityis small (6 cm in length) and slit-like
Cervix(neck) -cylindrical inferior part that projects into the superior vagina Uterine cavityis small (6 cm in length) and slit-like
Uterine horns are superolateral regions where the uterine (Fallopian tubes) enter Uterine wall has three layers
Perimetrium-outer layer of peritoneum with underlying connective tissue
Myometrium-middle, thick layer of smooth muscle
 Endometrium-vascular inner mucosal layer the thickness of which varies with menstrual cycle and age The uterus has two surfaces: anteroinferior and posterosuperior
Endometrium-vascular inner mucosal layer the thickness of which varies with menstrual cycle and age The uterus has two surfaces: anteroinferior and posterosuperior
Aportion of the cervix, body, and fundus of the uterus is covered with peritoneum Cervix
Thick-walled canal, 2.5 cm long, connecting the bodyof the uterus with the vagina
Communicates superiorlyvia internal os with uterus
Communicates with vagina inferiorlyvia external os
Approximatelyhalf of the cervixlies above the vagina (supravaginal) and is covered posteriorlywith the peritoneum of the rectouterine pouch
The bladder is separated from the anterior surface of the supravaginal part of the cervixbyconnective tissue The lower half of the cervix(vaginal part) protrudes into the vagina and can be examined clinically
Relationships of the uterus
|
Laterally- |
Broad ligament, transverse cervical (cardinal ligaments), ureters |
|
|
|
|
|
286 / 425
Anterior- |
Vesicouterine pouch, superior surface of bladder |
PosteriorRectouterine pouch and anterior surface of rectum, loops of intestine in pouch
Vascular supply of uterus (including cervix)
Arterial
Uterine arteries (branches of internal iliac arteries)
Vaginal arteries (branches of uterine arteries with anastomoses with internal pudendal arteries)
Venous drainage: via uterine venous plexus to internal iliac veins
Lymphatics drain to
External iliac nodes
Internal iliac and sacral nodes
Superficial inguinal nodes (along round ligament)
Innervation
From the uterovaginal plexus, a subdivision of the inferior hypogastric (pelvic) plexus
Sympathetic, parasympathetic, and visceral afferents to and from the uterus pass through this plexus
Sympathetic innervation from lower lumbar spinal cord segments via lumbar splanchnic nerves and intermediate plexuses Parasympathetic innervation from pelvic splanchnic nerves (S2,3,4 spinal cord levels) via pelvic plexus
Afferent fibers with pain information from bodyand fundus ascend through plexuses to lumbar splanchnic nerves to reach upper lumber/lower thoracic spinal cord segments
Afferent fibers with pain information from cervixand all information except for pain from bodyand fundus follow parasympathetic fibers back to central nervous system
Vagina
Basic structure
Muscular tube, 8 to 10 cm long
Superior end surrounds the cervix: upper two thirds lie within pelvic cavity Slopes downward and forward through the pelvic diaphragm
Opens inferiorlyinto vestibule between labia minora Lining has multiple transverse folds-rugae
Recessed area of vagina around the cervixis called the vaginal fornix; composed of shallow anterior, deep posterior, and lateral fornices Posterior fornixdirectlyrelated to rectouterine pouch
Relationships of the vagina
Superior |
External os cervix |
Inferior |
Vestibule between labia minora |
Anterior |
Posterior wall bladder |
Posterior |
Rectouterine pouch |
|
Ampulla of rectum |
Lateral |
Levator ani muscles |
Blood supply
Uterine arteries supplies superior part
Vaginal arteries supplymiddle part
Lower part supplied bymiddle rectal and internal pudendal arteries
Venous drainage
Vaginal venous plexus to uterine venous plexus to internal iliac veins
Innervation
Upper three fourths same as uterus
Lower one fourth is somatic via the pudendal nerve
Visceral and sympathetic fibers reach the lower one fourth via the pudendal nerve; no parasympathetics
Variations in Position of the Uterus
When the bladder is empty, bodyof the uterus bent anteriorlyon the cervix: anteflexion
Axis of cervixalso bent forward relative to axis of vagina: anteversion
Thus the bodyof uterus lies on superior surface bladder
Full bladder reduces these angles
Reversal of these angles is called retroversion and retroflexion
Ligaments Associated with the Uterus
Broad ligament
Double layer of peritoneum that sweeps up and over the uterus, ovaries, and the uterine tubes
Thus has an anterior and a posterior lamina
Extends from the sides of the uterus to the lateral pelvic walls
287 / 425
Part that suspends the ovaryfrom the posterior lamina is the mesovarium
Part of broad ligament above the level of the ovaryand mesovarium that sweeps over the uterine tubes is the mesosalpinx
Part of broad ligament below the mesovarium or the mesenteryof the uterus
Uterine arteries and veins run mediallyfrom the internal iliac arteries to the uterus at its base Encloses the plexus of uterine veins
Ligament of the ovary
Extends from the medial pole of ovaryto the lateral wall of the uterus, just beneath the entrance of the uterine tube, on each side Remnant of proximal part of embryonic gubernaculums
page 182 page 183
Round ligament of the uterus
Extends from the lateral wall of the uterus, just beneath the entrance of the uterine tube, to the lateral pelvic wall on each side Crosses external iliac vessel to enter deep inguinal ring
Passes through inguinal canal to labium majus Remnant of distal part of embryonic gubernaculums
Suspensory ligament of the ovary
An extension of the broad ligament superiorlyon the posterolateral pelvic wall
Covers the ovarian vessels, associated nerves, and lymphatics
Uterine (Fallopian) Tubes
Basic anatomy
Approximately10 cm long, extending laterallyfrom the uterine horns to the peritoneal cavitynear the ovaries
Run in free upper border of broad ligament (mesosalpinx)
Provide a channel for ova from ovaryto uterine cavityand site for fertilization
Divided into four parts for descriptive and functional purposes
Infundibulum
Horn-shaped distal end
Opens into peritoneal cavity
Has finger-like processes (fimbriae) at distal end that spread over surface of ovary
Ampulla
Widest and longest part
Where fertilization usuallyoccurs
Connects infundibulum and isthmus
Isthmus
Thick-walled
Enters uterine horn
Uterine part: passes through the wall of the uterus
Blood supply
Arterial (anastomoses)
Uterine arteries
Ovarian arteries
Venous drainage
Uterine venous plexus
Ovarian veins
Lymphatics
To lumbar lymph nodes
Innervation
Ovarian and uterine plexuses = subdivisions of pelvic plexus
page 183 page 184
Ovaries
Basic structure
Ovoid in shape
Approximately4 cm long and 2 cm wide
Lie in the ovarian fossa on lateral pelvic wall between external and internal iliac vessels Attached to the broad ligament bymesovarium, which transmits ovarian vessels
Connected to lateral wall bysuspensoryligaments of the ovary, containing ovarian vessels, nerves, and lymphatics
Arterial supply
Ovarian artery
288 / 425
Branch of abdominal aorta
Terminates in ovarian and tubal branches
Venous drainage
Pampiniform plexus combines to form single ovarian vein
On right this drains into the inferior vena cava
On the left drains into the left renal vein
Lymphatics
Follow ovarian vessels to lumbar lymph nodes
Innervation
Sympathetic and afferent fibers reach the ovaryvia the ovarian vessels
Parasympathetic fibers from pelvic splanchnic nerves (S2,3,4 spinal cord levels) reach ovaryvia same route
289 / 425
