
- •1. Topographic Surface Anatomy
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •3. Superficial Face
- •Guide
- •Facts & Hints
- •4. Neck
- •Guide
- •Facts & Hints
- •5. Nasal Region
- •Guide
- •Facts & Hints
- •6. Oral Region
- •Guide
- •Facts & Hints
- •7. Pharynx
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •13. Cerebral Vasculature
- •Guide
- •Facts & Hints
- •14. Topographic Anatomy
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •16. Spinal Cord
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Thorax
- •18. Topographic Anatomy
- •Guides
- •Facts & Hints
- •19. Mammary Gland
- •Guides
- •Facts & Hints
- •20. Body Wall
- •Guides
- •Facts & Hints
- •21. Lungs
- •Guides
- •Facts & Hints
- •22. Heart
- •Guides
- •Facts & Hints
- •23. Mediastinum
- •Guides
- •Facts & Hints
- •Abdomen
- •24. Topographic Anatomy
- •Guide
- •Facts & Hints
- •25. Body Wall
- •Guide
- •Facts & Hints
- •26. Peritoneal Cavity
- •Guide
- •Facts & Hints
- •27. Viscera (Gut)
- •Guide
- •Facts & Hints
- •28. Viscera (Accessory Organs)
- •Guide
- •Facts & Hints
- •29. Visceral Vasculature
- •Guide
- •Facts & Hints
- •30. Innervation
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •32. Topographic Anatomy
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •35. Urinary Bladder
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •39. Testis, Epididymis & Ductus Deferens
- •Guide
- •Facts & Hints
- •40. Rectum
- •Guide
- •Facts & Hints
- •41. Vasculature
- •Guide
- •Facts & Hints
- •42. Innervation
- •Guide
- •Facts & Hints
- •Upper Limb
- •43. Topographic Anatomy
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •48. Neurovasculature
- •Guide
- •Facts & Hints
- •Lower Limb
- •49. Topographic Anatomy
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •51. Knee
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •54. Neurovasculature
- •Guide
- •Facts & Hints

30 Innervation
STUDYAIMS
At the end of your study, you should be able to:
Describe the parasympathetic contribution to the autonomic innervation of abdominal viscera Describe the sympathetic contribution to the autonomic innervation of abdominal viscera Understand the organization of the autonomic plexuses of the abdomen
Describe the somatic innervation of the abdominal wall Know the branches of the lumbar plexus
Understand the principle of referred pain and describe common patterns of pain referral from the abdominal viscera
239 / 425
GUIDE
Abdomen: Innervation
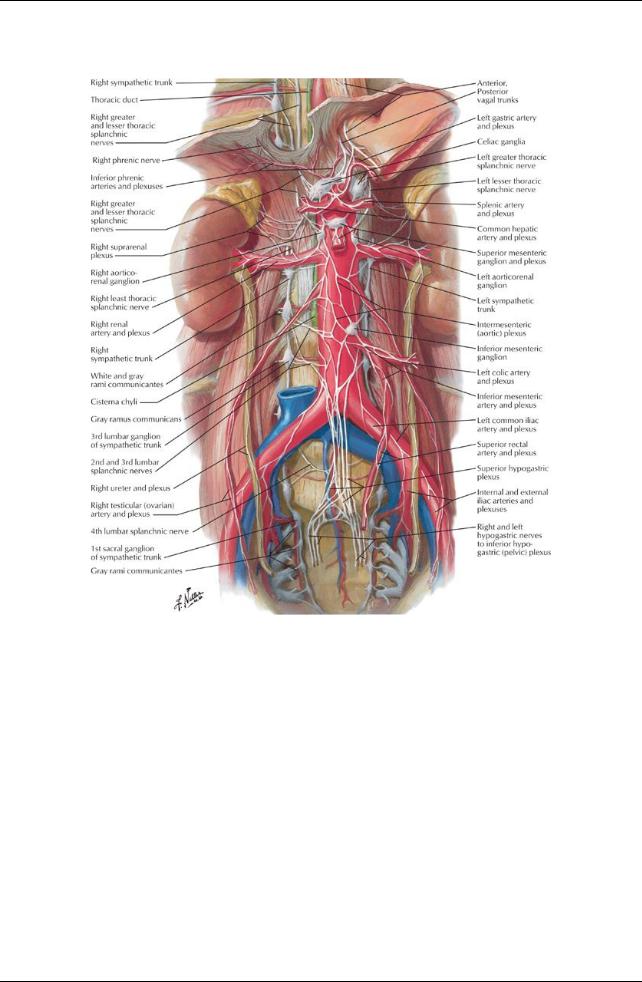
[Plate 297, Autonomic Nerves and Ganglia of Abdomen]
240 / 425
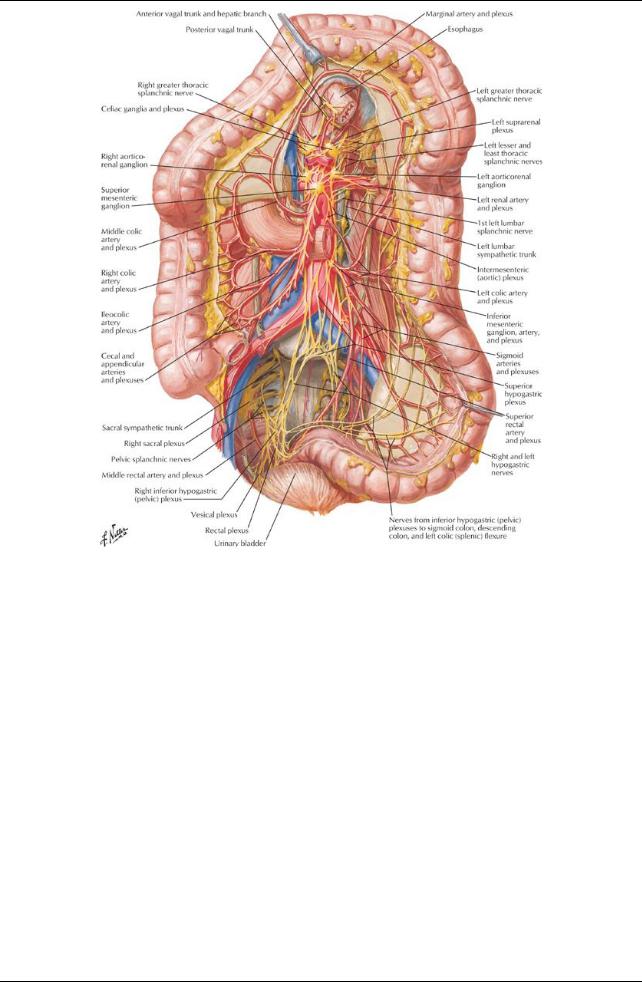
[Plate 302, Autonomic Innervation of Large Intestine]
241 / 425
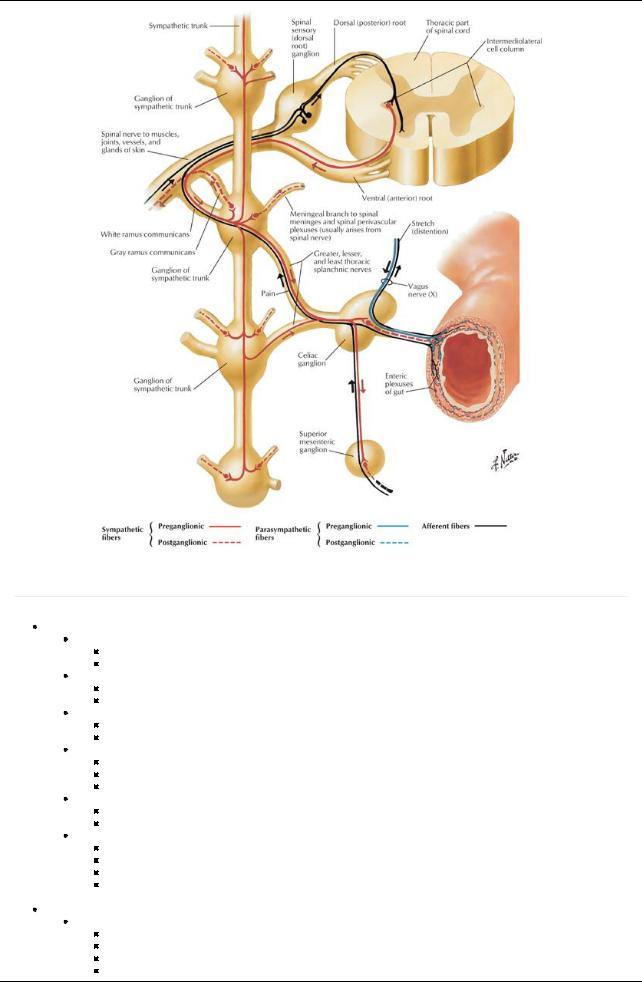
[Plate 304, Autonomic Reflex Pathways: Schema]
Autonomic Nerves
page 158
page 159
Parasympathetic nerves
Preganglionic fibres
Provided byvagus nerve and sacral splanchnic nerves
Synapse with postganglionic fibres in the walls of the relevant organs
Vagus nerve (CN X)
Give rise to anterior and posterior vagal trunks in thorax
Trunks enter abdomen at the esophageal hiatus
Anterior trunk (mainlyfrom the left vagus)
Enters anterior to the esophagus
Gives branches to the anterior surface of the stomach and to the liver
Posterior trunk (mainlyfrom the right vagus)
Enters posterior to the esophagus
Gives branches to the posterior surface of the stomach and celiac plexus
Fibers pass inferiorlyto root of superior mesenteric artery
Fibers contribute to perivascular plexuses
Accompanying celiac and superior mesenteric arteryand their branches
Extend as far as the arterial supply(two thirds of the way along the transverse colon)
Pelvic splanchnic nerves
From spinal cord levels S2-S4
Emerge through pelvic sacral foramina
Ascend from pelvis running in sigmoid mesocolon and peritoneum of posterior abdominal wall
Supplydistal one third of transverse colon, descending colon, sigmoid colon, and superior rectum
 Postganglionic (postsynaptic) parasympathetic neurons found in enteric ganglia in wall of viscus Sympathetic nerves
Postganglionic (postsynaptic) parasympathetic neurons found in enteric ganglia in wall of viscus Sympathetic nerves
Right and left sympathetic trunks
Enter behind the medial arcuate ligament of the diaphragm
Descend along psoas major, with right trunk behind inferior vena cava (IVC)
Lie on anterolateral sides of lumbar vertebrae
Receive white rami communicantes from, and send grayrami communicantes to, ventral rami of L1-L3 spinal nerves
242 / 425
Postganglionic fibers in grayrami communicantes to corresponding ventral rami of spinal nerves distributed to the bodywall and lower limb
Give off three to four lumbar splanchnic nerves (presynaptic sympathetic fibers) mediallyto:
Intermesenteric plexus
Inferior mesenteric plexus
Superior hypogastric plexus
Postsynaptic fibers from these plexuses innerve nearbytarget organs.
Sympathetic (paravertebral) ganglia
Total of four abdominal sympathetic ganglia per trunk
Prevertebral sympathetic ganglia
Cell bodies of postsynaptic sympathetic neurons
 Found in plexuses around roots of major branches of aorta Aortic plexuses
Found in plexuses around roots of major branches of aorta Aortic plexuses
Network of parasympathetic and sympathetic nerves
Parasympathetic mainlyfrom posterior vagal trunk (see above)
Sympathetic fibers from thoracic and lumbar splanchnic nerves (Section 3: Thorax)
Contain prevertebral ganglia
Include:
Celiac plexus
Aorticorenal plexus
Renal plexus
Superior mesenteric plexus
Intermesenteric plexus
Inferior mesenteric plexus
Perivascular plexuses derived from the aortic plexuses
Visceral afferent fibers
Carrypain information
Travel with sympathetic fibers back to spinal cord
Referred pain
Information carried byvisceral afferent fibers
Fibers travel back to T5-L2/3 spinal cord levels via thoracic and lumbar splanchnic nerves
Clinical phenomenon of referred pain is visceral pain perceived as somatic pain over the dermatomes innervated bycutaneous nerves with fibers from those spinal cord levels:
Organ |
Spinal Level |
Area of Referred Pain |
Stomach |
T5-T9 |
Epigastric or left hypochondrium |
Duodenum |
T5-T8 |
Epigastric or right hypochondrium |
Jejunum |
T6-T10 |
Periumbilical |
Ileum |
T7-T10 |
Periumbilical |
Caecum |
T10-T11 |
Periumbilical or right lower quadrant |
Appendix |
T10-T11 |
Periumbilical, then to right iliac fossa |
Ascending colon |
T10-T12 |
Periumbilical or right lumbar |
Sigmoid colon |
L1-L2 |
Left lower quadrant |
Spleen |
T6-T8 |
Left hypochondrium |
Liver & gallbladder |
T6-T9 |
Epigastric, later to right hypochondrium |
Pancreas |
T7-T9 |
Inferior epigastrium |
Kidney |
T10-L1 |
Small of back, flank |
Ureter |
T11-L1 |
Loin to groin |
Somatic Nerves
Thoracoabdominal nerves
Ventral primaryrami of T7-T11
Travel in the neurovascular plane between the internal oblique and transversus abdominis muscles
 Innervate anterolateral abdominal wall, including parietal peritoneum Subcostal nerves
Innervate anterolateral abdominal wall, including parietal peritoneum Subcostal nerves
Ventral primaryrami of T12
Follow the inferior border of the 12th rib
Enter abdomen behind lateral arcuate ligaments
Cross quadratus lumborum muscles and pierces transversus abdominis muscles to enter neurovascular plane
 Innervate anterolateral abdominal wall (including parietal peritoneum) Lumbar plexus
Innervate anterolateral abdominal wall (including parietal peritoneum) Lumbar plexus
Iliohypogastric nerve (L1)
Divides into lateral and anterior cutaneous branches
Pierces internal and external oblique muscles
Supplies buttocks and suprapubic region
Ilioinguinal nerve (L1)
Travels in inguinal canal
Joins spermatic cord after piercing internal abdominal oblique (Note: does not enter inguinal canal through deep inguinal ring)
Provides cutaneous branches to skin of inguinal region
Genitofemoral nerve (L1,2)
Emerges from anterior surface of psoas major muscle
Genital branch enters deep inguinal ring to innervate the cremaster muscle
Femoral branch passes beneath inguinal ligament in vascular compartment to enter femoral triangle and provides
243 / 425
cutaneous branches to anteromedial thigh Lateral femoral cutaneous nerve (L2,3)
Passes beneath or through inguinal ligament, medial to anterior superior iliac spine (ASIS)

 Innervates anterolateral thigh Obturator nerve (L2-L4)
Innervates anterolateral thigh Obturator nerve (L2-L4)
Emerges from medial border of psoas major muscle
Passes through pelvis
Exits via obturator canal

 Supplies skin and adductor muscles of medial thigh Femoral nerve (L2-L4)
Supplies skin and adductor muscles of medial thigh Femoral nerve (L2-L4)
Emerges from lateral psoas major muscle
Innervates iliacus
Passes beneath inguinal ligament on surface of iliopsoas muscle in muscular compartment
Enters femoral triangle to innervate flexors of the hip/extensors of leg at knee, and skin of anterior thigh, medial aspect of leg and foot.
Lumbosacral trunk (L4,5)
Enters pelvis passing over ala of sacrum
Contributes to formation of sacral plexus with ventral rami of S1-S4 spinal nerves
244 / 425
