
- •1. Topographic Surface Anatomy
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •3. Superficial Face
- •Guide
- •Facts & Hints
- •4. Neck
- •Guide
- •Facts & Hints
- •5. Nasal Region
- •Guide
- •Facts & Hints
- •6. Oral Region
- •Guide
- •Facts & Hints
- •7. Pharynx
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •13. Cerebral Vasculature
- •Guide
- •Facts & Hints
- •14. Topographic Anatomy
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •16. Spinal Cord
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Thorax
- •18. Topographic Anatomy
- •Guides
- •Facts & Hints
- •19. Mammary Gland
- •Guides
- •Facts & Hints
- •20. Body Wall
- •Guides
- •Facts & Hints
- •21. Lungs
- •Guides
- •Facts & Hints
- •22. Heart
- •Guides
- •Facts & Hints
- •23. Mediastinum
- •Guides
- •Facts & Hints
- •Abdomen
- •24. Topographic Anatomy
- •Guide
- •Facts & Hints
- •25. Body Wall
- •Guide
- •Facts & Hints
- •26. Peritoneal Cavity
- •Guide
- •Facts & Hints
- •27. Viscera (Gut)
- •Guide
- •Facts & Hints
- •28. Viscera (Accessory Organs)
- •Guide
- •Facts & Hints
- •29. Visceral Vasculature
- •Guide
- •Facts & Hints
- •30. Innervation
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •32. Topographic Anatomy
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •35. Urinary Bladder
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •39. Testis, Epididymis & Ductus Deferens
- •Guide
- •Facts & Hints
- •40. Rectum
- •Guide
- •Facts & Hints
- •41. Vasculature
- •Guide
- •Facts & Hints
- •42. Innervation
- •Guide
- •Facts & Hints
- •Upper Limb
- •43. Topographic Anatomy
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •48. Neurovasculature
- •Guide
- •Facts & Hints
- •Lower Limb
- •49. Topographic Anatomy
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •51. Knee
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •54. Neurovasculature
- •Guide
- •Facts & Hints

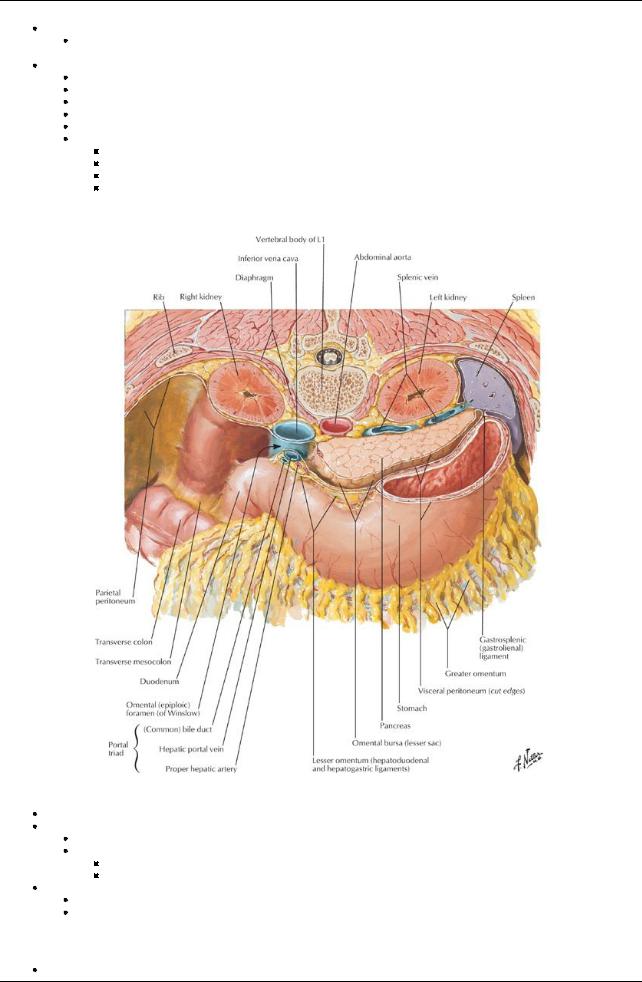
26 Peritoneal Cavity
STUDYAIMS
At the end of your study, you should be able to:
Understand the difference between the abdominopelvic and peritoneal cavities
Be able to explain the difference between the greater sac and the lesser sac (omental bursa)
Understand the organization of the peritoneal folds that form the greater omentum, lesser omentum, the mesentryof the small intestine, and other mesenteries and peritoneal ligaments
Know which organs are intraperitoneal, retroperitoneal, and secondarilyretroperitoneal Describe the subdivisions of the peritoneal cavity
203 / 425
GUIDE
Abdomen: Peritoneal Cavity
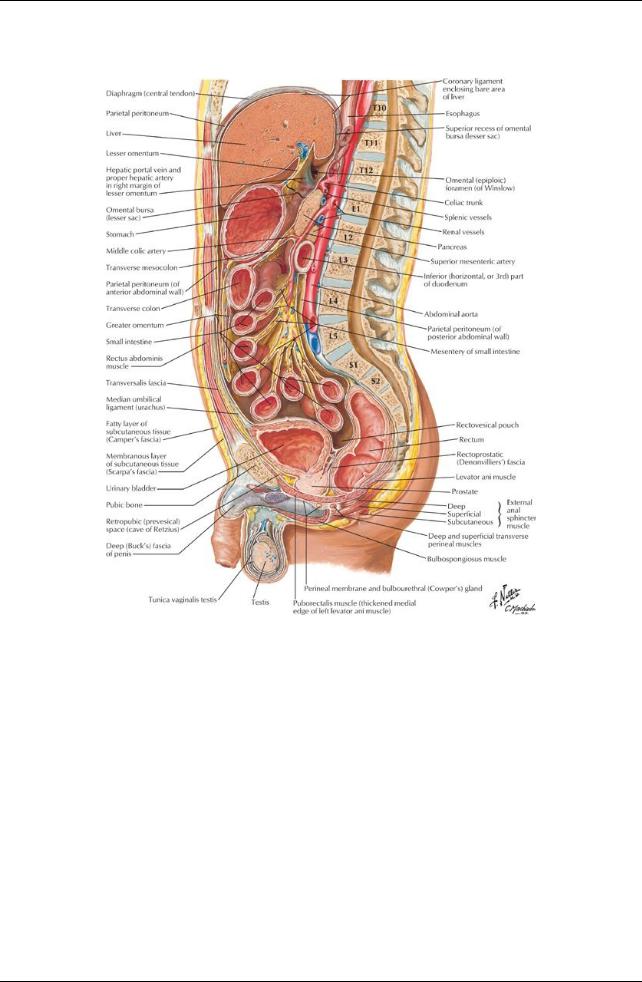
[Plate 323, Abdominal Wall and Viscera: Paramedian (Parasagittal) Section]
204 / 425
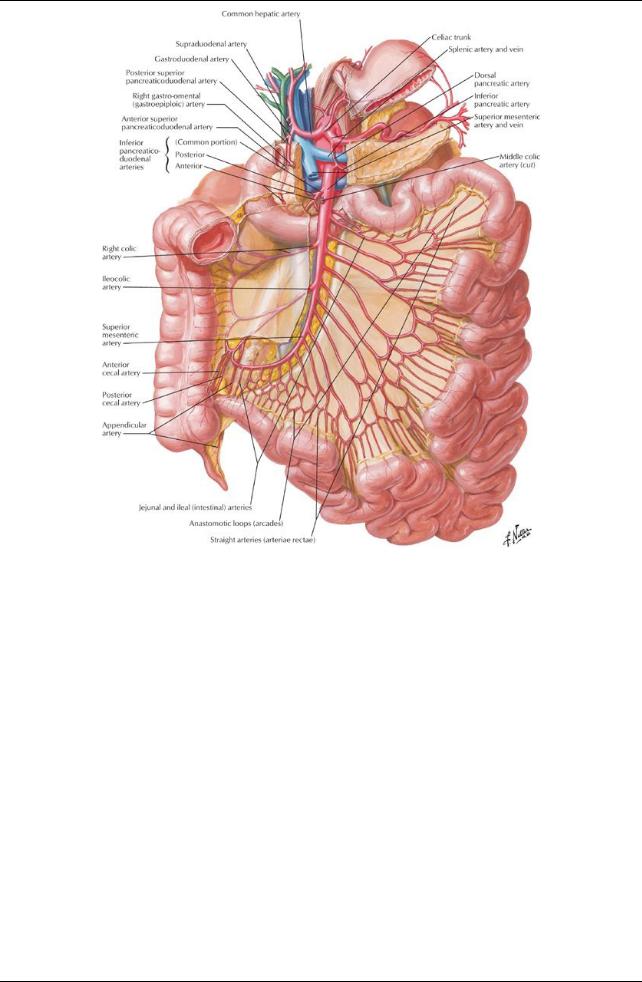
[Plate 287, Arteries of Small Intestine]
205 / 425
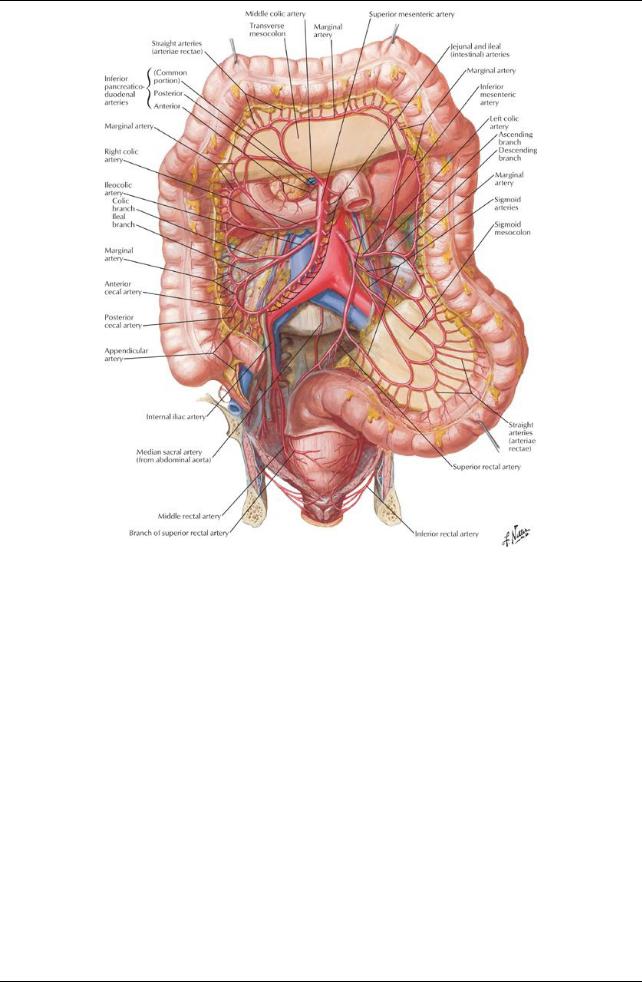
[Plate 288, Arteries of Large Intestine]
206 / 425
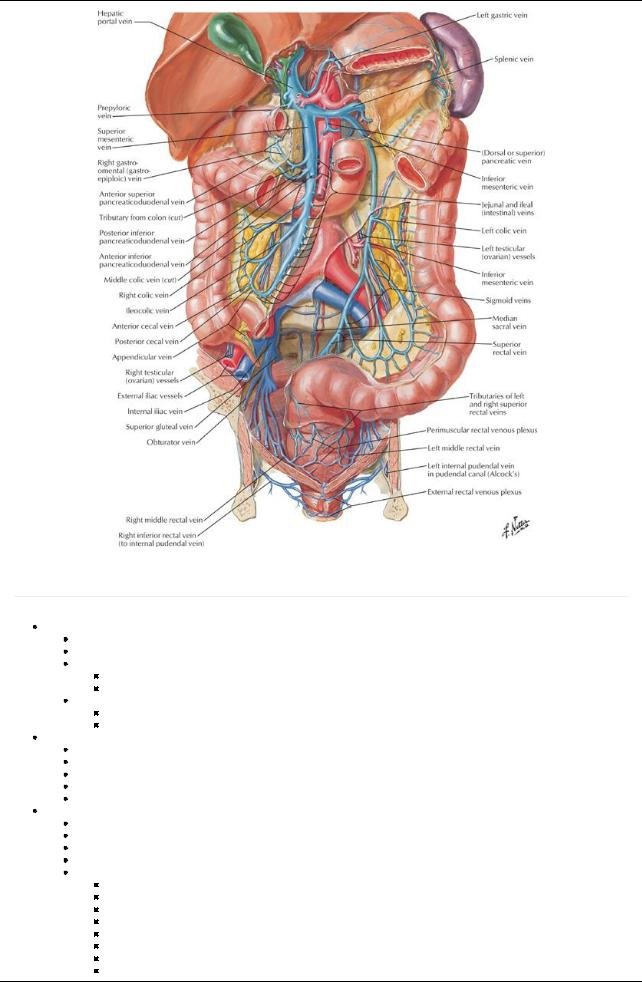
[Plate 291, Veins of Large Intestine]
Peritoneum
page 138
page 139
Serous membrane
Lines the abdominopelvic cavity
Consists of two continuous layers of mesothelium:
Parietal peritoneum
Lines the internal abdominal wall
Receives its neurovascular supplyfrom the region of the wall it lines
Visceral peritoneum
Invests abdominal viscera
Receives its neurovascular supplyfrom that of organ
Peritoneal cavity
Apotential space between the parietal and visceral layers of the peritoneum
Contains a thin film of fluid
No organs actuallylie within this potential space
Males: peritoneal cavityis completelyclosed
Females: communicates with exterior of bodyvia uterine tubes, uterus, and vagina
Intraperitoneal organs
Are organs nearlytotallycovered byvisceral peritoneum
Not actuallyinside the peritoneal cavity, but project into the peritoneal cavity
Are covered byperitoneum
Are attached to bodywall and other organs bymesenteries and ligaments
Include:
Liver
Spleen
Stomach
First part of duodenum
Jejunum
Ileum
Transverse colon
Sigmoid colon
207 / 425
 Superior rectum Primarilyretroperitoneal organs
Superior rectum Primarilyretroperitoneal organs
Organs that develop and remain beneath the parietal peritoneum
 Onlythe kidneys Secondarilyretroperitoneal organs
Onlythe kidneys Secondarilyretroperitoneal organs
Organs that developed with a short mesentery
Become pushed against parietal peritoneum lining the bodywall bygrowth of other organs, primarilythe small intestine.
Mesenteryof organ fuses with parietal peritoneum: fusion fascia
Peritoneum covers onlyits anterior surface, hence, secondarilyretroperitoneal
Organ can be freed at its lateral edge, along the plane of the fusion fascia
Include
Adrenal glands
Pancreas
Parts two through four of the duodenum Ascending and descending colon
Omenta
[Plate 265, Omental Bursa: Cross Section]
Omentum = double-layered fold of peritoneum
Lesser omentum: connects lesser curve of stomach and proximal duodenum to liver
Passes from the stomach and first part of the duodenum to adjacent organs
Consists of two parts:
Hepatogastric ligament
Hepatoduodenal ligament
Greater omentum
Hangs down from the greater curve of the stomach and proximal duodenum
Folds back on itself to attach to the transverse colon
Mesenteries
Mesentery= double layer of peritoneum created byinvagination of peritoneum byan organ
208 / 425
Is the continuityof visceral and parietal peritoneum
Provides a pathwayfor neurovascular communication between organ and bodywall
Contains lymph nodes and variable amounts of fat
The mesentery is the mesenteryof the small intestine
The mesocolon is the mesenteryof the large intestine
Transverse mesocolon
Sigmoid mesocolon
Peritoneal ligaments
page 139 page 140
Ligament = double layer of peritoneum connecting an organ to another organ or to the abdominal wall
Ligaments of the liver:
Falciform ligament: from liver to anterior abdominal wall
Gastrohepatic ligament
From lesser curvature of stomach to liver
= a portion of lesser omentum
Hepatoduodenal ligament
From the liver to the first part of the duodenum
= Right, thickened free edge of lesser omentum
Contains portal triad (portal vein, hepatic artery, bile duct)
Ligaments of the stomach
Gastrophrenic ligament: from stomach to inferior diaphragmatic surface
Gastrosplenic ligament: from stomach to hilum of spleen
Gastrocolic ligament: from stomach as the greater omentum to the transverse colon
Ligaments of the spleen
Gastrosplenic: from stomach to hilum of spleen
Splenorenal (lienorenal): from spleen to the left kidney
Phrenicocolic ligament (sustentaculum lienis)
From the left hepatic flexure of transverse colon to diaphragm
Supports the spleen
Peritoneal subdivisions
Greater sac: main peritoneal cavity Lesser sac (omental bursa)
Posterior to the stomach
Visible through the lesser omentum
Superior recess: limited bythe diaphragm and posterior layers of the coronaryligament of the liver (Section 4-4: Abdomen-Viscera (Gut))
Inferior recess: potential space between layers of the greater omentum Communicates with the greater sac via the epiploic foramen (of Winslow)
Boundaries of the epiploic foramen
Boundary |
Structures |
Anterior |
Hepatoduodenal ligament containing portal triad |
Posterior |
Inferior vena cava (IVC) and right crus of diaphragm which is covered bythe parietal peritoneum |
Superior |
Caudate lobe of liver which is covered bythe visceral peritoneum |
Inferior |
First part of duodenum, portal vein, hepatic artery, bile duct |
Supracolic compartment
Greater sac above the transverse mesocolon
 Contains stomach, liver, and spleen Infracolic compartment
Contains stomach, liver, and spleen Infracolic compartment
Greater sac below transverse mesocolon,
Contains small bowel, ascending and descending colon.
Divided into left and right divisions bythe mesenteryof the small intestine
Free communication between the supracolic and infracolic compartments via the paracolic gutter
Grooves or recesses between the ascending and descending colon and the posterior abdominal wall along their lateral borders
209 / 425
