
- •1. Topographic Surface Anatomy
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •3. Superficial Face
- •Guide
- •Facts & Hints
- •4. Neck
- •Guide
- •Facts & Hints
- •5. Nasal Region
- •Guide
- •Facts & Hints
- •6. Oral Region
- •Guide
- •Facts & Hints
- •7. Pharynx
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •13. Cerebral Vasculature
- •Guide
- •Facts & Hints
- •14. Topographic Anatomy
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •16. Spinal Cord
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Thorax
- •18. Topographic Anatomy
- •Guides
- •Facts & Hints
- •19. Mammary Gland
- •Guides
- •Facts & Hints
- •20. Body Wall
- •Guides
- •Facts & Hints
- •21. Lungs
- •Guides
- •Facts & Hints
- •22. Heart
- •Guides
- •Facts & Hints
- •23. Mediastinum
- •Guides
- •Facts & Hints
- •Abdomen
- •24. Topographic Anatomy
- •Guide
- •Facts & Hints
- •25. Body Wall
- •Guide
- •Facts & Hints
- •26. Peritoneal Cavity
- •Guide
- •Facts & Hints
- •27. Viscera (Gut)
- •Guide
- •Facts & Hints
- •28. Viscera (Accessory Organs)
- •Guide
- •Facts & Hints
- •29. Visceral Vasculature
- •Guide
- •Facts & Hints
- •30. Innervation
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •32. Topographic Anatomy
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •35. Urinary Bladder
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •39. Testis, Epididymis & Ductus Deferens
- •Guide
- •Facts & Hints
- •40. Rectum
- •Guide
- •Facts & Hints
- •41. Vasculature
- •Guide
- •Facts & Hints
- •42. Innervation
- •Guide
- •Facts & Hints
- •Upper Limb
- •43. Topographic Anatomy
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •48. Neurovasculature
- •Guide
- •Facts & Hints
- •Lower Limb
- •49. Topographic Anatomy
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •51. Knee
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •54. Neurovasculature
- •Guide
- •Facts & Hints

16 Spinal Cord
STUDYAIMS
At the end of your study, you should be able to:
Draw a schematic transverse section through the spinal cord, meninges, and vertebrae
Understand the structure and function of the dorsal and ventral spinal nerve roots and rami
Understand the general topographyand synaptic transmitters of the autonomic nervous system
Know the levels of the principle dermatomes
Describe the vasculature supplyof the spinal cord and vertebral column
115 / 425
GUIDE
Back and Spinal Cord: Spinal Cord
Spinal Cord
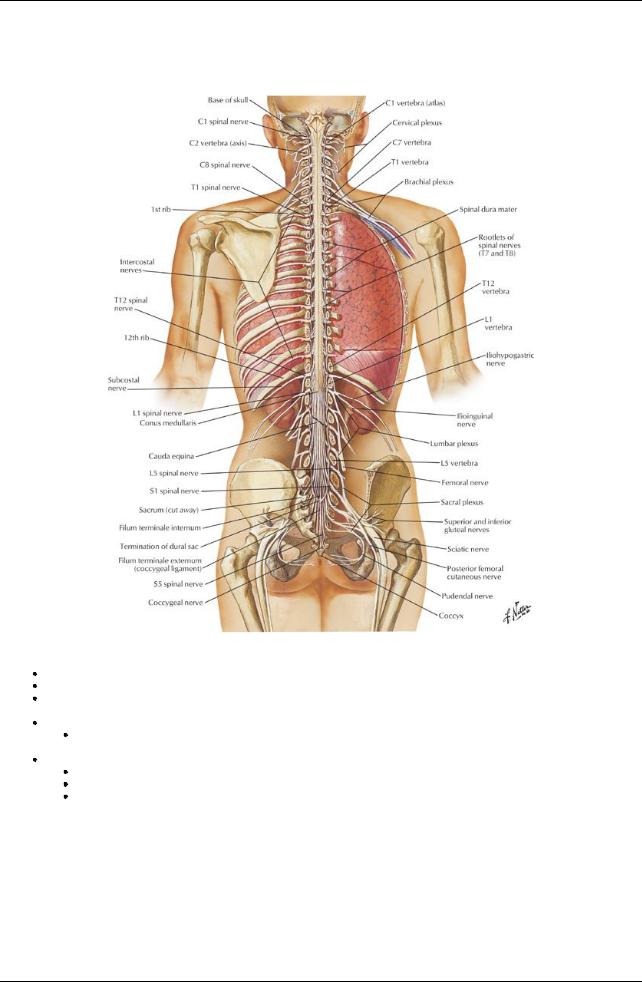
[Plate 157, Spinal Cord and Ventral Rami In Situ]
Originates at the inferior end of the medulla oblongata and terminates as conus medullaris Is approximately42 to 45 cm long from the foramen magnum to L2 (variable from T12-L3)
Is connected from the conus medullaris to the coccyxbythe filum terminale (a strand of connective tissue that connects exits from the dural sac and passes through the sacral hiatus)
Has two regional enlargements
Cervical-origin of the brachial plexus innervating the upper limb
 Lumbosacral-origin of the lumbar and sacral plexuses innervating the lower limb Has the following features in cross section
Lumbosacral-origin of the lumbar and sacral plexuses innervating the lower limb Has the following features in cross section
Dorsal median sulcus and ventral median fissure that divide cord into symmetrical halves
Central canal carrying cerebrospinal fluid (CSF)
White matter surrounding an H-shaped core of greymatter (ventral and dorsal horns)
Structure of Spinal Nerves
116 / 425
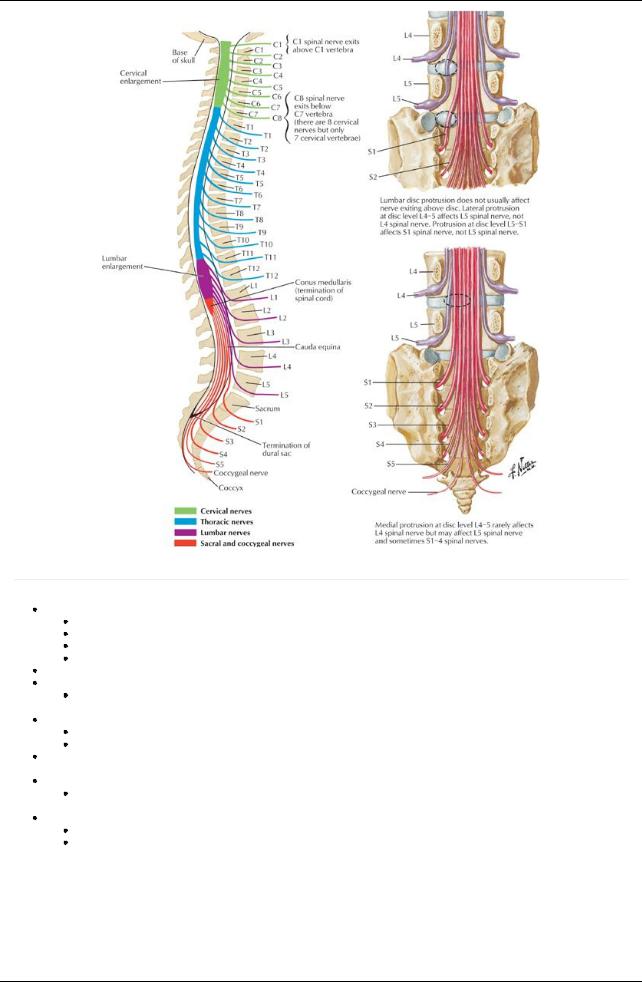
[Plate 158, Relation of Spinal Nerve Roots to Vertebrae]
page 89 page 90
31 pairs of spinal nerves
8 cervical, 12 thoracic, 5 lumbar, 5 sacral, 1 coccygeal
C1-C7 exit superior to corresponding vertebrae
C8 exits inferior to the C7 vertebra
T1-Co exit inferior to corresponding vertebrae
Cauda equina: spinal nerve roots inferior to the conus medullaris, travelling obliquelyto exit vertebral canal Ventral roots
Carryefferent (motor) fibers with their cell bodies in the ventral horn of the cord
 Maycontain presynaptic autonomic fibers Dorsal roots
Maycontain presynaptic autonomic fibers Dorsal roots
Carryafferent (general and visceral sensory) fibers with their cell bodies in the dorsal root ganglion (DRG)
Maybe absent in C1 and Co
Ventral and dorsal roots: combine to form a (mixed) spinal nerve which exits through the intervertebral foramen and divides almost immediatelyinto (mixed) ventral and dorsal rami
Ventral rami
Anterior and lateral branches
 Form plexuses and supplythe limbs and trunk Dorsal rami
Form plexuses and supplythe limbs and trunk Dorsal rami
Medial and lateral branches
Supplythe skin and true muscles of the back
117 / 425
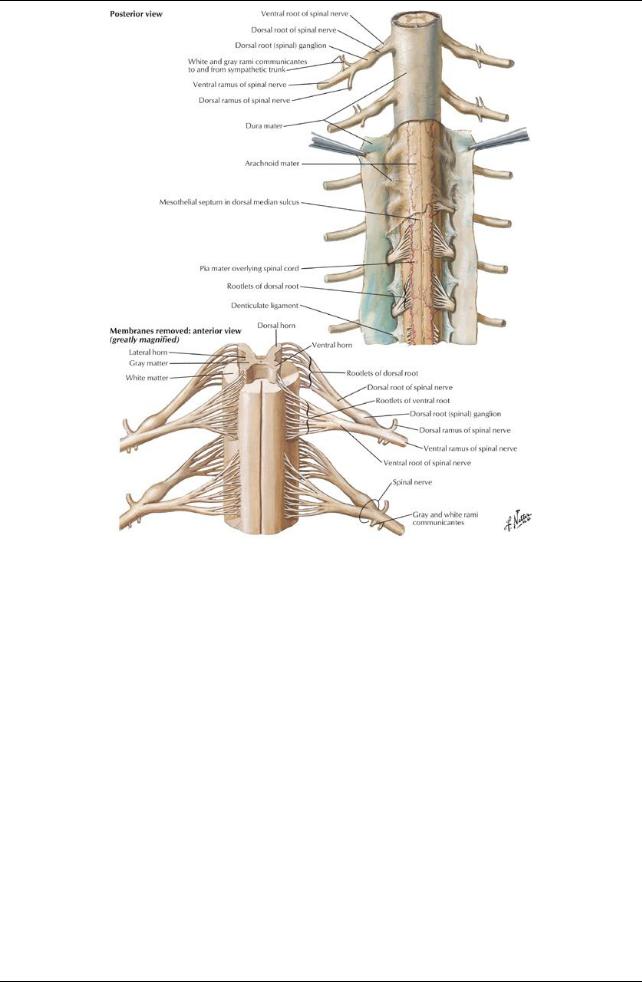
[Plate 162, Spinal Membranes and Nerve Roots]
118 / 425
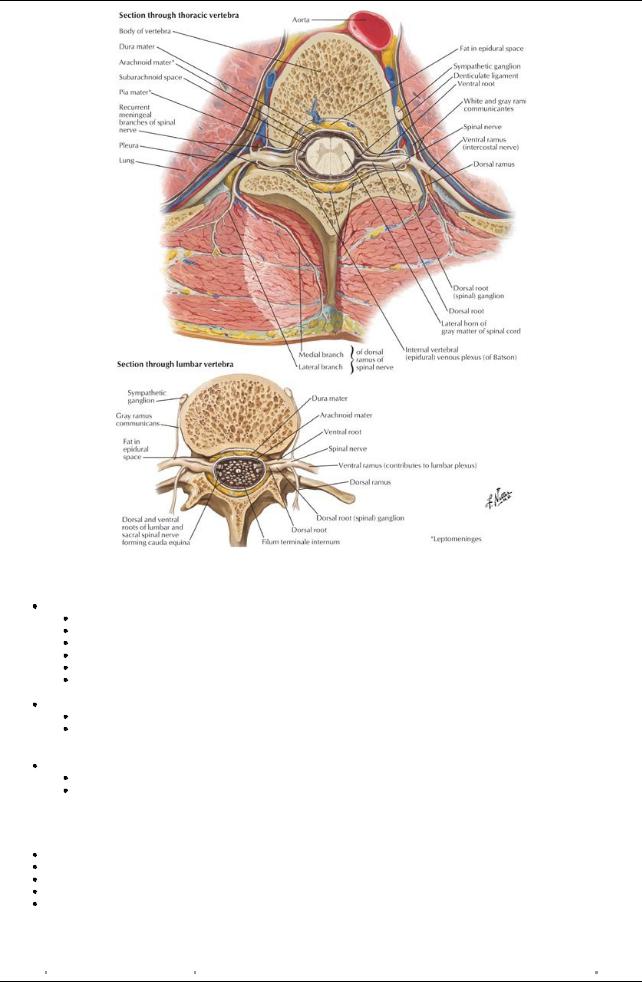
[Plate 163, Spinal Nerve Origin: Cross Sections]
Meninges
Dura mater: Tough fibroelastic membrane
Is continuous with the inner (meningeal) layer of the cranial dura
Attached to the margins of the foramen magnum and posterior longitudinal ligament
Separated bythe epidural space from vertebral periosteum
Extends as a sac from the margin of the foremen magnum to the level of S2
Pierced byspinal nerves
Anchored to the coccyxbythe external filum terminale
 Forms dural root sleeves covering the spinal nerves before fusing with the epineurium Arachnoid mater: Delicate, avascular, fibroelastic membrane lining dural sac
Forms dural root sleeves covering the spinal nerves before fusing with the epineurium Arachnoid mater: Delicate, avascular, fibroelastic membrane lining dural sac
Opposed (held to inner surface) to dura byCSF pressure
Is external to the subarachnoid space, between arachnoid and pia, containing CSF, traversed bystrands of connective tissue (arachnoid trabeculae)
 Contains the lumbar cistern, an enlargement of subarachnoid space between L2 (end of spinal cord) and S2 (end of dural sac) Pia mater: Highlyvascular innermost layer covering roots of spinal nerves
Contains the lumbar cistern, an enlargement of subarachnoid space between L2 (end of spinal cord) and S2 (end of dural sac) Pia mater: Highlyvascular innermost layer covering roots of spinal nerves
Continues as the filum terminale
Suspends the spinal cord within the dural sac bylateral extensions between the anterior and posterior roots, called denticulate ligaments
Dermatomes: a well-defined strip of skin extending from the anterior to the posterior midline, supplied bya single spinal nerve
Cervical supplyneck and upper limb
Thoracic supplytrunk (T1 also supplies upper limb)
C5 abuts T1 on the superior anterior chest wall
Lumbar predominantlysupplyanterior lower limb
Sacral predominantlysupplyposterior lower limb
Level |
Somatic Supply |
C5 |
Clavicles |
T4 |
Nipples |
119 / 425
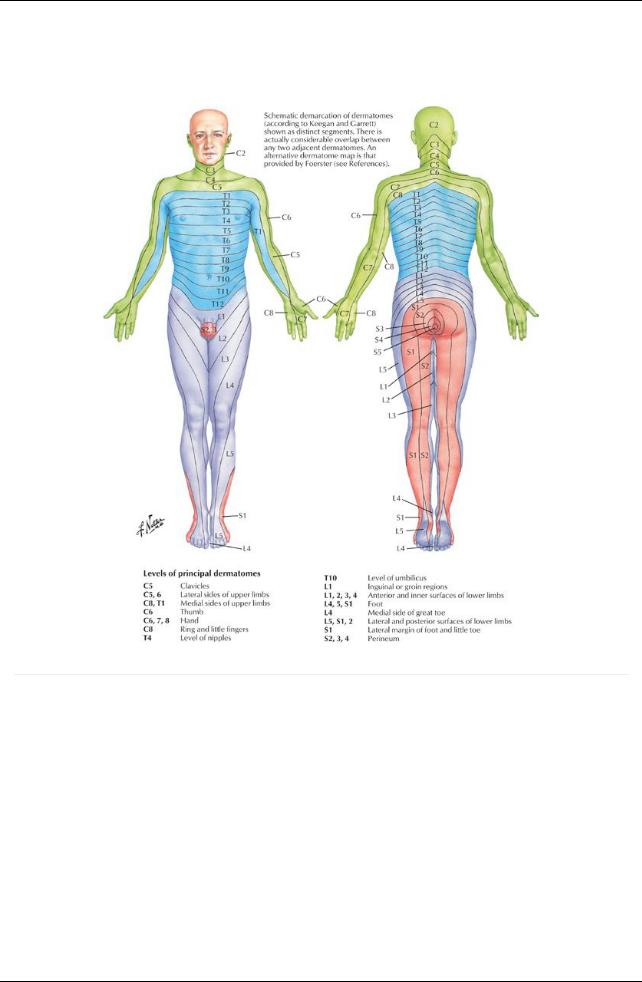
T10 |
Level of umbilicus |
L1 |
Inguinal ligament |
L3/4 |
Over the knee |
S2-S4 |
Perineum |
Dermatome levels to know:
[Plate 159, Dermatomes]
page 90
page 91
Vasculature of Spinal Cord and Vertebral Column
120 / 425
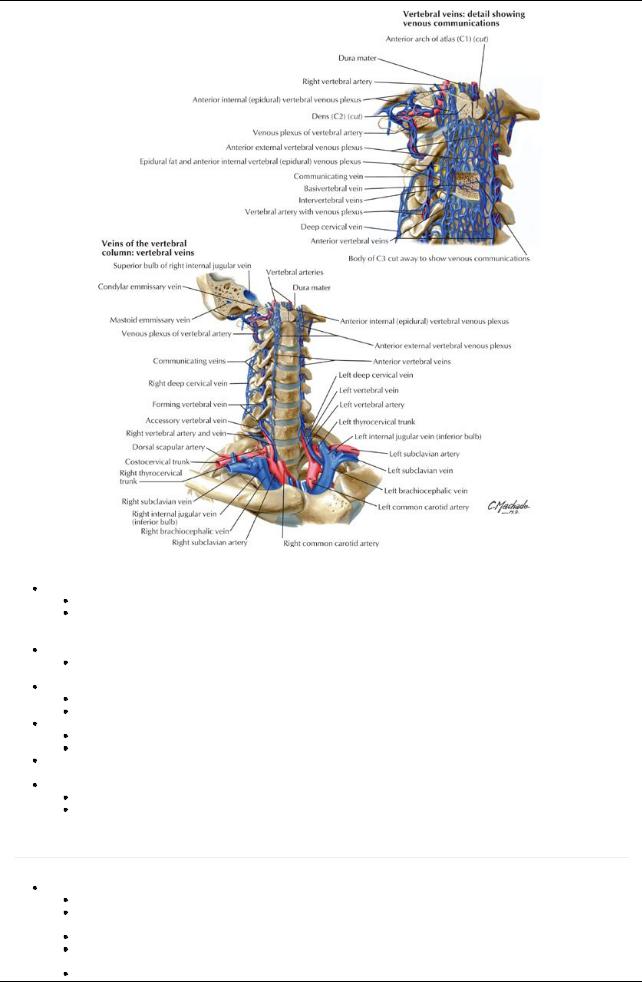
[Plate 167, Veins of the Vertebral Column: Vertebral Veins]
Anterior spinal artery
Is a single arteryrunning in ventromedian fissure
Arising from branches of the vertebral arteries (with contributions from the ascending cervical, deep cervical, intercostal, lumbar, and sacral arteries)
 Supplies the anterior two thirds of the spinal cord and vertebral bodies Posterior spinal arteries
Supplies the anterior two thirds of the spinal cord and vertebral bodies Posterior spinal arteries
Are paired, longitudinal arteries arising from vertebral or posterior inferior cerebellar arteries
 Supplyposterior one third of the spinal cord and vertebral bodies Radicular arteries
Supplyposterior one third of the spinal cord and vertebral bodies Radicular arteries
Are dorsal and ventral arteries arising from ascending cervical, deep cervical, intercostal, lumbar, and sacral arteries
Supplythe nerve roots (called segmental arteries if they reach the anterior or posterior spinal arteries)
Great anterior segmental artery(ofAdamkiewicz)
Occurs on the left side in 65% of individuals
Contributes to two thirds of the circulation to the inferior spinal cord
Veins: Usually3 anterior and 3 posterior longitudinal spinal veins with tributaries from the posterior medullaryand radicular veins. They drain into the valveless vertebral venous plexus.
Vertebral venous plexus is continuous with the cranial dural venous sinuses and contains no valves
Internal vertebral plexus (lying in the extradural space) drains the spinal cord External vertebral plexus connects with azygos vein, superior and inferior vena cavae
Autonomic Nervous System (ANS)
page 91 page 92
Sympathetic NS: catabolic system for fight or flight
T1-L2/3 (thoracolumbar) levels
Presynaptic (preganglionic) neurons have cell bodies located in the intermediolateral cell columns of the spinal cord (T1-L2 only) and utilize acetylcholine (Ach) as their neurotransmitter and synapse in paraor prevertebral ganglia
Postsynaptic (postganglionic) neurons have cell bodies in the paravertebral and prevertebral ganglia
Paravertebral ganglia linked to form right and left sympathetic chains (superior, middle and inferior cervical ganglia, T1-S5, ganglion impar)
Paravertebral ganglia attached to spinal nerves bywhite (T1-L2) and grey(C1-Co) rami communicantes
121 / 425
Long postsynaptic neurons utilize norepinephrine as their neurotransmitter
Prevertebral ganglia (celiac, superior, and inferior mesenteric, aorticorenal) are in plexuses surrounding the origins of the main branches of the abdominal aorta
Splanchnic nerves are presynaptic fibers that pass through the paravertebral ganglia without synapsing to enter cardiac, pulmonary, esophageal, various abdominal and pelvic plexuses, where theysynapse
 Sympathetic fibers innervate smooth muscle, modified cardiac muscle, glands, and medulla of suprarenal glands Parasympathetic NS: anabolic system for homeostasis
Sympathetic fibers innervate smooth muscle, modified cardiac muscle, glands, and medulla of suprarenal glands Parasympathetic NS: anabolic system for homeostasis
S2-S4 levels and cranial nerves III, VII, IX, X(craniosacral)
Long presynaptic neurons (Ach) with cell bodies in the mediolateral greymatter (S2-S4)
Short postsynaptic neurons arising near target organs (Ach)
 Innervation of smooth muscle, modified cardiac muscle, and glands of thoracic, abdominal, and pelvic viscera Visceral afferent NS: provides sensoryinput from the body's internal environment
Innervation of smooth muscle, modified cardiac muscle, and glands of thoracic, abdominal, and pelvic viscera Visceral afferent NS: provides sensoryinput from the body's internal environment
Provides visceral sensation
Can trigger both somatic and visceral reflexes
122 / 425
