
- •Preface to the 3rd edition
- •General Pharmacology
- •Systems Pharmacology
- •Therapy of Selected Diseases
- •Subject Index
- •Abbreviations
- •General Pharmacology
- •History of Pharmacology
- •Drug and Active Principle
- •The Aims of Isolating Active Principles
- •European Plants as Sources of Effective Medicines
- •Drug Development
- •Congeneric Drugs and Name Diversity
- •Oral Dosage Forms
- •Drug Administration by Inhalation
- •Dermatological Agents
- •From Application to Distribution in the Body
- •Potential Targets of Drug Action
- •External Barriers of the Body
- •Blood–Tissue Barriers
- •Membrane Permeation
- •Binding to Plasma Proteins
- •The Liver as an Excretory Organ
- •Biotransformation of Drugs
- •Drug Metabolism by Cytochrome P450
- •The Kidney as an Excretory Organ
- •Presystemic Elimination
- •Drug Concentration in the Body as a Function of Time—First Order (Exponential) Rate Processes
- •Time Course of Drug Concentration in Plasma
- •Time Course of Drug Plasma Levels during Repeated Dosing (A)
- •Time Course of Drug Plasma Levels during Irregular Intake (B)
- •Accumulation: Dose, Dose Interval, and Plasma Level Fluctuation (A)
- •Dose–Response Relationship
- •Concentration–Effect Curves (B)
- •Concentration–Binding Curves
- •Types of Binding Forces
- •Agonists—Antagonists
- •Other Forms of Antagonism
- •Enantioselectivity of Drug Action
- •Receptor Types
- •Undesirable Drug Effects, Side Effects
- •Drug Allergy
- •Cutaneous Reactions
- •Drug Toxicity in Pregnancy and Lactation
- •Pharmacogenetics
- •Placebo (A)
- •Systems Pharmacology
- •Sympathetic Nervous System
- •Structure of the Sympathetic Nervous System
- •Adrenergic Synapse
- •Adrenoceptor Subtypes and Catecholamine Actions
- •Smooth Muscle Effects
- •Cardiostimulation
- •Metabolic Effects
- •Structure–Activity Relationships of Sympathomimetics
- •Indirect Sympathomimetics
- •Types of
- •Antiadrenergics
- •Parasympathetic Nervous System
- •Cholinergic Synapse
- •Parasympathomimetics
- •Parasympatholytics
- •Actions of Nicotine
- •Localization of Nicotinic ACh Receptors
- •Effects of Nicotine on Body Function
- •Aids for Smoking Cessation
- •Consequences of Tobacco Smoking
- •Dopamine
- •Histamine Effects and Their Pharmacological Properties
- •Serotonin
- •Vasodilators—Overview
- •Organic Nitrates
- •Calcium Antagonists
- •ACE Inhibitors
- •Drugs Used to Influence Smooth Muscle Organs
- •Cardiac Drugs
- •Cardiac Glycosides
- •Antiarrhythmic Drugs
- •Iron Compounds
- •Prophylaxis and Therapy of Thromboses
- •Possibilities for Interference (B)
- •Heparin (A)
- •Hirudin and Derivatives (B)
- •Fibrinolytics
- •Intra-arterial Thrombus Formation (A)
- •Formation, Activation, and Aggregation of Platelets (B)
- •Inhibitors of Platelet Aggregation (A)
- •Presystemic Effect of ASA
- •Plasma Volume Expanders
- •Lipid-lowering Agents
- •Diuretics—An Overview
- •NaCl Reabsorption in the Kidney (A)
- •Aquaporins (AQP)
- •Osmotic Diuretics (B)
- •Diuretics of the Sulfonamide Type
- •Potassium-sparing Diuretics (A)
- •Vasopressin and Derivatives (B)
- •Drugs for Gastric and Duodenal Ulcers
- •Laxatives
- •Antidiarrheal Agents
- •Drugs Affecting Motor Function
- •Muscle Relaxants
- •Nondepolarizing Muscle Relaxants
- •Depolarizing Muscle Relaxants
- •Antiparkinsonian Drugs
- •Antiepileptics
- •Pain Mechanisms and Pathways
- •Eicosanoids
- •Antipyretic Analgesics
- •Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
- •Cyclooxygenase (COX) Inhibitors
- •Local Anesthetics
- •Opioid Analgesics—Morphine Type
- •General Anesthesia and General Anesthetic Drugs
- •Inhalational Anesthetics
- •Injectable Anesthetics
- •Sedatives, Hypnotics
- •Benzodiazepines
- •Pharmacokinetics of Benzodiazepines
- •Therapy of Depressive Illness
- •Mania
- •Therapy of Schizophrenia
- •Psychotomimetics (Psychedelics, Hallucinogens)
- •Hypothalamic and Hypophyseal Hormones
- •Thyroid Hormone Therapy
- •Glucocorticoid Therapy
- •Follicular Growth and Ovulation, Estrogen and Progestin Production
- •Oral Contraceptives
- •Antiestrogen and Antiprogestin Active Principles
- •Aromatase Inhibitors
- •Insulin Formulations
- •Treatment of Insulin-dependent Diabetes Mellitus
- •Treatment of Maturity-Onset (Type II) Diabetes Mellitus
- •Oral Antidiabetics
- •Drugs for Maintaining Calcium Homeostasis
- •Drugs for Treating Bacterial Infections
- •Inhibitors of Cell Wall Synthesis
- •Inhibitors of Tetrahydrofolate Synthesis
- •Inhibitors of DNA Function
- •Inhibitors of Protein Synthesis
- •Drugs for Treating Mycobacterial Infections
- •Drugs Used in the Treatment of Fungal Infections
- •Chemotherapy of Viral Infections
- •Drugs for the Treatment of AIDS
- •Drugs for Treating Endoparasitic and Ectoparasitic Infestations
- •Antimalarials
- •Other Tropical Diseases
- •Chemotherapy of Malignant Tumors
- •Targeting of Antineoplastic Drug Action (A)
- •Mechanisms of Resistance to Cytostatics (B)
- •Inhibition of Immune Responses
- •Antidotes and Treatment of Poisonings
- •Therapy of Selected Diseases
- •Hypertension
- •Angina Pectoris
- •Antianginal Drugs
- •Acute Coronary Syndrome— Myocardial Infarction
- •Congestive Heart Failure
- •Hypotension
- •Gout
- •Obesity—Sequelae and Therapeutic Approaches
- •Osteoporosis
- •Rheumatoid Arthritis
- •Migraine
- •Common Cold
- •Bronchial Asthma
- •Emesis
- •Alcohol Abuse
- •Local Treatment of Glaucoma
- •Further Reading
- •Further Reading
- •Picture Credits
- •Drug Indexes

230 Psychopharmacologicals
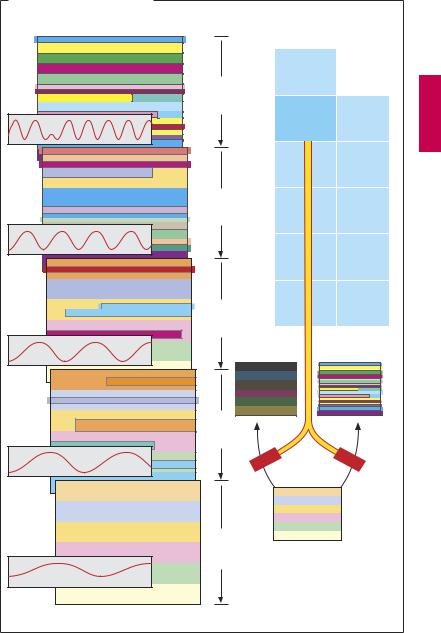
Mania
The manic phase is characterized by exaggerated elation, flight of ideas, and a pathologically increased psychomotor drive. This is symbolically illustrated in (A) by a disjointed structure and aggressive color tones. The patients are overconfident, continuously active, show progressive incoherence of thought and loosening of associations, and act irresponsibly (financially, sexually, etc.).
Lithium. Lithium is the lightest of the alkali metal atoms (A), of which family sodium and potassium have special significance for the organism. Lithium ions (Li+) distribute nearly evenly in the extracellular and intracellular fluid compartments and thus build up only a small concentration gradient across the cell membrane. The lithium ion cannot be transported by the membranal Na+/K+-ATPase. Intracellularly, lithium ions interfere in transduction mechanisms. For instance, they reduce the hydrolysis of inositol phosphate, leading to a reduced sensitivity to transmitter of nerve cells. In addition, the metabolism of transmitters is thought to be altered in the presence of lithium ions. These and other biochemical findings observed after administration of lithium do not provide a satisfactory explanation for the therapeutic effect of this “simple” pharmaceutical, particularly so because the somatic disturbance underlying mania remains unknown. As in endogenous depression, it is surmised that imbalances between different transmitter systems are at fault. Remarkably, Li+ ions do not exert psychotropic effects in healthy humans, although they elicit the typical adverse effects.
Indications for lithium therapy.
1.Acute treatment of manic phase; therapeutic response develops only in the course of several days (A).
2.Long-term administration (6–12 months until full effect reached) for the prophy-
laxis of both manic and depressive phases of bipolar illness (A).
3.Adjunctive therapy in severe therapy-re- sistant depressions.
Lithium therapy of acute mania is dif cult because of the narrow margin of safety and because the patient being treated lacks insight. Therapeutic levels should be closely monitored and kept between 0.8 and 1.2 mM in fasting morning blood samples. For prevention of relapse, slightly lower blood levels of 0.6–0.8 mM are recommended. Adverse effects that occur at therapeutic serum concentration during longterm intake of lithium salts include renal (diabetes insipidus) and endocrine manifes-
tations |
(goiter and/or |
hypothyroidism, |
|
glucose |
intolerance, |
hyperparathyroidism, |
|
sexual |
dysfunction). |
At |
concentrations |
> 1.2–1.5 mM, signs of mild toxicity are evident, including a fine hand tremor, weakness, fatigue, and abdominal complaints. As blood levels rise further, decreased ability to concentrate, agitation, confusion, and cerebellar signs are noted. In the most severe cases of poisoning, seizures may occur and the patient may lapse into a comatose state. During lithium therapy, fluctuations in blood level are quasi expected because changes in dietary daily intake of NaCl or fluid losses (diarrhea, diuretics) can markedlyalter renal elimination of lithium. Lithium therapy thus requires special diligence on the part of the physician and cooperation on the part of the patient or his or her relatives.
Luellmann, Color Atlas of Pharmacology © 2005 Thieme
All rights reserved. Usage subject to terms and conditions of license.
Therapy of Manic States |
231 |
A. Effect of lithium salts in mania |
|
|
|
Mania |
|
H |
|
|
|
|
|
|
Day 2 |
Li+ |
Be |
|
|
||
|
|
Lithium |
|
|
|
Na |
Mg |
|
4 |
K |
Ca |
|
Day |
|
|
|
|
Rb |
Sr |
|
|
Cs |
Ba |
|
Day 6 |
|
|
|
|
Depression |
Mania |
|
Day 8 |
|
|
Normal state |
Day10 |
Normal state |
|
|
|
||
Normal drive |
|
|
|
Luellmann, Color Atlas of Pharmacology © 2005 Thieme
All rights reserved. Usage subject to terms and conditions of license.

232 Psychopharmacologicals
Therapy of Schizophrenia
Schizophrenia is an endogenous psychosis of episodic character; in most cases, recovery is incomplete (residual defects, burned-out end stage). The different forms of schizophrenic illness will not be considered here. From a therapeutic perspective, it is relevant to differentiate between
Positive signs including delusions, hallucinations, disorganized speech, behavior disturbance; and
Negative signs, such as social isolation, affective flattening, avolition, poverty of speech, and anhedonia
since both symptom complexes respond differently to antipsychotic drugs.
Neuroleptics
After neuroleptic treatment of a psychotic episode is initiated, the antipsychotic effect proper manifests following a latent period. Acutely, psychomotor damping with anxiolysis and distancing is noted. Tormenting paranoid ideas and hallucinations lose their subjective importance (A, dimming of flashy colors); initially, however, the psychotic process persists but then wanes gradually over the course of several weeks.
Complete normalization often cannot be achieved. Even though a “cure” is unrealizable, these changes signify success because
(a)thepatientobtainsrelieffromthetorment of psychotic personality changes; (b) care of the patient is facilitated; and (c) return into a familiar community environment is accelerated. Neuroleptic therapy utilizes different drugclasses,namelyphenothiazines,butyrophenones, and the atypical neuroleptics.
The phenothiazines were developed from the H1-antihistamine promethazine: prototype chlorpromazine and congeners with a tricyclic ring system and a side chain containing a protonatable nitrogen atom. Phenothiazines exhibit af nity for various receptors and exert corresponding antagonistic actions. Blockade of dopamine receptors, specifically in the mesolimbic prefron-
tal system, appears important for the antipsychotic effect. The latency of the antipsychotic effect suggests that adaptive processes induced by receptor blockade play a role in the therapeutic response. Besides af nity for D2 dopamine receptors, neuroleptics also exhibit varying af nity to other receptors, including M-ACh receptors, α1- adrenoceptors, and histamine H1 and 5-HT receptors. Antagonism at these receptors contributes to the adverse effects. Af nity profiles of “classical” neuroleptics (phenothiazine and butyrophenone derivatives) differ significantlyfromthose ofnewer atypical drugs (see p.235B), in which af nity for 5-HT receptors predominates.
Neuroleptics do not have anticonvulsant activity. Because they inhibit the thermoregulatory center, neuroleptics can be employed for controlled hypothermia (“artificial hibernation”).
Chronicuseofneurolepticscanonoccasion give rise to hepatic damage associated with cholestasis. A very rare, but dramatic, adverse effect is the malignant neuroleptic syndrome (skeletal muscle rigidity, hyperthermia, stupor), which can have a fatal outcome in the absence of intensive countermeasures (including treatment with dantrolene).
With other phenothiazines (e.g., fluphenazine with a piperazine side chain substituent), antagonism at other receptor types tends to recede into the background vis-à- vis the blockade of D2 dopamine receptors. In panel (B) on p.235 the D2 receptor af nity of the drugs concerned is defined as ++, while the differences in absolute af nity for the other receptors are ignored.
The butyrophenones (prototype haloperidol) were introduced after the phenothiazines. With these agents, blockade of D2 receptors predominates entirely (p.235B). Antimuscarinic and antiadrenergic effects are attenuated. The “extrapyramidal” motor disturbances that result from D2 receptor blockade are, however, preserved and constitute the clinically most important adverse reactions that often limit therapy.
Luellmann, Color Atlas of Pharmacology © 2005 Thieme
All rights reserved. Usage subject to terms and conditions of license.

Therapy of Schizophrenia |
233 |
A. Effects of neuroleptics in schizophrenia |
|
|
|
|
|
|
|
|
|
Neuroleptics |
|
|
|
|
|||
therapy |
|
S |
|
Phenothiazine type: |
|
|||
|
|
|
Chlorpromazine |
|
||||
|
|
|
|
|
||||
|
N |
|
Cl |
CH3 |
|
|
||
of |
|
|
|
|
||||
|
H2C |
CH2 |
CH2 |
N |
|
|
||
Week 3 after start |
|
|
|
|||||
|
|
|
|
CH3 |
|
|
||
|
Desired |
|
|
Undesired effect |
|
|||
|
|
|
|
|
||||
|
|
|
Antipsychotic effect |
|
|
|||
|
|
|
D2 |
|
Prolactin |
|
|
|
5 |
D2 |
Dyskinesias |
Sedation |
H1 |
||||
Week |
||||||||
|
|
|
|
Antiemetic |
D2 |
|||
|
M |
Glaucoma |
||||||
|
|
M |
Inhibition of salivary |
|
||||
|
|
secretion |
|
|
||||
|
|
|
|
|
|
|||
7 |
|
|
α |
1 |
Hypotension |
|
|
|
Week |
|
|
|
|
||||
|
M |
|
Tachycardia |
|
|
|||
|
|
|
|
|
||||
|
|
|
|
Arrhythmia |
|
|
||
|
|
|
|
Cholestasis |
|
|
||
9 |
|
|
|
|
|
|
|
|
Week |
|
|
M |
Bowel atonia |
|
|
||
|
|
|
|
|
|
|
||
|
|
M |
|
Disturbance of |
|
|
||
|
|
|
micturition |
|
|
|||
|
|
|
|
|
|
|||
|
|
Butyrophenone type: |
|
|
||||
|
|
|
Antipsychotic effect |
|
|
|||
|
|
D2 |
Dyskinesias |
|
|
|||
|
|
|
|
Antiemetic |
D2 |
|
||
Luellmann, Color Atlas of Pharmacology © 2005 Thieme
All rights reserved. Usage subject to terms and conditions of license.

234 Psychopharmacologicals
Early dyskinesias occur immediately after neuroleptization and are manifested by involuntary abnormal movements in the head neck and shoulder region. After treatment of several weeks to months, a parkinsonian syndrome (pseudoparkinsonism) (p.188) or akathisia (motor restlessness) may develop. All these disturbances can be treated by administration of antiparkinsonian drugs of the anticholinergic type, such as biperiden. As a rule, these disturbances disappear after withdrawal of neuroleptic medication. Tardive dyskinesia may become evident after chronic neuroleptization for several years, particularly when the drug is discontinued. Its postulated cause is a hypersensitivity of the dopamine receptor system. The condition is exacerbated by administration of anticholinergics.
The butyrophenones carry an increased risk of adverse motor reactions because they lack anticholinergic activity and, hence, are prone to upset the balance between striatal cholinergic and dopaminergic activity.
Atypical neuroleptics differ in structure and pharmacological properties from the aforementioned drug groups. Extrapyramidal motor reactions are absent or less prevalent. The antipsychotic effect involves not only the positive but also the negative symptoms. In the case of clozapine, it was assumed at first that the drug acted as a selective antagonist at D4 dopamine receptors. Subsequently, however, the drug was recognized as a high-af nity ligand and antagonist at other receptors (B). Clozapine can be used when other neuroleptics have to be discontinued because of extrapyramidal motor reactions. Clozapine may cause agranulocytosis, necessitating close hematological monitoring. It produces marked sedation.
Olanzapine is structurally related to clozapine; thus far the risk of agranulocytosis appears to be low or absent.
Risperidone differs in structure from the aforementioned drugs; it possesses relatively lower af nity for all “non–D2-recep-
tors.” Ziprasidone shows high af nity for 5- HT2A receptors. Remarkably, this new substance also stimulates 5-HT1A receptors, which translates into an antidepressant effect. Ziprasidone particularly influences negative symptoms, its effect on positive symptoms reportedly being equivalent to that of classical neuroleptics. Adverse effects due to blockade of M-ACh, H1 and α1-receptors are comparatively weak. Central disturbances (giddiness, ataxia, etc.) mayoccur. Moreover, QT interval prolongation has been observed; concurrent administration of QT-prolonging drugs must therefore be avoided.
Uses. Managementofacute psychoticphases requires high-potency neuroleptics. In highly agitated patients, i.v. injection of haloperidol may be necessary. The earlier therapy is started, the better is the clinical outcome. Most schizophrenic patients require maintenance therapyfor which alowdosage can be selected. For stabilizationandprevention of relapse, atypical neuroleptics are especially suited since they improve negative symptoms in responsive patients. The patients need good care and, if possible, integration into a suitable milieu. Dif culties arise because patients do not take their prescribed medication (N.B.: counseling of both patient and caregivers). To circumvent lack ofcompliance, depot preparationshave been developed, e.g., fluphenazine decanoate (i.m. every 2 weeks) and haloperidol decanoate (i.m. every 4 weeks), which yield stable blood levels for the period indicated.
Luellmann, Color Atlas of Pharmacology © 2005 Thieme
All rights reserved. Usage subject to terms and conditions of license.

Therapy of Schizophrenia |
235 |
A. Conventional and atypical neuroleptics |
|
|
|
|
|
|
|
Positive symptoms |
|
Negative symptoms |
|
||
|
– Hallucinations |
Schizophrenia |
– Avolition |
|
|
|
|
|
|
|
|||
|
– Delusions |
|
– Affective flattening |
|
||
|
– Disorganized |
|
– Social isolation |
|
||
|
thoughts |
|
|
|
|
|
Butyrophenone derivative |
H |
|
H |
|
|
|
|
|
|
|
|
||
|
OH |
N |
|
N |
S |
CH3 |
|
|
|
|
|
||
|
Cl |
|
|
|
|
|
O |
|
|
|
|
|
|
|
N |
|
N |
|
|
|
|
N |
|
|
|
||
|
|
N |
|
N |
|
|
|
Cl |
|
|
|
|
|
F |
|
|
N |
|
N |
|
Haloperidol |
|
CH3 |
|
CH3 |
||
|
|
Clozapine |
Olanzapine |
|
||
Phenothiazine derivative |
|
|
|
|
|
|
S |
|
N |
CH3 |
|
|
|
|
|
|
|
|
|
|
N |
|
N |
N |
|
|
|
CF3 |
|
|
|
|
||
O |
|
|
|
|
||
|
N |
|
|
|
|
|
|
|
|
|
F |
|
|
|
N |
|
|
N |
|
|
|
|
|
|
|
||
|
OH |
|
|
O |
|
|
Fluphenazine |
|
Risperidone |
|
|
||
B. Receptor affinity profile with reference to D2-dopamine receptor
|
D2 |
MACh |
α 1 |
H1 |
5-HT2A |
5-HT1A |
||||
|
|
|
|
|
|
|
|
|
|
|
Chlorpromazine |
++ |
+ |
+++ |
++ |
+++ |
|
|
|
||
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
Fluphenazine |
++ |
|
|
|
+ |
+ |
+ |
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
Haloperidol |
++ |
+ |
+ |
+ |
+ |
|
|
|
||
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
Clozapine |
++ |
+++ |
+++ |
+++ |
+++ |
|
|
|
||
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
Olanzapine |
++ |
++ |
++ |
+++ |
+++ |
|
|
|
||
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
Risperidone |
++ |
|
|
|
++ |
++ |
++ |
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
Ziprasidone |
++ |
+ |
+ |
+ |
+++ |
!++! |
||||
|
|
|
|
|
|
|
|
|
|
|
The receptor affinities of each drug are compared in relation to its D2-receptor affinity, arbitrarily set at (++); antagonistic effects, except for ziprasidone (5-HT1A agonism)
Luellmann, Color Atlas of Pharmacology © 2005 Thieme
All rights reserved. Usage subject to terms and conditions of license.
