
- •Preface to the 3rd edition
- •General Pharmacology
- •Systems Pharmacology
- •Therapy of Selected Diseases
- •Subject Index
- •Abbreviations
- •General Pharmacology
- •History of Pharmacology
- •Drug and Active Principle
- •The Aims of Isolating Active Principles
- •European Plants as Sources of Effective Medicines
- •Drug Development
- •Congeneric Drugs and Name Diversity
- •Oral Dosage Forms
- •Drug Administration by Inhalation
- •Dermatological Agents
- •From Application to Distribution in the Body
- •Potential Targets of Drug Action
- •External Barriers of the Body
- •Blood–Tissue Barriers
- •Membrane Permeation
- •Binding to Plasma Proteins
- •The Liver as an Excretory Organ
- •Biotransformation of Drugs
- •Drug Metabolism by Cytochrome P450
- •The Kidney as an Excretory Organ
- •Presystemic Elimination
- •Drug Concentration in the Body as a Function of Time—First Order (Exponential) Rate Processes
- •Time Course of Drug Concentration in Plasma
- •Time Course of Drug Plasma Levels during Repeated Dosing (A)
- •Time Course of Drug Plasma Levels during Irregular Intake (B)
- •Accumulation: Dose, Dose Interval, and Plasma Level Fluctuation (A)
- •Dose–Response Relationship
- •Concentration–Effect Curves (B)
- •Concentration–Binding Curves
- •Types of Binding Forces
- •Agonists—Antagonists
- •Other Forms of Antagonism
- •Enantioselectivity of Drug Action
- •Receptor Types
- •Undesirable Drug Effects, Side Effects
- •Drug Allergy
- •Cutaneous Reactions
- •Drug Toxicity in Pregnancy and Lactation
- •Pharmacogenetics
- •Placebo (A)
- •Systems Pharmacology
- •Sympathetic Nervous System
- •Structure of the Sympathetic Nervous System
- •Adrenergic Synapse
- •Adrenoceptor Subtypes and Catecholamine Actions
- •Smooth Muscle Effects
- •Cardiostimulation
- •Metabolic Effects
- •Structure–Activity Relationships of Sympathomimetics
- •Indirect Sympathomimetics
- •Types of
- •Antiadrenergics
- •Parasympathetic Nervous System
- •Cholinergic Synapse
- •Parasympathomimetics
- •Parasympatholytics
- •Actions of Nicotine
- •Localization of Nicotinic ACh Receptors
- •Effects of Nicotine on Body Function
- •Aids for Smoking Cessation
- •Consequences of Tobacco Smoking
- •Dopamine
- •Histamine Effects and Their Pharmacological Properties
- •Serotonin
- •Vasodilators—Overview
- •Organic Nitrates
- •Calcium Antagonists
- •ACE Inhibitors
- •Drugs Used to Influence Smooth Muscle Organs
- •Cardiac Drugs
- •Cardiac Glycosides
- •Antiarrhythmic Drugs
- •Iron Compounds
- •Prophylaxis and Therapy of Thromboses
- •Possibilities for Interference (B)
- •Heparin (A)
- •Hirudin and Derivatives (B)
- •Fibrinolytics
- •Intra-arterial Thrombus Formation (A)
- •Formation, Activation, and Aggregation of Platelets (B)
- •Inhibitors of Platelet Aggregation (A)
- •Presystemic Effect of ASA
- •Plasma Volume Expanders
- •Lipid-lowering Agents
- •Diuretics—An Overview
- •NaCl Reabsorption in the Kidney (A)
- •Aquaporins (AQP)
- •Osmotic Diuretics (B)
- •Diuretics of the Sulfonamide Type
- •Potassium-sparing Diuretics (A)
- •Vasopressin and Derivatives (B)
- •Drugs for Gastric and Duodenal Ulcers
- •Laxatives
- •Antidiarrheal Agents
- •Drugs Affecting Motor Function
- •Muscle Relaxants
- •Nondepolarizing Muscle Relaxants
- •Depolarizing Muscle Relaxants
- •Antiparkinsonian Drugs
- •Antiepileptics
- •Pain Mechanisms and Pathways
- •Eicosanoids
- •Antipyretic Analgesics
- •Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
- •Cyclooxygenase (COX) Inhibitors
- •Local Anesthetics
- •Opioid Analgesics—Morphine Type
- •General Anesthesia and General Anesthetic Drugs
- •Inhalational Anesthetics
- •Injectable Anesthetics
- •Sedatives, Hypnotics
- •Benzodiazepines
- •Pharmacokinetics of Benzodiazepines
- •Therapy of Depressive Illness
- •Mania
- •Therapy of Schizophrenia
- •Psychotomimetics (Psychedelics, Hallucinogens)
- •Hypothalamic and Hypophyseal Hormones
- •Thyroid Hormone Therapy
- •Glucocorticoid Therapy
- •Follicular Growth and Ovulation, Estrogen and Progestin Production
- •Oral Contraceptives
- •Antiestrogen and Antiprogestin Active Principles
- •Aromatase Inhibitors
- •Insulin Formulations
- •Treatment of Insulin-dependent Diabetes Mellitus
- •Treatment of Maturity-Onset (Type II) Diabetes Mellitus
- •Oral Antidiabetics
- •Drugs for Maintaining Calcium Homeostasis
- •Drugs for Treating Bacterial Infections
- •Inhibitors of Cell Wall Synthesis
- •Inhibitors of Tetrahydrofolate Synthesis
- •Inhibitors of DNA Function
- •Inhibitors of Protein Synthesis
- •Drugs for Treating Mycobacterial Infections
- •Drugs Used in the Treatment of Fungal Infections
- •Chemotherapy of Viral Infections
- •Drugs for the Treatment of AIDS
- •Drugs for Treating Endoparasitic and Ectoparasitic Infestations
- •Antimalarials
- •Other Tropical Diseases
- •Chemotherapy of Malignant Tumors
- •Targeting of Antineoplastic Drug Action (A)
- •Mechanisms of Resistance to Cytostatics (B)
- •Inhibition of Immune Responses
- •Antidotes and Treatment of Poisonings
- •Therapy of Selected Diseases
- •Hypertension
- •Angina Pectoris
- •Antianginal Drugs
- •Acute Coronary Syndrome— Myocardial Infarction
- •Congestive Heart Failure
- •Hypotension
- •Gout
- •Obesity—Sequelae and Therapeutic Approaches
- •Osteoporosis
- •Rheumatoid Arthritis
- •Migraine
- •Common Cold
- •Bronchial Asthma
- •Emesis
- •Alcohol Abuse
- •Local Treatment of Glaucoma
- •Further Reading
- •Further Reading
- •Picture Credits
- •Drug Indexes
334 Therapy of Selected Diseases
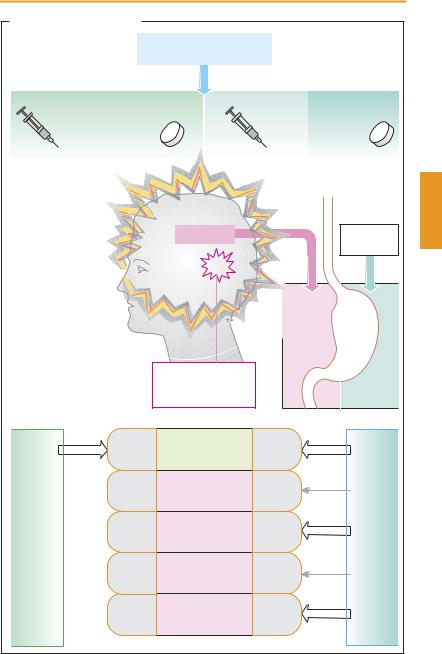
Migraine
Migraine is a syndrome characterized by recurrent attacks of intense headache and nausea that occur at irregular intervals and last for several hours. In classical migraine, the attack is typically heralded by an “aura” accompanied by spreading homonymous visual field defects with colored sharp edges (“fortification” spectra). In addition, the patient cannot focus on certain objects, has a ravenous appetite for particular foods, and is hypersensitive to odors (hyperosmia) or light (photophobia). The exact cause of these complaints is unknown; conceivably, the underlying pathogenetic mechanisms involve local release of proinflammatory mediators from nociceptive primary afferents (neurogenic inflammation) or a disturbance in cranial blood flow. In addition to an often inherited predisposition, precipitating factors are required to provoke an attack, e. g., psychic stress, lack of sleep, certain foods. Pharmacotherapy of migraine has two aims: stopping the acute attack and preventing subsequent ones.
Treatment of the attack. For symptomatic relief, headaches are treated with analgesics (acetaminophen, acetylsalicylic acid), and nausea is treated with metoclopramide (pp.116, 342) or domperidone. Since there is delayed gastric emptying during the attack, drug absorption can be markedly retarded and hence effective plasma levels are not obtained. Because metoclopramide stimulates gastric emptying, it promotes absorption of ingested analgesic drugs and thus facilitates pain relief.
If acetylsalicylic acid is administered i.v. as the lysine salt, its bioavailability is complete. Therefore, i.v. injection may be advisable in acute attacks.
Should analgesics prove insuf ciently effective, sumatriptan (prototype of the triptans) or ergotamine may help prevent an imminent attack in many cases. Both substances are effective in migraine and cluster
headaches but not in other forms of headache. The probable common mechanism of action is a stimulation of serotonin receptors of the 5-HT1D subtype. Moreover, ergotamine has af nity for dopamine receptors (†nausea, emesis), as well as α-adrenocep- tors and 5-HT2 receptors (⁄ vascular tone, ⁄ platelet aggregation). With frequent use, the vascular side effects may give rise to severe peripheral ischemia (ergotism). Paradoxically, overuse of ergotamine (> once per week) may provoke “rebound” headaches, thought to result from persistent vasodilation. Though different in character (tensiontype headache), these prompt further consumption of ergotamine. Thus, a vicious circle develops with chronic abuse of ergotamine or other analgesics that may end with irreversible disturbances of peripheral blood flow and impairment of renal function.
Administered orally, ergotamine and sumatriptan have only limited bioavailability. Dihydroergotamine may be given by i.m. or slow i.v. injection, sumatriptan subcutaneously, by nasal spray, or as a suppository. When given orally, other triptans such as zolmitriptan, naratriptan, and rizatriptan have higher bioavailability than sumatriptan.
Prophylaxis. Taken regularly over a longer period, a heterogeneous group of drugs comprising propranolol, nadolol, atenolol, and metoprolol (β-blockers), flunarizine (H1-his- tamine, dopamine, and calcium antagonist), pizotifen (pizotyline, 5-HT antagonist with structural resemblance to tricyclic antidepressants), and methysergide (partial 5-HT antagonist) may decrease the frequency, intensity, and duration of migraine attacks. The drug of first choice is one of the β-block- ers mentioned.
Luellmann, Color Atlas of Pharmacology © 2005 Thieme
All rights reserved. Usage subject to terms and conditions of license.
|
|
|
|
|
Migraine |
335 |
A: Migraine and its treatment |
|
|
|
|
|
|
|
Acetylsalicylic acid 1000 mg |
|
|
|||
|
or acetaminophen 1000 mg |
|
|
|||
When therapeutic effect inadequate |
|
|
|
|
||
Sumatriptan |
or |
(Dihydro)-Ergotamine |
|
|||
and other triptans |
|
|
|
|
|
|
6 mg |
50–100 mg |
|
|
1 mg |
1–2 mg |
|
|
|
Migraine |
|
|
|
Meto- |
|
|
|
|
|
|
clopramide |
Migraine attack: |
|
|
|
|
Gastric emptying |
|
|
|
|
|
|
||
Headache |
|
|
|
inhibited |
accelerated |
|
Hypersensitivity of |
|
|
|
|||
|
|
|
|
|
|
|
olfaction, gustation, |
|
|
|
|
|
|
audition, vision, |
|
|
|
|
|
|
nausea, vomiting |
|
|
|
|
Drug |
|
|
|
Neurogenic |
|
|
|
|
|
|
|
|
absorption |
||
|
|
inflammation, |
|
|
|
|
|
|
local edema, |
|
delayed |
improved |
|
|
|
vasodilation |
|
|
|
|
|
5-HT1B/1D |
Relief of migraine |
|
5-HT1B/1D |
|
|
Sumatriptan and other triptans |
5-HT1A |
Psychosis |
|
5-HT1A |
|
|
D2 |
Nausea, |
|
D2 |
|
Ergotamine |
|
|
vomiting |
|
|
|
||
5-HT2 |
Platelet aggregation |
5-HT2 |
|
|||
|
|
|
||||
|
α 1 + α 2 |
Vasoconstriction |
|
α 1 + α 2 |
|
|
Luellmann, Color Atlas of Pharmacology © 2005 Thieme
All rights reserved. Usage subject to terms and conditions of license.
336 Therapy of Selected Diseases
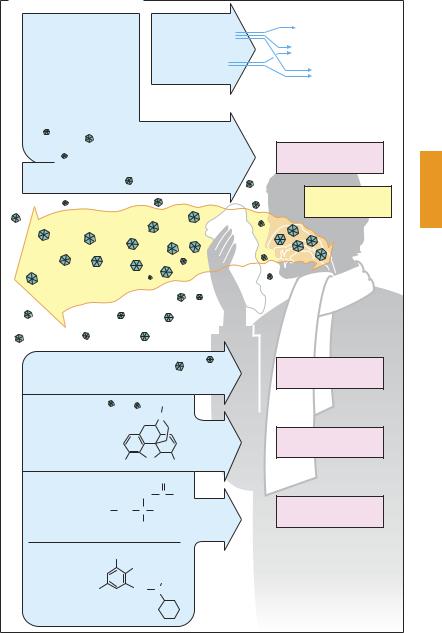
Common Cold
The common cold—colloquially the flu, catarrh, or grippe (strictly speaking the rarer infection with influenza viruses)—is an acute infectious inflammation of the upper respiratory tract. Its symptoms—sneezing, running nose (due to rhinitis), hoarseness (laryngitis), dif culty in swallowing and sore throat (pharyngitis and tonsillitis), cough associated with first serous then mucous sputum (tracheitis, bronchitis), sore muscles, and general malaise—can be present individually or concurrently in varying combination or sequence. The term stems from an old popular belief that these complaints are caused by exposure to chilling or dampness. The causative pathogensare differentviruses (rhino-, adeno-, and parainfluenza viruses) that may be transmitted by aerosol droplets produced by coughing and sneezing.
Therapeutic measures. Causal treatment with a virustatic is not possible at present. Since cold symptoms abate spontaneously, there is no compelling need to use drugs. However, conventional remedies are intended for symptomatic relief.
Rhinitis. Nasal discharge could be prevented by parasympatholytics; however, other atropine-like effects (p.108) would have to be accepted. Parasympatholytics are threfore hardly ever used, although a corresponding action is probably exploited in the case of H1-antihistaminics, an ingredient of many cold remedies. Locally applied (nasal drops), vasoconstricting α-sympatho- mimetics decongest the nasal mucosa and dry up secretions, clearing the nasal passage. Long-term use may cause damage to nasal mucous membranes (p. 94).
Sore throat, swallowing problems. Demulcent lozenges containing surface anesthetics such as lidocaine (caveat: benzocaine and tetracaine contain an allergenic p-ami- nophenyl group; p. 207) may provide shortterm relief; however, the risk of allergic reactions should be kept in mind.
Cough. Since coughing serves to expel excess tracheobronchial secretions, suppression of this physiological reflex is justified only when coughing is dangerous (after surgery) or unproductive because of absent secretions. Codeine and noscapine (p. 210) suppress cough by a central action. A different, though incompletely understood, mechanism of action is evident in antitussives such as clobutinol, which do not derive from opium. The available clinical studies concerning the benefits of antitussives in common colds do not present a convincing picture.
Mucous airway obstruction. Expectorants are meant to promote clearing of bronchial mucus by a liquefying action that involves either cleavage of mucous substances (mucolytics) or stimulation of production of watery mucus (e.g., hot beverages). Whether mucolytics are indicated in the common cold and whether expectorants such as bromohexine or ambroxole effectively lower viscosity of bronchial secretions may be questioned. In clinical studies of chronic obstructive bronchitis (but not common cold infections), N-acetylcysteine was shown to have clinical effectiveness, as evidenced by a lowered incidence of exacerbations during chronic intake.
Fever. Antipyretic analgesics (acetylsalicylic acid, acetaminophen, p.198) are indicated only when there is high fever. Fever is a natural response and useful in monitoring the clinical course of an infection.
Muscle aches and pains, headache. Antipyretic analgesics are effective in relieving these symptoms.
Luellmann, Color Atlas of Pharmacology © 2005 Thieme
All rights reserved. Usage subject to terms and conditions of license.
Common Cold |
337 |
A. Drugs used in common cold
Local use of |
Acetylsalicylic acid |
Soreness |
|
||
α -sympathomimetics |
|
Headache |
(nasal drops or spray) |
Acetaminophen |
|
|
Fever |
|
|
|
|
|
|
|
Mucosal decongestion
Nose breathing facilitated
Caution: habituation
H1-Antihistamines
Caution: sedation
Viral infection
Causal therapy impossible
Surface anesthetics
Caution:
risk of sensitization
Antitussive: |
|
|
CH3 |
|
|
|
|
|
|
|
N |
Codeine |
O |
|
|
|
H3CO |
OH |
|
|
|
||
Mucolytics |
|
|
O |
|
|
|
|
|
|
NH |
C CH3 |
|
HS CH2 |
C |
COOH |
Acetylcysteine |
H |
|
|
|
|
||
Give |
Br |
|
|
warm fluids |
|
NH2 |
|
Elderberry |
|
|
CH3 |
Br |
CH2 |
N |
|
tea |
|
|
|
Bromhexine
Sniffles, runny nose
Common cold
Flu
Sore throat
Cough
Airway congestion
Accumulation in airways of mucus, inadequate expulsion by cough
Luellmann, Color Atlas of Pharmacology © 2005 Thieme
All rights reserved. Usage subject to terms and conditions of license.
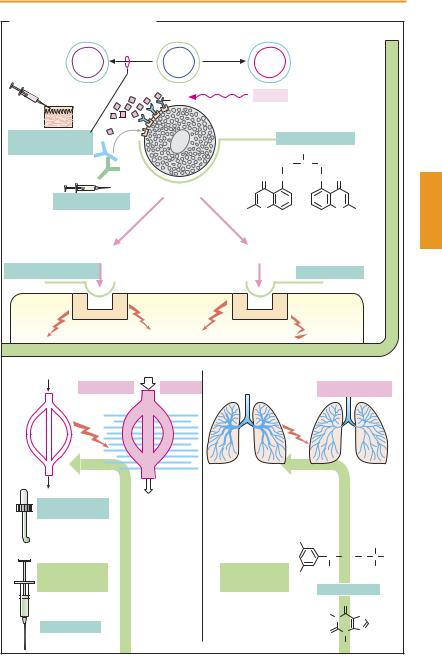
6. Functional antagonists of mediators of allergy.
a α-Sympathomimetics, such as naphazoline, oxymetazoline, and tetrahydrozoline, are applied topically to the conjunctival and nasal mucosa to produce local vasoconstriction. Their use should be shortterm at most.
b Epinephrine, given i.v., is the most important drug in the management of anaphylactic shock: it constricts blood vessels, reduces capillary permeability, and dilates bronchi.
c β2-Sympathomimetics, such as terbutaline, fenoterol, and albuterol, are employed in bronchial asthma, mostly by inhalation, and parenterally in emergencies. Even after inhalation, effective amounts can reach the systemic circulation and cause side effects (e. g., palpitations, tremulousness, restlessness, hypokalemia). The duration of action of both salmeterol and formoterol, given by inhalation, is 12 hours. These long-acting β2-mimetics are included in the treatment of severe asthma. Given at nighttime, they can prevent attacks that preferentially occur in the early morning hours.
d Theophylline belongs to the methylxanthines. Its effects are attributed to both inhibition of phosphodiesterase (cAMP increase, p. 66) and antagonism at adenosine receptors. In bronchial asthma, theophylline can be given orally for prophylaxis or parenterally to control the attack. Manifestations of overdosage include ton- ic-clonic seizures and cardiac arrhythmias (blood level monitoring).
e Glucocorticoids (p.244) have significant antiallergic activity and probably interfere with different stages of the allergic response. Indications: hay fever, bronchial asthma (preferably local application of analogues with high presystemic elimination, e.g., beclomethasone dipropionate, budesonide, flunisolide, fluticasone propionate); and anaphylactic shock (i.v. in high dosage)—a probably nongenomic action of
inducedLuellmann,bronchospasmColor Atlas. of Pharmacology © 2005immediateThieme onset.
All rights reserved. Usage subject to terms and conditions of license.
|
|
|
|
Antiallergie Therapy |
|
339 |
|||||
A. Atopy and antiallergic therapy |
|
|
|
|
|
|
|
|
|
|
|
TH1 |
|
TH0 |
|
TH2 |
|
|
|
|
|
|
|
Skin |
|
IgE |
|
Atopy |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
Anti- |
Allergen |
|
|
|
Mast cell |
|
|
|
|
||
gen |
|
|
|
|
|
|
|
||||
|
|
|
stabilization by |
|
|
||||||
|
|
|
|
|
|
|
|||||
Specific |
|
|
|
|
cromolyn |
|
|
|
|
||
immunotherapy |
|
|
|
|
|
OH |
|
|
|
|
|
IgE |
|
|
|
CH2 |
C |
CH2 |
|
|
|
Glucocorticoids |
|
|
|
|
|
O |
O |
H |
O |
O |
|
|
|
|
|
|
|
|
|
|
|||||
|
|
Mast cell |
|
|
|
|
|
|
|
|
|
Omalizumab |
|
-OOC |
O |
|
|
|
O |
COO- |
|||
|
|
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|
|
|
|
Histamine |
|
Leukotrienes |
|
|
|
|
|
|
|||
H1-Antihistaminics |
|
|
|
|
Antileukotriene, |
|
|
||||
|
|
|
|
e.g., montelukast |
|
|
|||||
|
Histamine |
|
|
Leukotriene |
|
|
|
|
|||
|
receptor |
|
|
receptor |
|
|
|
|
|||
|
Reaction of target cells |
|
|
|
|
|
|
|
|
|
|
Vascular smooth muscle, permeability |
|
Bronchial musculature |
|
|
|
||||||
Vasodilation |
Edema |
|
|
|
|
Contraction |
|
||||
|
|
|
|
|
|
|
Bronchial asthma |
|
|||
α -Sympatho- Mucous membranes |
|
|
β |
2-Sympathomimetics: |
|||||||
mimetics: |
of nose and eye: |
|
|
||||||||
e. g., |
redness, swelling, |
|
|
e. g., terbutaline |
|
||||||
naphazoline |
secretion |
|
|
|
HO |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
CH3 |
||
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
CH |
|
CH2 |
N C |
CH3 |
Vaso- |
|
|
Broncho- |
|
|
|
|
|
H |
|
|
|
|
HO |
|
OH |
|
|
CH3 |
||||
constriction |
|
|
dilation |
|
|
|
|
|
|
||
Skin: |
|
|
|
Theophylline |
|
||||||
|
|
|
|
|
|
|
|||||
|
wheal formation |
|
|
|
|
|
|
O |
H |
|
|
|
|
|
|
|
|
|
H3C |
|
|
|
|
|
|
|
|
|
|
|
|
|
N |
|
|
|
Circulation: |
|
|
|
|
|
N |
|
|
||
Epinephrine |
|
|
|
|
|
|
|
|
|||
anaphylactic shock |
|
|
|
|
O |
|
N |
N |
|
||
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
CH3 |
|
|
Luellmann, Color Atlas of Pharmacology © 2005 Thieme
All rights reserved. Usage subject to terms and conditions of license.
