
- •Preface to the 3rd edition
- •General Pharmacology
- •Systems Pharmacology
- •Therapy of Selected Diseases
- •Subject Index
- •Abbreviations
- •General Pharmacology
- •History of Pharmacology
- •Drug and Active Principle
- •The Aims of Isolating Active Principles
- •European Plants as Sources of Effective Medicines
- •Drug Development
- •Congeneric Drugs and Name Diversity
- •Oral Dosage Forms
- •Drug Administration by Inhalation
- •Dermatological Agents
- •From Application to Distribution in the Body
- •Potential Targets of Drug Action
- •External Barriers of the Body
- •Blood–Tissue Barriers
- •Membrane Permeation
- •Binding to Plasma Proteins
- •The Liver as an Excretory Organ
- •Biotransformation of Drugs
- •Drug Metabolism by Cytochrome P450
- •The Kidney as an Excretory Organ
- •Presystemic Elimination
- •Drug Concentration in the Body as a Function of Time—First Order (Exponential) Rate Processes
- •Time Course of Drug Concentration in Plasma
- •Time Course of Drug Plasma Levels during Repeated Dosing (A)
- •Time Course of Drug Plasma Levels during Irregular Intake (B)
- •Accumulation: Dose, Dose Interval, and Plasma Level Fluctuation (A)
- •Dose–Response Relationship
- •Concentration–Effect Curves (B)
- •Concentration–Binding Curves
- •Types of Binding Forces
- •Agonists—Antagonists
- •Other Forms of Antagonism
- •Enantioselectivity of Drug Action
- •Receptor Types
- •Undesirable Drug Effects, Side Effects
- •Drug Allergy
- •Cutaneous Reactions
- •Drug Toxicity in Pregnancy and Lactation
- •Pharmacogenetics
- •Placebo (A)
- •Systems Pharmacology
- •Sympathetic Nervous System
- •Structure of the Sympathetic Nervous System
- •Adrenergic Synapse
- •Adrenoceptor Subtypes and Catecholamine Actions
- •Smooth Muscle Effects
- •Cardiostimulation
- •Metabolic Effects
- •Structure–Activity Relationships of Sympathomimetics
- •Indirect Sympathomimetics
- •Types of
- •Antiadrenergics
- •Parasympathetic Nervous System
- •Cholinergic Synapse
- •Parasympathomimetics
- •Parasympatholytics
- •Actions of Nicotine
- •Localization of Nicotinic ACh Receptors
- •Effects of Nicotine on Body Function
- •Aids for Smoking Cessation
- •Consequences of Tobacco Smoking
- •Dopamine
- •Histamine Effects and Their Pharmacological Properties
- •Serotonin
- •Vasodilators—Overview
- •Organic Nitrates
- •Calcium Antagonists
- •ACE Inhibitors
- •Drugs Used to Influence Smooth Muscle Organs
- •Cardiac Drugs
- •Cardiac Glycosides
- •Antiarrhythmic Drugs
- •Iron Compounds
- •Prophylaxis and Therapy of Thromboses
- •Possibilities for Interference (B)
- •Heparin (A)
- •Hirudin and Derivatives (B)
- •Fibrinolytics
- •Intra-arterial Thrombus Formation (A)
- •Formation, Activation, and Aggregation of Platelets (B)
- •Inhibitors of Platelet Aggregation (A)
- •Presystemic Effect of ASA
- •Plasma Volume Expanders
- •Lipid-lowering Agents
- •Diuretics—An Overview
- •NaCl Reabsorption in the Kidney (A)
- •Aquaporins (AQP)
- •Osmotic Diuretics (B)
- •Diuretics of the Sulfonamide Type
- •Potassium-sparing Diuretics (A)
- •Vasopressin and Derivatives (B)
- •Drugs for Gastric and Duodenal Ulcers
- •Laxatives
- •Antidiarrheal Agents
- •Drugs Affecting Motor Function
- •Muscle Relaxants
- •Nondepolarizing Muscle Relaxants
- •Depolarizing Muscle Relaxants
- •Antiparkinsonian Drugs
- •Antiepileptics
- •Pain Mechanisms and Pathways
- •Eicosanoids
- •Antipyretic Analgesics
- •Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
- •Cyclooxygenase (COX) Inhibitors
- •Local Anesthetics
- •Opioid Analgesics—Morphine Type
- •General Anesthesia and General Anesthetic Drugs
- •Inhalational Anesthetics
- •Injectable Anesthetics
- •Sedatives, Hypnotics
- •Benzodiazepines
- •Pharmacokinetics of Benzodiazepines
- •Therapy of Depressive Illness
- •Mania
- •Therapy of Schizophrenia
- •Psychotomimetics (Psychedelics, Hallucinogens)
- •Hypothalamic and Hypophyseal Hormones
- •Thyroid Hormone Therapy
- •Glucocorticoid Therapy
- •Follicular Growth and Ovulation, Estrogen and Progestin Production
- •Oral Contraceptives
- •Antiestrogen and Antiprogestin Active Principles
- •Aromatase Inhibitors
- •Insulin Formulations
- •Treatment of Insulin-dependent Diabetes Mellitus
- •Treatment of Maturity-Onset (Type II) Diabetes Mellitus
- •Oral Antidiabetics
- •Drugs for Maintaining Calcium Homeostasis
- •Drugs for Treating Bacterial Infections
- •Inhibitors of Cell Wall Synthesis
- •Inhibitors of Tetrahydrofolate Synthesis
- •Inhibitors of DNA Function
- •Inhibitors of Protein Synthesis
- •Drugs for Treating Mycobacterial Infections
- •Drugs Used in the Treatment of Fungal Infections
- •Chemotherapy of Viral Infections
- •Drugs for the Treatment of AIDS
- •Drugs for Treating Endoparasitic and Ectoparasitic Infestations
- •Antimalarials
- •Other Tropical Diseases
- •Chemotherapy of Malignant Tumors
- •Targeting of Antineoplastic Drug Action (A)
- •Mechanisms of Resistance to Cytostatics (B)
- •Inhibition of Immune Responses
- •Antidotes and Treatment of Poisonings
- •Therapy of Selected Diseases
- •Hypertension
- •Angina Pectoris
- •Antianginal Drugs
- •Acute Coronary Syndrome— Myocardial Infarction
- •Congestive Heart Failure
- •Hypotension
- •Gout
- •Obesity—Sequelae and Therapeutic Approaches
- •Osteoporosis
- •Rheumatoid Arthritis
- •Migraine
- •Common Cold
- •Bronchial Asthma
- •Emesis
- •Alcohol Abuse
- •Local Treatment of Glaucoma
- •Further Reading
- •Further Reading
- •Picture Credits
- •Drug Indexes
340 Therapy of Selected Diseases
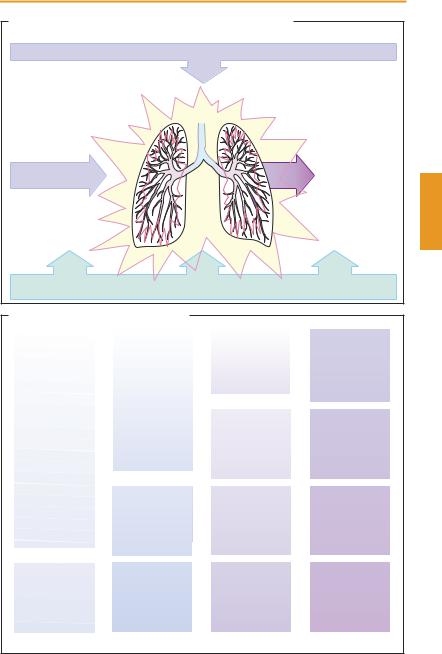
Bronchial Asthma
Definition. A recurrent, episodic shortness of breath caused by bronchoconstriction arising from airway inflammation and hyperreactivity.
Pathophysiology. One of the main pathogenetic factors is an allergic inflammation of the bronchial mucosa. For instance, leukotrienes that are formed during an IgE-medi- ated immune response (p. 72) exert a chemotactic effect on inflammatory cells. As the inflammation develops, bronchi become globally hyperreactive to spasmogenic stimuli. Thus, stimuli other than the original antigen(s) can act as triggers (A); e. g., breathing of cold air is an important trigger in exerciseinduced asthma. Cyclooxygenase inhibitors (p. 200) exemplify drugs acting as asthma triggers.
Management. Avoidance of asthma triggers is an important prophylactic measure, though not always feasible. Drugs that inhibit allergic inflammatory mechanisms or reduce bronchial hyperreactivity (glucocorticoids, “mast-cell stabilizers,” and leukotriene antagonists) attack crucial pathogenetic links. Bronchodilation is achieved by inhalation of β2-sympathomimetics (with high presystemic elimination) or, in the case of chronic obstructive lung disease, the anticholinergic, tiotropium (long-acting; single daily dose).
The step scheme (B) illustrates successive levels of pharmacotherapeutic management at increasing degrees of disease severity.
Step 1. Medications of first choice for the acute attack are short-acting, aerosolized β2- sympathomimetics, e.g., salbutamol or fenoterol. Their action occurs within minutes after inhalation and lasts for 4–6 hours.
Step 2. If β2-mimetics have to be used more frequently than once a week, more severe disease is present. At this stage, management includes anti-inflammatory drugs, preferably an inhalable glucocorticoid
(p. 246). Inhalational treatment with glucocorticoids must be administered regularly, improvement being evident only after several weeks. With proper inhalational use of glucocorticoids undergoing high presystemic elimination, concern about systemic adverse effects (“cortisone fear”) is unwarranted. Possible local adverse effects are oropharyngeal candidiasis and dysphonia. To minimize the risk of candidiasis, drug administration should occur before morning or evening meals. Alternatively, a “mast-cell stabilizer” (p.118) given by inhalation may prove adequately successful. Oral administration of timed-release theophylline (p. 338) is considered a further alternative, particularly so since the effect of theophylline is thought to possess an additional in- flammation-inhibiting component, apart from bronchodilation. The margin of safety is narrow (cardiac or CNS stimulation; plasma level controls!). A leukotriene antagonist (montelukast, p. 338) may also merit consideration.
Anti-inflammatory therapy is the more successful the less use is made of asneeded β2-mimetic medication.
Step 3. Continuous bronchodilator treatment is added to the low-dose glucocorticoid regimen. Preference is given to local use of a long-acting inhalable β2-mimetic (salmeterol or formoterol; p.338). If this proves insuf cient, the glucocorticoid dose is increased. Instead of a long-acting β2-mimetic, oral administration of timed-release theophylline, of a controlled release β2-agonist, or of a leukotriene antagonist would be possible.
Step 4. The dose of inhalable glucocorticoid is increased further. When this proves unsatisfactory, the active principles shown in (B) can be added on, including systemic administration of a glucocorticoid.
Luellmann, Color Atlas of Pharmacology © 2005 Thieme
All rights reserved. Usage subject to terms and conditions of license.
|
|
Bronchial Asthma |
341 |
A. Asthma bronchiale, pathophysiology and therapeutic approach |
|
||
|
Allergens |
|
|
|
Inflammation |
|
|
Antigens, |
Bronchial hyperreactivity |
|
|
|
|
|
|
infections, |
|
|
|
ozone, |
|
|
|
SO2, NO2 |
|
|
|
Noxious stimuli |
|
Bronchial |
|
|
spasm |
|
|
Dust, |
|
|
|
cold air, |
|
|
|
drugs |
|
|
|
Avoid |
Treat |
Dilate |
|
exposure |
inflammation |
bronchi |
|
B. Bronchial asthma treatment algorithm
Preferred substances |
|
|
|
|
|
If needed (orally): |
||
for adults |
|
|
|
|
|
|||
after: Global Strategy |
|
|
|
|
|
Glucocorticoid |
||
for Asthma Management |
|
|
|
|
|
β 2-Mimetic |
||
and Prevention 2002 |
|
|
|
|
|
|||
|
|
|
|
|
Montelukast |
|||
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
Theophylline |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
Maintained bronchodilation |
|
|
|
|
|
|
|
|
Long-acting β 2-mimetic by inhalation |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
Antiinflammatory treatment, inhalative, chronically |
|
||||
|
|
|
Glucocorticoid with high presystemic elimination |
|
||||
|
|
|
low dose |
medium dose |
high dose |
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
Bronchodilation as needed: short-acting inhalative β 2-mimetics |
|
||||||
|
< 1 x /week |
|
< 4 x/day |
|
as needed |
|||
|
|
– |
|
|||||
|
Mild asthma |
|
Moderate asthma |
|
Severe asthma |
|||
Luellmann, Color Atlas of Pharmacology © 2005 Thieme
All rights reserved. Usage subject to terms and conditions of license.
342 Therapy of Selected Diseases
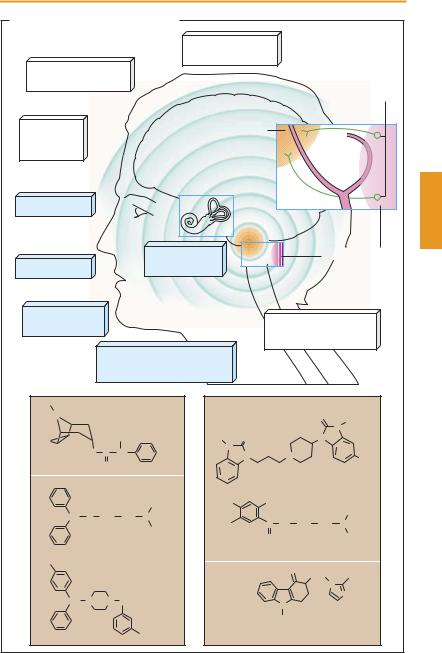
Emesis
In emesis the stomach empties in a retrograde manner. The pyloric sphincter is closed while cardia and esophagus relax to allow gastric contents to be propelled orad by a forceful synchronous contraction of abdominal wall muscles and diaphragm. Closure of the glottis and elevation of the soft palate prevent entry of vomitus into the trachea and the nasopharynx. As a rule, there is prodromal salivation or yawning. Coordination between these different stages depends on the medullary center for emesis, which can be activated by diverse stimuli. These are conveyed via the vestibular apparatus, visual, olfactory, and gustatory inputs, as well as viscerosensory afferents from the upper alimentary tract. Psychic stress may also activate the emetic center. The mechanisms underlying motion sickness (kinetosis, sea sickness) and vomiting during pregnancy are still unclear.
Polar substances cannot reach the emetic center itself because it is protected by the blood–brain barrier. However, they can indirectly excite the center by activating chemoreceptors in the area postrema or receptors on peripheral vagal nerve endings.
Antiemetic therapy. Vomiting can be a useful reaction enabling the body to eliminate an orally ingested poison. Antiemetic drugs are used to prevent kinetosis, pregnancy vomiting, cytotoxic drug-induced or postoperative vomiting, as well as vomiting due to radiation therapy.
Motion sickness. Effective prophylaxis can be achieved with the parasympatholytic scopolamine (p.110) and H1-antihistaminics (p.118) of the diphenylmethane type (e. g., diphenhydramine, meclizine). Antiemetic activity is not a property shared by all parasympatholytics or antihistaminics. The ef - cacy of the drugs mentioned depends on the actual situation of the individual (gastric filling, ethanol consumption), environmental conditions (e. g., the behavior of fellow trav-
elers), and the type of motion experienced. The drugs should be taken 30 minutes before the start of travel and repeated every 4–6 hours. Scopolamine applied transdermally through an adhesive patch 6–8 hours before travel can provide effective protection for up to 3 days.
Pregnancy vomiting is prone to occur in the first trimester; thus, pharmacotherapy would coincide with the period of maximal fetal vulnerability to chemical injury. Accordingly, antiemetics (antihistaminics, or neuroleptics if required; p. 232) should be used only when continuous vomiting threatens to disturb electrolyte and water balance to a degree that places the fetus at risk.
Drug-induced vomiting. To prevent vomiting during anticancer chemotherapy (especially, with cisplatin), effective use can be made of 5-HT3 receptor antagonists (e. g., ondansetron, granisetron, and tropisetron), alone or in combination with glucocorticoids (methylprednisolone, dexamethasone). Anticipatory nausea and vomiting, resulting from inadequately controlled nausea and emesis in patients undergoing cytotoxic chemotherapy, can be attenuated by a benzodiazepine such as lorazepam. Dopamine ag- onist-induced nausea in parkinsonian patients (p.188) can be counteracted with D2- receptor antagonists that penetrate poorly into the CNS (e. g., domperidone, sulpiride).
Metoclopramide is effective in nausea and vomiting of gastrointestinal origin (5-HT4 receptor agonism) and at high dosage also in chemotherapy- and radiation-induced sickness (low potency antagonism at 5-HT3 and D3-receptors). Phenothiazines (e. g., levomepromazine, trimeprazine, and perphenazine) or metoclopramide may suppress nausea/emesis that follows certain types of surgery or is due to opioid analgesics, gastrointestinal irritation, uremia, and diseases accompanied by elevated intracranial pressure.
The synthetic cannabinoids dronabinol and nabilone have antiemetic effects that may benefit AIDS and cancer patients.
Luellmann, Color Atlas of Pharmacology © 2005 Thieme
All rights reserved. Usage subject to terms and conditions of license.
Emesis 343
A. Emetic stimuli and antiemetic drugs
Kinetoses
e.g., sea sickness
Pregnancy
vomiting
Chemoreceptors
Emetic center
Psychogenic vomiting
Sight |
|
|
|
Vestibular |
Area postrema |
Olfaction |
system |
|
|
|
|
Taste |
|
Chemoreceptors |
|
|
(drug-induced |
|
|
vomiting) |
Intramucosal sensory nerve endings in mouth, pharynx, and stomach
H3C Parasympatholytics
N
OCH2OH
O C CH
O Scopolamine
H1-Antihistamines
CH3
CH O CH2 CH2 N
CH3
Diphenhydramine
Cl
Meclozine
CH N N CH2
CH3
|
Dopamine D2 antagonists |
|
||||
|
|
|
|
|
O |
H |
|
|
|
|
|
N |
|
|
|
|
|
|
|
|
H |
O |
|
|
|
N |
|
N |
|
|
|
|
|
|
|
N |
|
N |
|
|
Cl |
|
|
|
|
|
Domperidone |
|
H2N |
|
OCH3 |
|
|
|
|
|
|
|
|
|
|
C2H5 |
Cl |
|
C |
NH |
CH2 |
CH2 |
N |
|
|
O |
|
|
|
C2H5 |
Metoclopramide |
|
|
|
|
|
|
|
|
|
O |
|
CH2 |
CH3 |
|
|
|
|
|
||
|
|
|
|
|
N |
|
|
|
|
|
|
|
N |
Ondansetron |
|
N |
|
|
|
|
|
CH3 |
|
|
|
||
|
|
|
|
|
|
|
|
5-HT3-antagonist |
|
||||
Luellmann, Color Atlas of Pharmacology © 2005 Thieme
All rights reserved. Usage subject to terms and conditions of license.
