
- •Preface to the 3rd edition
- •General Pharmacology
- •Systems Pharmacology
- •Therapy of Selected Diseases
- •Subject Index
- •Abbreviations
- •General Pharmacology
- •History of Pharmacology
- •Drug and Active Principle
- •The Aims of Isolating Active Principles
- •European Plants as Sources of Effective Medicines
- •Drug Development
- •Congeneric Drugs and Name Diversity
- •Oral Dosage Forms
- •Drug Administration by Inhalation
- •Dermatological Agents
- •From Application to Distribution in the Body
- •Potential Targets of Drug Action
- •External Barriers of the Body
- •Blood–Tissue Barriers
- •Membrane Permeation
- •Binding to Plasma Proteins
- •The Liver as an Excretory Organ
- •Biotransformation of Drugs
- •Drug Metabolism by Cytochrome P450
- •The Kidney as an Excretory Organ
- •Presystemic Elimination
- •Drug Concentration in the Body as a Function of Time—First Order (Exponential) Rate Processes
- •Time Course of Drug Concentration in Plasma
- •Time Course of Drug Plasma Levels during Repeated Dosing (A)
- •Time Course of Drug Plasma Levels during Irregular Intake (B)
- •Accumulation: Dose, Dose Interval, and Plasma Level Fluctuation (A)
- •Dose–Response Relationship
- •Concentration–Effect Curves (B)
- •Concentration–Binding Curves
- •Types of Binding Forces
- •Agonists—Antagonists
- •Other Forms of Antagonism
- •Enantioselectivity of Drug Action
- •Receptor Types
- •Undesirable Drug Effects, Side Effects
- •Drug Allergy
- •Cutaneous Reactions
- •Drug Toxicity in Pregnancy and Lactation
- •Pharmacogenetics
- •Placebo (A)
- •Systems Pharmacology
- •Sympathetic Nervous System
- •Structure of the Sympathetic Nervous System
- •Adrenergic Synapse
- •Adrenoceptor Subtypes and Catecholamine Actions
- •Smooth Muscle Effects
- •Cardiostimulation
- •Metabolic Effects
- •Structure–Activity Relationships of Sympathomimetics
- •Indirect Sympathomimetics
- •Types of
- •Antiadrenergics
- •Parasympathetic Nervous System
- •Cholinergic Synapse
- •Parasympathomimetics
- •Parasympatholytics
- •Actions of Nicotine
- •Localization of Nicotinic ACh Receptors
- •Effects of Nicotine on Body Function
- •Aids for Smoking Cessation
- •Consequences of Tobacco Smoking
- •Dopamine
- •Histamine Effects and Their Pharmacological Properties
- •Serotonin
- •Vasodilators—Overview
- •Organic Nitrates
- •Calcium Antagonists
- •ACE Inhibitors
- •Drugs Used to Influence Smooth Muscle Organs
- •Cardiac Drugs
- •Cardiac Glycosides
- •Antiarrhythmic Drugs
- •Iron Compounds
- •Prophylaxis and Therapy of Thromboses
- •Possibilities for Interference (B)
- •Heparin (A)
- •Hirudin and Derivatives (B)
- •Fibrinolytics
- •Intra-arterial Thrombus Formation (A)
- •Formation, Activation, and Aggregation of Platelets (B)
- •Inhibitors of Platelet Aggregation (A)
- •Presystemic Effect of ASA
- •Plasma Volume Expanders
- •Lipid-lowering Agents
- •Diuretics—An Overview
- •NaCl Reabsorption in the Kidney (A)
- •Aquaporins (AQP)
- •Osmotic Diuretics (B)
- •Diuretics of the Sulfonamide Type
- •Potassium-sparing Diuretics (A)
- •Vasopressin and Derivatives (B)
- •Drugs for Gastric and Duodenal Ulcers
- •Laxatives
- •Antidiarrheal Agents
- •Drugs Affecting Motor Function
- •Muscle Relaxants
- •Nondepolarizing Muscle Relaxants
- •Depolarizing Muscle Relaxants
- •Antiparkinsonian Drugs
- •Antiepileptics
- •Pain Mechanisms and Pathways
- •Eicosanoids
- •Antipyretic Analgesics
- •Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
- •Cyclooxygenase (COX) Inhibitors
- •Local Anesthetics
- •Opioid Analgesics—Morphine Type
- •General Anesthesia and General Anesthetic Drugs
- •Inhalational Anesthetics
- •Injectable Anesthetics
- •Sedatives, Hypnotics
- •Benzodiazepines
- •Pharmacokinetics of Benzodiazepines
- •Therapy of Depressive Illness
- •Mania
- •Therapy of Schizophrenia
- •Psychotomimetics (Psychedelics, Hallucinogens)
- •Hypothalamic and Hypophyseal Hormones
- •Thyroid Hormone Therapy
- •Glucocorticoid Therapy
- •Follicular Growth and Ovulation, Estrogen and Progestin Production
- •Oral Contraceptives
- •Antiestrogen and Antiprogestin Active Principles
- •Aromatase Inhibitors
- •Insulin Formulations
- •Treatment of Insulin-dependent Diabetes Mellitus
- •Treatment of Maturity-Onset (Type II) Diabetes Mellitus
- •Oral Antidiabetics
- •Drugs for Maintaining Calcium Homeostasis
- •Drugs for Treating Bacterial Infections
- •Inhibitors of Cell Wall Synthesis
- •Inhibitors of Tetrahydrofolate Synthesis
- •Inhibitors of DNA Function
- •Inhibitors of Protein Synthesis
- •Drugs for Treating Mycobacterial Infections
- •Drugs Used in the Treatment of Fungal Infections
- •Chemotherapy of Viral Infections
- •Drugs for the Treatment of AIDS
- •Drugs for Treating Endoparasitic and Ectoparasitic Infestations
- •Antimalarials
- •Other Tropical Diseases
- •Chemotherapy of Malignant Tumors
- •Targeting of Antineoplastic Drug Action (A)
- •Mechanisms of Resistance to Cytostatics (B)
- •Inhibition of Immune Responses
- •Antidotes and Treatment of Poisonings
- •Therapy of Selected Diseases
- •Hypertension
- •Angina Pectoris
- •Antianginal Drugs
- •Acute Coronary Syndrome— Myocardial Infarction
- •Congestive Heart Failure
- •Hypotension
- •Gout
- •Obesity—Sequelae and Therapeutic Approaches
- •Osteoporosis
- •Rheumatoid Arthritis
- •Migraine
- •Common Cold
- •Bronchial Asthma
- •Emesis
- •Alcohol Abuse
- •Local Treatment of Glaucoma
- •Further Reading
- •Further Reading
- •Picture Credits
- •Drug Indexes
|
132 |
Cardiac Drugs |
|
|
|
|||
|
Cardiac Drugs |
|
|
|
Na+/K+-ATPases, (p.134), the Ca-antagonists |
|||
|
|
|
|
to Ca2+ channels (p.126), and antiarrhyth- |
||||
|
|
Possible ways of influencing heart function |
mics of the local anaesthetic type to Na+ |
|||||
|
|
(A). The pumping capacity of the heart de- |
channels (p.136) in the plasmalemma. |
|||||
|
|
pends on different factors: with increasing |
|
|||||
|
|
heart rate, the force of contraction increases |
Events underlying contraction and relaxa- |
|||||
|
|
(“positive staircase”); the degree of diastolic |
tion (B). The signal triggering contraction is |
|||||
|
|
filling regulates contraction amplitude (Star- |
apropagated actionpotential(AP) generated |
|||||
|
|
ling’s law of the heart). The sympathetic in- |
in the sinoatrial node. Depolarization of the |
|||||
|
|
nervation with its transmitter norepineph- |
plasmalemma leads to a rapid rise in cyto- |
|||||
|
|
rine and the hormone epinephrine promote |
solic Ca2+ levels, which causes contraction |
|||||
|
|
contractile force generation (but also oxygen |
(electromechanical coupling). The level of |
|||||
|
||||||||
|
|
consumption), and raise beating rate and |
Ca2+ concentration attained determines the |
|||||
|
|
excitability (p.88). The parasympathetic in- |
degree of shortening, i.e., the force of con- |
|||||
|
|
nervation lowers beat frequency because |
traction. Sources of calcium are: (a) extra- |
|||||
|
|
acetylcholine |
inhibits |
pacemaker |
cells |
cellular calcium entering the cell through |
||
|
|
(p.104). |
|
|
|
|
|
voltage-gated Ca2+ channels; (b) calcium |
|
|
From the influence of the autonomic ner- |
stored in the sarcoplasmic reticulum (SR); |
|||||
|
|
vous system it follows that all sympatholytic |
(c) calcium bound to the inside of the plas- |
|||||
|
|
or sympathomimetic and parasympatholytic |
malemma. The plasmalemma of cardiomyo- |
|||||
|
|
or parasympathomimetic drugs can produce |
cytes extends into the cell interior in the |
|||||
|
|
corresponding effects on cardiac perform- |
form of tubular invaginations (transverse tu- |
|||||
|
|
ance. These possibilities are exploited ther- |
buli). |
|||||
|
|
apeutically: for instance, β-blockers for sup- |
The trigger signal for relaxation isthe re- |
|||||
|
|
pressing excessive sympathetic drive (p.96); |
turn of the membrane potential to its resting |
|||||
|
|
ipratropium for treating sinus bradycardia |
level. During repolarization Ca2+ levels fall |
|||||
|
|
(p.108). An unwanted activation of the sym- |
below the threshold for activation of the |
|||||
|
|
pathetic system can result from anxiety, |
myofilaments (3 × 10–7 M): the plasmalem- |
|||||
|
|
pain, and other emotional stress. In these |
mal Ca binding sites regain their Ca-binding |
|||||
|
|
cases, the heart can be protected from harm- |
capacity; calcium ions are pumped back into |
|||||
|
|
ful stimulation |
by |
psychopharmaceuticals |
the SR lumen andtheplasmalemmal ATPases |
|||
|
|
such as benzodiazepines (diazepam and |
move Ca2+ that entered during systole back |
|||||
|
|
others; important in myocardial infarction). |
out of the cell under expenditure of energy. |
|||||
|
|
Cardiac work |
furthermore depends |
Additionally, Ca2+ isextrudedfromthe cellin |
||||
|
|
strongly on the state of the circulation sys- |
exchange for Na+ (Na/Ca exchanger). |
|||||
|
|
tem: physical rest or work demand appro- |
|
|||||
|
|
priate cardiac performance; the level of |
|
|||||
|
|
mean blood pressure is an additional deci- |
|
|||||
|
|
sive factor. Chronic elevation of afterload |
|
|||||
|
|
leads to myocardial insuf |
ciency. Therefore, |
|
||||
|
|
all blood pressure-lowering drugs can have |
|
|||||
|
|
an important therapeutic influence on the |
|
|||||
|
|
myocardium. Vasodilator |
substances |
(e.g., |
|
|||
nitrates) lower the venous return and/or peripheral resistance and, hence, exert a favorable effect in angina pectoris or heart failure.
The heart muscle cells can also be reached directly. Thus, cardiac glycosides bind to the
Luellmann, Color Atlas of Pharmacology © 2005 Thieme
All rights reserved. Usage subject to terms and conditions of license.

|
|
|
Cardiac Drugs |
133 |
A. Possible mechanisms for influencing heart function |
|
|
||
Drugs with |
|
|
Drugs with direct action |
|
indirect action |
|
|
|
|
|
|
|
Nutrient solution |
|
Psycho- |
|
|
|
|
tropic drugs |
|
|
|
|
|
|
|
Force |
|
Parasympathetic |
|
|
Rate |
|
|
|
|
|
|
Sympathetic |
Cardiac |
β -Sympathomimetics |
|
|
Phosphodiesterase inhibitors |
|
|||
|
|
|||
Epinephrine |
glycosides |
Rate |
|
|
|
|
Force |
|
|
Drugs altering |
|
|
Parasympathomimetics |
|
|
|
Catamphiphilic |
|
|
preand afterload |
|
|
Ca-antagonists |
|
|
|
|
|
|
|
|
|
Local anesthetics |
|
B. Processes in myocardial contraction and relaxation |
|
||||||
Contraction |
|
2+ |
|
-3 |
|
|
Membrane potential |
|
Ca |
|
10 M |
|
[mV] |
||
Electrical |
|
|
|
||||
excitation |
|
|
|
|
|
|
0 |
Ca-channel |
|
|
|
|
|
|
|
Sarcoplasmic |
|
|
|
|
|
|
|
reticulum |
|
|
|
|
|
cell |
Action potential |
|
|
|
|
|
|
||
Transverse tubule |
|
Ca2+ |
|
|
muscle |
|
|
|
|
|
|
|
|||
|
|
|
|
Heart |
|
||
Plasmalemmal |
|
10-5M |
|
|
-80 |
||
binding sites |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
t |
Relaxation |
Ca |
2+ |
10 |
-3 |
M |
|
Force |
|
|
||||||
|
|
|
|
|
|||
|
Na+ |
|
|
|
|
|
|
|
Ca2+ |
Ca-ATPase |
|
|
|
||
Na/Ca- |
|
|
|
|
|
cell |
Contraction |
exchange |
|
|
|
|
|
|
|
Ca2+ |
|
Ca2+ |
|
muscle |
|
||
Na+ |
|
Na+ |
|
||||
|
Ca2+ |
|
|
|
|||
|
|
|
|
|
Heart |
|
|
Plasma- |
|
10-7M |
|
|
|
||
lemmal |
|
|
|
|
|
|
|
binding sites |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
300 ms |
|
|
|
|
|
|
|
t |
Luellmann, Color Atlas of Pharmacology © 2005 Thieme
All rights reserved. Usage subject to terms and conditions of license.

134 Cardiac Drugs
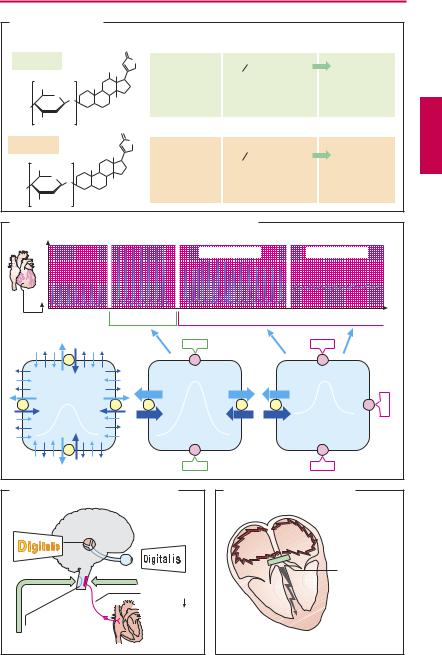
Cardiac Glycosides
Diverse plants are sources of sugar-contain- ing compounds (glycosides) that also contain a steroid ring system (structural formulas, A) and augment the contractile force of heart muscle: cardiotonic glycosides, cardiosteroids, “digitalis.”
The cardiosteroids possess a small therapeutic margin, signs of intoxication are arrhythmia and contracture (B). This therapeutic drawback can be explained by the mechanism of action.
Cardiac glycosides (CG) bind to the extracellular domain of Na+/K+-ATPases and exclude this enzyme molecule for a time from further ion transport activity. The high-af nity binding of CG is restricted to a particular conformation that the enzyme adopts during its transport cycle. In the resting state, Na+/K+-ATPase molecules are not binding partners. Under normal conditions only a fraction of the Na+/K+-ATPase transport activity is required to maintain the high gradients of Na+ and K+ across the plasmalemma. Low therapeutic concentrations of CG occupy onlya fraction of Na+/K+-ATPases; the decrease of the resulting pump activity can easily be compensated for by recruitment of resting ATPase molecules via a small increase of the intracellular Na+ concentration.
Attached to the ATPases there are Na+ channels which, upon binding of CG to the enzyme, lose their specificity for Na+ and are converted to nonselective, promiscuous channels: during systole, Ca2+ will easily pass through this channel owing to its huge gradient (almost 4 orders of magnitude!). This results in an increased Ca2+-influx and augmented contractile force. It should, however, be noted that the mode of action of cardiosteroids is still a matter of debate.
Mobilization of edema (weight loss) and lowering of heart rate are simple but decisive criteria for achieving optimal dosing. If ATPase activity is inhibited too much, K+ and Na+ homeostasisisdisturbed:the membrane
potential declines, arrhythmias occur. Intracellular flooding with Ca2+ prevents relaxation during diastole: contracture.
The CNS effects of CGs (C) are also due to binding to Na+/K+-ATPases. Enhanced vagal nerve activity causes a decrease in sinoatrial beating rate and velocity of atrioventricular conduction. In patients with heart failure, improved circulation also contributes to the reduction in heart rate. Stimulation of the area postrema leads to nausea and vomiting.
Indications for CGs are:
1 chronic congestive heart failure,
2 atrial fibrillation or flutter, where inhibition of AV conduction protects the ventricles from excessive atrial impulse activity and thereby improves cardiac performance (D).
Signs of intoxication are:
1Cardiac arrhythmias, which under certain circumstancesarelife-threatening,e.g.,si- nus bradycardia, AV-block, ventricular ex-
trasystoles, ventricular fibrillation (ECG); 2 CNS disturbances: characteristically, altered color vision (xanthopsia), and also fatigue, disorientation, hallucinations;
3 anorexia, nausea, vomiting, diarrhea;
4renal: loss of electrolytes and water; this must be differentiated from mobilization of edema fluid accumulated in front of the heart during congestive failure, an effect expected with therapeutic dosage.
Therapy of intoxication: administration of K+, which inter alia reduces binding of CG, but may impair AV-conduction; administration of antiarrhythmics, such as phenytoin or lidocaine (p.136); oral administration of colestyramine (p.160) for binding and preventing absorption of digitoxin present in the intestines (enterohepatic cycle), and most importantly injection of antibody (Fab) fragments that bind and inactivate digitoxin and digoxin. Compared with fullantibodies, fragments have superior tissue penetrability, more rapid renal elimination, and lower antigenicity.
Luellmann, Color Atlas of Pharmacology © 2005 Thieme
All rights reserved. Usage subject to terms and conditions of license.
|
|
|
|
|
|
Cardiac Glycosides |
135 |
||
A. Cardiac glycosides |
|
|
|
|
|
|
|
||
|
|
|
Enteral absorption |
Elimination |
|
|
|||
|
|
O |
|
|
|
|
|
|
|
Digoxin |
|
HO |
O |
t 1 2 : 2–3 days |
better control |
||||
|
|
|
|||||||
|
|
CH3 |
|
|
|
|
|
|
|
CH3 |
H3C |
|
~80% |
prolonged with |
|
|
|||
O |
|
OH |
decreased renal |
|
|
||||
O |
|
|
function |
|
|
||||
HO |
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
||
OH |
3 |
|
|
|
|
|
|
|
|
|
O |
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
||
Digitoxin |
|
|
O |
|
|
|
|
|
|
|
|
|
t 1 |
|
: 5–7 days |
Slow waning |
|
||
|
|
CH3 |
|
2 |
|
||||
|
|
|
|
|
|
of intoxication |
|||
CH3 |
H3C |
14 |
100% |
independent |
|||||
|
|
||||||||
O |
|
|
|
|
|||||
|
|
|
of renal |
|
|
||||
O |
3 |
OH |
|
|
|
||||
HO |
|
|
|
function |
|
|
|||
OH |
3 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
B. Therapeutic and toxic effects of cardiac glycosides (CG)
|
Contraction |
|
Arrhythmia |
|
|
|
|
|
Time |
“therapeutic” |
“toxic” |
|
Na+ Na/K-ATPase |
|
CG |
|
Na+ |
Na+ |
|
|
Coupling- |
Ca2+ |
|
|
Ca2+ |
||
K+ |
K+ |
K+ |
|
|
Heart muscle cell |
|
CG |
Contracture
Dose of cardiac glycoside (CG)
CG
Na+ |
|
Ca2+ |
CG |
K+ |
|
CG |
|
C. Cardiac glycoside effects on the CNS |
D. Cardiac glycoside effects in |
|
atrial fibrillation |
Disturbance |
“Re-entrant” |
of color vision |
excitation in |
|
atrial |
|
fibrillation |
|
Cardiac |
Excitation of |
glycoside |
|
|
N. vagus: |
Decrease in |
Heart rate |
|
|
ventricular |
Area postrema: |
rate |
|
|
nausea, vomiting |
|
Luellmann, Color Atlas of Pharmacology © 2005 Thieme
All rights reserved. Usage subject to terms and conditions of license.
