
- •Preface to the 3rd edition
- •General Pharmacology
- •Systems Pharmacology
- •Therapy of Selected Diseases
- •Subject Index
- •Abbreviations
- •General Pharmacology
- •History of Pharmacology
- •Drug and Active Principle
- •The Aims of Isolating Active Principles
- •European Plants as Sources of Effective Medicines
- •Drug Development
- •Congeneric Drugs and Name Diversity
- •Oral Dosage Forms
- •Drug Administration by Inhalation
- •Dermatological Agents
- •From Application to Distribution in the Body
- •Potential Targets of Drug Action
- •External Barriers of the Body
- •Blood–Tissue Barriers
- •Membrane Permeation
- •Binding to Plasma Proteins
- •The Liver as an Excretory Organ
- •Biotransformation of Drugs
- •Drug Metabolism by Cytochrome P450
- •The Kidney as an Excretory Organ
- •Presystemic Elimination
- •Drug Concentration in the Body as a Function of Time—First Order (Exponential) Rate Processes
- •Time Course of Drug Concentration in Plasma
- •Time Course of Drug Plasma Levels during Repeated Dosing (A)
- •Time Course of Drug Plasma Levels during Irregular Intake (B)
- •Accumulation: Dose, Dose Interval, and Plasma Level Fluctuation (A)
- •Dose–Response Relationship
- •Concentration–Effect Curves (B)
- •Concentration–Binding Curves
- •Types of Binding Forces
- •Agonists—Antagonists
- •Other Forms of Antagonism
- •Enantioselectivity of Drug Action
- •Receptor Types
- •Undesirable Drug Effects, Side Effects
- •Drug Allergy
- •Cutaneous Reactions
- •Drug Toxicity in Pregnancy and Lactation
- •Pharmacogenetics
- •Placebo (A)
- •Systems Pharmacology
- •Sympathetic Nervous System
- •Structure of the Sympathetic Nervous System
- •Adrenergic Synapse
- •Adrenoceptor Subtypes and Catecholamine Actions
- •Smooth Muscle Effects
- •Cardiostimulation
- •Metabolic Effects
- •Structure–Activity Relationships of Sympathomimetics
- •Indirect Sympathomimetics
- •Types of
- •Antiadrenergics
- •Parasympathetic Nervous System
- •Cholinergic Synapse
- •Parasympathomimetics
- •Parasympatholytics
- •Actions of Nicotine
- •Localization of Nicotinic ACh Receptors
- •Effects of Nicotine on Body Function
- •Aids for Smoking Cessation
- •Consequences of Tobacco Smoking
- •Dopamine
- •Histamine Effects and Their Pharmacological Properties
- •Serotonin
- •Vasodilators—Overview
- •Organic Nitrates
- •Calcium Antagonists
- •ACE Inhibitors
- •Drugs Used to Influence Smooth Muscle Organs
- •Cardiac Drugs
- •Cardiac Glycosides
- •Antiarrhythmic Drugs
- •Iron Compounds
- •Prophylaxis and Therapy of Thromboses
- •Possibilities for Interference (B)
- •Heparin (A)
- •Hirudin and Derivatives (B)
- •Fibrinolytics
- •Intra-arterial Thrombus Formation (A)
- •Formation, Activation, and Aggregation of Platelets (B)
- •Inhibitors of Platelet Aggregation (A)
- •Presystemic Effect of ASA
- •Plasma Volume Expanders
- •Lipid-lowering Agents
- •Diuretics—An Overview
- •NaCl Reabsorption in the Kidney (A)
- •Aquaporins (AQP)
- •Osmotic Diuretics (B)
- •Diuretics of the Sulfonamide Type
- •Potassium-sparing Diuretics (A)
- •Vasopressin and Derivatives (B)
- •Drugs for Gastric and Duodenal Ulcers
- •Laxatives
- •Antidiarrheal Agents
- •Drugs Affecting Motor Function
- •Muscle Relaxants
- •Nondepolarizing Muscle Relaxants
- •Depolarizing Muscle Relaxants
- •Antiparkinsonian Drugs
- •Antiepileptics
- •Pain Mechanisms and Pathways
- •Eicosanoids
- •Antipyretic Analgesics
- •Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
- •Cyclooxygenase (COX) Inhibitors
- •Local Anesthetics
- •Opioid Analgesics—Morphine Type
- •General Anesthesia and General Anesthetic Drugs
- •Inhalational Anesthetics
- •Injectable Anesthetics
- •Sedatives, Hypnotics
- •Benzodiazepines
- •Pharmacokinetics of Benzodiazepines
- •Therapy of Depressive Illness
- •Mania
- •Therapy of Schizophrenia
- •Psychotomimetics (Psychedelics, Hallucinogens)
- •Hypothalamic and Hypophyseal Hormones
- •Thyroid Hormone Therapy
- •Glucocorticoid Therapy
- •Follicular Growth and Ovulation, Estrogen and Progestin Production
- •Oral Contraceptives
- •Antiestrogen and Antiprogestin Active Principles
- •Aromatase Inhibitors
- •Insulin Formulations
- •Treatment of Insulin-dependent Diabetes Mellitus
- •Treatment of Maturity-Onset (Type II) Diabetes Mellitus
- •Oral Antidiabetics
- •Drugs for Maintaining Calcium Homeostasis
- •Drugs for Treating Bacterial Infections
- •Inhibitors of Cell Wall Synthesis
- •Inhibitors of Tetrahydrofolate Synthesis
- •Inhibitors of DNA Function
- •Inhibitors of Protein Synthesis
- •Drugs for Treating Mycobacterial Infections
- •Drugs Used in the Treatment of Fungal Infections
- •Chemotherapy of Viral Infections
- •Drugs for the Treatment of AIDS
- •Drugs for Treating Endoparasitic and Ectoparasitic Infestations
- •Antimalarials
- •Other Tropical Diseases
- •Chemotherapy of Malignant Tumors
- •Targeting of Antineoplastic Drug Action (A)
- •Mechanisms of Resistance to Cytostatics (B)
- •Inhibition of Immune Responses
- •Antidotes and Treatment of Poisonings
- •Therapy of Selected Diseases
- •Hypertension
- •Angina Pectoris
- •Antianginal Drugs
- •Acute Coronary Syndrome— Myocardial Infarction
- •Congestive Heart Failure
- •Hypotension
- •Gout
- •Obesity—Sequelae and Therapeutic Approaches
- •Osteoporosis
- •Rheumatoid Arthritis
- •Migraine
- •Common Cold
- •Bronchial Asthma
- •Emesis
- •Alcohol Abuse
- •Local Treatment of Glaucoma
- •Further Reading
- •Further Reading
- •Picture Credits
- •Drug Indexes

294 Antiparasitic Drugs
Antimalarials
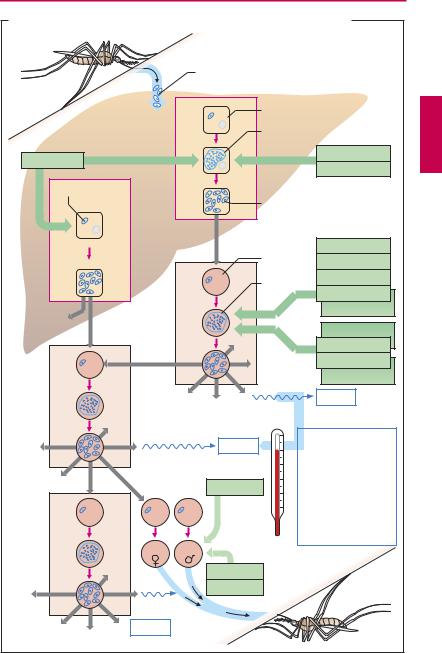
The causative agents of malaria are plasmodia, unicellular organisms (Order Hemosporidia, Class Protozoa). The infective form, the sporozoite, is inoculated into skin capillaries when infected female Anopheles mosquitoes (A) suck blood from humans. The sporozoites invade liver parenchymal cells, where they develop into primary tissue schizonts. These give rise to numerous merozoites that enter the blood. The preerythrocytic stage is asymptomatic. In blood, the parasite enters erythrocytes (erythrocytic stage), where it again multiplies by schizogony, resulting in the formation of more merozoites. Rupture of the infected erythrocytes releases the merozoites and pyrogens. A fever attack ensues and more erythrocytes are infected. The generation period for the next crop of merozoites determines the interval between fever attacks. With Plasmodium vivax and P. ovale, there can be a parallel multiplication in the liver (paraerythrocytic stage). Moreover, some sporozoites may become dormant in the liver as “hypnozoites” before entering schizogony.
Different antimalarials selectively kill the parasite’s different developmental forms. The mechanism of action is known for some agents: Chloroquine and quinine accumulate within the acidic vacuoles of blood schizonts and inhibit polymerization of heme released from digested hemoglobin, free heme being toxic for the schizonts. Pyrimethamine in-
hibits protozoal |
dihydrofolate |
reductase |
(p.274), as does |
chlorguanide |
(proguanil) |
via its active metabolite cycloguanil. The sulfonamide sulfadoxine inhibits synthesis of dihydrofolic acid (p.274). Dihydrofolate reductase is also blocked by cycloguanil, the active form of proguanil. Atoquavone suppresses synthesis of pyrimidine bases, probably by interfering with mitochondrial electron transport. Artemesinin derivatives (artemether, artesunate) originate from the East Asian plant Qinghaosu (Artemisia sp.) Its antischizontal effect appears to involve a re-
action between heme iron and the epoxide group of these compounds.
Antimalarial drug choice takes tolerability and plasmodial resistance into account.
Tolerability. The oldest antimalarial, quinine, has the smallest therapeutic margin. All newer agents are rather well tolerated.
Plasmodium falciparum, responsibleforthe most dangerous form of malaria, is particularly prone to develop drug resistance. The prevalence of resistant strains rises with increasingfrequencyofdruguse.Resistancehas been reported for chloroquine and also the combination pyrimethamine/sulfadoxine.
Drug choice for antimalarial chemoprophylaxis. In areas with a risk of malaria, continuous intake of antimalarials affords the best protection against the disease, though not against infection. Primaquine would be effective against primary tissue schizonts of all plasmodial species; however, it is not used for long-term prophylaxis because of unsatisfactory tolerability and the risk of plasmodial resistance. Instead, prophylactic regimens employ agents against blood schizonts. Depending on the presence of resistant strains, use can be made of chloroquine, and/or proguanil, mefloquine, the tetracycline doxycycline, as well as the combination of atoquavone and proguanil.
These drugs do not prevent the (symp- tom-free) hepatic infection but only the dis- ease-causing infection of erythrocytes (“suppression therapy”). On a person’s return from an endemic malaria region, a two-week course of primaquine is adequate for eradication of the late hepatic stages (P. vivax and
P. ovale).
Protection from mosquito bites (with nets, skin-covering clothes, etc.) is a very important prophylactic measure.
Therapy. Antimalarial therapy employs the same agents, in addition to the combinations of artemether plus lumefantrine or pyrimethamine plus sulfadoxine.
Luellmann, Color Atlas of Pharmacology © 2005 Thieme
All rights reserved. Usage subject to terms and conditions of license.
|
|
Antimalarials |
295 |
|
A. Malaria: stages of the plasmodial life cycle in the human: therapeutic options |
|
|||
|
Sporozoites |
|
|
|
|
|
Hepatocyte |
|
|
|
|
Primary tissue schizont |
|
|
Primaquine |
cycle |
|
Proguanil |
|
Preerythrocytic 1-4 weeks |
P. falciparum |
|
||
|
|
Pyrimethamine |
|
|
Hypnozoite |
Merozoites |
|
|
|
|
|
|
||
|
|
|
|
|
|
Only |
|
|
|
|
P. vivax |
|
Chloroquine |
|
|
P. ovale |
|
|
|
|
Erythrocyte |
|
||
|
|
|
||
|
|
Blood |
Mefloquine |
|
|
|
Quinine |
|
|
|
|
schizont |
|
|
|
|
|
|
|
|
cycle |
|
Lumefantrine |
|
|
|
Artemether |
|
|
|
Erythrocytic |
|
|
|
|
|
Atovaquone |
|
|
|
|
Proguanil |
|
|
|
|
Pyrimethamine |
|
|
|
|
|
|
|
|
|
|
Sulfadoxine |
|
|
|
|
Fever |
|
|
Fever |
|
2 days : |
|
|
|
Tertian malaria |
|
|
|
|
|
P. vivax, P. ovale |
|
|
|
|
3 days: |
|
|
Primaquine |
|
Quartan malaria |
|
|
|
P. malariae |
|
|
|
|
|
|
|
|
|
|
No fever |
|
|
|
|
periodicity: |
|
|
|
|
Pernicious malaria: |
|
|
|
|
P. falciparum |
|
|
not P. falciparum |
|
|
|
|
Chloroquine |
|
|
|
|
Gametocytes |
|
|
|
|
Quinine |
|
|
|
|
Fever |
|
|
|
Luellmann, Color Atlas of Pharmacology © 2005 Thieme
All rights reserved. Usage subject to terms and conditions of license.

extrapyramidal motor disturbances, Parkin-
|
Other Tropical Diseases |
son-like signs, coma, and death. Therapy: |
|||||
|
|
||||||
|
In addition to malaria, other tropical diseases |
Long-term suramine i.v. or pentamidine(less |
|||||
|
and their treatment will be considered for |
effective); |
arsenicals |
(e.g., |
melarsoprol, |
||
|
the following reasons. (1) Owing to the tre- |
highly toxic), when the CNS is involved. |
|||||
|
mendous growth in global travel, inhabitants |
T. cruzi is confined to Central and South |
|||||
|
of temperate climatic zones have become |
America and transmitted by blood-sucking |
|||||
|
exposed to the hazard of infection with trop- |
reduviid bugs. These parasites preferentially |
|||||
|
ical disease pathogens. (2) The spread of |
infiltrate the cardiac musculature, where |
|||||
|
some tropical diseases is of unimaginable |
they cause damage to muscle fibers and the |
|||||
|
dimensions, with humans victims number- |
specialized conducting tissue. Death results |
|||||
|
ing in the millions. The pharmacotherapeutic |
from cardiac failure. Therapy: unsatisfactory. |
|||||
|
|||||||
|
possibilitiesknown to date will be presented. |
|
|
|
|
|
|
|
|
Schistosomiasis |
(bilharziasis) |
(see |
also |
||
|
Amebiasis. The causative agent, Entamoeba |
p.292). The causative organisms are trema- |
|||||
|
histolytica, lives and multiplies in the colon |
todes with a complex life cycle that need |
|||||
|
(symptom: diarrhea), its cyst form residing |
(aquatic) snails as intermediate hosts. Free- |
|||||
|
also in the liver among other sites. In tropical |
swimming larval cercariae penetrate the in- |
|||||
|
regions, up to half the population can be |
tact skin of humans. The adult worms (Schis- |
|||||
|
infested, transmission occurring by the fe- |
tosoma mansoni, D) livein thevenousvascu- |
|||||
|
cal–oral route. The most effective treatment |
lature. Occurrence: tropical countries rich in |
|||||
|
against both intestinal infestation and sys- |
aquatic habitats. About 200 million humans |
|||||
|
temic disease is administration of metroni- |
are af icted. Therapy: praziquantel, 10– |
|||||
|
dazole. If monotherapy fails, combination |
40 mg/kg,singledose,ishighlyeffectivewith |
|||||
|
therapy with chloroquine, emetine or tetra- |
minimal adverse effects. Substancesreleased |
|||||
|
cyclines may be indicated. |
from decaying worms may cause problems. |
|||||
|
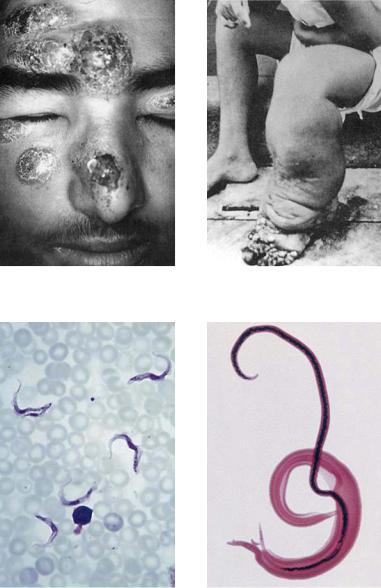
Leishmaniasis. The causative agents are flag- |
Filariasis. In its microform, Wuchereria ban- |
|||||
|
ellated protozoa that are transmitted by |
crofti istransmittedbymosquitoes;theadult |
|||||
|
sand flies to humans. The parasites are taken |
parasites live in the lymph system and cause |
|||||
|
up into phagocytes, where they remain in |
inflammations and blockage of lymph drain- |
|||||
|
phagolysosomes and multiply until the cell |
age leading to elephantiasis in extreme cases |
|||||
|
dies and the parasites can infect new cells. |
(B). Therapy: diethylcarbamazepine for sev- |
|||||
|
Symptoms: A visceral form, known as kala- |
eral weeks; adverse reactions are chiefly due |
|||||
|
azar, and cutaneous or mucocutaneous |
to products from disintegrating worms. |
|||||
|
forms exist (A). An estimated 12 million hu- |
|
|
|
|
|
|
|
mans are affected. Therapy is dif cult; pen- |
Onchocerciasis (“River Blindness”). The |
|||||
|
tavalent antimonial compounds, such as sti- |
causative organism is Onchocerca volvulus, |
|||||
|
bogluconate, must be given for extended |
a filaria transmitted by black flies (genus |
|||||
|
periods. Adverse effects are pronounced. |
Simulium). The adult parasites (several cen- |
|||||
|
|
timeters long) form tangles and proliferating |
|||||
|
Trypanosomiasis. The pathogens, Trypano- |
nodules (onchocercomas) in the skin and |
|||||
|
soma brucei (sleeping sickness) and T. cruzi |
have a particular propensity for invading |
|||||
|
(Chagas disease), are flagellated protozoa. T. |
the eyeball, resulting in blindness. About 20 |
|||||
|
brucei (C) is transmitted by the tsetse fly, |
million people inhabiting banks of fast-flow- |
|||||
|
distributed in West and East Africa. An initial |
ing rivers are af |
icted with river blindness. |
||||
|
stage (swelling of lymph nodes, malaise, |
Therapy: |
ivermectin |
(0.15 mg/kg, |
single |
||
|
hepatosplenomegaly, among others) is fol- |
dose); adverse reactions are in part caused |
|||||
|
lowedLuellmann,by invasionColor ofAtlastheofCNSPharmacologywith lethargy,© 2005by disintegratingThieme |
worms. |
|
|
|||
|
All rights reserved. Usage subject to terms and conditions of license. |
|
|
||||
|
|
|
|
|
|
Other Tropical Diseases |
297 |
|
|
||
|
|
A. Cutaneous leishmaniasis |
|
|
|
B. Elephantiasis |
|
|
|
|
|
|
|
Causative agent: Leishmania major |
|
|
Causative agent: Wuchereria bancrofti |
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
C. Trypanosoma brucei |
|
|
|
D. Schistosoma mansoni |
|
|
Causative agent of sleeping sickness |
|
|
Causative agent of bilharziasis |
||
|
|
|
|
|
|
|
Luellmann, Color Atlas of Pharmacology © 2005 Thieme
All rights reserved. Usage subject to terms and conditions of license.
